Abstract
Background:
Although the adverse health effects of ambient air pollution are well documented, evidence on the depression effects of household air pollution (HAP) are scarce.
Objectives:
We investigated the effects of HAP exposure from the use of solid fuel on depression using a nationally representative dataset of middle-aged and older population in China.
Methods:
By employing the propensity score matching method, we first matched the type of household fuel based on background information, including demographic characteristics, lifestyles, health status, and household economic levels. Based on the matched data, we conducted OLS and logistic regressions with cluster standard error at community level to examine the effects of household solid fuel use on depression and adjusted for potential confounders. Heterogeneous effects for vulnerable population were also considered.
Results:
We found a significantly higher Center for Epidemiologic Studies Depression Scale (CES-D) score and depression risk among current household solid fuel users. After matching and adjusting for potential confounders, current solid fuel users had a higher CES-D score of 0.59 (95% confidence interval [CI]: 0.31, 0.89) than clean fuel users. The OR of depression risk were 1.26 (95% CI: 1.14, 1.41). Solid fuel users had the highest CES-D scores (β = 0.99, 95% CI: 0.62, 1.36) and depression risk (OR = 1.49, 95% CI: 1.30, 1.73) for over five years. These associations were generally higher in females, participants aged 65 years and older, with a BMI ≥ 25, with low education, with low household economic levels, and those suffer from chronic diseases, including diabetes, chronic lung diseases, and cardiovascular diseases.
Conclusions:
Exposure to HAP from solid fuel combustion was linked with strong depression outcomes. Findings suggested a need to strengthen public health efforts, such as controlling the social, health, and economic costs of depression by taking the physical environment, including HAP exposure, into account.
Keywords: Depression, Household solid fuel use, Household air pollution, Propensity Score Matching, CHARLS
Graphical Abstract
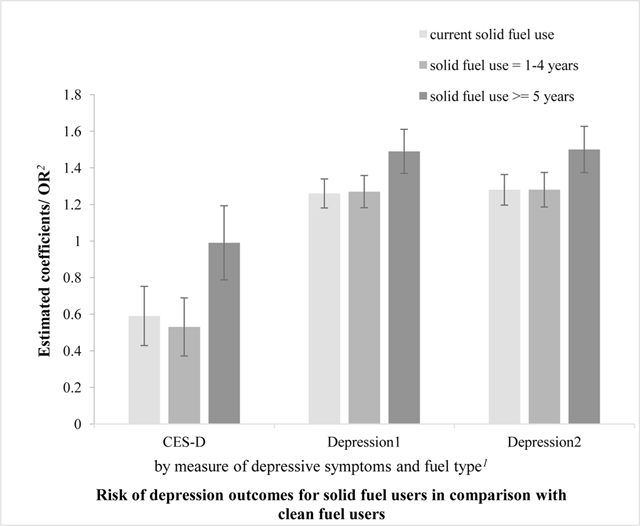
Notes:
Depression1: depression episode when the CES-D score is 10 or above;
Depression2: depression episode when the CES-D score is 12 or above;
1 Reference group: clean fuel users
2 Estimated coefficients and confidence intervals from the linear regression for “CES-D” are displayed. Odds ratios (OR) from the logistic regression for “Depression1” and “Depression2” are displayed.
1. Background
Depression is one of the most common mental health problems nowadays. It results from a complex interaction of biological, physical, psychological, and social factors (Fuller-Thomson et al. 2016; Kessler and Bromet 2013; Paykel 2008). Depression has been experienced by a large number of elderly worldwide, which contributes to a high risk of disability, substantial expenditure on health services, decreased labor productivity, and thus, low quality of life which may even lead to suicide (Ekman et al. 2013; Goldney et al. 2004; Ruo et al. 2003). These adverse effects of depression can eventually lead to a high risk of mortality. In 2013, depressive disorders accounted for approximately 30% of all mental disorder disability-adjusted life years in China and is expected to increase further (Charlson et al. 2016). Depression can be triggered by various factors, including genetic susceptibility, brain damage, substance abuse, lifestyle (e.g., smoking and drinking), socioeconomic status, and so on (Cole and Dendukuri 2003; Lim et al. 2012; Pun et al. 2017).
Recent epidemiological studies reported that physical environmental factors like short- and long-term ambient air pollution exposure also have effects on neurobehavioral and psychological outcomes. These factors particularly increase the risk of depression and decreasing cognitive function. However, results were not entirely consistent (Kim et al. 2016; Power et al. 2011; Vert et al. 2017; Wang et al. 2018; Wang et al. 2014; Zhang et al. 2017; Zijlema et al. 2016). For example, elevation in concentrations of ambient air pollutants was linked with emergency room visits for depression in Canada (Szyszkowicz et al. 2016), increased risk of hospitalization for depression in China (Wang et al. 2018), and the use of antidepressants and benzodiazepines (Vert et al. 2017). Studies also focused on susceptible population; depression was considerably impacted by increasing ambient air pollution among the elderly (Lim et al. 2012; Pun et al. 2017), and middle-aged and older women in the U.S. (Kioumourtzoglou et al. 2017). Additionally, the effects of air pollution on depression was strong among females, individuals aged 65 years and above, and those who suffered from chronic diseases such as cardiovascular diseases (CVDs) and diabetes mellitus (Cho et al. 2014; Kim et al. 2016; Wang et al. 2018).
Compared with ambient air pollution, limited evidence is available on associations between mental health and household air pollution (HAP) from solid fuel consumption like coal and biomass (e.g., charcoal, wood, crop residues, and animal dung) worldwide (Bonjour et al. 2013), except for a study on the association between biomass and depression among premenopausal women in India (Banerjee et al. 2012). More than 700 million people in China depend on solid fuel as their major household energy source, resulting in numerous toxic air pollutants (e.g., particles, nitrogen oxide, carbon monoxide, and organic air pollutants) and high indoor concentrations of HAP (Bonjour et al. 2013; Smith et al. 2013). HAP has been one of the leading contributors to disease burden (Clark Maggie et al. 2013) and is responsible for approximately 3.8 million deaths in 2016 (WHO 2019). Despite many studies on the physical health impacts of HAP on many diseases, such as CVDs and respiratory diseases (Baumgartner et al. 2011; Guan et al. 2016; Hystad et al. 2019; Li et al. 2019; Yan et al. 2016), the potential effects of HAP from the use of solid fuel on depression in China and worldwide have not been evaluated to date.
Depression is highly prevalent among the elderly. Given the substantial personal and societal burdens from depression and the problems of an aging population and air pollution in China, identifying modifiable risk factors for depression is imperative. The goal of the present study is to evaluate the effects of HAP from solid fuel combustion on depression among middle-aged and older individuals, which is one of the most sensitive age groups to air pollution and depression. Evaluating the effects of household solid fuel use on depression may provide insights into the mental effects of HAP and information to help in energy, environmental, and health policy making.
2. Data and methods
2.1. Data source
We obtained our data from the China Health and Retirement Longitudinal Study (CHARLS, website: http://charls.pku.edu.cn/zh-CN), a nationally representative longitudinal survey of more than 17,000 persons in China aged 45 years or older, covering 150 counties in 28 provinces. The study is biennially conducted by the National School of Development at Peking University. Ethical approval for the study was granted by the Ethical Review Committee of Peking University, and all participants provided informed consent. Three national waves of data are available to date: waves in 2011, 2013, and 2015. Most of the survey data are self-reported. Detailed information about this survey is available in Zhao et al. (2014).
Our sample included participants who were involved in all three waves of the study. We employed wave 2015 in our main analysis. For eligibility, we first excluded participants who were below 45 years old; then, individuals diagnosed with memory-related diseases (e.g., dementia and Alzheimer’s disease), brain damage, or mental retardation. We also excluded participants who use unidentifiable fuels. Lastly, samples with missing values of major outcomes and independents were also dropped. The final sample before analysis is N=9,107.
2.2. Depression outcomes
Depressive symptoms were measured using the 10-item Center for Epidemiologic Studies Depression (CES-D) scale (Andresen et al. 1994), which is widely used to measure depression among older adults in prior studies (Guo et al. 2017). The answers are indicated in a four-scale metric, from “rarely” to “some days” (1–2 days), “occasionally” (3–4 days), or “most of the time” (5–7 days). For the two positive questions— “I was happy” and “I felt hopeful about the future”—answers were reversely coded before the summary. We then recorded all answers as values, from 0 to 3 as “rarely” and “most of the time,” respectively. The total range of CES-D scores in this study was 0–30, with higher scores indicating greater depression severity. A cutoff of 10 was used to define a binary variable of depression episode based on previous studies (Andresen et al. 1994), with 1 for individuals who had a score of 10 or above, otherwise 0. According to self-reported chronic disease history, individuals diagnosed with emotional, nervous, or psychiatric problems, taking antidepressants, tranquilizers, or sleeping pills, or receiving psychiatric or psychological treatment were also considered to be suffering from an episode of depression, which is coded as 1.
2.3. Solid fuel use
According to CHARLS, cooking fuel was categorized as clean fuel (liquefied gas, natural gas, and electricity) and solid fuel (coal, biomass charcoal, wood, and straw). Two measures for fuel types as surrogates of HAP were used as independents in this study. The first was whether household solid fuel was used at the time of the survey (current solid fuel users), with 1 indicating “yes” and 0 otherwise. The second was the duration of solid fuel use, which was marked as 0, 1–4 years, and 5 years or more. The duration of solid fuel use was calculated based on the fuel types used in waves 2011, 2013, and 2015. For example, one was considered a user of solid fuel for 5 years or more if he/she used solid fuel for all three waves. If an individual used clean fuel for all three waves, then the duration of solid fuel use is 0 years. For the subgroup analysis, the duration of solid fuel use was categorized as a dummy variable indicating a duration of 5 years or more and less than 5 years.
2.4. Covariates
Following a previous study (Cole and Dendukuri 2003; Lim et al. 2012; Vert et al. 2017; Zhang et al. 2017), we considered potentially confounding covariates, including demographic characteristics (age, gender, education, rural area, marital status, and retirement status), lifestyle (smoking, sleep time, and social activity participation), health status (body mass index [BMI], diabetes, lung diseases, CVDs, disability, and self-reported health), and household economic level to be associated with depression.
In this study, education was categorized as primary or below, middle school, and college or above. We also included retirement as a dichotomous variable because it is a possible risk factor for depression (Reitzes et al. 1996). Non-smokers, defined as those who had never smoked, were given the value of 0, whereas those who had smoked were given the value of 1. Drinkers were defined as a binary variable equal to 1 for regular drinkers who drink more than once a week. We categorized sleeping time into three groups: less than 7 hours, 7–9 hours, and more than 9 hours. Social activity participation was a dummy variable, with 1 suggesting that the observation has done at least one of the enumerated activities during the last month, and 0 otherwise. BMI was calculated by dividing weight by squared height, with a BMI≥25 considered obese. For chronic diseases, we coded diabetes and CVDs (hypertension, dyslipidemia, heart diseases, stroke, and asthma) using the “Health Status” section of CHARLS. CVDs equaled 1 if a participant suffer from one or more of the five diseases mentioned, and 0 otherwise. Disability was coded as 1 if a participant had a physical disability, vision problem, hearing problem, or speech impediment, and 0 otherwise. Self-reported health was defined as poor, fair, or good. Lastly, given that no direct indicator for individual or household economic level or income level is provided in CHARLS, we obtained household economic levels by using a principal component analysis (PCA) based on household living expenditure and household ownership of equipment, consumer durables, and other valuables. An indicator was excluded if everybody or nobody owned a given item. A composite score based on the first component generated from PCA has been suggested to be a qualified measure of socioeconomic status and has been widely employed in previous studies (Krefis et al. 2010; Neupane et al. 2015; Vyas and Kumaranayake 2006).
2.5. Statistical Analysis
The major empirical challenge for this study is that the fuel type choice may not be randomly assigned. For example, participants with high income or high educational attainment are likely to choose clean fuel (Jeuland et al. 2015), which can lead to biased estimation. The PSM method is a useful tool that allows selection bias and addresses covariate imbalance between treated and comparison groups in observational studies. However, it is underused in epidemiological research (Garrido et al. 2014; Juhn et al. 2010). Therefore, we employed the PSM technique to control potential selection bias in the empirical estimation.
We first calculated propensity scores by fitting a logit regression model to predict the probability of using solid fuel, which was matched by available background variables as follows:
| (1) |
where represents the propensity scores of individual i, is a vector including all the matching covariates listed in the part of Covariates, and is the error term. A full matching technique with k-nearest neighbor matching within 0.2 SD caliper was employed for matching as suggested by Austin (2013). Matching quality and balance were then checked by testing the common support assumption and the overlap in the range of propensity scores across treatment and control groups. Covariate balance of the matched data was also examined by testing the absolute standard bias (ASB) between the treatments and controls after matching. Balance was assumed to be well achieved when the ASB was less than 0.25 after matching (Ho et al. 2007; Stuart and Green 2008).
Based on the matched data above, final models using ordinary least squares and logistic regressions were performed to obtain the average treatment effect on the treated (ATT). The matching covariates and propensity scores were retained in all models to account for any remaining imbalance and potential confounding effects. Our main model specification is as follows:
| (2) |
where the dependent variable is depression outcomes of respondent i. Two different depression outcomes were examined including a continuous variable of CES-D scores and a dichotomous variable indicating a depression episode. The key variable is the HAP measure of respondent i, which is surrogated by the household fuel type. Two different independents (current solid fuel users and duration of solid fuel use) were employed in the models and regressed separately. is a vector including all the matching covariates. represents the propensity scores of individual i obtained from model (1). is the error term. The coefficient of interest here is , which measures the ATT of HAP on depression outcomes. A 95% CI was reported using standard errors clustered at the community level.
We also conducted several additional sensitivity analyses to evaluate the robustness of our findings. First, previous studies on elderly Chinese claimed that a cutoff of 12 is an optimal threshold to identify clinical depression (Cheng et al. 2016; Cheng and Chan 2005). Therefore, we repeated all analyses using 12 to define a depression episode. Second, previous studies suggested that the neurocognitive effects of air pollution may vary across population groups, socioeconomic status (education and income levels), and history of chronic diseases (Cho et al. 2014; Kim et al. 2016). We likewise considered subgroup analyses to examine the possible heterogeneous effects for gender, age (≥65 or <65), obesity (BMI ≥25 or <25), educational attainment, household economic levels, and chronic diseases (diabetes, chronic lung diseases, and CVDs). Third, participants taking antidepressants, tranquilizers or sleeping pills, or receiving psychiatric or psychological treatment were excluded in all models for another sensitivity analysis. Lastly, given that the results of PSM may vary according to different matching methods (Garrido et al. 2014), we repeated all the analyses by using k-nearest neighbor matching (k=2, 3, or 4), caliper matching, and kernel matching to test the robustness of our results.
All statistical analyses were conducted using STATA version MP14.0 software. P-value < 0.05 was considered as statistically significant.
3. Results
3.1. Summary of characteristics
A total of 9,107 participants in wave 2015 were included in our study. Table 1 summarizes the characteristics of the study population across different fuel types. Over half (53.5%) were female with a mean age of 62.6 years old (SD: 9.33). The average CES-D score was 7.35 (SD: 6.06) and 9.07 (SD: 6.70) for current clean and solid fuel users, respectively. Compared with solid fuel users, participants who use clean fuel were more likely to suffer from a depression episode (28.4% and 39.4%). Two groups using different fuel types were statistically different before matching in most of the covariates except for gender, marital status, drinking habits, and CVDs.
Table 1.
Characteristics summary of currently clean fuel users and Solid fuel users
| variable | Current clean fuel users (N=5007) a | Current solid fuel users (N=4100) a | p-value b | ||
|---|---|---|---|---|---|
|
|
|
||||
| Mean (N) | SD (N%) | Mean (N) | SD (N%) | ||
|
|
|
|
|
||
| CES-D scores | 7.35 | 6.06 | 9.07 | 6.70 | <0.001 |
| Depression using cutoff of 10 | 1,414 | 28.44 | 1,614 | 39.37 | <0.001 |
| Depression using cutoff of 12 | 1,037 | 20.71 | 1,246 | 30.39 | <0.001 |
| Duration of solid fuel use | |||||
| 0 yrs | 3,970 | 79.29 | 0 | 0.00 | <0.001 |
| 1–4yrs | 1,037 | 20.71 | 1,061 | 25.88 | |
| > =5 yrs | 0 | 0.00 | 3,039 | 74.12 | |
| Age | 62.59 | 9.32 | 64.21 | 9.13 | <0.001 |
| Gender | |||||
| Female | 2,679 | 53.52 | 2,191 | 53.44 | 0.71 |
| Male | 2,327 | 46.48 | 1,909 | 46.56 | |
| Rural area | 3,210 | 64.12 | 3,735 | 91.10 | <0.001 |
| Education | |||||
| primary or less | 3,093 | 61.79 | 3,255 | 79.45 | <0.001 |
| middle school | 1,762 | 35.02 | 827 | 20.19 | |
| college or above | 151 | 3.02 | 15 | 0.37 | |
| Household economic level c | 0.31 | 1.97 | −1.12 | 1.37 | <0.001 |
| Marital status | 3,901 | 77.93 | 3,212 | 78.36 | 0.62 |
| Retire status | 957 | 19.26 | 219 | 5.38 | <0.001 |
| Smokers | 1,985 | 40.91 | 1,752 | 43.88 | 0.005 |
| Drinkers | 1,286 | 25.72 | 1,005 | 24.54 | 0.20 |
| Sleep time | |||||
| <7 hrs | 2,559 | 52.88 | 2,033 | 51.92 | <0.001 |
| 7–9 hrs | 2,061 | 42.59 | 1,645 | 42.01 | |
| >9 hrs | 219 | 4.53 | 238 | 6.08 | |
| Social activity participation | 2,868 | 57.31 | 1,825 | 44.52 | <0.001 |
| BMI | 23.36 | 3.64 | 23.95 | 3.65 | <0.01 |
| Diabetes | 305 | 4.9 | 544 | 10.73 | <0.001 |
| Lung diseases | 738 | 13.39 | 806 | 18.75 | <0.001 |
| CVDs | 2,271 | 44.12 | 2,862 | 45.54 | 0.42 |
| Disability | 530 | 10.59 | 590 | 14.39 | <0.001 |
| Self-reported Health | |||||
| Bad | 1,077 | 22.04 | 1,271 | 31.82 | <0.001 |
| Fair | 2,660 | 54.43 | 1,932 | 48.37 | |
| Good | 1,150 | 23.53 | 791 | 19.80 | |
Notes: CES-D, The Center for Epidemiological Studies Depression Scale; BMI, Body Mass
Index; CVDs, cardiovascular diseases.
Total observation of different variables was slightly different due to the missing value
P-value for comparing the difference between current solid fuel users versus current clean fuel users, given by t test for continuous variables and Chi-square test for categorical variables
Household economic level was obtained using PCA method
3.2. Matching quality and balancing tests
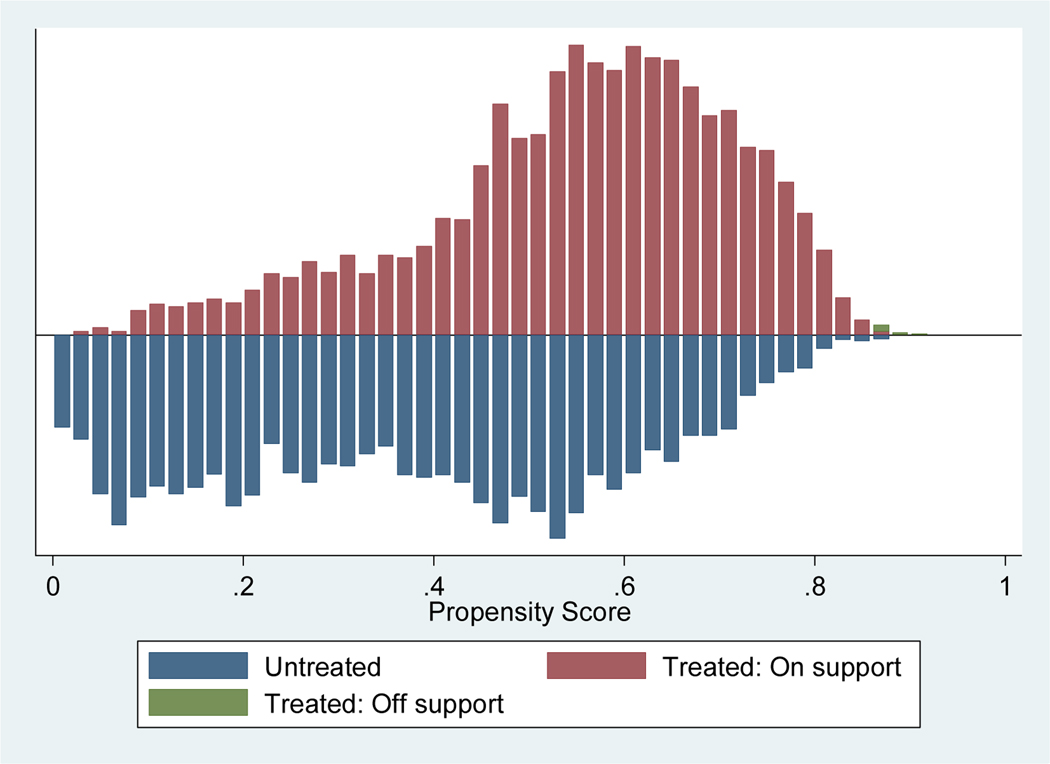
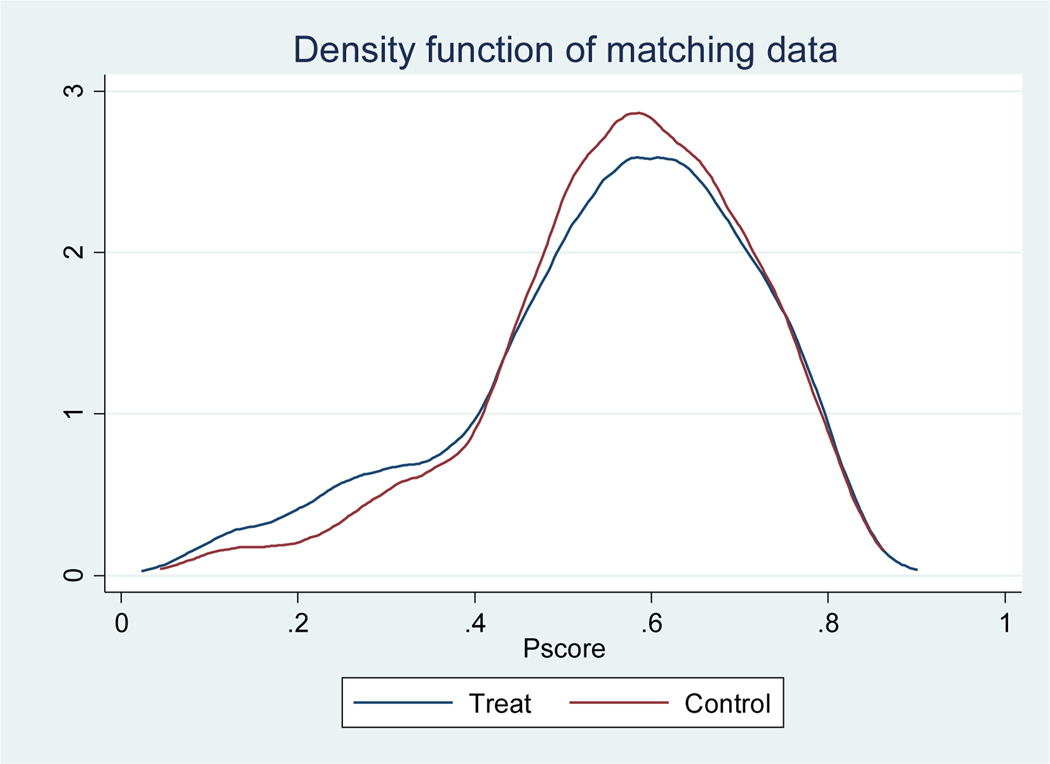
To validate the quality of the matching, we examined the assumption of common support of the propensity scores. Appendix figure 1 (AF1) presents the common range of propensity scores of the matching data. Almost all observations were within the common range (on support), and only a small number of samples were off support after matching. Appendix figure 2 (AF2) presents the density function of propensity scores after matching. Similar distributions of the matched cohort in propensity scores suggested that most of the propensity score intervals of the treated and control groups have substantial overlap. This finding indicates that our matching sample can meet the matching requirements for the following estimation.
Table 2 shows the results of covariates balancing test. Almost all the standard bias of the matching covariates are reduced substantially and all of ASB are below 10%. Moreover, the pseudo R2 is less than 0.01 for the balance testing, and the likelihood ratio test of joint significance became nonsignificant after matching. This result suggests no systematic difference between the treatment and control group. Results indicated good quality of data matching.
Table 2.
Covariate balancing of nearest-neighbor with caliper matching
| Variable | Mean | Bias (%) | Bias reduction (%) | t | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Treated | Control | |||||
|
| ||||||
| Age | 63.05 | 62.93 | 1.30 | 92.60 | 0.59 | 0.55 |
| Gender | 0.53 | 0.54 | −1.10 | 37.70 | −0.52 | 0.60 |
| Rural area | 0.91 | 0.91 | −1.10 | 98.30 | −0.69 | 0.49 |
| Education | 0.23 | 0.22 | 1.20 | 96.80 | 0.61 | 0.54 |
| Household economic level | −0.95 | −0.95 | 0.00 | 99.90 | −0.02 | 0.98 |
| Marital status | 0.83 | 0.83 | −1.10 | −187.80 | −0.52 | 0.60 |
| Retire status | 0.05 | 0.05 | −0.20 | 99.60 | −0.10 | 0.92 |
| Smokers | 0.45 | 0.46 | −1.60 | 77.90 | −0.74 | 0.46 |
| Drinkers | 0.25 | 0.24 | 2.00 | 21.30 | 0.93 | 0.35 |
| Sleep time | 0.54 | 0.54 | 0.00 | 98.80 | 0.02 | 0.99 |
| Social activity participation | 0.46 | 0.47 | −4.70 | 82.10 | −1.71 | 0.09 |
| BMI | 23.40 | 23.49 | −2.30 | 86.10 | −1.05 | 0.29 |
| Diabetes | 0.06 | 0.06 | −1.50 | 83.70 | −0.73 | 0.47 |
| Lung diseases | 0.15 | 0.15 | 0.70 | 94.10 | 0.30 | 0.76 |
| CVDs | 0.42 | 0.43 | −0.70 | 32.20 | −0.31 | 0.76 |
| Disability | 0.14 | 0.14 | 0.20 | 98.00 | 0.09 | 0.93 |
| Self-reported health | 0.88 | 0.91 | −3.80 | 78.80 | 1.04 | 0.30 |
|
| ||||||
| Sample | Pseudo R2 | LR chi2 | p > chi2 | Mean Bias | R | Var (%) |
|
| ||||||
| Unmatched | 0.147 | 1899.82 | 0.00 | 20.00 | 0.38* | 67 |
| Matched | 0.001 | 15.75 | 0.54 | 1.40 | 1.14 | 0 |
Notes: BMI, Body Mass Index; CVDs, cardiovascular diseases.
3.3. Effect of HAP on depression
Table 3 describes the results indicating the effects of household solid fuel use on depression using unmatched and matched data. Estimated coefficients of CES-D scores and OR of depression risk with clustered standard errors at the community level are reported. Two measures of independents including current solid fuel users and the duration of solid fuel use were examined. Overall, the unmatched and matched results were statistically significant at the 0.05 level, with slightly small matched results. Using the matched data after control on the potential confounders, current solid fuel users had a 0.59 (95% CI: 0.31, 0.89) higher CES-D score and an OR of 1.26 (95% CI: 1.14, 1.41) suffering from depression compared with current users of clean fuel. The adverse effects of sustained use of solid fuel on depression became increasingly evident. Compared with participants who use clean fuel all the time, individuals exposed to solid fuel combustion for 5 years or more had a significantly higher CES-D score of 1.07 (95% CI: 0.65, 1.5) and an OR of 1.55 (95% CI: 1.29, 1.86) and risk of depression. A long duration of solid fuel use indicated a high effect for CES-D scores and depression episode risk.
Table 3.
Effect of HAP on depression using unmatched and matched data
| Outcomes | Unmatched Model | Matched Model | ||
|---|---|---|---|---|
|
|
|
|||
| β/ OR (95% CI) | P | β/ OR (95% CI) | P | |
|
| ||||
| CES-D | ||||
| current solid fuel users | 0.71 (0.4, 1.01) | <0.001 | 0.59 (0.31, 0.89) | 0.002 |
| duration of solid fuel use | ||||
| 1–4 yrs. | 0.62 (0.32, 0.92) | <0.001 | 0.53 (0.23, 0.81) | <0.001 |
| >5 yrs. | 1.15 (0.76, 1.54) | <0.001 | 0.99 (0.62, 1.36) | <0.001 |
|
| ||||
| Depression (cutoff=10) | ||||
| current solid fuel users | 1.29 (1.16, 1.44) | <0.001 | 1.26 (1.14, 1.41) | <0.001 |
| duration of solid fuel use | ||||
| 1–4 yrs. | 1.29 (1.13, 1.48) | <0.001 | 1.27 (1.13, 1.46) | 0.004 |
| >5 yrs. | 1.55 (1.34, 1.8) | <0.001 | 1.49 (1.30, 1.73) | <0.001 |
|
| ||||
| Depression (cutoff=12) | ||||
| current solid fuel users | 1.32 (1.17, 1.48) | <0.001 | 1.28 (1.15, 1.44) | <0.001 |
| duration of solid fuel use | ||||
| 1–4 yrs. | 1.3 (1.13, 1.5) | <0.001 | 1.28 (1.12, 1.46) | 0.005 |
| >5 yrs. | 1.57 (1.34, 1.84) | <0.001 | 1.50 (1.29, 1.75) | <0.001 |
Notes: CES-D, Center for Epidemiological Studies Depression Scale.
All the models were regressed separately and adjusted by covariates as aforementioned using the matched data.
95% CI was reported based on standard errors clustered at the community level.
Heterogeneous effects of HAP on depression by age, gender, BMI, education, household economic level, and chronic disease status were discussed. Tables 4, 5, and 6 show the results of subgroups analysis, with almost all estimates positively statistically significant for all separate groups. The hazardous effects of HAP on depression were significant for almost all the different populations. For the subgroups of age, gender and BMI, table 4 suggests that groups of age ≥65 years old, female, and BMI ≥25 had slightly higher CES-D scores and higher risk of depression episode compared with their counterparts. However, only part of the estimates was statistically significant at the 0.05 level. We then conducted stratified analysis of education and household economic levels, which may be associated with the assignment of fuel types of participants. Table 5 reports the results. Generally, HAP has large effects on depression outcomes in participants with low educational attainment and low household economic levels. Only the modification effect of education was statistically significant for the association between current HAP exposure and CES-D scores. When stratified by underlying chronic diseases, high effects were observed in participants suffering from diabetes, chronic lung disease, and CVDs. However, we did not find any significant effect modification for these groups except for the modified effect of diabetes and chronic lung diseases on the associations between solid fuel use duration of 5 year or more and CES-D scores.
Table 4.
Effect of HAP on depression stratified by gender, age and BMI
| Outcomes | Age | Gender | BMI | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| >=65 yrs. | <65 yrs. | p a | Female | Male | p a | BMI>=25 | BMI<25 | p a | |
|
| |||||||||
| CES-D | |||||||||
| current solid fuel users | 0.54 (0.16, 0.92) | 0.43 (−0.09, 0.95) | 0.04 | 0.61 (0.2, 1.02) | 0.37 (0.01, 0.75) | 0.01 | 0.72 (0.33, 1.11) | 0.25 (−0.28, 0.77) | 0.04 |
| duration more than 5yrs. | 0.73 (0.25, 1.2) | 0.55 (0.17, 0.93) | 0.55 | 0.81 (0.4, 1.21) | 0.37 (−0.02, 0.76) | 0.01 | 0.63 (0.25, 1.01) | 0.59 (0.02, 1.15) | 0.01 |
|
| |||||||||
| Depression (cutoff=10) | |||||||||
| current solid fuel users | 1.29 (1.11, 1.49) | 1.17 (0.98, 1.4) | 0.09 | 1.3 (1.12, 1.51) | 1.18 (1, 1.41) | 0.03 | 1.28 (1.1, 1.49) | 1.22 (0.99, 1.5) | 0.09 |
| duration more than 5yrs. | 1.26 (1.07, 1.49) | 1.25 (1.09, 1.44) | 0.89 | 1.27 (1.09, 1.46) | 1.25 (1.06, 1.47) | 0.51 | 1.28 (1.03, 1.57) | 1.24 (1.08, 1.43) | 0.51 |
|
| |||||||||
| Depression (cutoff=12) | |||||||||
| current solid fuel users | 1.31 (1.11, 1.53) | 1.19 (0.98, 1.45) | 0.04 | 1.28 (1.1, 1.49) | 1.24 (1.02, 1.51) | 0.67 | 1.31 (1.12, 1.53) | 1.19 (0.94, 1.5) | 0.13 |
| duration more than 5yrs. | 1.27 (1.1, 1.47) | 1.24 (1.04, 1.48) | 0.95 | 1.28 (1.06, 1.55) | 1.25 (1.09, 1.43) | 0.95 | 1.22 (1.01, 1.49) | 1.17 (0.93, 1.48) | 0.46 |
Notes: CES-D, Center for Epidemiological Studies Depression Scale; BMI, Body Mass Index.
p-value indicating the statistical significance of the modification effects.
All the models were regressed separately and adjusted by covariates as aforementioned using the matched data.
95% CI was reported based on standard errors clustered at the community level.
Table 5.
Effect of solid fuel use on depression stratified by education and household economic level
| Outcomes | Education | Household economic Level | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Primary school and below | High school and above | P a | Low | High | P a | |
|
|
|
|
||||
| CES-D | ||||||
| current solid fuel users | 0.68 (0.3, 1.05) | 0.27 (−0.27, 0.82) | 0.03 | 0.67 (0.2, 1.13) | 0.54 (0.11, 0.96) | 0.82 |
| duration more than 5yrs.chul | 0.57 (0.18, 0.96) | 0.51 (−0.1, 1.13) | 0.28 | 0.7 (0.09, 1.3) | 0.55 (0.15, 0.96) | 0.79 |
|
|
|
|
||||
| Depression (cutoff=10) | ||||||
| current solid fuel users | 1.26 (1.15, 1.37) | 1.25 (1.09, 1.43) | 0.58 | 1.31 (1.06, 1.62) | 1.23 (1.06, 1.44) | 0.77 |
| duration more than 5yrs. | 1.36 (1.02, 1.8) | 1.25 (1.09, 1.43) | 0.96 | 1.4 (1.1, 1.78) | 1.24 (1.07, 1.44) | 0.48 |
|
|
|
|
||||
| Depression (cutoff=12) | ||||||
| current solid fuel users | 1.33 (1, 1.77) | 1.26 (1.1, 1.45) | 0.94 | 1.4 (1.12, 1.75) | 1.24 (1.05, 1.46) | 0.54 |
| duration of solid fuel use | 1.35 (1.01, 1.81) | 1.24 (1.08, 1.42) | 0.96 | 1.31 (1.02, 1.68) | 1.26 (1.07, 1.48) | 0.91 |
Notes:
p-value indicating the statistical significance of the modification effects.
All the models were regressed separately and adjusted by covariates as aforementioned using the matched data.
95% CI was reported based on standard errors clustered at the community level.
Table 6.
Effect of solid fuel use on depression stratified by chronic diseases
| Outcomes | Diabetes | Lung Diseases | CVDs | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| diabetes=1 | diabetes=0 | P a | lung diseases=1 | lung diseases=0 | P a | CVDs=1 | CVDs=0 | P a | |
|
|
|
|
|
||||||
| CES-D | |||||||||
| current solid fuel users | 0.8 (−0.37, 1.96) | 0.48 (0.17, 0.8) | 0.07 | 0.86 (0.08, 1.64) | 0.44 (0.12, 0.76) | 0.13 | 0.58 (0.2, 0.97) | 0.4 (−0.07, 0.86) | 0.08 |
| duration more than 5yrs. | 0.88 (−0.28, 2.03) | 0.58 (0.27, 0.9) | 0.03 | 1.17 (0.36, 1.98) | 0.51 (0.19, 0.83) | 0.01 | 0.59 (0.12, 1.06) | 0.62 (0.23, 1.02) | 0.85 |
|
| |||||||||
| Depression (cutoff=10) | |||||||||
| current solid fuel users | 1.49 (0.96, 2.31) | 1.23 (1.08, 1.39) | 0.62 | 1.32 (1, 1.75) | 1.23 (1.09, 1.39) | 0.74 | 1.3 (1.11, 1.51) | 1.18 (0.99, 1.42) | 0.50 |
| duration more than 5yrs. | 1.58 (1.01, 2.46) | 1.23 (1.1, 1.39) | 0.43 | 1.36 (1.01, 1.82) | 1.24 (1.1, 1.4) | 0.76 | 1.29 (1.12, 1.49) | 1.21 (1.02, 1.45) | 0.72 |
|
| |||||||||
| Depression (cutoff=12) | |||||||||
| current solid fuel users | 1.53 (0.99, 2.38) | 1.24 (1.09, 1.41) | 0.19 | 1.49 (1.1, 2.02) | 1.22 (1.07, 1.4) | 0.33 | 1.28 (1.08, 1.5) | 1.24 (1.04, 1.49) | 0.76 |
| duration more than 5yrs. | 1.76 (1.12, 2.78) | 1.23 (1.09, 1.39) | 0.08 | 1.39 (1.03, 1.87) | 1.24 (1.09, 1.4) | 0.22 | 1.27 (1.1, 1.48) | 1.24 (1.04, 1.48) | 0.81 |
Notes: CES-D, Center for Epidemiological Studies Depression Scale; CVDs, cardiovascular diseases.
p-value indicating the statistical significance of the modification effects.
All the models were regressed separately and adjusted by covariates as aforementioned using the matched data.
95% CI was reported based on standard errors clustered at the community level.
Results of sensitivity analyses were all reasonably consistent with our primary models. The last panels of tables 3, 4, and 5 present the results of household solid fuel use on the risk of depression using a cutoff of 12. Overall, a slight difference was observed in using a cutoff of 10 to define a depression episode, suggesting robust estimates of our models. These results remained largely consistent when we 1) excluded participants taking antidepressants, tranquilizers, or sleeping pills or receiving psychiatric or psychological treatment; and 2) employed different matching methods in the PSM (data are not shown but are available upon request).
4. Discussion
By using a matching method, household solid fuel use was found to have a significant effect on depression among the middle-aged and older population in China. This effect remained significant even after controlling for confounders like demographics, socioeconomic status, and health-related covariates. To our knowledge, this study is the first to employ a nationally representative data and matching technology to explore the relationship between HAP from solid fuel combustion and depression in China. Our results can lend support for the role of HAP in neurobehavioral disorders, thereby providing valuable insights for policy and promotional program designs. These policies and programs can improve mental health and control the disease burden of air pollution in China and worldwide.
We found hazardous effects of HAP on depressive symptoms and the risk of experiencing a depression episode among the middle-aged and older population in China. We cannot directly compare our estimates with prior studies because no existing studies have evaluated the effects of household solid fuel use on depression. A similar study found that premenopausal women who cooked using biomass had a high prevalence of depression (OR=1.67, 95% CI: 1.18–2.95) in India (Banerjee et al. 2012); where the values were larger than our estimates (1.26, 95% CI: 1.14, 1.41). Apart from the independent variables and estimate methods, other potential explanations for this difference may include different sample sizes, outcome measures, and population characteristics. For example, we used a large nationally representative dataset with a sample size of more than 9,000, whereas the other study focused on premenopausal women and had a sample size of 952. Additionally, our findings conform with prior epidemiological studies on the associations of ambient air pollution and depression, which have found strong depressive symptoms, high risk of depression disorders, and increased hospitalization for depression with increasing ambient air pollutant concentrations. Similarly, our results were consistent with HAP research on physical health effects, where HAP from solid fuel use was linked with high blood pressure (Baumgartner et al. 2011; Yan et al. 2016) and increased risk of mortality from CVDs (Yu et al. 2018), respiratory diseases (Bates Michael et al. 2013), lung cancer (Hosgood et al. 2010), and cataracts (Ravilla Thulasiraj et al. 2016). This finding suggests that HAP not only has adverse effects on physical health but also on mental health.
Our second important finding was that long exposure to HAP can lead to increased adverse impact on depression, which provided further evidence that HAP exposure poses a significant threat to mental health. This point was also similar to prior research on HAP and physical health, which provided evidence that long exposure was associated with high blood pressure and increased risk of hypertension, stroke, and diabetes (Lee et al. 2012; Yan et al. 2016).
Our subgroup analysis suggested that the associations between HAP and depression were significant in almost all different subgroups categorized by age, gender, BMI, education, household economic levels, and chronic diseases (including diabetes, chronic lung diseases, and CVDs). This finding confirmed our main results. However, no consistent evidence was found for the effect modification. In general, women, individuals aged 65 years and above, and individuals with obesity were reasonably more sensitive to HAP. This result is similar to prior studies, which suggested that ambient air pollution had major effects on depression among women and older people (Szyszkowicz et al. 2016; Zhang et al. 2017). However, different results were reported by Pun et al. (2017), where no significant effect of air pollution on depression and modification effect were found among all groups. Our results also suggested that individuals with low educational attainment and low household economic levels may respond strongly to HAP, which is similar with the results found by Zhang et al. (2017) and Pun et al. (2017). One reason for this finding may be that individuals with high educational attainment or high economic status can gain more knowledge on the adverse health effects of air pollution. Hence, they are able to take preventive actions, such as installing home air purifiers to reduce the harmful effects of pollutants. For the subgroup analysis of chronic diseases, prior evidence on the heterogeneity in effects of ambient pollution on depression has not been conclusive. Significantly strong effects were observed from individuals suffering from chronic diseases (Wang and Yang 2018; Zhang et al. 2017), CVDs (Wang et al. 2018), diabetes (Cho et al. 2014), stroke, heart failure, emphysema, or asthma (Cho et al. 2014; Pun et al. 2017). However, no significant effect modification was found for hypertension or diabetes in the study of Pun et al. (2017), nor for diabetes or CVDs in the study of Kim et al. (2016). In our study, we found moderately high effects in participants diagnosed with diabetes, chronic lung disease, and CVDs. However, only some of the interaction estimations were statistically significant. Differences in sample sizes, demographic characteristics, outcome measures, and empirical strategies used may have induced the heterogeneity in the results and made the direct comparison difficult. For reliable results regarding the effect modification in identifying vulnerable populations, more research with larger samples and experimental designs are needed in the future.
The underlying mechanisms for the effects of air pollution, especially HAP, on depression are not yet clearly understood. One hypothesized biological explanation is that mental disorders, including depression, occur as a result of increased oxidative stress, cerebrovascular damage, neurodegeneration, or neuroinflammation caused by air pollutants (Block and Calderón-Garcidueñas 2009; MohanKumar et al. 2008; Sirivelu et al. 2006). Another possible pathway is that of promotion or aggravation of chronic diseases (Pun et al. 2017), in which apart from biological effects, air pollution may also affect mental health though health-related behaviors, such as preventing participating in outdoor physical and social activities (Bresnahan et al. 1997; Goodwin 2003; Li et al. 2015; Sass et al. 2017), which are effective ways to reduce the risk of mental disorders (George et al. 2018). Additionally, besides generating substantial emissions of health-damaging pollutants, solid fuels use may also impact mental health through other ways, e.g. time allocation of the users, which can also significantly affect individuals’ health behaviors like social activity participation and physical exercise, and so on. For example, solid fuel users may take longer time for fuel collection and cooking (Bonjour et al. 2013; Rehfuess et al. 2006), reducing their time to participate other activities. Ideally, this assumption can be verified to include a control variable representing cooking or fuel use time into our models. However, this information is not available in CHARLS. Further studies are necessary to delineate the toxicological mechanisms and causal relationships between air pollution and mental disorders such as depression.
In the present study, we used a large and nationally representative dataset to evaluate the effect of HAP from solid fuel use on depression, allowing adequate power to detect modest but meaningful effects. We also used a matching strategy to control selection bias in fuel choice, which was neglected in prior HAP research. Prior studies provide limited evidence on the effectiveness of improved stoves in reducing HAP exposure. Thus, switching to clean fuels may be the only feasible way to reduce HAP from household energy combustion. Our findings shed light on the potential mental health benefits of fuel switching and provides important information to policy makers.
Despite its strengths, our study’s findings have limitations. First, we used proxy variables for HAP and could not use the personal exposure concentration of HAP because obtaining such information for a large population-based research is difficult. Second, our proxy variables for HAP included only household fuel types for cooking because household fuel information for heating was not available in wave 2015 of CHARLS. Household fuel information for heating is important for HAP research. Hence, future studies are encouraged to incorporate this information. Third, our findings may not be generalized to a young age group or population in other countries, because we focused on the middle-aged and older population in China. A different research background, including different study populations, culture, or sample size, and so on, may lead to different results. Although we included a series of demographic, socioeconomic, health–behavioral, and other covariates to control possible confounding, unobservable factors associated with depression (e.g., second-hand smoke exposure) were ignored.
5. Conclusions
Depression is a common and costly mental disorder worldwide. Using matching data, we first provided evidence of significant associations between HAP from solid fuel use and depression among a representative sample of middle-aged and older population in China. Results show that long usage of solid fuel had major impacts on depression, considering the different groups classified by gender, age, BMI, and chronic disease presence. Women, individuals aged 65 years old and above, individuals identified as obese, participants with low educational attainment and low household economic levels, and participants suffering from chronic diseases were moderately susceptible to depression. Our findings suggest a need to strengthen public health efforts, such as controlling the social, health, and economic costs of depression by taking the physical environment, including HAP exposure, into account. Future studies on specific toxicological mechanism and with experimental and longitudinal designs are needed to further understand how HAP from solid fuel combustion affects depression and mental health.
Highlights.
One of the first study to examine the association between household indoor air pollution from solid fuel use and depression among the middle-aged and older persons in China;
A large nationally representative dataset was used in the study, allowing adequate power to detect modest but meaningful effects;
We employed a matching strategy to remove selection bias in fuel choice, which was neglected in prior household air pollution research.
Heterogeneous effects for vulnerable populations were estimated.
Acknowledgments
Financial supports from National Natura Science Foundation of China (Grant Nos. 71572013, 71872013, and 71432002), Special Fund for Joint Development Program of Beijing Municipal Commission of Education, the James Tobin Research Fund at Yale Economics Department, Yale Macmillan Center faculty research award (2014-2016; 2017-2019), the U.S. PEPPER Center Scholar Award (P30AG021342), and two NIH/NIA grants (K01AG053408; R03AG048920) are acknowledged. The financial support provided by China Scholarship Council (CSC) during a visit of Yan Liu to Yale University is acknowledged. The views expressed herein and any remaining errors are the authors’ and do not represent any official agency. None of the authors have potential conflicts of interests that could bias this work.
APPENDIX
Appendix
Appendix figure 1.
Common range of propensity scores
Appendix figure 2.
Density function of propensity scores
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
7. Reference
- Andresen EM, Malmgren JA, Carter WB, et al. 1994. Screening for Depression in Well Older Adults - Evaluation of a Short-Form of the Ces-D. American Journal of Preventive Medicine 10:77–84. [PubMed] [Google Scholar]
- Austin PC. 2013. The Performance of Different Propensity Score Methods for Estimating Marginal Hazard Ratios. Statistics in medicine 32:2837–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee M, Siddique S, Dutta A, et al. 2012. Cooking with Biomass Increases the Risk of Depression in Pre-Menopausal Women in India. Social Science & Medicine 75:565–572. [DOI] [PubMed] [Google Scholar]
- Bates Michael N, Chandyo Ram K, Valentiner-Branth P, et al. 2013. Acute Lower Respiratory Infection in Childhood and Household Fuel Use in Bhaktapur, Nepal. Environmental health perspectives 121:637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner J, Schauer JJ, Ezzati M, et al. 2011. Indoor Air Pollution and Blood Pressure in Adult Women Living in Rural China. Environmental health perspectives 119:1390–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block ML, Calderón-Garcidueñas L. 2009. Air Pollution: Mechanisms of Neuroinflammation and Cns Disease. Trends in Neurosciences 32:506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonjour S, Adair-Rohani H, Wolf J, et al. 2013. Solid Fuel Use for Household Cooking: Country and Regional Estimates for 1980–2010. Environmental health perspectives 121:784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresnahan BW, Dickie M, Gerking S. 1997. Averting Behavior and Urban Air Pollution. Land Economics 73:340–357. [Google Scholar]
- Charlson FJ, Baxter AJ, Cheng HG. 2016. The Burden of Mental, Neurological, and Substance Use Disorders in China and India: A Systematic Analysis of Community Representative Epidemiological Studies. Lancet 388:1984–1984. [DOI] [PubMed] [Google Scholar]
- Cheng HG, Chen SN, McBride O, et al. 2016. Prospective Relationship of Depressive Symptoms, Drinking, and Tobacco Smoking among Middle-Aged and Elderly Community-Dwelling Adults: Results from the China Health and Retirement Longitudinal Study (Charls). Journal of Affective Disorders 195:136–143. [DOI] [PubMed] [Google Scholar]
- Cheng ST, Chan ACM. 2005. The Center for Epidemiologic Studies Depression Scale in Older Chinese: Thresholds for Long and Short Forms. International Journal of Geriatric Psychiatry 20:465–470. [DOI] [PubMed] [Google Scholar]
- Cho J, Choi YJ, Suh M, et al. 2014. Air Pollution as a Risk Factor for Depressive Episode in Patients with Cardiovascular Disease, Diabetes Mellitus, or Asthma. Journal of Affective Disorders 157:45–51. [DOI] [PubMed] [Google Scholar]
- Clark Maggie L, Peel Jennifer L, Balakrishnan K, et al. 2013. Health and Household Air Pollution from Solid Fuel Use: The Need for Improved Exposure Assessment. Environmental health perspectives 121:1120–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. 2003. Risk Factors for Depression among Elderly Community Subjects: A Systematic Review and Meta-Analysis. American Journal of Psychiatry 160:1147–1156. [DOI] [PubMed] [Google Scholar]
- Ekman M, Granström O, Omérov S, et al. 2013. The Societal Cost of Depression: Evidence from 10,000 Swedish Patients in Psychiatric Care. Journal of Affective Disorders 150:790–797. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Agbeyaka S, LaFond DM, et al. 2016. Flourishing after Depression: Factors Associated with Achieving Complete Mental Health among Those with a History of Depression. Psychiatry Research 242:111–120. [DOI] [PubMed] [Google Scholar]
- Garrido MM, Kelley AS, Paris J, et al. 2014. Methods for Constructing and Assessing Propensity Scores. Health services research 49:1701–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George LK, Blazer DG, Hughes DC, et al. 2018. Social Support and the Outcome of Major Depression. British Journal of Psychiatry 154:478–485. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Fisher LJ, Dal Grande E, et al. 2004. Subsyndromal Depression: Prevalence,Use of Health Services and Quality of Life in an Australianpopulation. Social Psychiatry and Psychiatric Epidemiology 39:293–298. [DOI] [PubMed] [Google Scholar]
- Goodwin RD. 2003. Association between Physical Activity and Mental Disorders among Adults in the United States. Preventive Medicine 36:698–703. [DOI] [PubMed] [Google Scholar]
- Guan WJ, Zheng XY, Chung KF, et al. 2016. Impact of Air Pollution on the Burden of Chronic Respiratory Diseases in China: Time for Urgent Action. Lancet 388:1939–1951. [DOI] [PubMed] [Google Scholar]
- Guo J, Guan LD, Fang LM, et al. 2017. Depression among Chinese Older Adults: A Perspective from Hukou and Health Inequities. Journal of Affective Disorders 223:115–120. [DOI] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, et al. 2007. Matching as Nonparametric Preprocessing for Reducing Model Dependence in Parametric Causal Inference. Political Analysis 15:199–236. [Google Scholar]
- Hosgood HD 3rd, Boffetta P, Greenland S, et al. 2010. In-Home Coal and Wood Use and Lung Cancer Risk: A Pooled Analysis of the International Lung Cancer Consortium. Environmental health perspectives 118:1743–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hystad P, Duong M, Brauer M, et al. 2019. Health Effects of Household Solid Fuel Use: Findings from 11 Countries within the Prospective Urban and Rural Epidemiology Study. Environmental health perspectives 127:057003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeuland M, Pattanayak SK, Bluffstone R. 2015. The Economics of Household Air Pollution. Annual Review of Resource Economics 7:81–108. [Google Scholar]
- Juhn YJ, Qin R, Urm S, et al. 2010. The Influence of Neighborhood Environment on the Incidence of Childhood Asthma: A Propensity Score Approach. Journal of Allergy and Clinical Immunology 125:838–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Bromet EJ. 2013. The Epidemiology of Depression across Cultures. Annual Review of Public Health 34:119–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K-N, Lim Y-H, Bae Hyun J, et al. 2016. Long-Term Fine Particulate Matter Exposure and Major Depressive Disorder in a Community-Based Urban Cohort. Environmental health perspectives 124:1547–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kioumourtzoglou M-A, Power MC, Hart JE, et al. 2017. The Association between Air Pollution and Onset of Depression among Middle-Aged and Older Women. American journal of epidemiology 185:801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krefis AC, Schwarz NG, Nkrumah B, et al. 2010. Principal Component Analysis of Socioeconomic Factors and Their Association with Malaria in Children from the Ashanti Region, Ghana. Malaria journal 9:201–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M-S, Hang J-q Zhang F-y, et al. 2012. In-Home Solid Fuel Use and Cardiovascular Disease: A Cross-Sectional Analysis of the Shanghai Putuo Study. Environmental health : a global access science source 11:18–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li FZ, Liu Y, Lü JJ, et al. 2015. Ambient Air Pollution in China Poses a Multifaceted Health Threat to Outdoor Physical Activity. Journal of Epidemiology and Community Health 69:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Qin C, Lv J, et al. 2019. Solid Fuel Use and Incident Copd in Chinese Adults: Findings from the China Kadoorie Biobank. Environmental health perspectives 127:057008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim YH, Kim H, Kim JH, et al. 2012. Air Pollution and Symptoms of Depression in Elderly Adults. Environmental health perspectives 120:1023–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MohanKumar SMJ, Campbell A, Block M, et al. 2008. Particulate Matter, Oxidative Stress and Neurotoxicity. NeuroToxicology 29:479–488. [DOI] [PubMed] [Google Scholar]
- Neupane M, Basnyat B, Fischer R, et al. 2015. Sustained Use of Biogas Fuel and Blood Pressure among Women in Rural Nepal. Environmental Research 136:343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES. 2008. Basic Concepts of Depression. Dialogues in clinical neuroscience 10:279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power MC, Weisskopf MG, Alexeeff SE, et al. 2011. Traffic-Related Air Pollution and Cognitive Function in a Cohort of Older Men. Environmental health perspectives 119:682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pun VC, Manjourides J, Suh H. 2017. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the Nshap Study. Environmental health perspectives 125:342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravilla Thulasiraj D, Gupta S, Ravindran Ravilla D, et al. 2016. Use of Cooking Fuels and Cataract in a Population-Based Study: The India Eye Disease Study. Environmental health perspectives 124:1857–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehfuess E, Mehta S, Prüss-Üstün A. 2006. Assessing Household Solid Fuel Use: Multiple Implications for the Millennium Development Goals. Environmental health perspectives 114:373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitzes DC, Mutran EJ, Fernandez ME. 1996. Does Retirement Hurt Weil-Being? Factors Influencing Self-Esteem and Depression among Retires and Workers1. The Gerontologist 36:649–656. [DOI] [PubMed] [Google Scholar]
- Ruo B, Rumsfeld JS, Hlatky MA, et al. 2003. Depressive Symptoms and Health-Related Quality of Life: The Heart and Soul Study. JAMA 290:215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sass V, Kravitz-Wirtz N, Karceski SM, et al. 2017. The Effects of Air Pollution on Individual Psychological Distress. Health & Place 48:72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirivelu MP, MohanKumar SMJ, Wagner JG, et al. 2006. Activation of the Stress Axis and Neurochemical Alterations in Specific Brain Areas by Concentrated Ambient Particle Exposure with Concomitant Allergic Airway Disease. Environmental health perspectives 114:870–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KR, Frumkin H, Balakrishnan K, et al. 2013. Energy and Human Health. Annual Review of Public Health 34:159–188. [DOI] [PubMed] [Google Scholar]
- Stuart EA, Green KM. 2008. Using Full Matching to Estimate Causal Effects in Nonexperimental Studies: Examining the Relationship between Adolescent Marijuana Use and Adult Outcomes. Developmental Psychology 44:395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyszkowicz M, Kousha T, Kingsbury M, et al. 2016. Air Pollution and Emergency Department Visits for Depression: A Multicity Case-Crossover Study. Environmental Health Insights 10:EHI.S40493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vert C, Sanchez-Benavides G, Martinez D, et al. 2017. Effect of Long-Term Exposure to Air Pollution on Anxiety and Depression in Adults: A Cross-Sectional Study. International Journal of Hygiene and Environmental Health 220:1074–1080. [DOI] [PubMed] [Google Scholar]
- Vyas S, Kumaranayake L. 2006. Constructing Socio-Economic Status Indices: How to Use Principal Components Analysis. Health Policy and Planning 21:459–468. [DOI] [PubMed] [Google Scholar]
- Wang F, Liu H, Li H, et al. 2018. Ambient Concentrations of Particulate Matter and Hospitalization for Depression in 26 Chinese Cities: A Case-Crossover Study. Environment International 114:115–122. [DOI] [PubMed] [Google Scholar]
- Wang Q, Yang ZM. 2018. Does Chronic Disease Influence Susceptibility to the Effects of Air Pollution on Depressive Symptoms in China? International journal of mental health systems 12:33–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Eliot Melissa N, Koutrakis P, et al. 2014. Ambient Air Pollution and Depressive Symptoms in Older Adults: Results from the Mobilize Boston Study. Environmental health perspectives 122:553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. 2019. Household Air Pollution: Health Impacts. Available: https://www.who.int/airpollution/household/health-impacts/en/.
- Yan ZJ, Liu Y, Yin QJ, et al. 2016. Impact of Household Solid Fuel Use on Blood Pressure and Hypertension among Adults in China. Air Quality, Atmosphere & Health 9:931–940. [Google Scholar]
- Yu K, Qiu G, Chan K, et al. 2018. Association of Solid Fuel Use with Risk of Cardiovascular and All-Cause Mortality in Rural China. JAMA 319:1351–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Zhang XB, Chen X. 2017. Happiness in the Air: How Does a Dirty Sky Affect Mental Health and Subjective Well-Being? Journal of Environmental Economics and Management 85:81–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao YH, Hu YS, Smith JP, et al. 2014. Cohort Profile: The China Health and Retirement Longitudinal Study (Charls). International Journal of Epidemiology 43:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijlema WL, Wolf K, Emeny R, et al. 2016. The Association of Air Pollution and Depressed Mood in 70,928 Individuals from Four European Cohorts. International Journal of Hygiene and Environmental Health 219:212–219. [DOI] [PubMed] [Google Scholar]