Abstract
Recurrent positivity in a patient with COVID-19 may be due to various reasons, not necessarily reinfection. There is concern about the occurrence frequency of reinfection. Five databases and a preprint/preprint repository were searched. All case reports, case series, and observational studies were included. Bias was assessed for each study with the Newcastle-Ottawa Scale tool and reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA-2020). After eligibility, 77 studies were included for qualitative synthesis (52 case reports, 21 case series, and four case-controls; 1131 patients included). Of these, 16 studies described a second contact with the SARS-CoV-2 positive case, five studies described healthcare profession-related infection, ten studies described that the source of reinfection was likely to be from the community, one study described travel-related infection, nine studies described vulnerability-related infection due to comorbidity. The mean number of days from discharge or negative test to reinfection ranged from 23.3 to 57.6 days across the different included studies. The risk of bias for all case report/series studies was moderate/high. For observational studies, the risk of bias was low. Reinfection of patients with COVID-19 occurs between the first and second month after the first infection, but beyond, and 90 days have been proposed as a point to begin to consider it. The main factor for reinfection is contact with COVID-19 positive cases.
Keywords: COVID-19, pandemic, recurrence, reinfection, SARS-CoV-2
Introduction
Approximately 18 months ago, the world witnessed the beginning of one of the worst pandemics that contemporary humanity has experienced; it is the Coronavirus Disease 2019 (COVID-19), which began as an outbreak of atypical pneumonia at the end of December 2019 in the city of Wuhan, China [1]. After a few days, it was confirmed to be a new coronavirus, which was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [2].
A few weeks after the outbreak, cases were reported outside China's borders, which is why the World Health Organization (WHO) declared this new respiratory disease a global health emergency [3]. On March 11, 2020, it officially declared a pandemic [4]. After this declaration, various strategies were implemented in the different countries of the world to stop the spread of the disease, such as closing borders, quarantining regions or entire countries, closing companies, schools, and universities; however, despite all this, cases increased, and mortality was on the rise.
Several countries expected to obtain herd immunity due to the increase in cases; however, this was not achieved [5]. In the meantime, different institutions and companies around the world began a race in the development of vaccines as another measure to stop the spread of COVID-19; some were able to successfully pass phase 3 with efficacies above 50% as the cut-off point established by the CDC, and commercialization began [6]. Many countries have started vaccinations, protecting first their health professionals, following with vulnerable populations such as the elderly or people with chronic comorbidities; although in most countries, this is very slow due to accessibility issues.
Regarding the possibility of reinfection with SARS-CoV-2 and developing COVID-19 disease again, there are worrying reports of cases of reinfection, i.e., people who have tested positive again in molecular or antigenic tests for the virus up to seven months after discharge, ranging from mild to severe cases [7]. It should be noted that reinfection or relapse of COVID-19 disease is not a common entity and should be studied in greater depth [8]; these reinfected patients should be followed up for a more extended period, and the clinical, epidemiological profile should be studied, as well as genetic sequencing of the virus to determine the presence of any variant [9,10]. The objective of this systematic review was to evaluate the clinical and epidemiological characteristics in patients with COVID-19 reinfection.
Methods
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020, Supplement table) [11]. The PROSPERO registry is CRD42021231573. The study evaluated the clinical and epidemiological features in patients with reinfection of COVID-19.
Data sources
We searched PubMed, Scopus, Web of Science, Ovid-Medline, Embase, and a preprints/preproofs repository (“https://www.medrxiv.org”). Some studies were also identified through a manual Google search. We performed a search strategy that can be found in the Supplementary table. No restriction was applied to the language. Searches only included documents published from inception to May 19, 2022. Primary search terms were “reinfection”, “reinfection drug”, “COVID-19".
Eligibility criteria
We included all the case report, case series, and observational studies. Systematic reviews, narrative reviews, conference proceedings, editorials, and letters to the editor without original data were excluded. The population will be patients with mild, moderate or severe COVID-19, independently of the associated comorbidities before the first infection. The main risk factor identified among the studies is reinfection by COVID-19, or recurrence regardless of the time after the first infection.
Outcomes
The outcomes were the severity of the second infection of COVID-19 (reinfection) or recurrence and the number of days until reinfection by COVID-19.
Study selection
According to the inclusion and exclusion criteria, two authors (FE, LP) independently screened search results by title and abstract using the web program rayyan (rayyan-qcri.org). Relevant studies were selected and searched by full text for the next phase of assessment. Discrepancies were consulted with another author (JB), and a consensus was reached. The selection of articles in each stage of the review process was made using Microsoft Excel®.
Data extraction
Two authors (CJ, MH) independently extracted the data using pre-piloted Excel spreadsheets. Again, discrepancies were consulted with another author (JB). The data extracted from each study were: author, year, country, type of research, number of patients, age, gender, type of patients (pre-infection and post-infection comorbidities), risk factors (exposure), the severity of first infection o symptoms during reinfection.
Risk of bias assessment
Two authors evaluated the risk of bias independently. Cohorts and case-control were assessed with the Newcastle–Ottawa scale. We used the modified Newcastle–Ottawa scale (NOS) tool [12]. For case report/series, the studies were evaluated with methodological quality assessment tools and synthesis of case series and case reports [13]. Again, discrepancies were consulted with another author (JB).
Ethical considerations
This is a systematic review of published and available information in which no human subjects participated. Thus, no ethics committee approval was required.
Results
Selection of studies
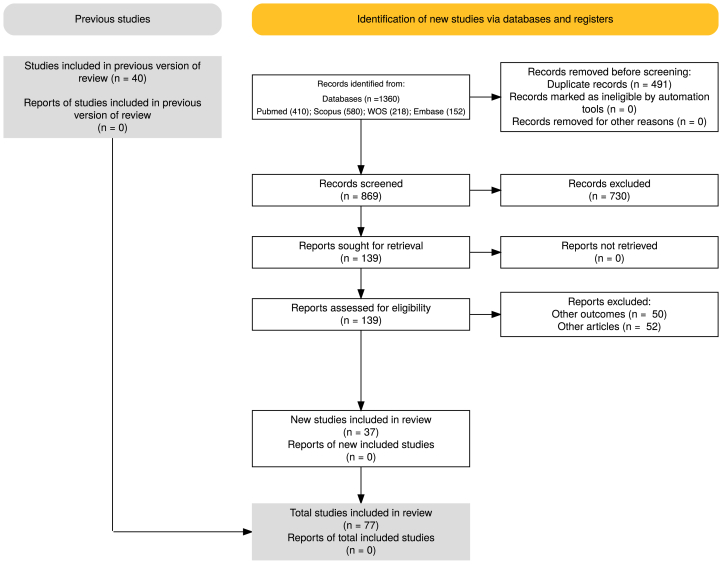
The search yielded 1400 results. After duplicates were excluded, 869 titles and abstracts were reviewed, of which 730 were excluded, and 139 scientific papers were evaluated in detail. Finally, 77 studies were included for the qualitative synthesis [[14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91]] (Fig. 1).
Fig. 1.
Flow-chart of the study selection process.
Characteristics of the studies included
Of the included studies in this systematic review, 52 studies were case report, 21 studies were case series, and four studies were case-control studies. The studies were grouped by risk factor or reason for infection. Of these, 16 studies that described a second contact with SARS-CoV-2 positive case reported a total of 165 reinfected patients with COVID-19 and five patients with recurrence of COVID-19. The mean of days after discharge or test-negative until reinfection was 56.1 (SD 53.5). These studies reported asymptomatic and mild to moderate severity of COVID-19 reinfection. Likewise, five studies that described infection related to the health profession reported a total of 11 reinfected patients with COVID-19 and two with recurrence of COVID-19. The mean of days after discharge or test negative until reinfection was 57.6 (SD 58.7). These studies reported mild to moderate severity of COVID-19 reinfection.
On the other hand, ten studies described that the source of reinfection was likely from the community and reported 107 reinfected patients with COVID-19 and 103 with recurrence of COVID-19. The mean of days after discharge or test negative until reinfection was 28.7 (SD 27.1). These studies reported mild to severe cases of COVID-19 reinfection.
Likewise, one study described travel-related infection and reported only one reinfected patient with COVID-19. The mean of days after discharge or test negative until reinfection was 102 days.
Finally, nine studies described infection related to the vulnerability due to comorbidity and reported 17 reinfected patients with COVID-19 and 423 with recurrence of COVID-19. The mean of days after discharge or test negative until reinfection was 23.3 (SD 45.8). These studies reported mild to severe cases of COVID-19 reinfection.
Finally, 36 studies did not report the risk factor or reason for reinfection and reported 87 reinfected patients with COVID-19 and 598 with recurrence of COVID-19. The mean of days after discharge or test negative until reinfection was 39.8 (SD 63.4). These studies reported asymptomatic, mild to severe cases of COVID-19 reinfection.
Assessment of risk of bias
All the case-control design studies had a low risk of bias with the Newcastle Ottawa Scale assessment. Case report and case series studies were not assessed with the risk of the bias assessment tool.
Discussion
Main findings
Our study found that patients with COVID-19 reinfection were in many risk groups, as a second contact with SARS-Cov-2, related to health profession, reinfection likely from the community, travel-related infection, and vulnerability due to comorbidity.
Reinfection and recurrence of disease by COVID-19
The human body has innate and adaptive immunity. When any viral infection occurs, IgM antibodies usually appear within one to two weeks [92]. These antibodies are then mobilized against the virus and then slowly begin to disappear. A few weeks after the infection has disappeared, IgG antibodies appear. SARS-CoV-2 positive patients begin to have detectable antibodies 10 to 14 days after the onset of symptoms, although antibody levels in patients with mild disease may be low or undetectable [93].
Protective, sustainable, and long-lasting immunity following COVID-19 infection is uncertain, and the possible associated mechanisms are not yet fully understood [94]. The immune response to COVID-19 may be variable and patient-specific regarding antibody development and persistence of antibodies in serum over time [95]. To consider the net protective effect of antibodies against reinfection, the evidence is still inadequate, and further research is warranted to clarify the interplay between the roles of adaptive and innate immunity. Immunosuppressive factors, such as drugs or pathological conditions, may hinder viral clearance and be associated with SARS-CoV-2 reactivation [96].
Inadequate immune response coupled with an inflammatory process could explain the recurrence of clinical symptoms. However, in some patients, viral RNA has been detected during the second episode, which allows us to understand the theory of reinfection or rebound virus replication [97]. Recurrences of COVID-19 must be differentiated from the persistence of viral RNA remnants that can be detected in respiratory samples up to 6 weeks after symptom onset in clinically cured patients [58].
The SARS-CoV-2 reinfection was first confirmed in August 2020 in Hong Kong by genetic sequencing of two samples collected by nasal swab from the same patient with a time difference of 142 days [92]. It was evident that the viral genomes belong to different lineages, one of which was more incident between March and April 2020, while the other is close to the strains found today [17]. Several causes have now been described for SARS-CoV-2 testing in COVID-19 patients to become positive again during the recovery period, including false RT-PCR results, intermittent viral shedding, viral reactivation or reinfection with another strain of SARS-CoV-2, or exposure to a contaminated environmental surface after discharge [98]. However, there is some possibility of false-negative RT-PCR results before patients are discharged.
In the recurrence of SARS-CoV-2, the transmission capacity depends on the cause of the re-positivity test. In addition, the replication capacity of the virus decreases when the amount of viral genetic material in the epithelial cell is low. Theoretically, if the patient is reinfected or if the virus reactivates, these patients are a potential source of transmission [49]. However, results of re-positivity testing among discharged patients have only been performed by PCR on different specimens. The RT-PCR test cannot distinguish between live and dead virus. To date, no cases of infection have been reported among persons who were in contact with repositive patients.
It is currently unclear whether the reappearance of SARS-CoV-2 RNA among COVID-19 patients after discharge could be contagious. Genetic traces of the virus detected by RT-PCR do not correlate with the transmission. However, if repositive patients are indeed carriers of live virus, they could become a potential new source of infection for others. Therefore, it is necessary to monitor the patient after discharge to prevent the spread of the pandemic. Since no treatment against SARS-CoV-2 has yet been approved and no specific vaccine is available, quarantine and prevention of infection in the community are crucial to controlling its spread [99].
Risk factors to reinfection and recurrence of disease by COVID-19
Regarding the second contact with SARS-CoV-2, the risk, in general, has been estimated to be of low risk. Likewise, related to the health profession, currently under high coverage for vaccination will be of low risk. Nevertheless, in the past, and among the first case reports, healthcare workers presented reinfection (e.g. India). In the same way, reinfection likely occurs from community transmission. Another risk factor is the travel-related infection, which currently, with regional variants circulation may pose a different risky exposure. Finally, related to the vulnerability due to comorbidities, some studies show that uncomplete vaccine schedules at those patients may pose a risk for infection but is less clear for reinfection.
Regarding to the time between reinfection, the study of Sootodeh et al. [100], referred that there are two times for epidemiological and clinical assessment of suspected reinfection cases [1]: persons with at least one detection of SARS- Cov-2 RNA test, more than 90 days after the first detection of SARS- Cov-2 RNA, whether or not symptoms were present, and [2] persons with COVID-19-like symptoms and detection of SARS-Cov-2 RNA between 45 and 89 days since first SARS-Cov-2 infection, with evidence of close-contacts with a confirmed case and without evidence of another cause of infections. This systematic review included only 25 studies and only 15 studies found reinfection.
Limitations
Still, the number of observational studies is limited. Most of the reports of reinfection consist of case series and case reports, then is still challenging to meta-analyze the prevalence of reinfection from observational studies.
Conclusions
Reinfection of patients with COVID-19 occurs between the first and second month after the first infection. The main factor for reinfection is contact with COVID-19 positive cases. However, some guidelines have provided a point of 90 days and beyond to suspect reinfection, whilst before as possible persistent infection. Further studies are required.
Funding disclosure
Financial support will not have been received for the study.
Conflicts of interest disclosure
No author has a conflict of interest.
Statement of financial support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure statement
Authors declare that they have no conflict of interest.
Patient consent
No patient consent was required for the conduct of this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nmni.2022.101021.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cook G., John Ashcroft A., Pratt G., Popat R., Ramasamy K., Kaiser M., et al. Real-world assessment of the clinical impact of symptomatic infection with severe acute respiratory syndrome coronavirus (COVID-19 disease) in patients with multiple myeloma receiving systemic anti-cancer therapy. Br J Haematol. 2020;190(2):e83–e86. doi: 10.1111/bjh.16874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elberry M.H., Ahmed H. Occult SARS-CoV-2 infection; a possible hypothesis for viral relapse. Med Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.109980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biswas A., Bhattacharjee U., Chakrabarti A.K., Tewari D.N., Banu H., Dutta S. Emergence of Novel Coronavirus and COVID-19: whether to stay or die out? Crit Rev Microbiol. 2020;46(2):182–193. doi: 10.1080/1040841x.2020.1739001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamed M.A. An overview on COVID-19: reality and expectation. Bull Natl Res Cent. 2020;44(1):86. doi: 10.1186/s42269-020-00341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shamim S., Khan M., Kharaba Z.J., Ijaz M., Murtaza G. Potential strategies for combating COVID-19. Arch Virol. 2020 doi: 10.1007/s00705-020-04768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willis V.C., Arriaga Y., Weeraratne D., Reyes F., Jackson G.P. A narrative review of emerging therapeutics for COVID-19. Mayo Clinic Proceedings: Innovations, Quality and Outcomes. 2020;4(6):745–758. doi: 10.1016/j.mayocpiqo.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dao T.L., Hoang V.T., Gautret P. Recurrence of SARS-CoV-2 viral RNA in recovered COVID-19 patients: a narrative review. European journal of clinical microbiology & infectious diseases. Official Publication of the European Society of Clinical Microbiology. 2020 doi: 10.1007/s10096-020-04088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alizargar J. Risk of reactivation or reinfection of novel coronavirus (COVID-19) Journal of the Formosan Medical Association. 2020;119(6):1123. doi: 10.1016/j.jfma.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvarez-Moreno C.A., Rodriguez-Morales A.J. Testing Dilemmas: post negative, positive SARS-CoV-2 RT-PCR - is it a reinfection? Travel Med Infect Dis. 2020;35 doi: 10.1016/j.tmaid.2020.101743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez-Morales A.J., Cardona-Ospina J.A., Villamil-Gómez W.E. Should we concern about reinfection in COVID-19? Infectio. 2020;25(2):77–78. doi: 10.22354/in.v25i2.922. [DOI] [Google Scholar]
- 11.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE. 2016;11(1) doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murad M.H., Sultan S., Haffar S., Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evidence-Based Medicine. 2018;23(2):60. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.AlFehaidi A., Ahmad S.A., Hamed E. SARS-CoV-2 re-infection: a case report from Qatar. Journal of Infection. 2020 doi: 10.1016/j.jinf.2020.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bongiovanni M. COVID-19 re-infection in an healthcare worker. Journal of Medical Virology. 2020 doi: 10.1002/jmv.26565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bongiovanni M., Basile F. Re-infection by COVID-19: a real threat for the future management of pandemia? Infectious Diseases (London, England) 2020;52(8):581–582. doi: 10.1080/23744235.2020.1769177. [DOI] [PubMed] [Google Scholar]
- 17.Bonifacio L.P., Pereira A.P.S., Araujo DCdAE., Balbao VdMP., Fonseca BALd, Passos A.D.C., et al. Are SARS-CoV-2 reinfection and Covid-19 recurrence possible? a case report from Brazil. Revista da Sociedade Brasileira de Medicina Tropical. 2020;53 doi: 10.1590/0037-8682-0619-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cao H., Ruan L., Liu J., Liao W. The clinical characteristic of eight patients of COVID-19 with positive RT-PCR test after discharge. Journal of Medical Virology. 2020;92(10):2159–2164. doi: 10.1002/jmv.26017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan P.K.S., Lui G., Hachim A., Ko R.L.W., Boon S.S., Li T., et al. Serologic responses in healthy adult with SARS-CoV-2 reinfection, Hong Kong. Emerging Infectious Diseases. 2020;26(12):3076–3078. doi: 10.3201/eid2612.203833. August 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen J., Xu X., Hu J., Chen Q., Xu F., Liang H., et al. Clinical course and risk factors for recurrence of positive SARS-CoV-2 RNA: a retrospective cohort study from Wuhan, China. Aging. 2020;12(17):16675–16689. doi: 10.18632/aging.103795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen L.Z., Lin Z.H., Chen J., Liu S.S., Shi T., Xin Y.N. Can elevated concentrations of ALT and AST predict the risk of 'recurrence' of COVID-19? Epidemiol Infect. 2020;148:e218. doi: 10.1017/s0950268820002186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Y., Bai W.Z., Liu B., Huang J., Laurent I., Chen F., et al. Re-evaluation of retested nucleic acid-positive cases in recovered COVID-19 patients: report from a designated transfer hospital in Chongqing, China. Journal of Infection and Public Health. 2020;13(7):932–934. doi: 10.1016/j.jiph.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colson P., Finaud M., Levy N., Lagier J.C., Raoult D. Evidence of SARS-CoV-2 re-infection with a different genotype. Journal of Infection. 2020 doi: 10.1016/j.jinf.2020.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coppola A., Annunziata A., Carannante N., Di Spirito V., Fiorentino G. Late reactivation of SARS-CoV-2: a case report. Front Med (Lausanne) 2020;7:531. doi: 10.3389/fmed.2020.00531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dou C.Y., Xie X., Peng Z.T., Tang H.B., Jiang Z., Zhong Z.F., et al. A case presentation for positive SARS-CoV-2 RNA recurrence in a patient with a history of type 2 diabetes that had recovered from severe COVID-19. Diabetes Research and Clinical Practice. 2020;166 doi: 10.1016/j.diabres.2020.108300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Du H.W., Chen J.N., Pan X.B., Chen X.L., Yixian Z., Fang S.F., et al. Prevalence and outcomes of re-positive nucleic acid tests in discharged COVID-19 patients. Eur J Clin Microbiol Infect Dis. 2020:1–5. doi: 10.1007/s10096-020-04024-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duggan N.M., Ludy S.M., Shannon B.C., Reisner A.T., Wilcox S.R. Is novel coronavirus 2019 reinfection possible? Interpreting dynamic SARS-CoV-2 test results through a case report. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.06.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fehdi M.A., Erragh A., Zerhouni A., Aissaoui O., Nsiri A., Alharrar R. Case report: a covid-19 reactivation case. Pan African Medical Journal. 2020;35(2):1–2. doi: 10.11604/pamj.2020.35.2.23326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandes Valente Takeda C., Moura de Almeida M., Goncalves de Aguiar Gomes R., Cisne Souza T., Alves de Lima Mota M., Pamplona de Goes Cavalcanti L., et al. Case report: recurrent clinical symptoms of COVID-19 in healthcare professionals: a series of cases from Brazil. Am J Trop Med Hyg. 2020;103(5):1993–1996. doi: 10.4269/ajtmh.20-0893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao G., Zhu Z., Fan L., Ye S., Huang Z., Shi Q., et al. Absent immune response to SARS-CoV-2 in a 3-month recurrence of coronavirus disease 2019 (COVID-19) case. Infection. 2020:1–5. doi: 10.1007/s15010-020-01485-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geling T., Huaizheng G., Ying C., Hua H. Recurrent positive nucleic acid detection in a recovered COVID-19 patient: a case report and literature review. Respir Med Case Rep. 2020;31 doi: 10.1016/j.rmcr.2020.101152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldman J.D., Wang K., Roltgen K., Nielsen S.C.A., Roach J.C., Naccache S.N., et al. Reinfection with SARS-CoV-2 and failure of humoral immunity: a case report. medRxiv : The Preprint Server for Health Sciences. 2020 doi: 10.1101/2020.09.22.20192443. [DOI] [Google Scholar]
- 33.Gousseff M., Penot P., Gallay L., Batisse D., Benech N., Bouiller K., et al. Clinical recurrences of COVID-19 symptoms after recovery: viral relapse, reinfection or inflammatory rebound? Journal of Infection. 2020;81(5):816–846. doi: 10.1016/j.jinf.2020.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gupta V., Bhoyar R.C., Jain A., Srivastava S., Upadhayay R., Imran M., et al. Asymptomatic reinfection in two healthcare workers from India with genetically distinct SARS-CoV-2. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Habadi M.I., Balla Abdalla T.H., Hamza N., Al-Gedeei A. COVID-19 reinfection. Cureus. 2020;13(1) doi: 10.7759/cureus.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanif M., Haider M.A., Ali M.J., Naz S., Sundas F.N.U. Reinfection of COVID-19 in Pakistan: a first case report. Cureus. 2020;12(10) doi: 10.7759/cureus.11176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He F., Luo Q., Lei M., Fan L., Shao X., Hu K., et al. Successful recovery of recurrence of positive SARS-CoV-2 RNA in COVID-19 patient with systemic lupus erythematosus: a case report and review. Clinical Rheumatology. 2020;39(9):2803–2810. doi: 10.1007/s10067-020-05230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He S.B., Tian J.X., Li X.D., Zhou Y.N., Xiao M.Z., Zhang Y., et al. Positive RT-PCR test results in 420 patients recovered from COVID-19 in Wuhan: an observational study. Frontiers in Pharmacology. 2020;11 doi: 10.3389/fphar.2020.549117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu R., Jiang Z., Gao H., Huang D., Jiang D., Chen F., et al. Recurrent positive reverse transcriptase-polymerase chain reaction results for coronavirus disease 2019 in patients discharged from a hospital in China. JAMA Netw Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang J., Zheng L., Li Z., Hao S., Ye F., Chen J., et al. Recurrence of SARS-CoV-2 PCR positivity in COVID-19 patients: a single center experience and potential implications. medRxiv. 2020 doi: 10.1101/2020.05.06.20089573. 2020.05.06.20089573. [DOI] [Google Scholar]
- 41.Jiang M., Li Y., Han M., Wang Z., Zhang Y., Du X. Recurrent PCR positivity after hospital discharge of people with coronavirus disease 2019 (COVID-19) J Infect. 2020;81(1):147–178. doi: 10.1016/j.jinf.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lafaie L., Celarier T., Goethals L., Pozzetto B., Grange S., Ojardias E., et al. Recurrence or relapse of COVID-19 in older patients: a description of three cases. Journal of the American Geriatrics Society. 2020;68(10):2179–2183. doi: 10.1111/jgs.16728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lan L., Xu D., Ye G., Xia C., Wang S., Li Y., et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15):1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lechien J.R., Chiesa-Estomba C.M., Vaira L.A., Saussez S., Hans S. COVID-19 reinfection and second episodes of olfactory and gustatory dysfunctions: report of first cases. Ear, Nose and Throat Journal. 2020 doi: 10.1177/0145561320970105. [DOI] [PubMed] [Google Scholar]
- 45.Lee J.-S., Kim S.Y., Kim T.S., Hong K.H., Ryoo N.-H., Lee J., et al. Evidence of severe acute respiratory syndrome coronavirus 2 reinfection after recovery from mild coronavirus disease 2019. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu F., Cai Z.B., Huang J.S., Niu H.Y., Yu W.Y., Zhang Y., et al. Repeated COVID-19 relapse during post-discharge surveillance with viral shedding lasting for 67 days in a recovered patient infected with SARS-CoV-2. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu F., Cai Z.B., Huang J.S., Yu W.Y., Niu H.Y., Zhang Y., et al. Positive SARS-CoV-2 RNA recurs repeatedly in a case recovered from COVID-19: dynamic results from 108 days of follow-up. Pathog Dis. 2020;78(4) doi: 10.1093/femspd/ftaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Loconsole D., Passerini F., Palmieri V.O., Centrone F., Sallustio A., Pugliese S., et al. Recurrence of COVID-19 after recovery: a case report from Italy. Infection. 2020;48(6):965–967. doi: 10.1007/s15010-020-01444-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lu J., Peng J., Xiong Q., Liu Z., Lin H., Tan X., et al. Clinical, immunological and virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR. EBioMedicine. 2020;59 doi: 10.1016/j.ebiom.2020.102960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luo A. Positive SARS-Cov-2 test in a woman with COVID-19 at 22 days after hospital discharge: a case report. Journal of Traditional Chinese Medical Sciences. 2020 doi: 10.1016/j.jtcms.2020.04.001. [DOI] [Google Scholar]
- 51.Marchev S., Hadzhimineva N., Simidchiev A. Clinical case: SARS-CoV-2 reactivation after a heavy Workout. Sciendo. 2020;47(3):38–40. doi: 10.2478/amb-2020-0033. [DOI] [Google Scholar]
- 52.Mardani M., Nadji S.A., Sarhangipor K.A., Sharifi-Razavi A., Baziboroun M. COVID-19 infection recurrence presenting with meningoencephalitis. New Microbes New Infect. 2020;37 doi: 10.1016/j.nmni.2020.100732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Munoz Mendoza J., Alcaide M.L. COVID-19 in a patient with end-stage renal disease on chronic in-center hemodialysis after evidence of SARS-CoV-2 IgG antibodies. Reinfection or inaccuracy of antibody testing. IDCases. 2020;22 doi: 10.1016/j.idcr.2020.e00943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nachmias V., Fusman R., Mann S., Koren G. The first case of documented Covid-19 reinfection in Israel. IDCases. 2020;22 doi: 10.1016/j.idcr.2020.e00970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ozaras R., Ozdogru I., Yilmaz A.A. Coronavirus disease 2019 re-infection: first report from Turkey. New Microbes New Infect. 2020;38 doi: 10.1016/j.nmni.2020.100774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peng D., Zhang J., Ji Y., Pan D. Risk factors for redetectable positivity in recovered COVID-19 children. Pediatr Pulmonol. 2020;55(12):3602–3609. doi: 10.1002/ppul.25116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prado-Vivar B., Becerra-Wong M., Guadalupe J.J., Márquez S., Gutierrez B., Rojas-Silva P., et al. A case of SARS-CoV-2 reinfection in Ecuador. The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30910-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Selvaraj V., Herman K., Dapaah-Afriyie K. Severe, symptomatic reinfection in a patient with COVID-19. Rhode Island Medical Journal. 2020;103(10):24–26. 2013. [PubMed] [Google Scholar]
- 59.Sharma R., Sardar S., Mohammad Arshad A., Ata F., Zara S., Munir W. A patient with asymptomatic SARS-CoV-2 infection who presented 86 Days later with COVID-19 pneumonia possibly due to reinfection with SARS-CoV-2. Am J Case Rep. 2020;21 doi: 10.12659/ajcr.927154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shui T.J., Li C., Liu H.B., Chen X., Zhang B.K. Characteristics of recovered COVID-19 patients with recurrent positive RT-PCR findings in Wuhan, China: a retrospective study. BMC Infect Dis. 2020;20(1):749. doi: 10.1186/s12879-020-05463-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.To K.K.-W., Hung I.F.-N., Ip J.D., Chu A.W.-H., Chan W.-M., Tam A.R., et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Torres DdA., Ribeiro LdCB., Riello APdFL., Horovitz D.D.G., Pinto L.F.R., Croda J. Reinfection of COVID-19 after 3 months with a distinct and more aggressive clinical presentation: case report. Journal of Medical Virology. 2020 doi: 10.1002/jmv.26637. [DOI] [PubMed] [Google Scholar]
- 63.Van Elslande J., Vermeersch P., Vandervoort K., Wawina-Bokalanga T., Vanmechelen B., Wollants E., et al. Symptomatic SARS-CoV-2 reinfection by a phylogenetically distinct strain. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu J., Cheng J., Shi X., Liu J., Huang B., Zhao X., et al. Recurrence of SARS-CoV-2 nucleic acid positive test in patients with COVID-19: a report of two cases. BMC Pulmonary Medicine. 2020;20(1):308. doi: 10.1186/s12890-020-01348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xing Y., Mo P., Xiao Y., Zhao O., Zhang Y., Wang F. Post-discharge surveillance and positive virus detection in two medical staff recovered from coronavirus disease 2019 (COVID-19), China, January to February 2020. Euro Surveill. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang C., Jiang M., Wang X., Tang X., Fang S., Li H., et al. Viral RNA level, serum antibody responses, and transmission risk in recovered COVID-19 patients with recurrent positive SARS-CoV-2 RNA test results: a population-based observational cohort study. Emerg Microbes Infect. 2020;9(1):2368–2378. doi: 10.1080/22221751.2020.1837018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ye G.M., Pan Z.Y., Pan Y.B., Deng Q.L., Chen L.J., Li J., et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. Journal of Infection. 2020;80(5):E14–E17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yoo S.Y., Lee Y., Lee G.H., Kim D.H. Reactivation of SARS-CoV-2 after recovery. Pediatrics International. 2020;62(7):879–881. doi: 10.1111/ped.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yuan B., Liu H.-Q., Yang Z.-R., Chen Y.-X., Liu Z.-Y., Zhang K., et al. Recurrence of positive SARS-CoV-2 viral RNA in recovered COVID-19 patients during medical isolation observation. Scientific Reports. 2020;10(1) doi: 10.1038/s41598-020-68782-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yuan J., Kou S., Liang Y., Zeng J., Pan Y., Liu L. Polymerase chain reaction assays reverted to positive in 25 discharged patients with COVID-19. Clinical Infectious Diseases. 2020;71(16):2230–2232. doi: 10.1093/cid/ciaa398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang J.-F., Yan K., Ye H.-H., Lin J., Zheng J.-J., Cai T. SARS-CoV-2 turned positive in a discharged patient with COVID-19 arouses concern regarding the present standards for discharge. Int J Infect Dis. 2020;97:212–214. doi: 10.1016/j.ijid.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang R.-Z., Deng W., He J., Song Y.-Y., Qian C.-F., Yu Q., et al. Case report: recurrence of positive SARS-CoV-2 results in patients recovered from COVID-19. Frontiers in Medicine. 2020;7 doi: 10.3389/fmed.2020.585485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhao W.P., Wang Y., Tang Y.F., Zhao W., Fan Y., Liu G., et al. Characteristics of children with reactivation of SARS-CoV-2 infection after hospital discharge. Clinical Pediatrics. 2020;59(9–10):929–932. doi: 10.1177/0009922820928057. [DOI] [PubMed] [Google Scholar]
- 74.Zheng J., Zhou R., Chen F., Tang G., Wu K., Li F., et al. Incidence, clinical course and risk factor for recurrent PCR positivity in discharged COVID-19 patients in Guangzhou, China: a prospective cohort study. PLoS Neglected Tropical Diseases. 2020;14(8) doi: 10.1371/journal.pntd.0008648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhu H., Fu L.Y., Jin Y.H., Shao J.L., Zhang S., Zheng N.H., et al. Clinical features of COVID-19 convalescent patients with re-positive nucleic acid detection. Journal of Clinical Laboratory Analysis. 2020;34(7) doi: 10.1002/jcla.23392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zou Y., Wang B.-R., Sun L., Xu S., Kong Y.-G., Shen L.-J., et al. The issue of recurrently positive patients who recovered from COVID-19 according to the current discharge criteria: investigation of patients from multiple medical institutions in Wuhan, China. The Journal of Infectious Diseases. 2020;222(11):1784–1788. doi: 10.1093/infdis/jiaa301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.de Brito C.A.A., Lima P.M.A., de Brito M.C.M., de Oliveira D.B. Second episode of COVID-19 in health professionals: report of two cases. Int Med Case Rep J. 2020;13:471–475. doi: 10.2147/imcrj.S277882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Adrielle Dos Santos L., Filho PGdG., Silva A.M.F., Santos J.V.G., Santos D.S., Aquino M.M., et al. Recurrent COVID-19 including evidence of reinfection and enhanced severity in thirty Brazilian healthcare workers. J Infect. 2021;82(3):399–406. doi: 10.1016/j.jinf.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Alonso F.O.M., Sabino B.D., Guimarães M.A.A.M., Varella R.B. Recurrence of SARS-CoV-2 infection with a more severe case after mild COVID-19, reversion of RT-qPCR for positive and late antibody response: case report. Journal of Medical Virology. 2021;93(2):655–656. doi: 10.1002/jmv.26432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arteaga-Livias K., Panduro-Correa V., Pinzas-Acosta K., Perez-Abad L., Pecho-Silva S., Espinoza-Sánchez F., et al. COVID-19 reinfection? A suspected case in a Peruvian patient. Travel Medicine and Infectious Disease. 2021;39 doi: 10.1016/j.tmaid.2020.101947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bellesso M., Bruniera F.R., Trunkel A.T., Nicodemo I.P. Second COVID-19 infection in a patient with multiple myeloma in Brazil - reinfection or reactivation? Hematology, Transfusion and Cell Therapy. 2021;43(1):109–111. doi: 10.1016/j.htct.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Caralis P. Case reports of COVID 19 recurrence. Journal of Primary Care & Community Health. 2021;12 doi: 10.1177/2150132720982752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Harrington D., Kele B., Pereira S., Couto-Parada X., Riddell A., Forbes S., et al. Confirmed reinfection with SARS-CoV-2 variant VOC-202012/01. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2021 doi: 10.1093/cid/ciab014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu F., Cai Z.-B., Huang J.-S., Niu H.-Y., Yu W.-Y., Zhang Y., et al. Repeated COVID-19 relapse during post-discharge surveillance with viral shedding lasting for 67 days in a recovered patient infected with SARS-CoV-2. Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 2021;54(1):101–104. doi: 10.1016/j.jmii.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Novoa W., Miller H., Mattar S., Faccini-Martínez Á.A., Rivero R., Serrano-Coll H. A first probable case of SARS-CoV-2 reinfection in Colombia. Ann Clin Microbiol Antimicrob. 2021;20(1):7. doi: 10.1186/s12941-020-00413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sicsic I., Chacon A.R., Zaw M., Ascher K., Abreu A., Chediak A. A case of SARS-CoV-2 reinfection in a patient with obstructive sleep apnea managed with telemedicine. BMJ Case Reports. 2021;14(2) doi: 10.1136/bcr-2020-240496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tuan J., Spichler-Moffarah A., Ogbuagu O. A new positive SARS-CoV-2 test months after severe COVID-19 illness: reinfection or intermittent viral shedding? BMJ Case Reports. 2021;14(2) doi: 10.1136/bcr-2020-240531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang P. Recurrent presence of SARS-CoV-2 RNA in a 33-year-old man. Journal of Medical Virology. 2021;93(2):592–594. doi: 10.1002/jmv.26334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.West J., Everden S., Nikitas N. A case of COVID-19 reinfection in the UK. Clinical Medicine (London, England) 2021;21(1):e52–e53. doi: 10.7861/clinmed.2020-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yeleti R., Guglin M., Saleem K., Adigopula S.V., Sinha A., Upadhyay S., et al. Fulminant myocarditis: COVID or not COVID? Reinfection or co-infection? Future Cardiology. 2021 doi: 10.2217/fca-2020-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zucman N., Uhel F., Descamps D., Roux D., Ricard J.-D. Severe reinfection with South African SARS-CoV-2 variant 501Y.V2: a case report. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2021 doi: 10.1093/cid/ciab129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.To K.K.W., Hung I.F.N., Ip J.D., Chu A.W.H., Chan W.M., Tam A.R., et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garcia-Beltran W.F., Lam E.C., Astudillo M.G., Yang D., Miller T.E., Feldman J., et al. COVID-19 neutralizing antibodies predict disease severity and survival. medRxiv : The Preprint Server for Health Sciences. 2020 doi: 10.1101/2020.10.15.20213512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoang V.T., Dao T.L., Gautret P. Recurrence of positive SARS-CoV-2 in patients recovered from COVID-19. J Med Virol. 2020;92(11):2366–2367. doi: 10.1002/jmv.26056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Elrashdy F., Aljaddawi A.A., Redwan E.M., Uversky V.N. On the potential role of exosomes in the COVID-19 reinfection/reactivation opportunity. Journal of Biomolecular Structure and Dynamics. 2020:1–12. doi: 10.1080/07391102.2020.1790426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ota M. Will we see protection or reinfection in COVID-19? Nature Reviews Immunology. 2020;20(6):351. doi: 10.1038/s41577-020-0316-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Falahi S., Kenarkoohi A. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes and New Infections. 2020;38 doi: 10.1016/j.nmni.2020.100812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.To K.K.-W., Hung I.F.-N., Chan K.-H., Yuan S., To W.-K., Tsang D.N.-C., et al. Serum antibody profile of a patient with COVID-19 reinfection. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2020 doi: 10.1093/cid/ciaa1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dao T.L., Hoang V.T., Gautret P. Recurrence of SARS-CoV-2 viral RNA in recovered COVID-19 patients: a narrative review. Eur J Clin Microbiol Infect Dis. 2020 doi: 10.1007/s10096-020-04088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sotoodeh Ghorbani S., Taherpour N., Bayat S., Ghajari H., Mohseni P., Hashemi Nazari S.S. Epidemiologic characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID-19: a systematic review and meta-analysis. J Med Virol. 2022;94(1):44–53. doi: 10.1002/jmv.27281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.