Abstract
Background
Obesity is associated with increased complications after total joint arthroplasty (TJA), leading some surgeons to recommend nutrition counseling and weight loss. We aim to evaluate the effect of preoperative nutritionist referral on weight loss and likelihood of surgery in obese patients seeking primary TJA.
Methods
A retrospective cohort of patients seeking primary TJA who were referred to a licensed nutritionist for weight loss was matched by age, sex, and body mass index (BMI) to an unreferred control group. BMI change was compared between groups up to 1 year of follow-up. Differences were determined using 2-tailed t-tests and chi-squared tests with a significance cutoff of P < .05.
Results
A total of 274 referred patients and 174 controls were included in our analysis. Patients who were referred to a nutritionist achieved significantly greater average BMI change (−1.5 kg/m2) than controls (−0.8 kg/m2) by 6 months after first contact (P = .01) although significance was lost at 1 year after first contact (P = .21). Thirty-eight percent of referred patients went on to TJA compared with 28% of controls (P < .01).
Conclusions
Referral to a licensed nutritionist modestly improves early weight loss and is associated with a higher rate of surgery in obese patients seeking primary TJA.
Keywords: Arthroplasty, Obesity, BMI, Nutrition, Weight loss
Introduction
Over 50% of the United States population is estimated to be overweight or obese [1,2]. Obese patients exhibit a 2-fold increased risk of osteoarthritis, and morbidly obese patients exhibit a 4-fold increased risk [2]. As a result, demand for lower extremity total joint arthroplasty (TJA) has been on the rise. Based on National Inpatient Sample combined with Census Bureau data from 2000 to 2014, total hip arthroplasties (THAs) performed in the United States are projected to increase 71%-129% between 2014 and 2030, and total knee arthroplasties (TKAs) are projected to increase 85%-182% [3,4].
Lower extremity TJA in obese patients has been associated with longer hospital stays, higher health-care costs, and increased rates of component malalignment and dislocation [[5], [6], [7], [8], [9], [10]]. Obese patients undergoing TJA also have a higher medical comorbidity burden than their nonobese counterparts, contributing to complications from anesthesia as well as need for postoperative intensive care unit monitoring and respiratory assistance [11,12]. Obesity is also known to independently increase risk of deep vein thrombosis and pulmonary embolism [13,14]. Lastly, obesity has been linked to significantly higher rates of both superficial and deep surgical site infections following TJA [15,16].
To mitigate these risks, many arthroplasty surgeons limit their surgical candidates to patients that fall below a body mass index (BMI) cutoff. These restrictions may stem from the 2013 American Association of Hip and Knee Surgeons consensus statement that morbidly obese (BMI >40) and super obese (BMI >50) patients have complication profiles that may outweigh the functional benefits of TJA [17]. Many surgeons utilize dietary counseling and exercise programs in order to help obese patients meet weight-loss goals and become more suitable surgical candidates. Despite these efforts, there have been no robust investigations to date about the effectiveness of preoperative weight-loss programs.
At our institution, it has been our guideline since November 2015 to refer all patients with a BMI of 40 or greater to a licensed nutritionist as part of a preoperative optimization program. We hypothesized that this intervention would help obese patients seeking TJA lose weight and become better surgical candidates. In the present study, we aimed to assess the effect of reflex referral to a nutritionist on weight loss by comparing to a historical control cohort prior to implementation of this policy.
Material and methods
Data collection
After obtaining approval from our institutional review board, we retrospectively compiled a list of adult patients of any BMI seeking primary TKA or THA who were referred to a nutritionist for weight loss.
Demographic data, including age, gender, height, and number of pertinent comorbidities, were collected via chart review for each patient (Table 1). Pertinent comorbidities were defined as coronary artery disease, congestive heart failure, atrial fibrillation, chronic lung pathology such as chronic obstructive pulmonary disease or interstitial lung disease, chronic kidney disease, diabetes mellitus, history of stroke, history of deep vein thrombosis or pulmonary embolism, hypertension, liver disease, obstructive sleep apnea, and hyperlipidemia. For both operative and nonoperative patients, weights were recorded at the time of first contact with a nutritionist, 6 months after first contact, and 1 year after first contact. Weights were measured in clinic, not patient-reported.
Table 1.
Patient demographics.
| Patient factor | Referred | Control | P value |
|---|---|---|---|
| N | 273 | 174 | |
| Sex | |||
| Male | 89 (33%) | 61 (35%) | .3 |
| Female | 184 (67%) | 113 (65%) | |
| Chief complaint | |||
| Hip | 79 (29%) | 60 (34%) | .06 |
| Knee | 194 (71%) | 114 (66%) | |
| Operative status | |||
| Operative | 105 (38%) | 48 (28%) | <.01 |
| Nonoperative | 168 (62%) | 126 (72%) | |
| Avg. # of comorbidities | 3 | 4 | .09 |
| Avg. # of nutritionist visits | 5 | ||
| Avg. starting BMI | 42.0 | 41.2 | .12 |
Number of total included patients, sex, chief complaint, operative status during the study period, average number of comorbidities, and average starting BMI were demographic factors collected for both referred and control groups. Average number of total nutritionist visits were also listed for the referred group. Only operative status was significantly different between groups (P < .01, in bold).
As a control, a list of new patients seen in our adult lower-extremity TJA clinic between January 2012 and October 2015 was generated using automated reports through the electronic medical records system. This timeframe predates implementation of our guidelines for routine nutritionist referral for morbidly obese patients. Patients were matched to our referred cohort by age (within 4 years), sex, and BMI (within 0.5 kg/m2). All matching occurred prior to patient exclusion. The same demographic and weight data outlined above were collected for our matched control cohort. For both operative and nonoperative control patients, weights were recorded at the time of first contact with our clinic, 6 months after first contact, and 1 year after first contact.
Inclusion/exclusion criteria
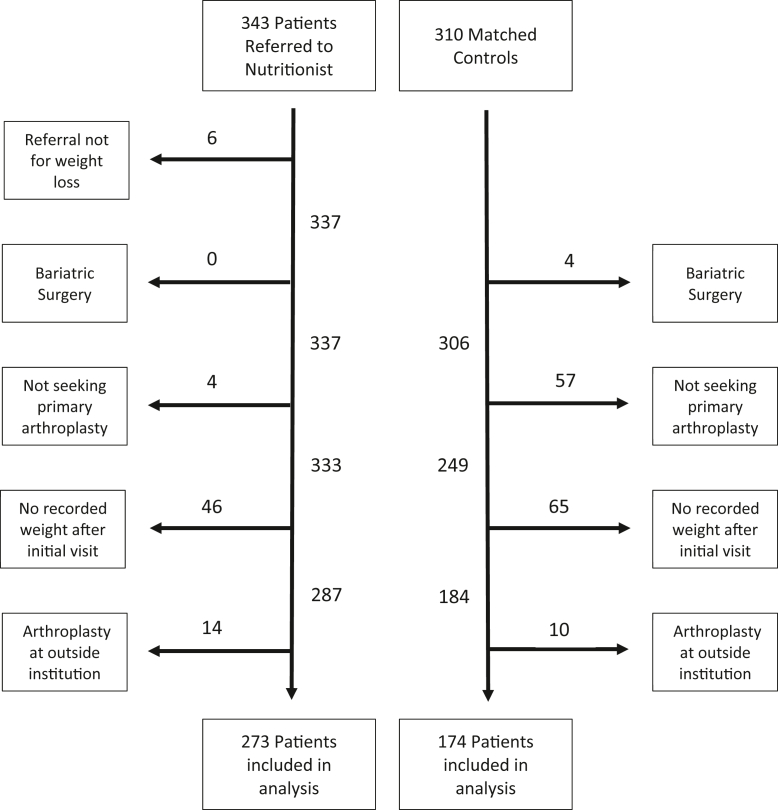
Patients older than 18 years who were referred for increased BMI and seeking primary THA or TKA met inclusion criteria. To be included in our referred cohort, the patients must have had at least 1 visit with a nutritionist after referral. Exclusion criteria (Fig. 1) included nutritionist referral for reasons other than weight loss, presenting for reasons other than seeking primary TJA, no recorded weights after first contact, having undergone arthroplasty at an outside institution during the study period, and bariatric surgery performed prior to or during the study period.
Figure 1.
Patients excluded from analysis. Exclusion criteria included nutritionist referral for reason other than weight loss, presenting for reason other than seeking primary TJA, no recorded weights after first contact, having undergone arthroplasty at an outside institution during the study period, and bariatric surgery performed prior to or during the study period. After application of exclusion criteria, 273 referred patients and 174 matched control patients were included in our final analysis.
Statistics
We used 2-tailed t-tests for BMI comparisons between our referred and control cohorts. Change in BMI (ΔBMI) was compared at 6-month intervals after first contact. Analysis was performed first without respect to operative status and then stratified by whether the patient went on to TJA. We used Pearson’s chi-squared test in comparing the rate of surgery between referred and control groups. A significance cutoff of P < .05 was used.
Additionally, we performed linear regression modeling using the Stata/MP (version 14.2; College Station, TX) software to assess how ΔBMI achieved by 6 months after the first nutritionist visit was associated with the number of nutritionist visits, age, gender, number of comorbidities, whether the primary complaint was hip or knee pain, and operative status.
Results
We identified 343 patients who had been referred to a nutritionist with at least 1 visit between November 2015 and August 2019. Seventy of these patients were ultimately excluded from analysis (Fig. 1); 6 patients were referred for reasons other than weight loss, 4 patients were not seeking primary TJA, 46 patients had no recorded weights after first contact with the nutritionist, and 14 patients went on to arthroplasty at an outside institution during the study period. After exclusion, 273 patients were included in our analysis. Of 105 operative referred patients, all 105 had recorded weights 6 months after their first nutritionist contact, and 74 patients had recorded weights at 1 year after first contact. Of 168 nonoperative patients, 152 had recorded weights at 6 months after their first nutritionist contact, and 123 patients had recorded weights at 1 year after first contact.
From an initial pool of 4149 new patient visits between January 2012 and October 2015, 310 patients were able to be matched based on age, sex, and BMI as outlined in the methods above. Of these 310 patients, 136 were excluded from the analysis (Fig. 1); 4 patients underwent bariatric surgery prior to or during the study period, 57 patients were not seeking primary joint arthroplasty, 65 patients had no recorded weights after first clinic contact, and 10 patients went on to arthroplasty at an outside institution during the study period. After exclusion, 174 matched control patients were included in our analysis. Of 48 operative control patients, all 48 had recorded weights at 6 months after their first clinic contact, and 46 patients had recorded weights at 1 year after first contact. Of 126 nonoperative control patients, 112 had recorded weights at 6 months after the first clinic contact, and 109 patients had recorded weights at 1 year after first contact. Fifteen of 174 control patients (8.6%) did have at least 1 visit with a nutritionist during the study period. Three patients were referred by an orthopaedic provider, while 12 were referred by their primary care physician. None of these patients were excluded from the analysis, as our original aim was to assess the effectiveness of the reflex referral policy for morbidly obese patients. It seems that prior to this policy, nutritionist referral (regardless of BMI) was rare.
Within the referred and control groups, respectively, 33% and 35% were male, 29% and 34% had a chief complaint of hip pain, 71% and 66% had a chief complaint of knee pain, 3 and 4 were the average number of medical comorbidities, and 42.0 (26.0-62.9) and 41.2 (26.1-55.9) were the average starting BMIs. Referred patients had an average of 5 nutritionist visits (range: 1 to 57 visits). There were no statistically significant differences in gender (P = .30), chief complaint (P = .06), number of comorbidities (P = .09), or starting BMI (P = .12). Thirty-eight percent of referred patients went on to TJA compared with 28% in the control group, which represents a statistically significant difference (P < .01) (Table 1).
As seen in Table 2, patients who were referred to a nutritionist achieved a statistically significant ΔBMI by 6 months after the first nutritionist contact (−1.5 kg/m2; P < .01). This also represents a significantly greater average ΔBMI than that of controls (−0.8 kg/m2) during this same time interval (P = .01). Referred patients maintained an average ΔBMI of −1.1 kg/m2 at 1 year after first contact. Control patients (not referred) maintained an average ΔBMI of −0.7 kg/m2 over this same time interval although the difference in ΔBMI was no longer statistically significant (P = .21). Control patients did not demonstrate significant ΔBMI throughout the study period.
Table 2.
Average BMI change of referred and control groups up to 1 y of follow-up.
| Patient group | Starting BMI | △BMI (6 mo) | △BMI (1 y) |
|---|---|---|---|
| Referred | 42.0 (26.0-62.9) | −1.5a | −1.1 |
| Control | 41.2 (26.1-55.9) | −0.8 | −0.7 |
| P value | .12 | .01 | .21 |
| Operative | |||
| Referred | 39.6 (26.0-49.2) | −2.4a | −2.1a |
| Control | 38.0 (28.6-52.1) | −2.0a | −1.3 |
| P value | .02 | .52 | .14 |
| Nonoperative | |||
| Referred | 43.6 (28.3-62.9) | −0.9 | −0.5 |
| Control | 42.4 (26.1-55.9) | −0.2 | −0.5 |
| P value | .09 | .02 | .98 |
BMI change (△BMI) was reported at 6-mo intervals up to 1 y after first nutritionist visit (for referred patients) or first clinic visit (for control patients). P values denoting statistically significant difference in BMI or △BMI between referred and control groups are bolded.
A statistically significant change from starting BMI (P < .05).
When stratified by operative status, patients who went on to joint arthroplasty did not demonstrate a significant difference in weight loss between referred and control groups at any point during the study period (Table 2). However, among patients who did not have surgery, referred patients achieved significantly greater ΔBMI (−0.9 kg/m2) than controls (−0.2 kg/m2) by 6 months after first contact (P = .02) (Table 2). This difference was lost by 1 year after contact, with both groups maintaining an average ΔBMI of −0.5 kg/m2 (P = .98).
Operative patients who were referred to a nutritionist achieved significantly greater ΔBMI (−2.4 kg/m2) than nonoperative referred patients (−0.9 kg/m2) by 6 months after the first nutritionist contact (P < .01). Operative referred patients were also able to maintain a significantly greater ΔBMI (−2.1 kg/m2) than nonoperative referred patients (−0.5 kg/m2) at 1 year after first contact (P < .01). Operative control patients achieved significantly greater ΔBMI (−2.0 kg/m2) than nonoperative control patients (−0.2 kg/m2) by 6 months after first clinic contact (P < .01). At 1 year after first clinic contact, however, operative control patients were not able to maintain a significantly greater ΔBMI (−1.3 kg/m2) than nonoperative control patients (−0.5 kg/m2) (P = .09).
When stratified by BMI, including only those patients with BMI ≥40, referred patients (N = 164) achieved a ΔBMI of −1.6 kg/m2 by 6 months after first nutritionist contact and ΔBMI of −1.2 kg/m2 by 1 year after first contact. Compared with controls (N = 96), who achieved a ΔBMI of −1.1 kg/m2 and −1.3 kg/m2 over the same time intervals, this did not represent a statistically significant difference at either 6 months (P = .20) or 1 year (P = .73) after first contact.
In the multivariable regression analysis, the only predictors that were associated with ΔBMI were the number of nutritionist visits (beta = −0.07; 95% confidence interval −0.12 to −0.02; P = .01) and operative status (beta = −1.42; 95% confidence interval −2.05 to −0.80; P < .01). Age, gender, number of comorbidities, and primary joint pathology were not predictive of ΔBMI.
Discussion
Obesity is a known risk factor for the development and progression of hip and knee osteoarthritis. Importantly, it is also associated with increased hospital costs and higher rates of perioperative complications in patients undergoing TJA [[5], [6], [7], [8], [9], [10], [11], [12], [13], [14],18]. For this reason, many surgeons have adopted strict BMI cutoffs in selecting the most favorable surgical candidates. The patients who do not meet this cutoff are often counseled on diet, nutrition, or exercise programs to aid in weight loss. Currently, there is a paucity of evidence on the effectiveness of nonoperative patient optimization programs on weight loss prior to TJA. We sought to determine the impact of nutritionist referral for obese patients seeking primary THA or TKA.
In this study, we have demonstrated that referral to a licensed nutritionist improves early weight loss and is associated with a higher rate of surgery in obese and morbidly obese patients seeking primary THA or TKA. Previous studies have demonstrated significant improvement in patient quality-of-life scores with access to arthroplasty surgery while patients waiting for arthroplasty have poorer scores [[19], [20], [21]]. Thus, nutritionist intervention can be utilized to positively impact patient quality of life through increasing eligibility for surgery.
Given the established risks associated with increased BMI in TJA, it is imperative that providers help their patients manage this modifiable risk factor. To our knowledge, this is the first study to demonstrate that a simple referral to a licensed nutritionist can result in greater preoperative weight loss and, therefore, could potentially reduce the risk of adverse outcomes. Unfortunately, there are few reports on preoperative weight loss and TJA outcomes. One study using the Total Joint Replacement Registry in California identified obese TJA patients and found that 12.4% of TKA and 18% of THA patients lost at least 5% of their body weight prior to surgery [22]. However, there was no statistically significant difference in surgical site infection or readmission in this cohort. In contrast, a 2019 single-institution study of morbidly obese TKA patients found that preoperative weight loss of at least 20 pounds reduced length of stay and odds of discharge to a rehabilitation facility after surgery [23]. Although there is no strong evidence of improved outcomes in TJA in the setting of preoperative weight loss, this may in part be due to the relative catabolic state and nutritional imbalance that can occur after significant weight loss [24,25]. Therefore, it is possible that a preoperative weight loss program guided by a nutritionist may result in different outcomes. There is an ongoing randomized trial to assess weight loss prior to TJA using a remote dietician and mobile app, which may provide further evidence to support this intervention [26].
Another important finding in our study was that the number of nutritionist visits correlated positively with ΔBMI. This finding is in agreement with previous literature [27,28]. More appointments may help patients with weight loss goals by holding patients accountable and providing ongoing motivation and guidance.
Operative referred patients achieved greater ΔBMI than nonoperative referred patients by 6 months after first nutritionist contact. This difference may be accounted for by an increased level of motivation caused by the upcoming surgery, as the average time to surgery in our cohort was 7 months after first contact. However, this finding may simply reflect that patients who were successful at losing weight were more likely to be offered surgery. When examining only surgical patients, there was no difference in ΔBMI between referred and control patients by 6 months after first contact. However, it should be noted that a significantly greater proportion of referred patients went on to TJA (38%) than controls (28%) (P < .01). This likely reflects improved weight loss and surgical candidacy among referred patients. When examining only nonoperative patients, referred patients lost significantly more weight than their control counterparts at 6 months but not at 1 year after first contact. This may reflect an early but unsustained impact of nutritionist referral on weight loss.
Although the focus of the present study was on referral for elevated BMI, nutritionist referral may also be indicated for correction of malnutrition. It has been demonstrated that malnutrition, often identified as low albumin, increases complications and cost after TJA [29,30]. Furthermore, obesity and malnutrition are often associated [31]. Therefore, connecting obese patients with a licensed nutritionist for weight loss may also be important for improving their overall nutritional status. Indeed, nutrition supplementation has been shown to reduce complications in geriatric hip fracture patients [32,33]. Future studies investigating nutritionist referral impact on arthroplasty patients should consider the role of nutritional status as well.
Limitations
Our study has several limitations. First, the decision to refer a patient to a nutritionist is at the discretion of the provider. Although all providers in the present study agreed upon referral for all patients with BMI >40, many patients with lower BMIs were also included in our analysis. When stratified to include only patients with starting BMI of 40 or above, the effect size of referral was notably decreased and importantly was no longer statically significant. This loss of significance may be partially attributed to decreased sample size but may also reflect the effect of motivated referred patients with BMI <40 whose disposition could not be accurately matched in the historical control group. Additionally, the BMI referral trigger of 40, although supported in the literature [23,34], may not accurately reflect the ideal candidates for nutritionist referral. It has been shown that increasing BMI is associated with a stepwise increase in complications [18], and perhaps patients with a BMI below 40 would benefit at least as much from nutritionist intervention.
Another limitation is the possibility that some patients, regardless of BMI, requested a nutritionist referral due to personal motivation and therefore were included. This may have introduced selection bias as motivation is an important factor in achieving and sustaining weight loss [35]. Additionally, our study setting was a large, academic center with an established referral pathway to a licensed nutritionist at the same institution. The ease of this referral may not exist in alternative practice settings, negatively impacting the generalizability of this study.
Although there were no differences in demographics between referred and control groups, this was a retrospective study in which we matched our referred patients to a historical control group. Therefore, there may have been differences between the 2 groups in providers encountered as well as access to weight loss services besides nutrition counseling. Follow-up among each group was also not complete, which may have introduced variability in the study groups affecting our results.
Lastly, the mean ΔBMI seen in both referred and control groups was modest, and its clinical significance is yet unclear. However, an increased proportion of referred patients (38%) compared with controls (28%) went on to surgery, and that group achieved greater overall weight loss. Thus, while the average effect size was small, it is likely that a select group benefited from nutritionist referral enough to increase their probability of meeting appropriateness criteria for surgery.
Conclusions
As obesity rates continue to rise, arthroplasty surgeons must be aware of the associated increased costs and perioperative complications. One simple approach to manage this modifiable risk factor is patient education through nutritionist referral. We have demonstrated that routine referral to a licensed nutritionist modestly improves early weight loss and is associated with a higher rate of surgery in obese and morbidly obese patients seeking primary THA or TKA. Future studies should aim to identify an optimal referral protocol and determine if nutritionist referral improves postoperative outcomes.
Conflicts of interest
Brian R. Hallstrom is a committee member for the Data Committee of the AAOS American Joint Replacement Registry. The remaining authors have no conflicts of interest or financial disclosures to report.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.07.018.
Ethical Review Committee Statement
IRB HUM00175680 approved 02/07/2020.
Acknowledgments
The authors would like to acknowledge the contributions of Nutrition Services at Michigan Medicine as well as Elie Ellenberg, MD.
Appendix A. Supplementary Data
References
- 1.Flegal K.M., Carroll M.D., Ogden C.L., Curtin L.R. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad A.H., Ford E.S., Bowman B.A., Dietz W.H., Vinicor F., Bales V.S., et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 3.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 4.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez-Merchan E.C. The influence of obesity on the outcome of TKR: can the impact of obesity be justified from the viewpoint of the overall health care system? HSS J. 2014;10:167–170. doi: 10.1007/s11420-014-9385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajgopal V., Bourne R.B., Chesworth B.M., MacDonald S.J., McCalden R.W., Rorabeck C.H. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23:795–800. doi: 10.1016/j.arth.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Davis W., Porteous M. Joint replacement in the overweight patient: a logical approach or new form of rationing? Ann R Coll Surg Engl. 2007;89:203–206. doi: 10.1308/003588407X183247. discussion 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mnatzaganian G., Ryan P., Norman P.E., Davidson D.C., Hiller J.E. Use of routine hospital morbidity data together with weight and height of patients to predict in-hospital complications following total joint replacement. BMC Health Serv Res. 2012;12:380. doi: 10.1186/1472-6963-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman R.J., Hess S., Berkowitz S.D., Homering M. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin Orthop Relat Res. 2013;471:3358–3366. doi: 10.1007/s11999-013-3049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwarzkopf R., Thompson S.L., Adwar S.J., Liublinska V., Slover J.D. Postoperative complication rates in the “super-obese” hip and knee arthroplasty population. J Arthroplasty. 2012;27:397–401. doi: 10.1016/j.arth.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Domi R., Laho H. Anesthetic challenges in the obese patient. J Anesth. 2012;26:758–765. doi: 10.1007/s00540-012-1408-4. [DOI] [PubMed] [Google Scholar]
- 12.Kulkarni K., Karssiens T., Kumar V., Pandit H. Obesity and osteoarthritis. Maturitas. 2016;89:22–28. doi: 10.1016/j.maturitas.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Mantilla C.B., Horlocker T.T., Schroeder D.R., Berry D.J., Brown D.L. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552–560. doi: 10.1097/00000542-200309000-00009. discussion 5A. [DOI] [PubMed] [Google Scholar]
- 14.Memtsoudis S.G., Besculides M.C., Gaber L., Liu S., González Della Valle A. Risk factors for pulmonary embolism after hip and knee arthroplasty: a population-based study. Int Orthop. 2009;33:1739–1745. doi: 10.1007/s00264-008-0659-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward D.T., Metz L.N., Horst P.K., Kim H.T., Kuo A.C. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015;30:42–46. doi: 10.1016/j.arth.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 16.Malinzak R.A., Ritter M.A., Berend M.E., Meding J.B., Olberding E.M., Davis K.E. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24:84–88. doi: 10.1016/j.arth.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Workgroup of the American Association of Hip and Knee Surgeons Evidence Based Committee Obesity and total joint arthroplasty: a literature based review. J Arthroplasty. 2013;28:714–721. doi: 10.1016/j.arth.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 18.Zusmanovich M., Kester B.S., Schwarzkopf R. Postoperative complications of total joint arthroplasty in obese patients stratified by BMI. J Arthroplasty. 2018;33:856–864. doi: 10.1016/j.arth.2017.09.067. [DOI] [PubMed] [Google Scholar]
- 19.Miettinen H.J.A., Mäkirinne-Kallio N., Kröger H., Miettinen S.S.A. Health-Related quality of life after hip and knee arthroplasty operations. Scand J Surg. 2020;110:427–433. doi: 10.1177/1457496920952232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lange J.K., Lee Y.-Y., Spiro S.K., Haas S.B. Satisfaction rates and quality of life changes following total knee arthroplasty in age-differentiated cohorts. J Arthroplasty. 2018;33:1373–1378. doi: 10.1016/j.arth.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 21.Shah A.M.U.D., Afzal F., Ans M., Ayaz S., Niazi S.G., Asim M., et al. Quality of life before and after total knee arthroplasty in clinical settings across Lahore, Pakistan. Pak J Pharm Sci. 2019;32:769–772. [PubMed] [Google Scholar]
- 22.Inacio M.C.S., Kritz-Silverstein D., Raman R., Macera C.A., Nichols J.F., Shaffer R.A., et al. The impact of pre-operative weight loss on incidence of surgical site infection and readmission rates after total joint arthroplasty. J Arthroplasty. 2014;29:458–464.e1. doi: 10.1016/j.arth.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 23.Keeney B.J., Austin D.C., Jevsevar D.S. Preoperative weight loss for morbidly obese patients undergoing total knee arthroplasty: determining the necessary amount. J Bone Joint Surg Am. 2019;101:1440–1450. doi: 10.2106/JBJS.18.01136. [DOI] [PubMed] [Google Scholar]
- 24.Koch T.R., Finelli F.C. Postoperative metabolic and nutritional complications of bariatric surgery. Gastroenterol Clin North Am. 2010;39:109–124. doi: 10.1016/j.gtc.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Granado-Lorencio F., Simal-Antón A., Salazar-Mosteiro J., Herrero-Barbudo C., Donoso-Navarro E., Blanco-Navarro I., et al. Time-course changes in bone turnover markers and fat-soluble vitamins after obesity surgery. Obes Surg. 2010;20:1524–1529. doi: 10.1007/s11695-010-0257-1. [DOI] [PubMed] [Google Scholar]
- 26.Seward M.W., Antonelli B.J., Giunta N., Iorio R., Fitz W., Lange J.K., et al. Weight loss before total joint arthroplasty using a remote dietitian and mobile app: study protocol for a multicenter randomized, controlled trial. J Orthop Surg Res. 2020;15:531. doi: 10.1186/s13018-020-02059-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schlicht C., Shaw C., Haglund K., Breakwell S. Evaluation of a primary care weight loss program. J Dr Nurs Pract. 2017;10:79–84. doi: 10.1891/2380-9418.10.1.79. [DOI] [PubMed] [Google Scholar]
- 28.Tussing-Humphreys L.M., Fitzgibbon M.L., Kong A., Odoms-Young A. Weight loss maintenance in African American women: a systematic review of the behavioral lifestyle intervention literature. J Obes. 2013;2013:437369. doi: 10.1155/2013/437369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bala A., Ivanov D.V., Huddleston J.I., Goodman S.B., Maloney W.J., Amanatullah D.F. The cost of malnutrition in total joint arthroplasty. J Arthroplasty. 2020;35:926–932.e1. doi: 10.1016/j.arth.2019.11.018. [DOI] [PubMed] [Google Scholar]
- 30.Ellsworth B., Kamath A.F. Malnutrition and total joint arthroplasty. J Nat Sci. 2016;2:e179. [PMC free article] [PubMed] [Google Scholar]
- 31.Peterson L.A., Cheskin L.J., Furtado M., Papas K., Schweitzer M.A., Magnuson T.H., et al. Malnutrition in bariatric surgery candidates: multiple micronutrient deficiencies prior to surgery. Obes Surg. 2016;26:833–838. doi: 10.1007/s11695-015-1844-y. [DOI] [PubMed] [Google Scholar]
- 32.Eneroth M., Olsson U.-B., Thorngren K.-G. Nutritional supplementation decreases hip fracture-related complications. Clin Orthop Relat Res. 2006;451:212–217. doi: 10.1097/01.blo.0000224054.86625.06. [DOI] [PubMed] [Google Scholar]
- 33.He Y., Xiao J., Shi Z., He J., Li T. Supplementation of enteral nutritional powder decreases surgical site infection, prosthetic joint infection, and readmission after hip arthroplasty in geriatric femoral neck fracture with hypoalbuminemia. J Orthop Surg Res. 2019;14:292. doi: 10.1186/s13018-019-1343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martin J.R., Watts C.D., Taunton M.J. Bariatric surgery does not improve outcomes in patients undergoing primary total knee arthroplasty. Bone Joint J. 2015;97-B:1501–1505. doi: 10.1302/0301-620X.97B11.36477. [DOI] [PubMed] [Google Scholar]
- 35.Williams G.C., Grow V.M., Freedman Z.R., Ryan R.M., Deci E.L. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.