Throughout its history, endourology has witnessed several turning points: the development of endoscopes and fiber optic technology, the introduction of shockwave lithotripsy, and most recently the emergence of thulium fiber laser (TFL) technology for lithotripsy. Sooner rather than later, TFL will overtake Ho:YAG lasers as the gold standard for lithotripsy for several reasons (Table 1).
Table 1.
Main features and advantages of thulium fiber laser in comparison to Ho:YAG laser technology according to the current review, including preclinical and clinical studies
| Thulium fiber laser features | Detail |
|---|---|
| Machine specifications | Constant peak power up to 500 W |
| Higher pulse energy range | |
| Higher pulse frequency range | |
| Very long pulse duration (up to 50 ms) | |
| Smaller and lighter than Ho:YAG lasers | |
| Quiet air-cooling mechanism | |
| Lower energy consumption | |
| Standard electrical power outlet | |
| Ablation efficiency | |
| Ablation speed | Fragment ablation two times faster than Ho:YAG |
| Dusting four to five times faster than Ho:YAG | |
| Shorter operating room time | |
| Dust and residual particles | Greater quantity of dust |
| Significantly smaller dust particles than with Ho:YAG | |
| Retropulsion | Lower degree of retropulsion |
| Different peak power, water absorption, and pulse shape | |
| Visibility | Less retropulsion, meaning better visibility |
| Snowstorm effect | |
| Laser fibers | Major deflection |
| Energy-resistant | |
| Optimal irrigation | |
| Lower fiber degradation (uniform beam profile) | |
| Miniaturization possibilities | |
| Smaller stone fragments | |
| Safety | Can be used in any anatomical location |
| Can be used in any endoscopic approach | |
| Smaller residual fragments (no basketing) | |
| Better visibility, meaning less unintended laser damage | |
| Temperature safety | No temperature differences between TFL and Ho:YAG |
| No amplified temperature rises with TFL | |
| Similar thermal safety precautions for TFL and Ho:YAG |
Preclinical studies have shown promising results, with more efficient stone ablation and faster ablation speed with TFL. In comparison to Ho:YAG lasers (or high-power Ho:YAG with Moses technology), the laser time and operative time with TFL were twice as fast when fragmentation settings were used and up to five times faster for dusting [1]. Moreover, TFL has greater ablative capacity for both soft uric acid stones and hard oxalate monohydrate stones, being 1.5 to four times more efficient than Ho:YAG lasers [1]. The TFL technology is not only able to produce stone dust from all prevailing stone types but is also superior to Ho:YAG lasers in generating stone particles <150 μm, regardless of the stone type or laser settings, and produces at least twice as much dust in comparison to Moses technology [1], [2]. Small particles are clearly advantageous as fewer basketing passes are required, which further reduces complications and operating room time.
These findings have been replicated in several clinical studies since the US Food and Drug Administration and European CE mark approvals in 2019 and 2020, respectively [3]. According to a prospective randomized study on stone lithotripsy following mini-percutaneous nephrolithotomy, the operative time was twice as fast with TFL and the stone-free rate was comparatively higher than with Ho:YAG laser [4]. Moreover, Ulvik et al. [5] have recently published the first prospective randomized trial showing that TFL is superior to Ho:YAG in terms of the stone-free rate, shorter operative time, and fewer intraoperative complications.
All these beneficial results are due to a lower degree of retropulsion. With the same energy and pulse frequency setting, the TFL device produces significantly lower retropulsion forces than the current Ho:YAG technology [6]. This can be explained by several TFL characteristics, including the different laser pulse shapes, prolonged peak power levels, and fourfold higher wavelength absorption by water [6], [7]. The lower degree of retropulsion has been objectively evaluated in in vitro studies and observed in several clinical studies, and it improves the view owing to minimum medium turbulence [3], [4], [5]. The better vision means that TFL is more easily operated by less experienced users, reducing the learning curve and the need to constantly adapt to a continuously changing stone position [1], [3].
Moreover, TFL generates a much more uniform and focused laser beam that can be transmitted by laser fibers with a smaller core diameter (50–150 μm) [8]. Smaller laser fibers allow better irrigation though the working channel and thus greater visibility. This is precisely the limitation of Ho:YAG lasers: they can only safely accept fibers with a core diameter of >200 μm. Another major potential would be the possibility to reduce the working channel diameter of ureteroscopes, thus allowing overall instrument miniaturization [1]. In addition, laser fibers for TFL are more capable of resisting important ureteroscope deflections than Ho:YAG lasers. This is important because the small laser fibers with TFL allow better instrument deflection and the urologist is therefore able to treat lower-pole calyceal stones. Furthermore, the smaller diameter of the laser fibers for TFL contributes to the production of smaller stone fragments and, despite their diameter, they still produce higher ablation volumes than the larger-diameter Ho:YAG fibers [1]. The use of smaller core diameters means that the energy density delivered by these fibers is significantly higher.
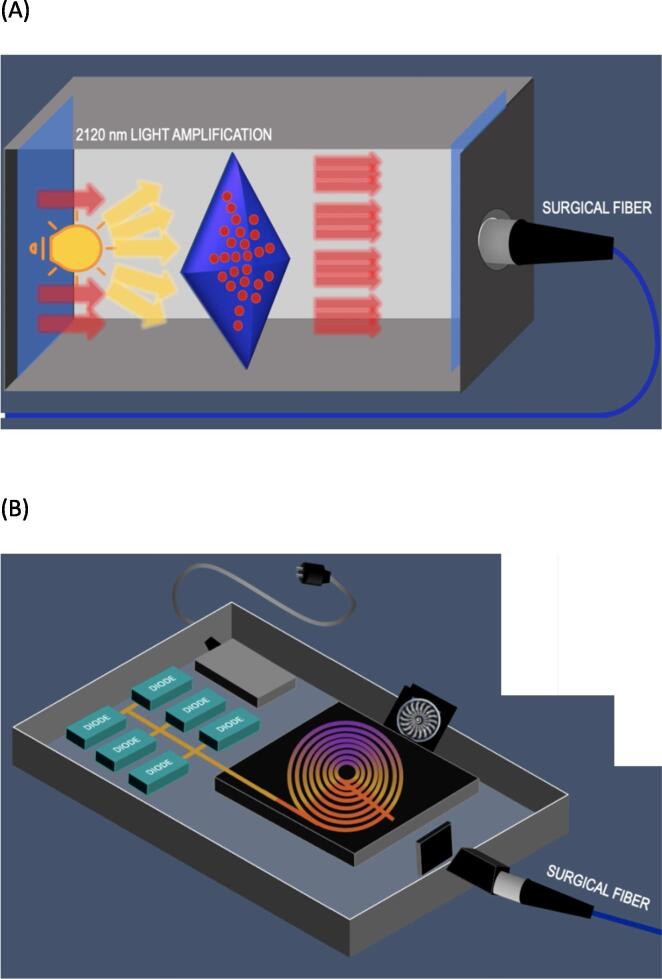
The TFL benefits are endless. These semiconductor devices work by converting electrical energy to optical energy, which is then used to excite thulium ions. Laser diodes have several advantages over flash lamps; in particular, there is lower energy loss in the form of heat and, as there are almost no moving parts, a simple air-cooling system is sufficient (Fig. 1). The apparatus weighs 30 kg, making it compact, portable, and space-saving. The portability is further enhanced by use of a standard power outlet (220–240 V), which reduces the cost of installing specialized high-amperage systems. In addition, minimal noise is produced. Furthermore, the device can convert electrical energy into optical energy at a rate of approximately 12%, while Ho:YAG has a conversion rate of approximately 1–2%. The lifetime of laser diodes is very long (often exceeding 10 000 h) and there are no lenses or mirrors with potential for contamination or and misalignment. Considering this, it is only logical to conclude that maintenance costs should be low [1].
Fig. 1.
(A) Schematic representation of a holmium:YAG laser low-power generator. Low-power generators consist of a single laser cavity (gray box) that emits its laser beam (red) in line with the output connector and the proximal end of the laser fiber (blue). (B) Schematic representation of a thulium fiber laser. Laser pumping is achieved via electronically modulating diode lasers (green boxes). A thulium-doped, 10–30-m-long silica fiber with a core diameter of 10–20 μm is used as the gain medium for generation of the laser beam. The uniform laser beam at the output connector allows the use of laser fibers as small as 50 μm (blue).
To date, the only TFL weakness is identification of the optimal settings. Pulse energy can range from 0.025 to 6 J and the pulse frequency can reach 2400 Hz, with peak power of 500 W and average power of 2–60 W. In addition, a short or long pulse duration (200 μs–50 ms) can be chosen [1]. These characteristics largely surpass those of the Ho:YAG technology. Some authors have attempted to clinically determine the best lithotripsy settings for ureteroscopy. However, the optimal laser settings are far from being established yet and further studies are needed [9].
So far, it has been demonstrated that TFL is a safe alternative to Ho:YAG lasers. Many of the above TFL advantages (significantly higher efficiency, faster ablation speed, less retropulsion, smaller fragments, and shorter operating time) contribute to reducing patient morbidity and complications [3]. TFL does not cause a greater rise in temperature during lithotripsy in comparison to Ho:YAG laser, even though water absorption of energy is lower with the latter [3]. Furthermore, TFL is safe for the operator given the fact that it does not cause eye lesions as long as the surgeon uses safety eyeglasses [10].
Conflicts of interest: Olivier Traxer is a consultant for Boston Scientific, Coloplast, EMS, IPG, Quanta, and Rocamed outside the scope of this manuscript. Alba Sierra and Mariela Corrales have nothing to disclose.
Associate Editor: Silvia Proietti
References
- 1.Kronenberg P., Traxer O. The laser of the future: reality and expectations about the new thulium fiber laser—a systematic review. Transl Androl Urol. 2019;8(Suppl 4):S398–S417. doi: 10.21037/tau.2019.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keller E.X., De Coninck V., Doizi S., Daudon M., Traxer O. Thulium fiber laser: ready to dust all urinary stone composition types? World J Urol. 2021;39:1693–1698. doi: 10.1007/s00345-020-03217-9. [DOI] [PubMed] [Google Scholar]
- 3.Traxer O., Corrales M. Managing urolithiasis with thulium fiber laser: updated real-life results—a systematic review. J Clin Med. 2021;10:3390. doi: 10.3390/jcm10153390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahajan A.D., Mahajan S.A. Thulium fiber laser versus holmium:yttrium aluminum garnet laser for stone lithotripsy during mini-percutaneous nephrolithotomy: a prospective randomized trial. Indian J Urol. 2022;38:42–47. doi: 10.4103/iju.iju_331_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ulvik Ø, Sørstrand Æsøy M, Juliebø-Jones P, Gjengstø P, Beisland C. Thulium fibre laser versus holmium:YAG for ureteroscopic lithotripsy: outcomes from a prospective randomised clinical trial. Eur Urol. In press. 10.1016/j.eururo.2022.02.027. [DOI] [PubMed]
- 6.Ventimiglia E., Doizi S., Kovalenko A., Andreeva V., Traxer O. Effect of temporal pulse shape on urinary stone phantom retropulsion rate and ablation efficiency using holmium:YAG and super-pulse thulium fibre lasers. BJU Int. 2020;126:159–167. doi: 10.1111/bju.15079. [DOI] [PubMed] [Google Scholar]
- 7.Ventimiglia E., Villa L., Doizi S., et al. Laser lithotripsy: the importance of peak power and pulse modulation. Eur Urol Focus. 2021;7:22–25. doi: 10.1016/j.euf.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 8.Germain T., Berthe L., Panthier F., Gorny C., Traxer O., Doizi S. Assessment of factors involved in laser fiber degradation with thulium fiber laser. J Endourol. 2022;36:668–673. doi: 10.1089/end.2021.0387. [DOI] [PubMed] [Google Scholar]
- 9.Sierra A, Corrales M, Piñero A, Traxer O. Thulium fiber laser pre-settings during ureterorenoscopy: Twitter’s experts’ recommendations. World J Urol. In press. 10.1007/s00345-022-03966-9. [DOI] [PubMed]
- 10.Panthier F, Chiron P, Gorny C, Berthe L, Doizi S, Corrales M, Traxer O. Laser-induced ocular lesions with thulium fiber laser in endourology: an ex vivo study. J Endourol. In press. 10.1089/end.2021.0948. [DOI] [PubMed]