Out-of-hospital cardiac arrest (OHCA) is one of the three leading causes of death in industrialized countries.[1,2] Some studies have described the impact of the first COVID-19 pandemic wave in terms of the number of cases and OHCA survival rates in various regions,[3-5] but few have addressed the relationship between the successive phases and how they affected OHCA.[6,7] The 14-d cumulative incidence peaked at more than 990 cases, with these rates remaining above 200 for an eight-month period between 15 March 2020 and 15 March 2021 in Madrid, Spain.
The objectives of the current study were twofold. First, we sought to describe how the different waves in the first pandemic year affected the healthcare activity of the Spanish emergency medical services (EMS). Second, we compared effects of the pandemic year on OHCA care to those of the preceding non-pandemic year in terms of initiating cardiopulmonary resuscitation and survival in a community with a high incidence of COVID-19.
METHODS
This was a retrospective study based on a continuous OHCA registry of the EMS Servicio de Urgencia Médica de la Comunidad de Madrid (SUMMA 112) in Spain. The registry collected all variables according to the definitions of the Utstein style,[8] and neurological status was defined according to the Cerebral Performance Categories scale.[9]
The study period was from 15 March 2019 to 14 March 2021. The data were divided into a non-pandemic period (NPP) from 15 March 2019 to 14 March 2020 and a pandemic period (PP) from 15 March 2020 to 14 March 2021. The PP was further divided into four sub-periods according to the 14-d cumulative incidence. All patients with OHCA who were treated with SUMMA 112 during the study period were included in our analysis.
Patients were categorized into one of the above-described periods according to the date of their OHCA onset.
Quantitative data are described using medians and interquartile ranges (IQRs), and qualitative data are described with number and percentage values. Comparative analyses were performed using Pearson’s Chi-square test or Fisher’s exact test for qualitative variables and the Wilcoxon test for quantitative variables. Differences were considered statistically significant when the P-value was less than 0.05. All statistical analyses were performed using R software v 4.1.
RESULTS
General characteristics of patients in the NPP and PP
During the PP, there were 1,743 patients with OHCA, compared with 1,781 patients during the NPP. The general characteristics of the patients included in both periods were shown in Table 1.
Table 1.
General characteristics of patients included in the NPP and PP
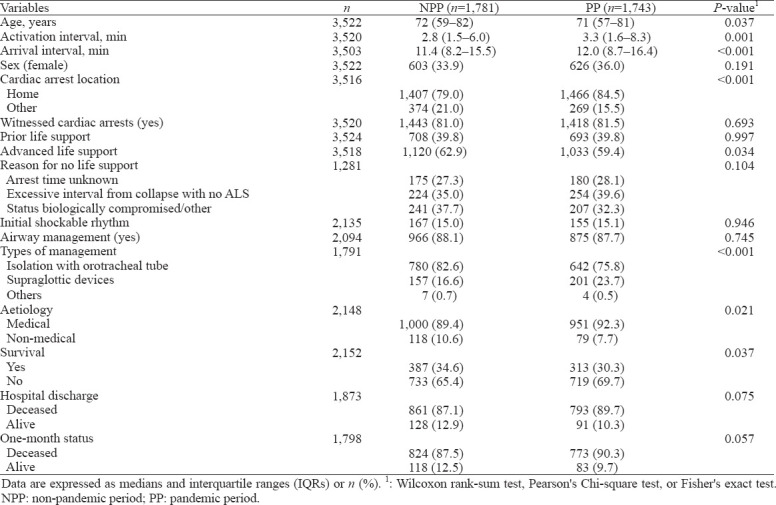
Compared with NPP, more OHCAs occurred at home during the PP (79.0% vs. 84.5%; P<0.001). There were no significant differences in the percentage of witnessed cardiac arrests (1,443 [81.0%] during NPP vs. 1,418 [81.5%] during PP; P=0.693) or resuscitation attempts prior to EMS arrival (708 [39.8%] during NPP vs. 693 [39.8%] during PP; P=0.997).
Compared with NPP, the percentage of advanced life support (ALS) attempts compared to the total number of OHCAs attended was lower during PP (62.9% during NPP vs. 59.4% during PP; P=0.034), although the percentage of shockable rhythms did not differ significantly (167 [15.0%] vs. 155 [15.1%]; P=0.946).
Survival on arrival at the hospital decreased significantly during the PP (387 [34.6%] during NPP vs. 313 [30.3%] during PP; P=0.037). When analyzing the status of patients at hospital arrival, the percentage who arrived with recovery of spontaneous circulation (ROSC) decreased during the pandemic (348 [31.1%] during NPP vs. 262 [25.4%] during PP).
General characteristics of patients in the different waves
The influence of different waves of the pandemic (three waves and one plateau period after the first wave) on OHCA care was shown in Table 2.
Table 2.
General characteristics of patients included in the different waves
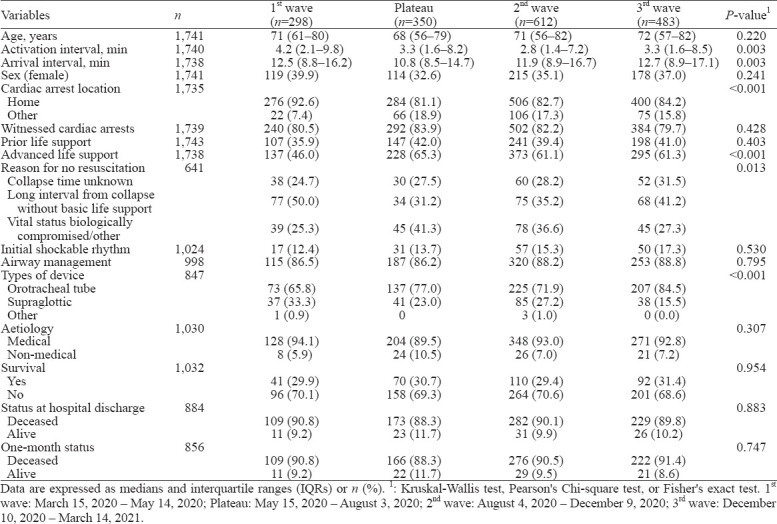
During the first wave, the proportion of resuscitation attempts was significantly lower than that during the other waves: 46.0% during the first wave vs. 65.3% during the plateau, 61.1% during the second wave, and 61.3% during the third wave (P<0.001). There was no significant difference when comparing the percentage of shockable rhythms (P=0.530) or whether the airway was managed (P=0.795). Significant differences were found when comparing the type of airway management, with supraglottic airway devices used more in the first wave (33.3%) compared to the plateau period (23.0%) and the second (27.2%) and third waves (15.5%; P<0.001), respectively.
In all three waves, there was a significant increase in the number of calls received at the dispatch centre compared to the NPP. Most calls were notably during the first wave. This work overload was assumed in the dispatch centre itself without increasing the mobilization of resources for face-to-face patient care (supplementary Figure 1).
DISCUSSION
The resuscitation attempt rates decreased significantly during the first pandemic wave, as reported in other studies,[3,10-12] but we also found that they recovered to non-pandemic levels during the remainder of the PP. The greatest pressure and work overload were experienced in the dispatch center, with a very significant increase in the number of calls without significant changes in the mobilization of resources.
The most common reason for non-resuscitation was the longer interval time in arrival of the EMS. During the PP, the aetiology of OHCA was most frequently medical, as other researchers have reported.[3,11,12]
We found no significant differences in whether the airway was managed, but our study and other studies have indicated that supraglottic airway management devices were more commonly used during the PP, a pattern that changed over time.[4,13,14]
OHCA survival at hospital admission was significantly reduced, as previously described in other studies.[3,4,10-12,13-18] One prediction might have been that as the first wave ended and COVID-19 incidence fell, the survival rate would have improved; however, it remained low, with no significant changes during the successive waves.
When comparing survival at the time of hospital discharge and comparing one-month survival rates, we found no significant differences between the NPP and PP, but there was a trend towards worse survival during the pandemic. We also found no significant differences in these outcomes among the different periods of the pandemic.
The results of this study highlight the influence that COVID-19 has had on OHCA and on EMS activity, showing how the pandemic has increased stress on the Emergency Coordination Centre in terms of attending the population. In the community of Madrid, as in Nantes[19] and Lausanne,[20] the number of calls increased during the first pandemic wave, whereas some studies in other regions showed that the number of calls actually decreased.[10,21] In Madrid, the increased number of EMS calls continued through successive waves, and this overload led to a delay in activation time for available resources throughout the PP. In some regions where the calls decreased, activations often decreased as well.[10,22] In other places, however, despite an increased number of calls, resource dispatches decreased[19] or remained the same, as in Madrid,[23] with a similar pattern occurring during subsequent waves. One possible inference is that at the time of high call volume, the various call handling systems significantly influenced how both resource dispatch and response time were handled, as Penverne et al[19] demonstrated.
CONCLUSIONS
The different waves of the pandemic variably affected OHCA care. Survival from OHCA has decreased since the onset of the pandemic and has not recovered since then. The number of calls to EMS increases as artificial intelligence increases, although the number of mobilizations does not.
Footnotes
Funding: None.
Ethical approval: The OHSCAR registry has been approved by ethics committees in Northwestern Malaga, Aragon, Cáceres, Navarra, and the Basque Country.
Conflicts of interests: The authors declare that they have no competing interests.
Contributors: JMNP and DMM designed the study. JMNP, AMR, and CAB coordinated the study and verified the data. DMM and FNS performed and supervised the statistical analysis. MJGL and BMI participated in the literature search. FNS and MJGL participated in data analysis and table and figure design. JMNP, MJGL, BMI, ACM, YMC, and JLG contributed to the development of the study and the data collection. All authors critically reviewed and approved the final version. All authors had full access to all study data and took the ultimate responsibility for the decision to submit this paper for publication.
All the supplementary files in this paper are available at http://wjem.com.cn.
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update:a report from the American Heart Association. Circulation. 2019;139(10):e56–528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Gräsner JT, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I, et al. Survival after out-of-hospital cardiac arrest in Europe:results of the EuReCa TWO study. Resuscitation. 2020;148:218–26. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 3.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. COVID-19 kills at home:the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41(32):3045–54. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai PH, Lancet EA, Weiden MD, Webber MP, Zeig-Owens R, Hall CB, et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5(10):1154–63. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kudo T, Lahey R, Hirschfeld CB, Williams MC, Lu B, Alasnag M, et al. Impact of COVID-19 pandemic on cardiovascular testing in Asia:the IAEA INCAPS-COVID study. JACC:Asia. 2021;1(2):187–99. doi: 10.1016/j.jacasi.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E, Primi R, Gentile FR, Mare C, Centineo P, et al. All the Lombardia CARe researchers. Out-of-hospital cardiac arrest incidence in the different phases of COVID-19 outbreak. Resuscitation. 2021;159:115–6. doi: 10.1016/j.resuscitation.2020.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sultanian P, Lundgren P, Strömsöe A, Aune S, Bergström G, Hagberg E, et al. Cardiac arrest in COVID-19:characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J. 2021;42(11):1094–106. doi: 10.1093/eurheartj/ehaa1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports:update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest:a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia);and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132(13):1286–300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 9.Rosell-ortiz F, Escalada-roig X, Fernández del Valle P, Sánchez-santos L, Navalpotro-Pascual JM, Echarri-sucunza A, et al. Out-of-hospital cardiac arrest (OHCA) attended by mobile emergency teams with a physician on board. Results of the Spanish OHCA Registry (OSHCAR) Resuscitation. 2017;113:90–5. doi: 10.1016/j.resuscitation.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 10.Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage:hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–63. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fothergill RT, Smith AL, Wrigley F, Perkins GD. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc Plus. 2021;5:100066. doi: 10.1016/j.resplu.2020.100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Treatment of out-of-hospital cardiac arrest in the COVID-19 era:a 100 days experience from the Lombardy region. PLoS One. 2020;15(10):e0241028. doi: 10.1371/journal.pone.0241028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishiyama C, Kiyohara K, Iwami T, Hayashida S, Kiguchi T, Matsuyama T, et al. Influence of COVID-19 pandemic on bystander interventions, emergency medical service activities, and patient outcomes in out-of-hospital cardiac arrest in Osaka City, Japan. Resusc Plus. 2021;5:100088. doi: 10.1016/j.resplu.2021.100088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosell Ortiz F, Fernández del Valle P, Knox EC, Jiménez Fábrega X, Navalpotro-Pascual JM, Mateo Rodríguez I, et al. Influence of the COVID- 19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230–40. doi: 10.1016/j.resuscitation.2020.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France:a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Out-of-hospital cardiac arrest during the covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–8. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim SL, Shahidah N, Saffari SE, Ng QX, Ho AFW, Leong BS, et al. Impact of COVID-19 on out-of-hospital cardiac arrest in Singapore. Int J Environ Res Public Health. 2021;18(7):3646. doi: 10.3390/ijerph18073646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021;6(3):296–303. doi: 10.1001/jamacardio.2020.6210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penverne Y, Leclere B, Labady J, Berthier F, Jenvrin J, Javaudin F, et al. Impact of two-level filtering on emergency medical communication center triage during the COVID-19 pandemic:an uncontrolled before-after study. Scand J Trauma Resusc Emerg Med. 2020;28(1):80. doi: 10.1186/s13049-020-00775-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dami F, Berthoz V. Lausanne medical dispatch centre's response to COVID-19. Scand J Trauma Resusc Emerg Med. 2020;28(1):37. doi: 10.1186/s13049-020-00735-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lerner EB, Newgard CD, Mann NC. Effect of the coronavirus disease 2019 (COVID-19) pandemic on the US emergency medical services system:a preliminary report. Acad Emerg Med. 2020;27(8):693–9. doi: 10.1111/acem.14051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kovach CP, Perman SM. Impact of the COVID-19 pandemic on cardiac arrest systems of care. Curr Opin Crit Care. 2021;27(3):239–45. doi: 10.1097/MCC.0000000000000817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Navalpotro-Pascual JM, Fernández Pérez C, Peinado Vallejo FA, Carrillo Moya A, Muñecas Cuesta Y, Muñoz Isabel B, et al. Caseload and cardiopulmonary arrest management by an out-of-hospital emergency service during the COVID-19 pandemic. Emergencias. 2021;33(2):100–6. [PubMed] [Google Scholar]


