Abstract
Introduction
A booster dose of messenger RNA vaccine protects against severe COVID-19 outcomes. This study examined the incidence of COVID-19 booster vaccination among active-duty U.S. military servicemembers between August 2021 and January 2022, factors associated with vaccination uptake, and trends over time.
Methods
This was a retrospective cohort study of active-duty military personnel using data from the Defense Medical Surveillance System. Participants were included if they served in the active component from August 2021 through January 2022 and were eligible to receive a COVID-19 booster dose by January 2022. Adjusted hazard ratio estimates of time to booster vaccination were calculated using Cox proportional hazards regression.
Results
Lower booster vaccine uptake was seen in the U.S. military (25%) than among the general U.S. population at the same time (45%). Booster vaccination increased with older age, with greater education, with higher income, among women, and among those stationed overseas; it decreased with previous COVID-19 infection and use of the Janssen vaccine. There were no significant racial or ethnic disparities in booster vaccination.
Conclusions
In the absence of a compulsory vaccination policy, lower booster vaccine uptake was seen among servicemembers than among the general U.S. population, particularly among members who were younger, were male, Marines, and had a previous history of infection. Low vaccination rates not only increase the risk of acute and long-term health effects from COVID-19 among servicemembers, but they also degrade the overall readiness of the U.S. military.
INTRODUCTION
People who complete a primary series of messenger RNA (mRNA) coronavirus disease 2019 (COVID-19) vaccine, followed by a booster dose, have better protection against severe adverse outcomes than do people who only receive the primary series.1 , 2 U.S. military personnel are required to receive the primary COVID-19 vaccination series, and an assessment of the effectiveness of the Department of Defense's distribution plan has been published.3 Booster doses of COVID-19 vaccine are recommended but not required for U.S. military personnel, so they are available to them on a strictly voluntary basis.4 This study examined the incidence of COVID-19 booster vaccination among U.S. military servicemembers between August 2021 and January 2022, factors associated with vaccination, and trends over time.
METHODS
This was a retrospective cohort study of the Active Component military personnel using data from the Defense Medical Surveillance System5; Reserve and National Guard members were excluded. Participants were included if they served from August 2021 through January 2022 and were eligible to receive a COVID-19 booster dose by January 2022. Servicemembers were defined as being eligible to receive the booster dose on the date that was 150 days after completing a 2-dose initial mRNA series or 60 days after receiving 1 dose of the Janssen vaccine. The percentages of those who received a booster dose were described and stratified by demographic and clinical characteristics, including having a recent medical encounter for a comorbid condition,6 and previous infection with COVID-19. Comorbid conditions were defined as in a previous study, but the authors further inspected some individual conditions of interest, such as mental health conditions and pregnancy.7
Time-to-event analyses were used to both assess delays in vaccination and to ensure valid comparisons of time at-risk. For these analyses, the start date was defined as the date the service member became eligible to be boosted or the start of the surveillance period on August 1, 2021, whichever came last. Adjusted hazard ratio (AHR) estimates were calculated using Cox proportional hazards regression. All analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC). The study was approved by the Uniformed Services University IRB.t
RESULTS
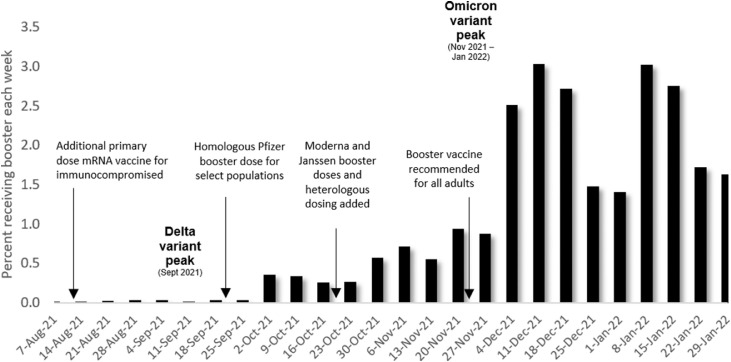
Among 1,340,712 members in service during August 2021, 980,963 (73.2%) were eligible for voluntary booster vaccination by January 31, 2022. Of these, 248,125 (25.3%) received a booster dose. Most personnel received an mRNA vaccine for both the primary series (n=856,652, 87.3%) and the booster (n=226,844, 91.4%). The incidence of booster vaccination uptake increased dramatically after the Centers for Disease Control and Prevention recommended universal adult booster vaccination (Figure 1 ). Uptake then decreased in late December and then increased again in early January 2022, concurrent with the emergence of the Omicron variant.
Figure 1.
COVID-19 booster vaccine uptake among eligible active-duty military service members, by week.
Aug, August; Dec, December; Jan, January; Nov, November; Oct, October; Sept, September.
As seen in Table 1 , the crude incidence of booster uptake among women was greater than among men and was highest in the oldest age group (≥45 years). Uptake was substantially reduced among servicemembers with a history of previous COVID-19 infection (14.1%) compared with uptake among those without previous infection (27.9%). Booster uptake was similar among different racial groups but varied by military service, with the lowest uptake in the Marine Corps and highest in the Air Force. In the adjusted analysis, servicemembers with previous COVID-19 infection had a substantially reduced adjusted incidence of booster vaccination (AHR=0.54; 95% CI=0.54, 0.55), whereas the association with comorbid diagnoses was minimal (AHR=0.97; 95% CI=0.96, 0.98). Interestingly, previous immunization with Janssen compared with immunization with an mRNA vaccine was also strongly associated with decreased booster uptake (AHR=0.43; 95% CI=0.42, 0.43). An increased rate of booster vaccination was seen among servicemembers who were female, were aged ≥30 years, were non-Hispanic Blacks and Hispanics, were officers, had higher education levels, were married, were employed in select occupations, and were stationed at overseas locations (AHR=2.11; 95% CI=2.09, 2.14).
Table 1.
COVID-19 Booster Uptake Among Eligible Active-Duty Service members, August 1, 2021–January 31, 2022
| Variables | Booster eligible | Number boosted | Percent boosted | Adjusteda hazard rate ratio (95% CI) |
|---|---|---|---|---|
| Full immunization type | ||||
| mRNA vaccine | 856,652 | 226,844 | 26.5 | ref |
| Janssen vaccine | 124,311 | 21,281 | 17.1 | 0.43 (0.42, 0.43) |
| Sex | ||||
| Male | 814,148 | 199,171 | 24.5 | ref |
| Female | 166,815 | 48,954 | 29.3 | 1.18 (1.17, 1.19) |
| Age, years | ||||
| <20 | 62,618 | 6,124 | 9.8 | ref |
| 20–24 | 287,599 | 42,627 | 14.8 | 0.80 (0.78, 0.82) |
| 25–29 | 223,136 | 48,910 | 21.9 | 0.91 (0.89, 0.94) |
| 30–34 | 164,151 | 48,547 | 29.6 | 1.11 (1.08, 1.14) |
| 35–39 | 131,193 | 47,941 | 36.5 | 1.29 (1.25, 1.33) |
| 40–44 | 69,589 | 30,814 | 44.3 | 1.44 (1.39, 1.48) |
| ≥45 | 42,677 | 23,162 | 54.3 | 1.63 (1.57, 1.68) |
| Race and ethnicity | ||||
| Non-Hispanic White | 543,194 | 138,625 | 25.5 | ref |
| Non-Hispanic Black | 142,189 | 33,573 | 23.6 | 1.07 (1.06, 1.09) |
| Hispanic | 173,067 | 38,539 | 22.3 | 1.08 (1.06, 1.09) |
| Other/unknown | 122,513 | 37,388 | 30.5 | 1.13 (1.11, 1.14) |
| Service | ||||
| Army | 360,335 | 84,365 | 23.4 | ref |
| Navy | 283,573 | 82,769 | 29.2 | 1.03 (1.02, 1.04) |
| Air Force | 221,011 | 66,073 | 29.9 | 1.03 (1.01, 1.04) |
| Marines | 116,044 | 14,918 | 12.9 | 0.54 (0.53, 0.55) |
| Rank | ||||
| Enlisted | 771,209 | 155,286 | 20.1 | ref |
| Officer | 209,754 | 92,839 | 44.3 | 1.34 (1.33, 1.36) |
| Education level | ||||
| High school or less | 573,530 | 94,416 | 16.5 | ref |
| Some college | 120,555 | 33,901 | 28.1 | 1.16 (1.14, 1.18) |
| Bachelor's or advanced degree | 265,400 | 111,702 | 42.1 | 1.41 (1.39, 1.43) |
| Other/unknown | 21,478 | 8,106 | 37.7 | 1.29 (1.26, 1.32) |
| Marital status | ||||
| Single, never married | 426,087 | 81,302 | 19.1 | ref |
| Married | 505,292 | 153,069 | 30.3 | 1.02 (1.01, 1.03) |
| Other/unknown | 49,584 | 13,754 | 27.7 | 0.94 (0.92, 0.96) |
| Geographic region | ||||
| Northeast | 30,272 | 9,031 | 29.8 | 1.23 (1.20, 1.26) |
| Midwest | 57,879 | 11,438 | 19.8 | 0.84 (0.82, 0.96) |
| South | 427,955 | 96,149 | 22.5 | ref |
| West | 248,559 | 47,741 | 19.2 | 0.79 (0.78, 0.79) |
| Overseas | 126,105 | 57,379 | 45.5 | 2.11 (2.09, 2.14) |
| Other/unknown | 90,193 | 26,387 | 29.3 | 1.21 (1.19, 1.23) |
| Occupation | ||||
| Combat related | 140,440 | 26,029 | 18.5 | ref |
| Motor transport | 27,722 | 4,545 | 16.4 | 1.08 (1.04, 1.11) |
| Pilot/aircrew | 40,494 | 15,297 | 37.8 | 1.08 (1.06, 1.10) |
| Repair/engineering | 286,356 | 62,770 | 21.9 | 1.11 (1.10, 1.13) |
| Communications/intelligence | 212,475 | 56,545 | 26.6 | 1.28 (1.26, 1.30) |
| Health care | 91,364 | 36,339 | 39.8 | 1.23 (1.21, 1.25) |
| Other/unknown | 182,112 | 46,600 | 25.6 | 1.15 (1.13, 1.17) |
| Comorbidity diagnosis before booster | ||||
| Any comorbidity | 299,129 | 84,183 | 28.1 | 0.97 (0.96, 0.98) |
| No comorbidity | 681,834 | 163,942 | 24.0 | ref |
| Previous infection | ||||
| COVID-19 infection before booster | 186,016 | 26,183 | 14.1 | 0.54 (0.54, 0.55) |
| No COVID-19 infection before booster | 794,947 | 221,942 | 27.9 | ref |
Model adjusted for all variables in the table (i.e., age, sex, race and ethnicity, rank, service, education level, geographic region, occupation, marital status, previous comorbidities, previous SARS-CoV-2 infection, and full immunization type).
mRNA, messenger RNA; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DISCUSSION
This report characterizes the initial months of COVID-19 booster vaccine uptake among a population of active-duty U.S. military servicemembers who had received a mandatory primary vaccination series. No other military forces have published comparable vaccine uptake data. Voluntary uptake of the booster vaccine was low (25%) compared with uptake among the general U.S. population (45%) at the same time.8 This difference may be partially attributable to the younger ages and better health status of the military population. As seen in a previous military study of COVID-19 vaccine initiation, increasing age, greater education levels, and higher rank (a proxy for income) were associated with increased rates of COVID-19 booster vaccination after adjusting for other factors7 and mirror early trends seen in the general U.S. population. Also consistent with primary vaccination in the U.S. military, previous comorbidity diagnoses were not strongly associated with booster vaccination rates after adjustment for other covariates.
In contrast, racial and ethnic disparities in booster vaccination seen in the older U.S. population were not seen in the military,9 despite such disparities having been shown with the primary vaccination series.7 In addition, female servicemembers had higher booster vaccine rates than males, in contrast to the 10% lower likelihood of primary vaccination previously seen among females.7 Previous infection with COVID-19 had a stronger association with not receiving a booster vaccine (AHR=0.54) than it did with the primary vaccine series (adjusted risk ratio=0.80). This may be owing to perceptions of being less at-risk owing to perceived partial or full immunity from previous infection, decreased vaccine confidence, or other factors. Conversely, the higher rate of booster vaccination among those serving overseas may be owing to a heightened perception of infection risk, earlier distribution and availability at these locations because of military requirements, or other factors. Overseas officials have also suggested that beneficiaries relied more on Department of Defense facilities overseas owing to vaccine unavailability through the host nations.3
Limitations
This study was limited by the fact that not all servicemembers were recommended for booster vaccination until November 22, 2021, several months after the start of the surveillance period. Therefore, servicemembers who were eligible for booster vaccination earlier in the study period may have differed from those who became eligible later. Vaccine uptake in the communities surrounding military installations was unavailable, but it may have influenced behavior among military beneficiaries. In addition, there were many complex individual, interpersonal, military, and societal factors influencing access to and willingness to receive this voluntary vaccination that were not measured in this study.
CONCLUSIONS
The findings from this study show that in the absence of a compulsory vaccination policy, lower COVID-19 booster vaccine uptake was seen among servicemembers than among the general U.S. population, particularly among members who were younger, were male, were Marines, and had a previous history of infection. Low vaccination rates not only increase the risk of acute and long-term health effects from COVID-19 among servicemembers, but they also degrade the overall readiness of the U.S. military. The low booster uptake found in this study suggests that public health messaging and outreach are needed across all populations to maximize the protection of military forces from COVID-19, and it also highlights that high levels of booster uptake are unlikely to be seen in military populations in the absence of a vaccination mandate. The findings of this study further suggest that those with previous COVID-19 infection may be key groups to receive targeted messaging campaigns. Further research efforts should be directed to effectively communicating with these groups.
Acknowledgments
ACKNOWLEDGMENTS
The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, assertions, opinions, or policies of the Uniformed Services University of the Health Sciences, the Department of Defense, or the U.S. Government.
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Erin L. Winkler: Methodology, Writing - original draft. Shauna L. Stahlman: Data curation, Methodology, Writing - review and editing. Natalie Y. Wells: Data curation, Methodology, Writing - review and editing. Aparna V. Chauhan: Data curation, Investigation, Methodology. Kayli M. Hiban: Data curation, Methodology, Writing - review and editing. Amy A. Costello: Methodology, Supervision, Writing - review and editing. James D. Mancuso: Conceptualization, Methodology, Supervision, Writing - review and editing.
REFERENCES
- 1.Tenforde MW, Patel MM, Gaglani M, et al. Effectiveness of a third dose of Pfizer-BioNTech and moderna vaccines in preventing COVID-19 hospitalization among immunocompetent and immunocompromised adults - United States, August-December 2021. MMWR Morb Mortal Wkly Rep. 2022;71(4):118–124. doi: 10.15585/mmwr.mm7104a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barda N, Dagan N, Cohen C, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398(10316):2093–2100. doi: 10.1016/S0140-6736(21)02249-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Defense Inspector General . Department of Defense Inspector General; Washington, DC: U.S: 2022. Audit of DoD Implementation of the DoD Coronavirus Disease-2019 Vaccine Distribution Plan.https://media.defense.gov/2022/Feb/03/2002932291/-1/-1/1/DODIG-2022-058.PDF Published February 2022. Accessed July 3, 2022. [Google Scholar]
- 4.Mbaeyi S, Oliver SE, Collins JP, et al. The Advisory Committee on Immunization Practices’ interim recommendations for additional primary and booster doses of COVID-19 vaccines - United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(44):1545–1552. doi: 10.15585/mmwr.mm7044e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubertone MV, Brundage JF. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002;92(12):1900–1904. doi: 10.2105/AJPH.92.12.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Updated September 2, 2022. Accessed September 9, 2022.
- 7.Lang MA, Stahlman S, Wells NY, et al. Disparities in COVID-19 vaccine initiation and completion among active component service members and health care personnel, 11 December 2020–12 March 2021. MSMR. 2021;28(4):2–9. https://health.mil/News/Articles/2021/04/01/Disparities-MSMR-2021 [PubMed] [Google Scholar]
- 8.COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total. Updated March 30, 2022. Accessed April 3, 2022.
- 9.Fast HE, Zell E, Murthy BP, et al. Booster and additional primary dose COVID-19 vaccinations among adults aged ≥65 years – United States, August 13, 2021-November 19, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(50):1735–1739. doi: 10.15585/mmwr.mm7050e2. [DOI] [PMC free article] [PubMed] [Google Scholar]