Abstract
OBJECTIVE:
Endometrial cancer (EC) is increasing in incidence and mortality rates, possibly due to the rising rates of obesity in the United States.1 The type I/II EC classification system was first proposed by Bokhman2 in 1983 following 20 years of personal observations among 366 women and established obesity as a classical risk factor for low-grade EC with a good prognosis. However, more recent pooled analyses suggest that the 2 types share many etiologic risk factors, including obesity.3 Given the increase in mortality as a consequence of high-risk EC, the relationship between obesity and uterine cancer, as proposed by Bohkman, may be oversimplified.4 This study aimed to analyze the trend of type I/II EC in the United States as it relates to obesity using national statistics.
STUDY DESIGN:
Data were obtained from the United States Cancer Statistics database and the Behavioral Risk Factors Surveillance System survey from 2001 to 2017. The incidence of uterine cancer, histologic type, obesity, and average annual percentage change (AAPC) were calculated using Joinpoint regression. Endometrial histology was classified according to traditional type I (endometrioid grade 1–3) and type II (serous, clear cell, carcinosarcoma) categories.
RESULTS:
Over this 17-year study period, 778,891 patients were diagnosed with uterine cancer. Overall, the rate of new uterine cancer cases increased by 0.82% annually (P<.005), leading to an incidence of 24.07 per 100,000 in 2001 as compared with 27.04 per 100,000 women in 2017. The incidence of type I EC remained stable (AAPC, 0.40; P=.061) with a stable incidence of grade I EC (AAPC, −0.48; P=.125) and a decreasing incidence of grade 2 and grade 3 EC (AAPC, −2.61 and −2.63, respectively; P<.001). Alternatively, the incidence of type II EC increased by 3.12% annually (P<.001), leading to an increase of 63% since 2001. Serous carcinoma increased by 4.88% annually (P<.001). Clear cell and carcinosarcoma also increased significantly (AAPC, 1.02 and 1.51, respectively; P<.05). For illustrative purposes, we calculated the percentage increase in the incidence of cancer types over the last 17 years in comparison with the year 2001 (Figure). Overall, the proportion of women with obesity also increased significantly from 19.5% to 27.5% during this period (AAPC, 1.5; P<.001).
CONCLUSION:
Utilizing 17 years of data from a national cancer registry, we demonstrated that the incidence of high-risk type II EC has increased, whereas the incidence of low-risk grade I EC has remained stable. In another survey study, we showed the rising incidence of obesity. These findings suggest that the traditional type I/II approach to classifying EC may be oversimplified, particularly as it relates to obesity. Recent studies utilizing The Cancer Genome Atlas classification for EC demonstrated an association between a mean body mass index (BMI) of ≥30 and each of the 4 clusters except for DNA polymerase epsilon gene ultramutated tumors. Furthermore, up-regulation of several genes known to play a role in EC pathogenesis were associated with BMI, suggesting that obesity may create a unique, proinflammatory microenvironment that affects tumor biology at a molecular level.5 Limitations of the current study include possible information reporting bias, lack of central pathology review, and limited ability to correlate data between multiple databases. Incidence rates are also not corrected for hysterectomy prevalence. However, these trends suggest a potential impact of obesity on the rising rates of type II EC that should be explored further.
FIGURE.
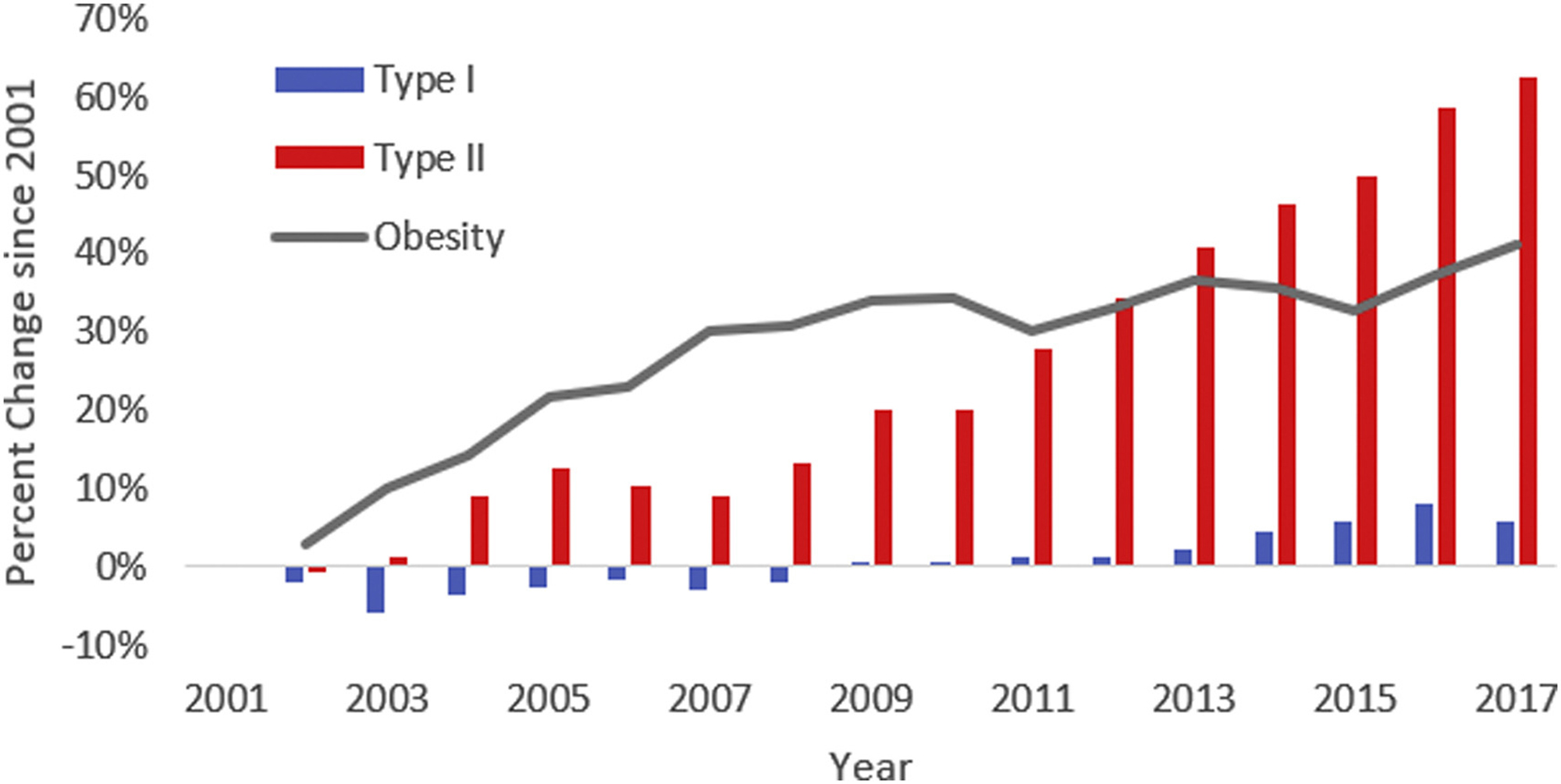
Trends in percent change in obesity and histologic type of uterine cancer
Footnotes
The authors report no conflict of interest.
Contributor Information
Cortney M. Eakin, Department of Obstetrics and Gynecology, University of California, Los Angeles, Los Angeles, CA.
Cheng-I Liao, Department of Obstetrics and Gynecology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan.
Ritu Salani, Department of Obstetrics and Gynecology, University of California, Los Angeles, Los Angeles, CA.
Joshua G. Cohen, Department of Obstetrics and Gynecology, University of California, Los Angeles, Los Angeles, CA.
Daniel S. Kapp, Department of Radiation Oncology, Stanford University, Stanford, CA.
John K. Chan, Division of Gynecologic Oncology, California Pacific Medical Center, Palo Alto Medical Foundation, Sutter Research Institute, 795 El Camino Real, Palo Alto, CA 94301.
REFERENCES
- 1.Giaquinto AN, Broaddus RR, Jemal A, Siegel RL. The changing landscape of gynecologic cancer mortality in the United States. Obstet Gynecol 2022;139:440–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 1983;15:10–7. [DOI] [PubMed] [Google Scholar]
- 3.Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol 2013;31:2607–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ueda SM, Kapp DS, Cheung MK, et al. Trends in demographic and clinical characteristics in women diagnosed with corpus cancer and their potential impact on the increasing number of deaths. Am J Obstet Gynecol 2008;198:218.e1–6. [DOI] [PubMed] [Google Scholar]
- 5.Roque DR, Makowski L, Chen TH, Rashid N, Hayes DN, Bae-Jump V. Association between differential gene expression and body mass index among endometrial cancers from the Cancer Genome Atlas Project. Gynecol Oncol 2016;142:317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]


