Abstract
Background
Vaccine hesitancy affects immunization programs worldwide and can impact vaccine coverage and fight against Coronavirus disease 2019 (COVID-19) too.
Objectives
Primary objectives: To find out the magnitude of COVID-19 vaccine hesitancy among the Health Care Worker Parents (HCWPs), the reasons for vaccine hesitancy, and their perceptions regarding COVID-19 vaccination of their children. Secondary objective: To analyze the clinic-socio-demographic correlates of COVID-19 vaccine hesitancy among HCWPs.
Methods
This was a cross sectional descriptive study. Health care workers who are parents were invited to participate in the study. Details about COVID vaccination status, COVID-19 illness of HCWPS and family members and its outcomes , reasons for not getting vaccinated, willingness to vaccinate their children, reasons for not willing to vaccinate their children, their responses to vaccine hesitancy survey (VHS) questionnaire and Modified Oxford COVID-19 vaccine hesitancy scale (MOVHS) were collected and analyzed using descriptive statistics.
Results
A total of 269 HCWPs participated in the study. Of the HCWPs, 97% had completed their COVID-19 vaccination schedule. Majority stated that they would vaccinate their children when it is available. Although majority of the responses were positive or towards agreement, there were some striking variations in the responses among some sections of HCWPs. Positive responses to the questionnaire were associated with higher self-vaccination and a decision to vaccinate their children.
Conclusion
Vaccine hesitancy was less common among HCWPs in our study. A section of the HCWPs might be disproportionately more hesitant than others. Majority were in favor of vaccinating their children.
Keywords: COVID-19, Vaccination, Health Care Workers, Hesitancy, Children
1. Introduction
Globally there have been more than 584 million cases of COVID-19 recorded and more than 6 million deaths as on 10th August 2022 and more than 12 billion doses of COVID-19 vaccine have been administered as on 8th August 2022. [1] India accounted for more than 44 million cases and over 500,000 deaths as on 10th August 2022. [1]Significant herd immunity in the community is needed to control the pandemic and the only way to safely attain it is through mass vaccination. [2] However, recent studies have shown that vaccine hesitancy in the community is one of the significant hindering factors for inadequate vaccination. [3], [4], [5] Health care workers (HCW) have the unique opportunity of being role models in the vaccination efforts and can spearhead the vaccination drive so that vaccination uptake increases even among the general population. However, it has been reported that even HCWs have vaccine hesitancy to the tune of 22.51 % out of 76,471 HCWs which can compromise their protection and that of their family members. [6] This hesitancy can be a result of a lack of trust, misinformation from social media, alternate beliefs, and experiences of adverse events during previous vaccination. [7] It is not known to what extent vaccine hesitancy is prevalent among HCWs in India and how it affects their family members, especially their children. Therefore, we aimed to describe the vaccine hesitancy for COVID-19 vaccine among HCWPs of a tertiary care institute in Puducherry, India. The primary objectives of our study are to find out the magnitude of COVID-19 vaccine hesitancy among the Health Care Worker Parents (HCWPs), the reasons for vaccine hesitancy, and to study their perceptions regarding COVID-19 vaccination of their children. The secondary objective is to analyze the clinic-socio-demographic correlates of COVID-19 vaccine hesitancy among HCWPs.
2. Methodology:
This was a cross sectional descriptive part of a mixed methods study involving health care workers who are also parents. For the purpose of this study, we have defined health care worker as any person (doctors, nurses, pharmacists, dieticians, lab technicians, OT technicians/assistants, ward attendants, sanitary workers, etc.) whose activities involve contact with patients or with body fluid of patients in a health care or laboratory setting. The definition of health care worker has been adapted from Centre for Disease Control and Prevention‘s “Public Health Service Guidelines for the Management of Health Care Worker Exposures to HIV and Recommendations for Post Exposure Prophylaxis” (MMWR 1998, Vol 47, RR-7). We have defined Health Care Worker-Parent(s) as those HCW who have a living child or children.
Assuming the proportion of health care workers with vaccine hesitancy to be 30 % based on published literature with 5 % absolute precision and 95 % confidence level, the required sample size would be 270. [8], [9] Sample size calculated from openepi.com. Depending on the proportion of doctors, nurses, and other health care workers, an equivalent proportion of HCWPs were recruited to make up the sample size as per convenience. Informed written consent was obtained from the participants. The study was approved by our Institute‘s scientific advisory committee and ethics committee for human studies (JIP/IEC/2021/270). Information pertaining to socio demographics including age, sex, religion, number of family members in the household, nature of their residence, and socioeconomic status, was collected. For the purpose of our study we have defined vaccine hesitancy as delay in acceptance or refusal of vaccination despite the availability of vaccination service. [10] Vaccination service was available at the health facility itself on all days of the week free of cost.
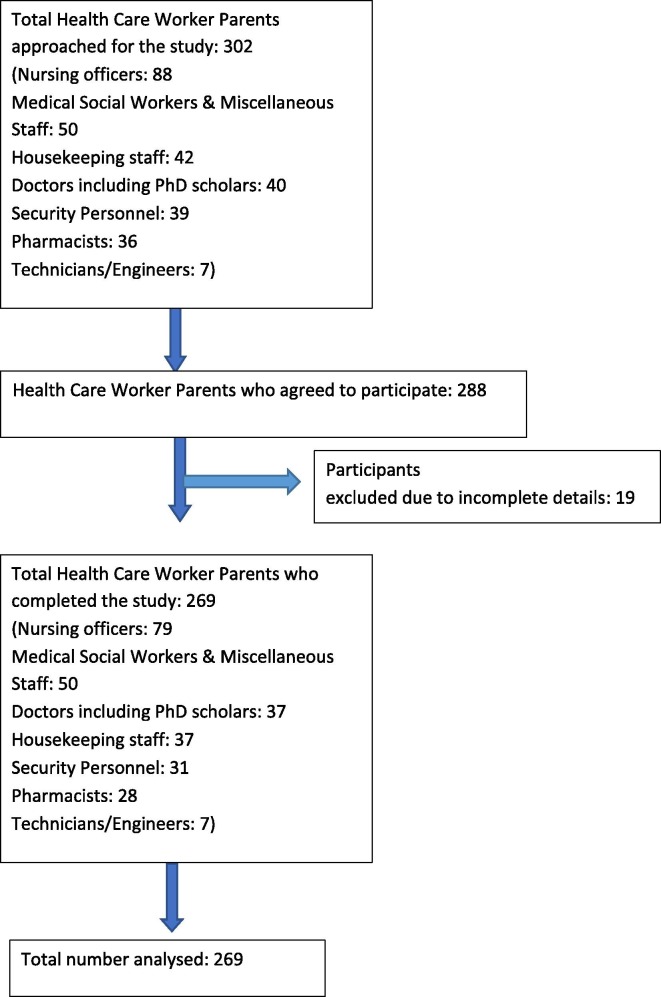
To assess vaccine hesitancy, a ten point validated vaccine hesitancy survey (VHS) questionnaire, developed by the SAGE working group of the World Health Organization and validated in a real world setting was used. [11], [12] Other set of questions in the form of investigator administered proforma was used to collect data regarding the inherent awareness of the benefits or dangers of the vaccine, health status (including hospitalization for COVID- 19 at any time in the past and the treatment details) and vaccination status of the family members, the reasons for postponing vaccination or hesitancy in vaccination, perceptions regarding child vaccination were recorded. For perception regarding child COVID-19 vaccination, a modified Oxford COVID- 19 vaccine hesitancy scale (MOVHS) was used. [13] The questionnaires (see appendix) were reviewed by two experts for content validity and was then translated to the local language Tamil and again back translated to English to ensure that the actual meaning is retained in both languages. Health care workers who were parents and who were willing to participate in the study were included. Those who had current COVID illness and hospitalized or in home isolation or home quarantine, not being present on the day of interview or unable to give sufficient information were excluded (Fig. 1 ). The data from the interview was entered into a data collection proforma from which the information was exported to excel chart and analysed using SPSS software. Categorical variables like gender, religion, socioeconomic status, health care worker type vaccination status, COVID-19 status, magnitude of vaccine hesitancy (defined as failure to get vaccinated or unduly delaying it due to any reason) is expressed as proportion and analysed, using chi square test. Association between vaccine hesitancy in HCWP and perceptions to child vaccination was explored using chi square test and a P value of less than 0.05 was considered for statistical significance.
Fig. 1.
Study Flow Diagram.
3. Results:
A total of 269 HCWPs were included (Fig. 1). Out of the 269 HCWPs, 125 (46 %) were males and the rest were females. Nurses constituted the majority of HCWPs accounting for about one third of the study population, followed by medical social workers (MSWs) and miscellaneous staff, doctors including research scholars, housekeeping staff, security personnel, pharmacists and technicians and engineers combined in that order (Table 1 ). The miscellaneous staff included counsellors, out patient department attendants, dressers, physiotherapists, and scholars pursuing Master of Public Health. Only eight HCWPs were not fully vaccinated against COVID-19 accounting for 3 % of the HCWPs. Of these eight individuals, males and females were equal in number, nurses accounted for five HCWPs followed by two housekeeping staff and one security personnel (Table 2 ). Recent COVID-19 infection, worries about adverse effects of the vaccine and recent abortion kept three participants from receiving the vaccination. When queried whether they would vaccinate their children when COVID-19 vaccination is rolled out for their children, 229 (85.13 %) HCWPs said they would vaccinate their children, 34 (12.6 %) said they wouldn’t and 6 (2.2 %) said they were not sure (Table 3 ). Of the HCWPs 100 % of MSWs and miscellaneous staff and pharmacists said they would get their children vaccinated. A higher proportion of security personnel and housekeeping staff said they wouldn’t vaccinate their children (Table 3). The reasons mentioned for not vaccinating their children is given in Table 4 . On analysing the COVID-19 infection status among the participants, it was found that the doctors were most often infected (56.8 %) and technicians/engineers were not affected at all.
Table 1.
Sociodemographic characteristics of the Health care-worker parents in a tertiary care institute, Puducherry, India, 2022.
| Sociodemographic | Characteristics | Total N (%) |
|---|---|---|
| Gender |
Male | 125 (45.9) |
| Female | 144 (54.1) | |
| Residence | Puducherry | 262 (97.4) |
| Others | 7 (2.6) | |
| Occupation | Doctors/PhD scholars | 37 (13.8) |
| Nursing officers | 79 (29.4) | |
| Medical Social Workers and Miscellaneous staff | 50 (18.6) | |
| Housekeeping staff | 37 (13.8) | |
| Security personnel | 31 (11.5) | |
| Pharmacists | 28 (10.4) | |
| Technicians/Engineers | 7 (2.6) |
Table 2.
COVID Vaccination status of study participants.
| Characteristics | Vaccination Status | ||
|---|---|---|---|
| YES N (%) |
NO N (%) |
||
| Completed two doses of vaccine prior to start of the study | 261 (97) | 8 (3) | |
| Gender | Male | 121 (46.3) | 4 (50) |
| Female | 140 (53.6) | 4 (50) | |
| Residence | Puducherry | 254 (97.3) | 8 (1 0 0) |
| Others | 7 (2.6) | 0 | |
| Occupation | Doctors/PhD scholars | 37 (14.1) | 0 |
| Nursing officers | 74 (28.3) | 5 (62.5) | |
| Medical Social Workers and Miscellaneous staff | 50 (19.1) | 0 | |
| Housekeeping staff | 35 (13.4) | 2 (25) | |
| Security personnel | 30 (11.4) | 1 (12.5) | |
| Pharmacists | 28 (10.7) | 0 | |
| Technicians/Engineers | 7 (2.6) | 0 | |
Completed vaccination is defined as those who had received two doses of COVID vaccine before the start of the study.
Table 3.
Willingness to vaccinate their children.
| Characteristics | RESPONSES | P value* | ||||
|---|---|---|---|---|---|---|
| Yes if rolls out N (%) | No N (%) |
Not sure N (%) |
Total | |||
| Gender |
Male | 107 (46.7) | 15 (44.1) | 3(50) | 125 | 0.958 |
| Female | 122 (53.3) | 19 (55.1) | 3(50) | 144 | ||
| Residence | Puducherry | 224 (97.8) | 32 (94.1) | 6 | 262 | 0.414 |
| Others | 5 (2.2) | 2 (5.9) | 0 | 7 | ||
| Doctors/PhD Scholars | 31 (13.5) | 5 (14.7) | 1(16.6) | 37 | 0.000 | |
| Nursing officers | 74 (32.3) | 3 (8.8) | 2( 33.3) | 79 | ||
| Medical Social Workers & Miscellaneous staff | 50 (21.8) | 0 | 0 | 50 | ||
| Housekeeping staff | 24 (10.4) | 12 (35.3) | 1(16.6) | 37 | ||
| Security Personnel | 17 (7.4) | 12 (35.3) | 2(33.3) | 31 | ||
| Pharmacists | 28 (12.2) | 0 | 0 | 28 | ||
| Technicians/Engineers | 5 (2.1) | 2 (5.9) | 0 | 7 | ||
Pearson‘s chi-square test.
Table 4.
Reasons for not willing to vaccinate their children when vaccine is made available.
| S. No | Reasons for not willing to vaccinate their children | Numbers N (%) N = 34 |
|---|---|---|
| 1 | Worried about adverse effects | 12 (4.5) |
| 2 | Was advised against it | 2 (0.7) |
| 3 | Illness not severe in children | 16 (6) |
| 4 | Underlying comorbidities preclude vaccination | 2 (0.7) |
| 5 | Adverse events following immunisation in the past | 2 (0.7) |
| 6 | Others (waiting for pan coronavirus vaccine, research lacuna, combined) | 3 (1.1) |
Multiple responses possible for each participant.
Majority of the infected had mild symptoms and were under home quarantine. Hospitalization and or intensive care unit stay was needed for two nurses and one housekeeping staff (Table 5 ). While analysing the responses to the MOVHS questionnaire (appendix 1), it was seen that the responses were predominantly positive for all the questions among doctors, nurses, MSWs, pharmacists, technicians and security whereas it was predominantly negative for housekeeping staff (Table 6 ).
Table 5.
Morbidity pattern of participants during their COVID-19 infection.
| Occupation | Home Quarantine | Hospitalization/ ICU Care | Not Infected | Total |
|---|---|---|---|---|
| Doctors/PhD Scholars | 21 | 0 | 16 (43.2) | 37 |
| Nursing officers | 25 | 2 | 52 (65.8) | 79 |
| Medical Social Workers & miscellaneous staff | 11 | 0 | 39 (78) | 50 |
| Housekeeping staff | 8 | 1 | 29(76.3) | 38 |
| Security Personnel | 7 | 0 | 24 (77.4) | 31 |
| Pharmacists | 7 | 0 | 21 (75) | 28 |
| Technicians/Engineers | 0 | 0 | 7 (1 0 0) | 7 |
Table 6.
Occupation wise response of the participants to the Modified Oxford VHS Questionnaire.
| S.No of question-naire items | Occupation | Responses to the questionnaire items |
P value* | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| 1 | Doctors/PhD Scholars (37) | 20 | 11 | 0 | 1 | 5 | 0 | 0.00 |
| Nursing officers(79) | 45 | 30 | 3 | 1 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 18 | 32 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 4 | 4 | 26 | 2 | 1 | 0 | ||
| Security Personnel(31) | 11 | 15 | 4 | 0 | 1 | 0 | ||
| Pharmacists(28) | 13 | 15 | 0 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 1 | 3 | 1 | 0 | 2 | 0 | ||
| 2 | Doctors/PhD Scholars (37) | 25 | 5 | 5 | 1 | 1 | 0 | 0.00 |
| Nursing officers(79) | 44 | 33 | 2 | 0 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 29 | 21 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 3 | 0 | 19 | 15 | 0 | 0 | ||
| Security Personnel(31) | 13 | 14 | 3 | 0 | 1 | 0 | ||
| Pharmacists(28) | 13 | 15 | 0 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 4 | 1 | 1 | 1 | 0 | 0 | ||
| 3 | Doctors/PhD Scholars (37) | 16 | 16 | 2 | 1 | 2 | 0 | 0.00 |
| Nursing officers(79) | 27 | 44 | 7 | 0 | 1 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 12 | 38 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 2 | 4 | 18 | 12 | 0 | 1 | ||
| Security Personnel(31) | 7 | 20 | 3 | 0 | 0 | 1 | ||
| Pharmacists(28) | 6 | 18 | 4 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 3 | 2 | 0 | 1 | 1 | 0 | ||
| 4 | Doctors/PhD Scholars (37) | 17 | 10 | 7 | 1 | 2 | 0 | 0.00 |
| Nursing officers(79) | 25 | 52 | 1 | 1 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 16 | 34 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 2 | 4 | 15 | 16 | 0 | 0 | ||
| Security Personnel(31) | 7 | 21 | 2 | 1 | 0 | 0 | ||
| Pharmacists(28) | 4 | 24 | 0 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 1 | 3 | 2 | 1 | 0 | 0 | ||
| 5 | Doctors/PhD Scholars (37) | 20 | 9 | 2 | 4 | 2 | 0 | 0.00 |
| Nursing officers(79) | 24 | 52 | 2 | 1 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 23 | 27 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 6 | 6 | 17 | 8 | 0 | 0 | ||
| Security Personnel(31) | 12 | 17 | 1 | 1 | 0 | 0 | ||
| Pharmacists(28) | 15 | 13 | 0 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 3 | 1 | 0 | 2 | 1 | 0 | ||
| 6 | Doctors/PhD Scholars (37) | 15 | 16 | 1 | 4 | 1 | 0 | 0.00 |
| Nursing officers(79) | 28 | 50 | 0 | 1 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 11 | 38 | 0 | 1 | 0 | 0 | ||
| Housekeeping staff (37) | 2 | 13 | 15 | 7 | 0 | 0 | ||
| Security Personnel(31) | 14 | 14 | 1 | 2 | 0 | 0 | ||
| Pharmacists(28) | 14 | 11 | 0 | 0 | 3 | 0 | ||
| Technicians/Engineers(7) | 3 | 1 | 1 | 2 | 0 | 0 | ||
| 7 | Doctors/PhD Scholars (37) | 18 | 13 | 4 | 0 | 1 | 0 | 0.00 |
| Nursing officers(79) | 38 | 36 | 5 | 0 | 0 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 24 | 26 | 0 | 0 | 0 | 0 | ||
| Housekeeping staff (37) | 6 | 9 | 15 | 6 | 1 | 0 | ||
| Security Personnel(31) | 11 | 15 | 4 | 0 | 1 | 0 | ||
| Pharmacists(28) | 11 | 14 | 3 | 0 | 0 | 0 | ||
| Technicians/Engineers(7) | 2 | 2 | 2 | 1 | 0 | 0 | ||
* P value by Pearson‘s Chi square test. For the list of questions and key to the scale response code refer to supplementary files
While analysing the responses to the VHS questionnaire, a tendency towards positive response was seen predominantly in all sections of HCWPs for statements 1–3. For statement 4, a tendency towards positive response was predominantly seen among all sections of HCWPs except nurses and MSWs and miscellaneous staff group. For statement 5, majority of HCWPs except doctors displayed a predominant trend towards disagreement. For statement 6 there was predominantly neutral response for majority of HCWPs except for doctors and nurses who displayed varying degrees of neutrality and agreement. For statements 7–9, a tendency towards agreement was seen predominantly in all sections of HCWPs. For statement 10, neutral responses or a trend towards agreement was seen predominantly in all classes of HCWPs except in housekeeping staff in whom the responses were predominantly towards disagreement (Table 7 ). On analysing the relationship between positive responses to MOVHS questionnaire and the likelihood of self-vaccination and vaccinating their children, it was seen that there was a significant association between proportion of HCWPs with positive response and self-vaccination and vaccinating their children for all classes with the exception of housekeeping staff in whom although the proportion with positive responses is low, the proportion of self-vaccination and vaccinating their children was high (Table 8 ).
Table 7.
Occupation wise response of the participants to the VHS LIKERT Scale questions.
| S.No of question-naire items | Occupation | Response to the LIKERT scale questions |
P value* | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| 1 | Doctors/PhD Scholars (37) | 1 | 1 | 2 | 2 | 31 | 0.223 |
| Nursing officers(79) | 0 | 1 | 5 | 10 | 63 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 1 | 3 | 46 | ||
| Housekeeping staff (37) | 0 | 1 | 1 | 0 | 35 | ||
| Security Personnel(31) | 2 | 1 | 1 | 2 | 25 | ||
| Pharmacists(28) | 0 | 0 | 3 | 0 | 25 | ||
| Technicians/Engineers(7) | 0 | 0 | 1 | 0 | 6 | ||
| 2 | Doctors/PhD Scholars (37) | 0 | 0 | 6 | 8 | 23 | 0.101 |
| Nursing officers(79) | 0 | 1 | 4 | 15 | 59 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 3 | 8 | 39 | ||
| Housekeeping staff (37) | 0 | 1 | 0 | 6 | 30 | ||
| Security Personnel(31) | 2 | 1 | 3 | 2 | 23 | ||
| Pharmacists(28) | 0 | 0 | 2 | 3 | 23 | ||
| Technicians/Engineers(7) | 0 | 0 | 1 | 0 | 6 | ||
| 3 | Doctors/PhD Scholars (37) | 1 | 0 | 2 | 7 | 27 | 0.044 |
| Nursing officers(79) | 0 | 1 | 5 | 13 | 60 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 0 | 15 | 35 | ||
| Housekeeping staff (37) | 0 | 0 | 1 | 12 | 24 | ||
| Security Personnel(31) | 3 | 1 | 1 | 10 | 16 | ||
| Pharmacists(28) | 0 | 0 | 0 | 6 | 22 | ||
| Technicians/Engineers(7) | 1 | 0 | 0 | 1 | 5 | ||
| 4 | Doctors/PhD Scholars (37) | 0 | 1 | 2 | 10 | 24 | 0.001 |
| Nursing officers(79) | 0 | 0 | 24 | 32 | 23 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 14 | 21 | 15 | ||
| Housekeeping staff (37) | 0 | 1 | 2 | 18 | 16 | ||
| Security Personnel(31) | 0 | 1 | 7 | 11 | 12 | ||
| Pharmacists(28) | 0 | 0 | 0 | 12 | 16 | ||
| Technicians/Engineers(7) | 0 | 0 | 2 | 0 | 5 | ||
| 5 | Doctors/PhD Scholars (37) | 11 | 6 | 16 | 3 | 1 | 0.001 |
| Nursing officers(79) | 12 | 41 | 24 | 2 | 0 | ||
| Medical Social Workers& Miscellaneous staff (50) | 14 | 29 | 6 | 0 | 1 | ||
| Housekeeping staff (37) | 4 | 24 | 8 | 0 | 1 | ||
| Security Personnel(31) | 6 | 20 | 2 | 2 | 1 | ||
| Pharmacists(28) | 2 | 17 | 8 | 1 | 0 | ||
| Technicians/Engineers(7) | 4 | 1 | 2 | 0 | 0 | ||
| 6 | Doctors/PhD Scholars (37) | 3 | 1 | 11 | 8 | 14 | 0.000 |
| Nursing officers(79) | 0 | 7 | 31 | 12 | 29 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 6 | 37 | 6 | 1 | ||
| Housekeeping staff (37) | 1 | 10 | 19 | 3 | 4 | ||
| Security Personnel(31) | 0 | 7 | 20 | 1 | 3 | ||
| Pharmacists(28) | 0 | 4 | 14 | 2 | 8 | ||
| Technicians/Engineers(7) | 1 | 0 | 3 | 1 | 2 | ||
| 7 | Doctors/PhD Scholars (37) | 1 | 0 | 5 | 17 | 14 | 0.007 |
| Nursing officers(79) | 1 | 1 | 1 | 28 | 48 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 2 | 29 | 19 | ||
| Housekeeping staff (37) | 1 | 1 | 0 | 16 | 19 | ||
| Security Personnel(31) | 0 | 1 | 5 | 20 | 5 | ||
| Pharmacists(28) | 0 | 0 | 1 | 12 | 15 | ||
| Technicians/Engineers(7) | 0 | 0 | 0 | 1 | 6 | ||
| 8 | Doctors/PhD Scholars (37) | 0 | 0 | 1 | 10 | 26 | 0.74 |
| Nursing officers(79) | 0 | 0 | 1 | 23 | 55 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 0 | 0 | 12 | 38 | ||
| Housekeeping staff (37) | 1 | 0 | 1 | 7 | 28 | ||
| Security Personnel(31) | 1 | 1 | 1 | 9 | 19 | ||
| Pharmacists(28) | 0 | 0 | 0 | 9 | 19 | ||
| Technicians/Engineers(7) | 0 | 0 | 0 | 1 | 6 | ||
| 9 | Doctors/PhD Scholars (37) | 2 | 9 | 9 | 9 | 8 | 0.000 |
| Nursing officers(79) | 4 | 16 | 7 | 28 | 24 | ||
| Medical Social Workers& Miscellaneous staff (50) | 0 | 2 | 5 | 25 | 18 | ||
| Housekeeping staff (37) | 1 | 1 | 2 | 15 | 18 | ||
| Security Personnel(31) | 1 | 1 | 5 | 19 | 5 | ||
| Pharmacists(28) | 0 | 7 | 0 | 10 | 11 | ||
| Technicians/Engineers(7) | 2 | 0 | 1 | 3 | 1 | ||
| 10 | Doctors/PhD Scholars (37) | 8 | 6 | 6 | 3 | 14 | 0.000 |
| Nursing officers(79) | 6 | 32 | 24 | 11 | 6 | ||
| Medical Social Workers& Miscellaneous staff (50) | 4 | 15 | 30 | 1 | 0 | ||
| Housekeeping staff (37) | 15 | 12 | 4 | 3 | 3 | ||
| Security Personnel(31) | 1 | 11 | 16 | 0 | 3 | ||
| Pharmacists(28) | 5 | 8 | 12 | 3 | 0 | ||
| Technicians/Engineers(7) | 2 | 3 | 1 | 1 | 0 | ||
* P value by Pearson‘s Chi square test. For the list of questions and key to the scale response code refer to supplementary files.
Table 8.
Comparison of positive response to NHS questionnaire and vaccination status of self and children occupation wise.
| S. No | Occupation | Positive Response N (%) | Self-Vaccination N (%) |
Vaccination of children N (%) |
P Value |
|---|---|---|---|---|---|
| 1 | Doctors/PhD Scholars (37) | 30 (13.7) | 37 (14.1) | 31 (13.5) | 0.001241 Pearson R −0.9464 |
| 2 | Nursing officers (79) | 75 (34.2) | 74 (28.3) | 74 (32.3) | |
| 3 | Medical Social Worker & miscellaneous staff (50) | 50 (22.8) | 50 (19.1) | 50 (21.8) | |
| 4 | Housekeeping Staff (37) | 7 (3.19) | 35 (13.4) | 24 (10.4) | |
| 5 | Security Personnel (31) | 27 (12.3) | 30 (11.4) | 17 (7.4) | |
| 6 | Pharmacists (28) | 26 (11.8) | 28 (10) | 28 (12.2) | |
| 7 | Technicians/Engineers (7) | 4 (1.8) | 7 (2.6) | 5 (2.1) | |
| Total | 219 | 261 | 229 |
4. Discussion:
In our study, majority (97 %) of HCWPs were fully vaccinated. Recent covid illness, fear of adverse effects and recent miscarriage were cited as reasons for not getting vaccinated. Majority of the HCWPs were willing to vaccinate the children once it is made available. Mild presentation of COVID-19 in children and adverse effects were the reasons for unwillingness among parents regarding vaccination of their children.
In the United States (U.S), 15 % of the health care workers were hesitant to receive COVID-19 vaccines compared to only 3 % in our study. [14] In another study done among medical students in Ethiopia, about 85 % of the participants responded favourably to questions related to covid-19 vaccination which is also similar to our study. [15] Our finding is also similar to the COVID-19 vaccine hesitancy survey report among general public from seven Caribbean countries published by the United Nation‘s Children‘s education fund (UNICEF) in 2021. According to the UNICEF report, 62 % of their study population indicated that they had been vaccinated and the majority also indicated that they would get their children vaccinated at secondary care or tertiary care institutions. [16].
In an Indian study conducted in early 2021 among 1638 participants from 27 states/union territories who took the survey, the majority of the participants being 18–30 years old (52 %), living in urban areas (69 %), with college education (81 %), without a history of COVID-19 infection (92 %). More than a fifth were either unaware of the vaccines (20.63 %) or were not sure if they will get the vaccine (27 %), and 10 % indicated that they will refuse to obtain the vaccine even if it was made available. Almost 70 % of the population had concerns regarding the vaccines. Statistically significant differences (p less than 0.01) in awareness about vaccine and acceptability were observed based on age, educational qualifications, and employment status. [17] Our findings are strikingly different from the above study as our study was done among HCWPs and almost every-one was aware of the importance of COVID-19 vaccines and the number of persons who had concerns with the vaccine was very negligible.
When analysing the reasons for not vaccinating, only three respondents indicated a reason each for not vaccinating themselves out of which one person was apprehensive of adverse effects of vaccination. Among the responses regarding vaccination of children although many parents felt COVID-19 is a mild illness in children and therefore do not require vaccination, the second most common cause was fear of adverse effects in their children. Similarly, another study from Turkey too reported that fear of adverse effects of vaccination is a significant driver of vaccine hesitancy. [18].
With reference to vaccinating their children, although the majority of HCWPs had a positive mind set about vaccinating their children, variations in opinions existed among different class of workers; a higher proportion of security personnel and housekeeping staff opined that they would not vaccinate their children compared to the rest of other professions indicating that differences in socio-economic and educational status might make people behave differently based on inadequate information and biased perceptions. Such differences have also been implicated as one of the reason for poor vaccine coverage in another Indian study which looked at the vaccination rates after the second wave. [19].
Our study attempted to look at vaccine hesitancy among health care worker parents and their perceptions about vaccinating their children against COVID-19. The major strength of our study is that it is one of the few studies carried out in a high risk population of health care workers who are parents. The limitations being a single centre study and inability to collect responses from all participants, the reasons for not vaccinating themselves and under representation of nursing officers, technicians and engineers and over representation of medical social workers and miscellaneous staff and pharmacists working at our institute. Although an attempt was made to sample all health care workers based on the proportion of their composition, we were not able to recruit the planned number of participants under each category. There may be a component of recall bias affecting the validity of our study result as information concerning vaccination was obtained by asking the participants for relevant details. As the study was descriptive in nature we did not check for any interaction and also did not do any analysis for confounding.
To conclude we find that vaccine hesitancy in our population of health care worker parents were much less compared to other studies. Most HCWPs responded positively about vaccination of self as well as their children. Among HCWPs certain groups had perceptual differences regarding vaccinating themselves and their children. Further studies are needed to analyse why such differences exist and how to mitigate them.
Contributions
All authors were involved in conceptualization and designing the methodology of the study. PS carried out the study under guidance and supervision from VC, DG, and PC. PS and VC were involved in data visualization and data analysis. PC was involved in data analysis and contributed to the intellectual content of the manuscript. All authors were involved in reviewing of literature and drafting of the manuscript. All authors have seen and approved the final draft.
Funding
Nil.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank the department of Preventive and Social Medicine for helping in the statistical analysis.
Data availability
Data will be made available on request.
References:
- 1.World health organization Coronavirus (COVID-19) Dashboard. Available from: covid19.who.int. Accessed on 10th August 2022.
- 2.Rasmussen AL. Vaccination is the only acceptable path to herd immunity. Cell press Elsevier Inc. 2020; 1:14-32. [DOI] [PMC free article] [PubMed]
- 3.Lazarus J.V., Ratzan S.C., Palayew A., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khubchandani J., Sharma S., Price J.H., et al. COVID-19 vaccine hesitancy in the United States: A rapid national assessment. J Community Health. 2021;46:270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sallam M. COVID-19 Vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biswas N., Mustapha T., Khubchandani J., et al. The nature and extent of COVID-19 vaccination hesitancy in health care workers. J Community Health. 2021 doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams S.E. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it? Human vaccines & immunotherapeutics. 2014;10:2584–2596. doi: 10.4161/hv.28596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:1–5. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; 33: 4161-4. [DOI] [PubMed]
- 11.The determinants of vaccine hesitancy: Sample survey questions. Available at https://www.who.int/immunization/sage/meetings/2013/april/4_survey_questionsRevised. Pdf.
- 12.Domek G.J., O'Leary S.T., Bull S., Bronsert M., Contreras-Roldan I.L., Ventura G.A., et al. Measuring vaccine hesitancy: Field testing the WHO SAGE Working Group on Vaccine Hesitancy survey tool in Guatemala. Vaccine. 2018;36(35):5273–5281. doi: 10.1016/j.vaccine.2018.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., et al. COVID-19 vaccine hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (OCEAN) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toth-Manikowski S.M., Swirsky E.S., Gandhi R., Piscitello G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am J Infect Control. 2022 Jan;50(1):20–25. doi: 10.1016/j.ajic.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mose A., Haile K., Timerga A. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS ONE. 2022 Jan 25;17(1) doi: 10.1371/journal.pone.0263081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 Vaccine Hesitancy Survey Report 2021. Available at: https://www.unicef.org/easterncaribbean/media/2996/file/COVID%20vaccine%20hesitancy%20rep.pdf. Accessed on 19th April 2022.
- 17.Chandani S., Jani D., Sahu P.K., et al. COVID-19 vaccination hesitancy in India: State of the nation and priorities for research. Brain Behav Immun Health. 2021;18 doi: 10.1016/j.bbih.2021.100375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yigit M., Ozkaya-Parlakay A., Senel E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatr Infect Dis J. 2021;40(4):e134–e136. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]
- 19.Chakraborty C., Sharma A.R., Bhattacharya M., Agoramoorthy G., Lee S.S. The current second wave and COVID-19 vaccination status in India. Brain Behav Immun. 2021;96:1–4. doi: 10.1016/j.bbi.2021.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.