Abstract
Background:
Open hindfoot surgery is associated with a relatively high rate of complications, including neurovascular injuries and wound healing problems compared with percutaneous techniques. However, there is a scarcity of literature describing the outcomes of these percutaneous techniques given their relatively recent adoption. The present study aims to assess the rate of postoperative complications for 3 commonly performed percutaneous calcaneal osteotomies.
Methods:
One hundred eighteen patients (unilateral feet) were treated with one of 3 common percutaneous calcaneal osteotomies. Sixty-five patients (55.1%) were treated with a medializing calcaneal osteotomy for hindfoot valgus, 32 patients with a Zadek osteotomy (27.1%) for insertional Achilles tendinopathy, and 21 patients (17.8%) with a modified Dwyer osteotomy for hindfoot varus. Fisher exact test was used to assess for associations between categorical variables.
Results:
The mean age was 46.2 years and there was a mean follow-up of 16.1 months. The overall rate of postoperative complications was 3.4% (n = 4), and no significant differences were found between the different osteotomy types. Complications included 2 cases (1.7%) of transient neuritis, 1 case of prolonged wound drainage (0.8%), and 1 nonunion (0.8%). None of the complications were associated with any recorded preoperative comorbidity.
Discussion:
In this series, we found that percutaneous calcaneal osteotomies are a safe alternative method for the treatment of conditions involving the hindfoot. The rate of postoperative complications may be less when compared to the reported rates of open hindfoot correction and should be considered in patients with a traditionally high risk of developing a postoperative complication.
Level of Evidence:
Level IV, retrospective analysis.
Keywords: percutaneous surgery, minimally invasive surgery, calcaneus osteotomy, postoperative complication
Introduction
Foot and ankle surgery is associated with a high rate of postoperative complications when compared to other orthopaedic procedures.4,12 Wound complications are among the most common postoperative complication following foot and ankle surgery, with reported rates ranging from 5% to 28%.9,21 Prior literature has identified age, diabetes, obesity, and active smoking status as independent risk factors for postoperative complications after foot and ankle surgery.13,15,21
To reduce the risk of these potential postoperative complications, percutaneous foot and ankle surgery has been gaining popularity. Some techniques such as those reported by DiDomenico et al utilize a Gigli-saw with multiple skin incisions. 3 In contrast, Wacker and colleagues described their percutaneous technique using a Shannon burr. 20 Currently, most surgeons perform these operations through <1-cm incisions using a high-speed burr, and percutaneous techniques are regarded as having less soft tissue injuries, less postoperative pain, and a quicker recovery.10,24 However, despite the minimally invasive approach, some studies on percutaneous techniques have reported on postoperative complications such as minor nerve damage, and to a lesser extent, wound complications.5,17
Therefore, the purpose of this study is to describe and report the risk of complications, with different types of calcaneal osteotomies performed via a percutaneous approach. This article adds to the existing body of literature on complications after medial displacement calcaneal osteotomies, and is the largest series, to our knowledge, to report on complications after percutaneous Dwyer and Zadek osteotomies. 2
Methods
The surgeries were performed by a single fellowship-trained foot and ankle surgeon from July 1, 2017, to August 1, 2019. There were no selectively performed open osteotomies during the study collection period. Inclusion criteria consisted of patients aged 18-65 years without a history of previous calcaneal osteotomy of the foot. Medializing (MDCOs) and modified Dwyer (DOs) calcaneus osteotomies were performed in patients affected by hindfoot valgus and hindfoot varus, respectively. Zadek osteotomies (ZOs) were indicated in patients with chronic insertional Achilles tendinopathy. All patients undergoing surgery had failed a minimum of 3 months of nonoperative treatment. Exclusion criteria consisted of prior open surgery to the hindfoot. The minimum follow-up required for the study was 12 months. Full weightbearing radiographs of the foot and ankle were obtained before surgery to assess the grade of deformity and to perform the operative planning.
History of diabetes mellitus (DM) and idiopathic neuropathy without a history of DM were registered at the preoperative visit. Postoperative complications (wound dehiscence, infection, transient sural neuritis, medial neurovascular bundle lesions, lateral overhang pain, malposition) were assessed for at each follow-up visit after surgery.
Surgical Procedures
All patients were positioned supine, no tourniquet was used. The osteotomy site was marked on the lateral aspect of the hindfoot under fluoroscopic guidance (Figures 1-3). A concomitant Vulpius gastrocnemius recession was performed in all patients except those undergoing an ankle fusion or those undergoing the Zadek procedure. All patients undergoing an MDCO also underwent the following procedures: 35 flexor digitorum longus transfers, 23 peroneus brevis to longus transfers, 16 lateral column lengthenings, 13 midfoot fusions, 7 total ankle replacements, 4 triple arthrodeses, 4 ankle fusions, and 2 supramalleolar osteotomies. In the Dwyer group, 4 patients underwent total ankle replacements, 6 peroneus longus to brevis transfers, 5 ankle fusions, 4 triple arthrodeses, 1 tibiotalocalcaneal fusion, and 1 midfoot derotational osteotomy.
Figure 1.
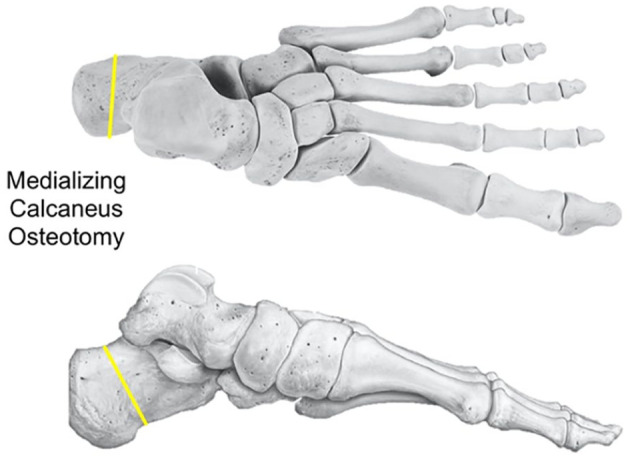
Medializing calcaneus osteotomy. The line demonstrates the orientation of the osteotomy.
Figure 2.
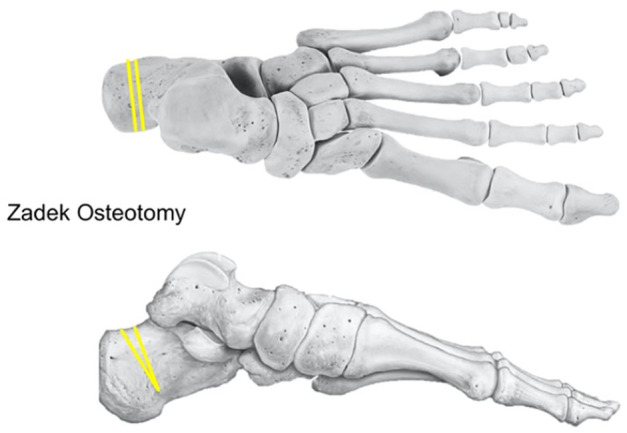
Dorsal closing wedge osteotomy, or Zadek osteotomy. The lines demonstrate the orientation of the osteotomy.
Figure 3.
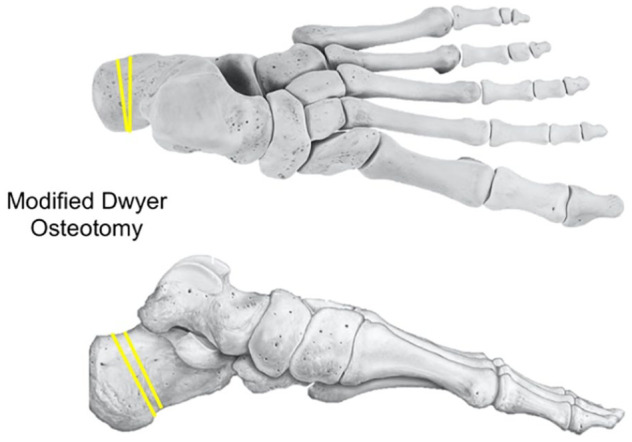
Modified Dwyer osteotomy. The line demonstrates the orientation of the osteotomy.
MDCO
Through a 3-mm incision at the center of the planned osteotomy, a Crile hemostat was introduced and used for blunt dissection. A 3 × 20-mm cutting burr attached to an irrigation system (Wright Medical, Memphis, TN) was advanced and the burr activated at 6000 to 7000 rpm. As per the senior author’s preference, the proximal half of the osteotomy was completed first at the level of the cancellous bone, followed by the plantar limb of the osteotomy. Then, the far cortex was poke-holed with the burr and ultimately the “dots were connected” by swiping through the far cortex with the burr. On completion of the osteotomy, the posterior tuberosity was medially shifted with the use of a freer elevator or a 3-mm Steinmann pin inserted through the incision. The osteotomy was stabilized with a single 7-mm or two 5-mm (in osteopenic bone) headless compression screws (Wright Medical). The wound was not flushed with saline to avoid washing out the bone paste that served as bone graft at the osteotomy site. The surgical incision was closed with a single simple 3-0 nylon suture (Figure 4).
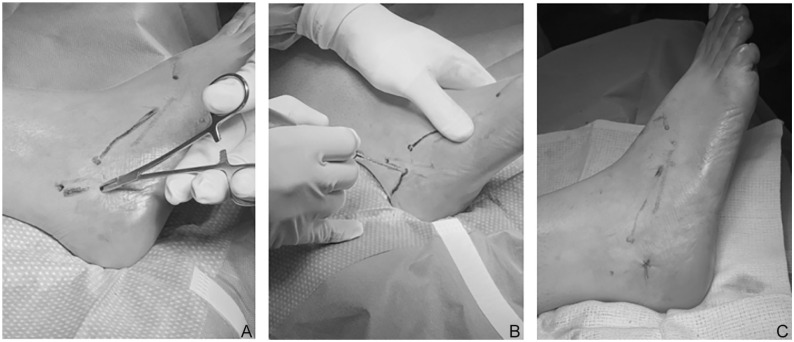
Figure 4.
(A) Intraoperative image of the minimally invasive approach for the calcaneal osteotomy. (B) Intraoperative image of the osteotomy performed with a 3x20 mm cutting burr wedge (Wright Medical). (C) Intraoperative image of the surgical area after closure.
DO
Through a 3-mm incision at the center of the planned osteotomy, a Crile hemostat was introduced and used for blunt dissection. A 3 × 20-mm cutting burr attached to an irrigation system (Wright Medical) was advanced and the burr activated at 6000 to 7000 rpm. As per the senior author’s preference, the proximal half of the osteotomy was completed first at the level of the cancellous bone, followed by the plantar limb of the osteotomy. Then, the far cortex was poke-holed with the burr and ultimately the “dots were connected” by swiping through the far cortex with the burr. On completion of the osteotomy, the burr was exchanged for a 3-mm wedge (shaving) burr (Wright Medical). Through the same incision, the burr was inserted to shave the near two-thirds of the cancellous bone on either side of the osteotomy. Depending on the degree of hindfoot varus correction necessary, the size of the lateral closing wedge varied on a case-by-case basis. The osteotomy was then manually closed, shifted laterally, and stabilized with a single 7-mm or two 5-mm (in osteopenic bone) headless compression screws. The wound was not flushed with saline to avoid washing out the bone paste that served as bone graft at the osteotomy site. The surgical incision was closed with a single simple 3-0 nylon suture.
ZO
The osteotomy was planned under fluoroscopic guidance at the lateral aspect of the hindfoot to remove a dorsally based wedge of 8 to 10 mm. The apex of the osteotomy was 5 to 10 mm proximal to the plantar cortex of the calcaneus. The skin was incised 3mm at the level of the apex of the osteotomy, and soft tissues dissected bluntly with a Crile hemostat. A 3x20mm cutting burr attached to an irrigation system (Wright Medical) was advanced and the burr activated at 6000-7000 rotations per minute (rpm). As per the senior author’s preference, the near cancellous bone followed by the far cancellous bone was cut. Then, the far cortex was poke-holed with the burr and ultimately the “dots were connected” by swiping through the far cortex with the burr. On completion of the osteotomy, the burr was exchanged for a 3-mm wedge (shaving) burr (Wright Medical). Through the same incision, the burr was inserted to shave either side of the osteotomy to remove the planned 8-10 mm of dorsal wedge. On completion of the osteotomy, the ankle was maximally dorsiflexed to achieve reduction. The osteotomy was stabilized with a single 7-mm or two 5-mm (in osteopenic bone) headless compression screws. The surgical incision was closed with a single simple 3-0 nylon suture.
Postoperative Care
All the patients were discharged from the hospital on the same day of surgery, and the foot was protected with a bulky splint or walking boot. The ZO cohort was encouraged to fully weightbear (WB) at 2 weeks from surgery in a walking boot with discontinuation of the boot at 6 weeks. The MDCO and DO cohorts were nonweightbearing (NWB) for the first 6 weeks, after which they were allowed full WB in a boot. It was important to initially protect these patients as most of them also underwent concurrent surgical procedures such as flexor digitorum tendon transfer, posterior tibial tendon transfer, lateral column lengthening, midfoot osteotomies, etc. The boot was discontinued after 12 weeks from surgery. All patients started stretching, strengthening, and proprioception rehabilitation 2 weeks from surgery. Postoperative visits and radiographs were done at 2 weeks, 6 weeks, and 3 months from surgery. After that the patients were revisited every 3-6 months.
Statistical Analysis
Data analysis was performed using Stata/MP 16.1 (College Station, TX). Descriptive statistical analysis was performed on all variables, yielding frequency and percentages for categorical variables, and mean, SD, and ranges for continuous variables. Fisher exact test was used to determine association between categorical variables. A P value ≤.05 was considered to be statistically significant.
Results
There were 118 consecutive patients (118 unilateral feet) with a mean age of 46.2 years (range, 13-87 years). The study population was composed of 54 males (46%) with a mean age of 48.4 years (range, 19-75 years) and 64 females (54%) with a mean age of 45 years (range, 13-87 years). Sixty-five patients (55.1%), mean age of 44.2 years (range, 18-87 years), were treated with an MDCO; 32 patients underwent a ZO (27.1%), mean age 56.1 years (range, 43-75 years); and 21 patients (17.8%) with a DO, mean age 37.3 years (range, 13-61 years).
Mean follow-up was 16.1 months (range, 12-25). There were 21 patients with hypertension (17.8%), 11 patients with DM (9.3%), and 1 patient with idiopathic neuropathy (0.8%). All patients with DM had a hemoglobin A1c <8.5% at the time of surgery.
The overall rate of postoperative complications was 3.4% (n=4). The rate of complications was 3.1% in the MDCO group, 3.1% in the ZO group, and 4.8% in the DO group, with no significant difference between the 3 groups (P > .99). The complications were 1 case of prolonged wound drainage (0.8%) that required advanced wound care (resolved after 4 weeks), 2 cases of transient sural neuritis (1.7%) that resolved spontaneously after 8 and 16 weeks, and 1 nonunion (0.8%). Injury to the lateral calcaneal nerve was specifically tested for and none noted. The nonunion occurred in a 60-year-old healthy man who likely developed the complication because of violation of the plantar cortex during the ZO. The patient underwent successful open revision with bone grafting, plate, and screws.
Discussion
Our study showed a low (3.4%) overall rate of postoperative complications after percutaneous osteotomies of the calcaneus when retrospectively evaluating 118 patients at an average of 18-month follow-up. More specifically, rate of complications was 3.1% in the MDCO group, 3.1% in the ZO group, and 4.8% in the DO group, with no significant difference found between the 3 groups. Given the increasing trend toward percutaneous surgery, this study adds to the growing body of literature demonstrating that percutaneous calcaneal osteotomies represent a powerful surgical tool for the treatment of foot and ankle deformities while minimizing the risk of postoperative complications.
Percutaneous surgery of the foot and ankle has gained popularity in the last decade as an approach with potential for quicker recovery, less complications, and use of fewer postoperative pain medications. 1 It was initially used as an operative tool for the treatment of forefoot deformities (hallux valgus, hammer toe, and metatarsalgia) and was successively adopted during the early 2000s for surgery of the hindfoot with good initial results.1,11,19 In the present study, the use of a percutaneous approach was associated with a 3.4% rate of postoperative complications. When considering only wound complications, this rate decreased to 2.9%. This is consistent with smaller cohorts found in literature, in which the observed rate of wound and soft tissue complications after percutaneous calcaneal osteotomies ranges from 0% to 6.5%.8,10
In the ZO group, no soft tissue complications were recorded. This is similar to published literature, in which a previous study of percutaneous ZO demonstrated no wound complications and only 2 other complications (nonunion and painful hardware), with an overall complication rate of 8%. 14 In comparison, open ZO for insertional Achilles tendinopathy has been reported to have a wound complication rate of 6.3%.7,18
Two cases of transient sural nerve injury were observed in this study (1.7%), which is lower than what has been reported in the literature; however, time to recovery was longer in our study (8-16 weeks vs 4 weeks). 8 The rate of postoperative nonunions and malunion after open calcaneal osteotomy ranges from 1.4% to 5%.16,22 We reported a single case of nonunion in the ZO (4.8%) probably related to a technique error (violation of the plantar hinge of the osteotomy).
None of the patients in the MDCO cohort had complaints of lateral overhang pain. Traditionally, it is thought that the large incision necessary for open calcaneal osteotomy is a source of pain secondary to the buildup of scar tissue, which can be aggravated by the lateral bone overhang impinging against it. Despite a rasping or reduction of the outcropping that results from the translational osteotomy in the open cases, the location of the incision that is over the osteotomy site has a propensity to cause pain. 6 This was not observed in our cohort, likely because the percutaneous incision was small and subsequently there was minimal formation of scar tissue at the site of the incision.
Patients with DM have a well-documented increased risk of postoperative wound complications and surgical site infections.17,23 The diabetes cohort in our study did not experience a postoperative complication. It should be noted, however, that the patients in our cohort had relatively well controlled diabetes, with a hemoglobin A1c <8.5% at time of surgery. In a study comparing percutaneous calcaneal osteotomy vs traditional open surgery, Gutteck et al 8 had similar results, finding that the presence of DM did not increase the risk of a postoperative complication in patients undergoing percutaneous surgery (0%). In contrast, this same study demonstrated that 50% of all patients in their cohort with diabetes had a wound healing complication with traditional open calcaneal osteotomy. Similar to diabetes, patients with idiopathic neuropathy have a 4.7-fold increased risk to develop a postoperative surgical site infection when compared to patients without this comorbidity. 23 In our study, there was only 1 patient with an idiopathic neuropathy and they did not develop a postoperative complication.
There are multiple hypotheses for the decreased rate of wound complication seen with percutaneous surgery of the hindfoot. The leading theory is that the minimally invasive nature of the approach leads to less soft tissue damage secondary to minimal dissection, consequently reducing neurovascular injuries and wound complications.
There are limitations to this study that are important to consider. First, this was a retrospective study and therefore subject to bias inherent to study populations not followed in a prospective manner. However, the consecutive nature of patient recruitment helps minimize study bias to a degree. Second, there was no control group (ie, open surgery) against which to compare our percutaneous cohort. Third, these surgeries were performed by a single fellowship-trained foot and ankle surgeon who performs a high volume of percutaneous surgery relative to the national average. This complication rate may not be generalizable to all orthopaedic surgeons nor to all patient populations. Importantly, however, Talusan and colleagues 16 have published on a well-defined safe zone for calcaneal osteotomies that can assist with the surgical “learning curve.” The authors of this study adhere to the safe zones defined by Talusan et al 16 in an attempt to minimize complications Fourth, the complications we describe include transient nerve pathology that can often be reported by patients at variable rates, particularly in the setting of extensive preoperative counseling on the issue. Therefore, this may lead to an underreporting and subsequent underestimation of nerve palsies. These symptoms, however, are specifically asked about at each postoperative visit, which hopefully minimizes the potential for underreporting.
Conclusions
In this series, we found percutaneous calcaneal osteotomies to be a safe alternative method for the treatment of conditions involving the hindfoot when compared to the classic open technique. The rate of postoperative complications may be less when compared to the reported rates of open hindfoot correction. Moreover, as there appears to be no correlation with preoperative comorbidities, minimally invasive surgery of the hindfoot should be considered in patients with a traditionally high risk of developing a postoperative complication.
Footnotes
Ethical Approval: This investigation was approved by our organization’s Institutional Review Board (IRB-18-01007).
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Ettore Vulcano, MD, is a consultant for Novastep. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Alirio J. deMeireles, MD, MBA,  https://orcid.org/0000-0002-3794-916X
https://orcid.org/0000-0002-3794-916X
Javier Z. Guzman, MD,  https://orcid.org/0000-0001-8083-1725
https://orcid.org/0000-0001-8083-1725
Andrea Nordio, MD,  https://orcid.org/0000-0003-2483-0853
https://orcid.org/0000-0003-2483-0853
Jimmy Chan, MD,  https://orcid.org/0000-0003-2154-4480
https://orcid.org/0000-0003-2154-4480
Jeffrey Okewunmi, BS,  https://orcid.org/0000-0001-9246-1186
https://orcid.org/0000-0001-9246-1186
References
- 1. Laffenete O, Coillard JY. Traitement Chirurgical de l’Hallux Valgus par Technique Percutanè [Surgical Treatment of Hallux Valgus by Percutaneous Technique]. Chirurgie de l’Avantpied. [Google Scholar]
- 2. Coleman MM, Abousayed MM, Thompson JM, Bean BA, Guyton GP. Risk factors for complications associated with minimally invasive medial displacement calcaneal osteotomy. Foot Ankle Int. 2021;42(2):121-131. doi: 10.1177/1071100720961094 [DOI] [PubMed] [Google Scholar]
- 3. Didomenico LA, Anain J, Wargo-Dorsey M. Assessment of medial and lateral neurovascular structures after percutaneous posterior calcaneal displacement osteotomy: a cadaver study. J Foot Ankle Surg. 2011;50(6):668-671. doi: 10.1053/j.jfas.2011.07.006 [DOI] [PubMed] [Google Scholar]
- 4. Donley BG, Philbin T, Tomford JW, Sferra JJ. Foot and ankle infections after surgery. Clin Orthop Relat Res. 2001;391:162-170. [DOI] [PubMed] [Google Scholar]
- 5. Durston A, Bahoo R, Kadambande S, Hariharan K, Mason L. Minimally invasive calcaneal osteotomy: does the Shannon burr endanger the neurovascular structures? A cadaveric study. J Foot Ankle Surg. 2015;54(6):1062-1066. doi: 10.1053/j.jfas.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 6. El-Sayed N, Fadel M, Yosef A, Soliman A. Medial displacement calcaneal osteotomy in treatment of stage II posterior tibial tendon deficiency. Egyptian Orthop J. 2018;53:14-20. [Google Scholar]
- 7. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2017;38(4):381-387. [DOI] [PubMed] [Google Scholar]
- 8. Gutteck N, Zeh A, Wohlrab D, Delank KS. Comparative results of percutaneous calcaneal osteotomy in correction of hindfoot deformities. Foot Ankle Int. 2019;40(3):276-281. [DOI] [PubMed] [Google Scholar]
- 9. Hunter JG, Baumhauer JF. A comparative analysis of the most common complications for patients undergoing traumatic foot and ankle surgery. Tech Foot Ankle Surg. 2017;16:86-90. [Google Scholar]
- 10. Kendal AR, Khalid A, Ball T, Rogers M, Cooke P, Sharp R. Complications of minimally invasive calcaneal osteotomy versus open osteotomy. Foot Ankle Int. 2015;36(6):685-690. [DOI] [PubMed] [Google Scholar]
- 11. Mendicino RW, Catanzariti AR, Reeves CL. Posterior calcaneal displacement osteotomy: a new percutaneous technique. J Foot Ankle Surg. 2004;43:332-335. [DOI] [PubMed] [Google Scholar]
- 12. Miller WA. Postoperative wound infection in foot and ankle surgery. Foot Ankle. 1983;4(2):102-104. [DOI] [PubMed] [Google Scholar]
- 13. Mulligan RP, McCarthy KJ, Grear BJ, Richardson DR, Ishikawa SN, Murphy GA. Preoperative risk factors for complications in elective ankle and hindfoot reconstruction. Foot Ankle Spec. 2018;11:54-60. [DOI] [PubMed] [Google Scholar]
- 14. Nordio A, Chan JJ, Guzman JZ, Hasija R, Vulcano E. Percutaneous Zadek osteotomy for the treatment of insertional Achilles tendinopathy. Foot Ankle Surg. 2020;26:818-821. [DOI] [PubMed] [Google Scholar]
- 15. Schipper ON, Jiang JJ, Chen L, Koh J, Toolan BC. Effect of diabetes mellitus on perioperative complications and hospital outcomes after ankle arthrodesis and total ankle arthroplasty. Foot Ankle Int. 2015;36(3):258-267. [DOI] [PubMed] [Google Scholar]
- 16. Talusan PG, Cata E, Tan EW, Parks BG, Guyton GP. Safe zone for neural structures in medial displacement calcaneal osteotomy: a cadaveric and radiographic investigation. Foot Ankle Int. 2015;36(12):1493-1498. [DOI] [PubMed] [Google Scholar]
- 17. Tennant JN, Carmont M, Phisitkul P. Calcaneus osteotomy. Curr Rev Musculoskelet Med. 2014;7:271-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Teoh K, Hariharan K. Minimally invasive calcaneal osteotomy: a comparison of 3 different osteotomies. Foot Ankle Orthop. 2018;3(3):2473011418. [Google Scholar]
- 19. Thomas M, Jordan M. Minimally invasive correction of lesser toe deformities and treatment of metatarsalgia. Article in German. Oper Orthop Traumatol. 2018;30:171-183. doi: 10.1007/s00064-018-0548-6 [DOI] [PubMed] [Google Scholar]
- 20. Wacker JT, Hennessy MS, Saxby TS. Calcaneal osteotomy and transfer of the tendon of flexor digitorum longus for stage-II dysfunction of tibialis posterior. Three- to five-year results. J Bone Joint Surg Br. 2002;84(1):54-58. doi: 10.1302/0301-620x.84b1.11847 [DOI] [PubMed] [Google Scholar]
- 21. Wiewiorski M, Barg A, Hoerterer H, Voellmy T, Henninger HB, Valderrabano V. Risk factors for wound complications in patients after elective orthopedic foot and ankle surgery. Foot Ankle Int. 2015;36(5):479-487. [DOI] [PubMed] [Google Scholar]
- 22. Wills B, Lee H, SR P.W. Calcaneal osteotomy safe zone to prevent neurological damage: fact or fiction? Foot Ankle Spec. 2019;12(1):34-38. [DOI] [PubMed] [Google Scholar]
- 23. Wukich DK, Crim BE, Frykberg RG, Rosario BL. Neuropathy and poorly controlled diabetes increase the rate of surgical site infection after foot and ankle surgery. J Bone Joint Surg Am. 2014;96:832-839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yassin M, Bowirat A, Robinson D. Percutaneous surgery of the forefoot compared with open technique—functional results, complications and patient satisfaction. Foot Ankle Surg. 2020;26:156-162. [DOI] [PubMed] [Google Scholar]