A 42-year-old multiparous woman presented with a 6-year history of a 2.2 cm painful, enlarging, umbilical nodule (Fig 1). She reported swelling of the nodule every 3-4 months, associated with intense pain but no bleeding or discharge.
Fig 1.

Question 1: What is the most likely diagnosis?
-
A.
Sister Mary Joseph nodule
-
B.
Keloid
-
C.
Cutaneous endometriosis
-
D.
Dermatofibrosarcoma protuberans
-
E.
Umbilical hernia
Answers:
A. Sister Mary Joseph nodule – Incorrect. Sister Mary Joseph nodule is a metastatic malignant umbilical nodule. Clinically, the nodule resembles a Sister Mary Joseph nodule. This diagnosis is less likely given the history of cyclical swelling and pain described in the case.
B. Keloid – Incorrect. Keloids occur with excessive proliferation of collagen after trauma. The absence of trauma or surgery and the presence of painful cyclical swelling make it less likely.
C. Cutaneous endometriosis – Correct. Cutaneous endometriosis is a rare condition, comprising less than 1% of endometriosis cases. The most common presentation is an umbilical nodule, which can be classified as primary or secondary based on the absence or presence of abdominopelvic surgical history, respectively.1 In a literature review, 61 published English studies of primary umbilical endometriosis were found between 2000 and 2020. The average age of the patient at the time of diagnosis was 35.7 years. The lesions averaged 1.62 cm in diameter, and the majority of lesions were brown. Blue, purple, black, and red nodules were also reported.
D. Dermatofibrosarcoma protuberans – Incorrect. Dermatofibrosarcoma protuberans (DFSP) is a rare fibrous tumor that typically grows continuously and will not have relapsing and remitting growth.
E. Umbilical hernia – Incorrect. Umbilical hernias most often occur in infants but can be acquired in adulthood. While the hernias can protrude with increased intrathoracic pressure, they are usually painless and reducible.
Question 2: Which test would be most diagnostic?
-
A.
Abdominal ultrasound
-
B.
CT scan of the abdomen and pelvis
-
C.
Laparoscopic evaluation
-
D.
Biopsy of the nodule
-
E.
MRI of the abdomen
Answers:
A. Abdominal ultrasound – Incorrect. While abdominal ultrasound can be used to diagnose and screen for complications of an umbilical hernia, it would not be diagnostic for umbilical endometriosis.
B. CT scan of the abdomen and pelvis – Incorrect. Umbilical endometriosis cannot be diagnosed on radiographic appearance alone. An abdominopelvic CT is necessary in the workup of a Sister Mary Joseph nodule to delineate the source and extent of metastatic malignancy.
C. Laparoscopic evaluation – Incorrect. Laparoscopy is the gold standard for diagnosing pelvic endometriosis but does not confirm cutaneous endometriosis. While many patients with primary umbilical endometriosis have concomitant pelvic endometriosis, the literature reveals patients with umbilical endometriosis without pelvic endometriosis.
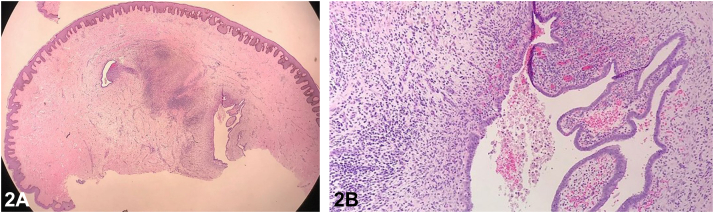
D. Biopsy of the nodule – Correct. Biopsy exhibits an acanthotic epidermis overlying ectatic glands lined by columnar-type epithelium and surrounded by endometrial-type stroma and hemosiderin-laden macrophages (Fig 2). Biopsy should be performed when cutaneous endometriosis is suspected due to the potential for malignant transformation. No malignant cells were detected in this case.
E. MRI of the abdomen – Incorrect. Magnetic resonance imaging cannot diagnose cutaneous endometriosis since radiographic findings are not diagnostic. MRI can be a useful tool for evaluating the depth of invasion of DFSP.2
Fig 2.
Question 3: What is the most appropriate treatment?
-
A.
Leuprolide acetate injections
-
B.
Surgical excision
-
C.
Mohs micrographic surgery
-
D.
Intralesional steroid injections
-
E.
Radiation therapy
Answers:
A. Leuprolide acetate injections – Incorrect. GnRH analogues such as leuprolide are second-line treatment for pelvic endometriosis but not umbilical endometriosis. A case report describes leuprolide acetate injection shrinking a nodule of umbilical endometriosis after 18 months of therapy but not complete resolution.3
B. Surgical excision of the nodule – Correct. Given the potential for malignant transformation, surgical excision remains the gold standard for treatment of cutaneous endometriosis. Recurrence after excision is very rare. The nodule in our case was removed by complete excision, and she was referred for gynecological examination for evaluation of probable pelvic endometriosis.
C. Mohs micrographic surgery – Incorrect. Mohs micrographic surgery (MMS) is unnecessary for cutaneous endometriosis, especially when no malignant cells are detected. MMS has become increasingly popular for the treatment of DFSP.4
D. Intralesional steroid injections – Incorrect. Intralesional steroid injections will not treat cutaneous endometriosis but are effective for keloids.
E. Radiation therapy – Incorrect. The diagnosis of cutaneous endometriosis does not warrant radiation therapy. Patients with a Sister Mary Joseph nodule will likely require radiation therapy or chemotherapy for treatment of the underlying malignancy.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not Applicable.
Consent for the publication of all patient photographs and medical information was provided by the authors at the time of article submission to the journal stating that all patients gave consent for their photographs and medical information to be published in print and online and with the understanding that this information may be publicly available.
References
- 1.Victory R., Diamond M.P., Johns D.A. Villar's nodule: a case report and systematic literature review of endometriosis externa of the umbilicus. J Minim Invasive Gynecol. 2007;14(1):23–32. doi: 10.1016/j.jmig.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Serra-Guillén C., Sanmartín O., Llombart B., et al. Correlation between preoperative magnetic resonance imaging and surgical margins with modified Mohs for dermatofibrosarcoma protuberans. Dermatol Surg. 2011;37(11):1638–1645. doi: 10.1111/j.1524-4725.2011.02077.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown M.E., Osswald S., Biediger T. Cutaneous endometriosis of the umbilicus (Villar's nodule) Int J Womens Dermatol. 2020;6(3):214–215. doi: 10.1016/j.ijwd.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snow S.N., Gordon E.M., Larson P.O., Bagheri M.M., Bentz M.L., Sable D.B. Dermatofibrosarcoma protuberans: a report on 29 patients treated by Mohs micrographic surgery with long-term follow-up and review of the literature. Cancer. 2004;101(1):28–38. doi: 10.1002/cncr.20316. [DOI] [PubMed] [Google Scholar]