Abstract
Introduction
School closures due to the COVID-19 pandemic affect children's daily structure, mealtimes, physical activity, and sleeping habits, possibly exacerbating weight gain, particularly in vulnerable children with overweight and obesity. This study aimed to evaluate both perceived and objectively measured weight gain in children in the Netherlands during the COVID-19 pandemic and the effect of prior lifestyle intervention.
Methods
A total of 150 children of the Children, Obesity and Lifestyle during COVID-19 (COLC) study (cohort A) reported perceptions of weight change during the COVID-19 pandemic. Anthropometric data of 65 children with overweight and obesity were collected at the expertise Centre for Overweight Adolescent and Children's Healthcare in the same period (COACH; cohort B).
Results
In cohort A, 43% of children with overweight and obesity perceived weight gain during the pandemic, compared to 15% of lean children. In cohort B, the BMI z -score increased significantly (+0.065 SD) within 5 months. Participation in a lifestyle intervention for >1 year and having parents with Dutch background was associated with less weight gain, specifically in children with obesity.
Discussion/Conclusion
In particular, children with overweight and obesity seem to be at risk for accelerated weight gain during the COVID-19 pandemic. Prior long-term participation in a lifestyle intervention protects against this weight gain, which emphasizes the importance of strong support for vulnerable populations during health crises and pleads for wide implementation of lifestyle interventions for children.
Keywords: COVID-19, Childhood obesity, Lifestyle intervention, Body mass index, Weight gain, Pediatric obesity, Quarantine
Introduction
The current pandemic, caused by the severe acute respiratory syndrome coronavirus SARS-CoV-2 (COVID-19) has far reaching consequences for human life. Among these consequences are the long-term effects of the pandemic and social distancing on the health of children. At the onset of the pandemic, experts feared that governmental restrictions could exacerbate the ongoing childhood obesity epidemic [1, 2, 3] as school environments provide structure and routine regarding mealtimes, physical activity, and sleep habits [4]. The loss of structure might negatively affect lifestyle behavior and weight development in children, particularly in those with overweight and obesity [5]. Recently published studies confirm these fears, reporting accelerated weight gain in children with healthy weight and with overweight and obesity with various outcome measures, measured in heterogeneous samples [6, 7, 8, 9, 10, 11]. A large study from Germany showed an increase in the BMI z -score of 0.06 SDS within 3 months, while a study from the USA reported a yearly increase in the BMI z -score of 0.34 SDS [8, 10]. Additionally, several international studies reported elevated screen time, a higher consumption of snacks and sugary drinks, and a decrease in physical activity during the COVID-19 lockdown [1, 4, 12]. These factors may contribute to unfavorable and unintentional weight gain. Besides these factors, studies have shown that parental education and migration background may be associated with unfavorable weight development [13, 14].
As social distancing restrictions have been periodically reinstated to control COVID-19 over the last year, which is expected to continue in the nearby future [15], it is important to obtain insight in the effects of these restrictions on lifestyle and weight development, particular in at-risk populations. Previous research has shown that children with overweight and obesity are at risk for developing cardiovascular disease, nonalcoholic fatty liver disease, and psychosocial issues already in childhood and that the risk for developing diseases later in life is even higher [16, 17, 18, 19, 20, 21]. Moreover, it has been shown that obesity is not only associated with COVID-19 severity but also increases the risk for COVID-19 infection in children [22]. Lifestyle intervention is the treatment of choice in children with overweight and obesity, resulting in significant weight loss and improvement of cardiovascular parameters [20, 21]. However, the recent literature indicates that treatment efficacy of pediatric obesity programs provided during the pandemic is markedly reduced [23]. The effect of participating in lifestyle intervention prior to the pandemic on weight gain during the pandemic, and possible protective effects, has not yet been investigated.
With insight in the effects of the COVID-19 pandemic on lifestyle, weight development, and treatment of pediatric obesity, healthcare professionals, educators, parents, and governmental officials can timely intervene, on both individual and population level, to prevent exacerbation of the obesity epidemic and associated health risks. Therefore, the aim of the present study was to evaluate perceived weight development of Dutch children of all weight categories and objective weight development of children with overweight and obesity during the COVID-19 pandemic and the effect of prior lifestyle intervention herein.
Materials and Methods
Setting and Participants
Data from two cohorts, cohort A and cohort B, were included in this study to investigate weight development of Dutch children during the COVID-19 pandemic. Cohort A (n = 150) was derived from the Children, Obesity and Lifestyle during COVID-19 (COLC) study, which is an ongoing prospective digital questionnaire study, aiming to investigate the effects of the COVID-19 pandemic on lifestyle and weight of children of all weight categories. All Dutch children, aged 4–18 years, were eligible to participate. Recruitment took place via (social) media, primary and secondary schools, and Dutch obesity expertise centers. Informed consent from all necessary parties (both parents and the child if aged ≥12 years) was obtained before inclusion.
Cohort B was derived from the Centre for Overweight Adolescent and Children's Healthcare (COACH) at the Maastricht University Medical Centre (MUMC+); COACH is an expertise center for clinical evaluation and treatment of children with overweight and obesity, providing a family-based, interdisciplinary, tailored lifestyle intervention. The setting and design of this intervention is described elsewhere [13]. Due to COVID-19 governmental measures, the center was closed between March 15th and June 1st. Sixty-five children aged between 4 and 18 years enrolled in the COACH lifestyle intervention visited the clinic before closing of the expertise center (between January 1st 2020 and March 15th 2020) and after reopening in June 2020 (between June 1st 2020 and September 1st 2020). In this period, care was continued via telephone or video consultations. Children were divided into subgroups based on whether they participated for >1 year or <1 year in the COACH intervention at their last prelockdown measurement.
Study Measurements
Perceived body weight development of children and their parents in cohort A was investigated using two digital questionnaires. A retrospective baseline questionnaire collected data on sex, age, height, body weight, and parental educational level (low, medium, high) from the pre-pandemic situation in February 2020. A second questionnaire was sent 3 weeks after the baseline questionnaire, collecting data on measured body weight and perception of weight development of both parents and children during the pandemic (May to July 2020). Self-perceived weight development was determined by asking whether the participant thought the child or parent gained, maintained, or lost weight during the COVID-19 pandemic. Parents were instructed to complete the questionnaires together with their child and to weigh and measure their child in underwear only.
To obtain insight in weight development of children with overweight and obesity and the potential effect of a lifestyle intervention, objectively measured anthropometrics from children in cohort B were analyzed. Data on sex, age, height, body weight, parent's highest education (categorized as low-medium, or high), marital status, and immigration background were extracted from medical records. Body weight was measured by a clinician using electric scales (Seca© 877, Seca, Hamburg, Germany) to the nearest 0.1 kg. Standing height was measured using a portable stadiometer (Seca© 213 stadiometer, Seca, Hamburg).
For both cohorts, body mass index (BMI) (weight [kg]/height [m]2) and age- and sex-specific BMI z -scores were calculated according to the TNO Growth Calculator (TNO, The Hague, The Netherlands). Children were allocated to one of five weight categories (underweight, normal weight, overweight, obesity, or severe obesity) based on the International Obesity Task Force (IOTF) criteria. These criteria provide age- and sex-specific BMI thresholds to distinguish between the aforementioned weight categories [24, 25].
Statistical Analyses
Data are presented as mean (SD) or median (25th–75th percentile). Normality of the data was tested with QQ-plots and Shapiro-Wilk tests or Kolmogorov-Smirnov tests where appropriate. Outliers were assessed using boxplots. One case in cohort B was removed based on an extreme, positive outlier on BMI z -score change. Missing data were not imputed. Differences between groups were assessed using Student's t tests or χ2 tests where appropriate. In cohort B, differences in BMI z -change were analyzed using univariate ANOVA with duration in lifestyle intervention (<1 year vs. > 1 year) as a between-group factor. The cutoff point of 1 year was chosen based on the previous literature on the long-term lifestyle intervention of COACH [20]. Subsequently, factors that showed significant independent associations with BMI z -score change were included as fixed factors in the ANOVA. A p value of <0.05 was considered statistically significant. Data were analyzed using SPSS version 25 (IBM, La Jolla, CA, USA).
Results
Baseline Characteristics of Children in Cohort A
In cohort A, 150 children of all ages (55.3% girls) completed the online questionnaires during the COVID-19 pandemic (specifically between May 10th 2020 and July 12th 2020). Baseline characteristics of children and their families are shown in Table 1. Self-reported weight and height from before the pandemic were available from a subgroup of children (n = 93) and parents (118 mothers and 90 fathers). The majority of children (66.7%) had a normal weight, 18.3% had underweight, and 15.1% had overweight or obesity according to the IOTF criteria. The percentage of children with overweight or obesity was similar to the Dutch population [26]. A total of 57.1% of children with overweight and obesity participated in pediatric obesity treatment programs.
Table 1.
Baseline characteristics cohort A
| Characteristics | (n = 150) | |
|---|---|---|
| Age (year) | 10.7 (7.6–13.7) | |
| Age range (year) | 4.6–18.0 | |
| Sex (% girls) | 55.3 (n = 83) | |
| Parental education level | Mothers (n = 150) | Fathers (n = 150) |
| Low | 3.3 (n = 5) | 9.3 (n = 14) |
| Medium | 29.3 (n = 44) | 29.3 (n = 44) |
| High | 66 (n = 99) | 56.0 (n = 84) |
| Not reported | 1.3 (n = 2) | 5.3 (n = 8) |
| IOTF classification | (n = 93) | |
| Underweight | 18.3 (n = 17) | |
| Normal weight | 66.7 (n = 62) | |
| Overweight/obesity | 15.1 (n = 14) |
Data are presented as percentage or median (interquartile range).
Perception of Body Weight Development in Children during the Pandemic (Cohort A)
A total of 22.0% of participants thought to have gained weight (Table 2). Within the subgroup of children with overweight and obesity, 42.9% of them thought to have gained weight, significantly more compared to 14.5% of lean children (p = 0.02). A total of 40.0% of children participating in pediatric obesity treatment programs thought to have gained weight (data not presented in tables). In the total cohort, 70.7% of participants thought to have maintained his or her body weight during the COVID-19 pandemic (Table 2). A decrease in body weight was perceived by 2.7% of the participants, and these children were either normal weight, or weight status was unknown due to missing data. None of the participants classified as having overweight or obesity reported perceived weight loss.
Table 2.
Perceived weight development of children during the COVID-19 pandemic
| Total cohort (n = 150) | Underweight (n = 17) | Normal weight (n = 62) | Overweight or obesity (n = 14) | IOTF class unknown (n = 57) | |
|---|---|---|---|---|---|
| Perception of | |||||
| Weight gain | 22.0 (n = 33) | 17.6 (n = 3) | 14.5 (n = 9) | 42.9 (n = 6) | 26.3 (n = 15) |
| Weight maintenance | 70.7 (n = 106) | 82.4 (n = 14) | 82.3 (n = 51) | 50.0 (n = 7) | 59.6 (n = 34) |
| Weight loss | 2.7 (n = 4) | None | 1.6 (n = 1) | None | 5.3 (n = 3) |
| ‘I don't know’ | 4.7 (n = 7) | None | 1.6 (n = 1) | 7.1 (n = 1) | 8.8 (n = 5) |
Data are presented as percentages and absolute numbers.
Parental Perception of Their Own Weight Development (Cohort A)
When parents were questioned on the perception of their own weight development, 27.6% of mothers and 18.0% of fathers thought they gained weight themselves during the COVID-19 pandemic, while 55.0% of mothers and 51.3% of fathers reported to think they maintained their body weight. Perceived weight loss was reported by 15.4% of mothers and 14.7% of fathers, with 2.0% of mothers and 16.0% of fathers reporting they do not know or that the question is not applicable to their family. In the subgroup of parents with overweight and obesity (47 mothers and 48 fathers), perceived weight gain was reported significantly more often: 38.3% and 25.0% of mothers and fathers thought they gained weight, compared to 19.1% and 4.8% in the normal weight group (p = 0.02 and p = 0.01).
Within the subgroup of children with overweight and obesity, significantly more parents perceived weight gain in themselves (57.1%), compared to only 27.4% of parents with children with normal weight (p = 0.03). Within families reporting perceived weight gain for at least one parent (n = 55), 32.7% of children also perceived weight gain during the COVID-19 lockdown. This is significantly more compared to 15.8% of children that perceived weight gain, in families with both parents reporting maintaining or losing weight (p = 0.02).
Objective Weight Development in Children with Overweight or Obesity (Cohort B)
A total of 65 children visited the COACH expertise center within 3 months before the COVID-19 lockdown (baseline) and returned for a follow-up visit after the lockdown, between June 1st and September 1st. Of these children, 32.3% were classified as overweight, and 67.7% were classified as having obesity or severe obesity. Baseline characteristics of children in cohort B are presented in Table 3. Time between measurements was 5.0 (±1.1) months. A total of 61.5% (n = 40) of children with overweight or (severe) obesity had an increase in the BMI z -score (+0.18 SDS [±0.13]; p < 0.001) compared to before the COVID-19 pandemic, when measured objectively at the outpatient clinic. A total of 38.5% (n = 25) of the children maintained or had a decrease in the BMI z -score (−0.12 SDS [±0.14]; p < 0.001). Overall, the mean BMI z -score of children in cohort B increased by 0.065 SDS (±0.20) during the first 5 months of the pandemic (p = 0.01).
Table 3.
Baseline characteristics cohort B
| Characteristic | Total cohort (n = 65) | Duration of LI |
||||
|---|---|---|---|---|---|---|
| <1 year (n = 28) | >1 year (n = 37) | |||||
| Age, year | 12.42 (2.79) | 12.09 (2.71) | 12.67 (2.87) | |||
| Age range, year | 6.11–17.31 | 6.86–17.26 | 6.11–17.31 | |||
| Sex (% girls) | 52.3 (n = 34) | 60.7 (n = 17) | 45.9 (n = 17) | |||
| BMI z-score | 3.06 (0.66) | 2.93 (0.68) | 3.16 (0.63) | |||
| IOTF classification* | ||||||
| Overweight | 32.3 (n = 21) | 50.0 (n = 14) | 18.9 (n = 7) | |||
| (Severe) obesity | 67.7 (n = 45) | 50.0 (n = 14) | 81.1 (n = 30) | |||
| Immigration background | ||||||
| Both parents Dutch | 66.2 (n = 43) | 60.7 (n = 17) | 70.3 (n = 26) | |||
| At least one parent non-Dutch | 33.8 (n = 22) | 39.3 (n = 11) | 29.7 (n = 11) | |||
| Highest education level parents | Mothers (n = 57) | Fathers (n = 54) | Mothers (n = 22) | Fathers (N = 22) | Mothers (n = 35) | Fathers (N = 32) |
| Low | 38.6 (n = 22) | 37.0 (n = 20) | 40.9 (n = 9) | 45.5 (n = 10) | 37.1 (n = 13) | 31.3 (n = 10) |
| Medium | 42.1 (n = 24) | 37.0 (n = 20) | 40.9 (n = 9) | 36.4 (n = 8) | 42.9 (n = 15) | 37.5 (n = 12) |
| High | 19.3 (n = 11) | 25.9 (n = 14) | 18.2 (n = 4) | 18.2 (n = 4) | 20.0 (n = 7) | 31.3 (n = 10) |
Data are presented as percentage or mean (SD). LI, lifestyle intervention. p < 0.05 was considered statistically significant.
Significant difference of the proportion of children with (severe) obesity between the >1 year or <1 year LI groups.
Influencing Factors on BMI Z -Score Change (Cohort B)
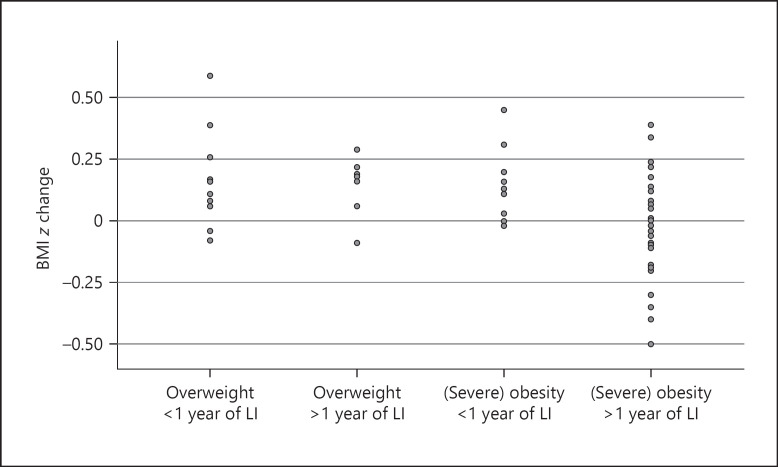
Children who participated >1 year in the lifestyle intervention prior to the pandemic gained less weight compared to children who participated <1 year (BMI z -change +0.02 SDS [0.20] vs. +0.13 SDS [0.17]; p = 0.02) (Fig. 1). Immigration background was found to be a significant determinant of BMI z -score change after adjusting for intervention duration and IOTF status (p = 0.03). Sex, age, and parental marital status were not significantly associated with BMI z -score change (p = 0.82, p = 0.94, p = 0.51, respectively). When compared to a low-medium education level, a high parental education level showed a trend toward a negative association with BMI z -score change (mean difference 0.11 [SD 0.06], p = 0.06).
Fig. 1.
BMI z -score change by subgroups of duration of LI and IOTF category during the COVID-19 pandemic. Children with (severe) obesity and who were >1 year in the intervention showed less weight gain during the pandemic compared to children who received <1 year intervention. LI, lifestyle intervention.
Post hoc comparisons in the subgroup of children with (severe) obesity showed that >1 year of participation in lifestyle intervention effectively prevented weight gain during the pandemic (−0.01SDS [0.21] versus +0.14 SDS [0.16], p = 0.02), compared to <1 year of participation. No such difference was seen in children with overweight (0.14 SDS [0.12] versus 0.12 SDS [0.19], p = 0.76) (Table 4). Children with two Dutch parents (n = 31) showed a BMI z -score change of −0.01 (0.20) compared to +0.14 (0.17) in children who had at least one parent from non-Dutch descent (n = 13) (p = 0.02). ANOVA analysis confirmed both duration of >1 year of intervention (mean difference −0.14, p = 0.02) and immigration background (mean difference 0.14, p = 0.03) as independent predictors of BMI z -score change in the subgroup of children with (severe) obesity.
Table 4.
BMI z-score change by duration of LI and IOTF category during the COVID-19 pandemic
| Duration of LI |
p value | ||
|---|---|---|---|
| <1 year | >1 year | ||
| Total cohort | 0.13 (0.17) (p = 0.001^) (n = 28) | 0.02 (0.20) (p = 0.65^) (n = 37) | 0.02* |
| Overweight | 0.12 (0.19) (p = 0.04^) (n = 14) | 0.14 (0.12) (p = 0.02^) (n = 7) | 0.76 |
| (Severe) obesity | 0.14 (0.16) (p = 0.01^) (n = 14) | −0.01 (0.21) (p = 0.70^) (n = 30) | 0.02* |
Data are presented as mean (SD). LI, lifestyle intervention. Time between measurements was not significantly different between groups <1 and >1 year in intervention. ^Paired-sampled t test of the BMI z-score before and after lockdown within the subgroup. p < 0.05 is considered statistically significant.
p < 0.05 is considered statistically significant.
Discussion
This study describes both perceived and objectively measured weight gain in children with and without overweight and obesity during the COVID-19 pandemic and the effect of lifestyle intervention on this weight gain. A total of 43% of children participating in cohort A with overweight and obesity perceived weight gain during the first COVID-19 lockdown in the Netherlands, compared to only 15% of children with normal weight. This perceived weight gain was confirmed with repeated objective measurements in a cohort of children with overweight and obesity (cohort B): 62% of these children showed a significant increase in the BMI z -score during the first 5 months of the pandemic. Our results strengthen the findings from previous studies, reporting both accelerated weight gain in children of different weight categories during the COVID-19 pandemic and an increase in prevalence of overweight and obesity among Dutch children aged 4–16 years (as reported by Statistics Netherlands) [2, 6, 7, 8, 9, 10, 11, 27] Notwithstanding, some of these studies reported mixed results on the subgroup of children with overweight. While Weaver et al. [9] reported no acceleration in BMI z -score change for children with overweight or obesity, Vogel et al. [8] reported children with obesity as a risk group for increased BMI z -score change during COVID-19. Our study strengthens these last findings, by reporting more data for children with obesity as a possible risk group for weight gain during COVID-19. While a BMI z -score difference of 0.06 seems small, this increase was measured in a vulnerable population in a short period of time. It is alarming to notice that children with overweight and obesity gained more weight during the pandemic as the risk for complications such as hypertension and high total cholesterol increases with an increasing BMI z -score in children [28]. Nutrition and physical activity changes are most likely the underlying factors for weight change in children during the lockdown, with studies reporting lower levels of physical activity and diet quality, more snacking, and increased screen time [1, 4, 12, 29].
Fortunately, this study also provides direction on how to address this challenging problem. Our data indicate that >1 year participation in a lifestyle intervention makes children with (severe) obesity less susceptible to weight gain during an unexpected event such as a lockdown. We believe this protective effect to be the result of improved skills in coping with (unexpected) situations that interfere with normal daily structure and behavior, such as holidays, life events or COVID-19-related restrictions. This is an important objective of the lifestyle intervention offered by the COACH expertise center, in addition to supporting healthy nutrition and physical activity [20]. Besides underlining the importance of targeting coping with unexpected situations during lifestyle interventions, our results also show that long-term lifestyle intervention, more than 1 year, is necessary for developing those skills in such a way that it can protect from weight gain during a crisis like the COVID-19 pandemic.
Accelerated weight gain could not be prevented in children who participated <1 year in our lifestyle intervention. These results are in agreement with outcomes of Appelhans et al. [23] who reported an increase in the BMI z -score in children with overweight and obesity measured 6 and 12 months after participation in a lifestyle intervention during the COVID-19 pandemic. Although weight gain might be reduced or other positive effects of the guiding of children and families might be present, short-term lifestyle intervention seems to be insufficient to halt accelerated weight gain during the COVID-19 pandemic. Altogether, these results plead for long-term guidance in lifestyle change for children with overweight and obesity and their families.
Although our results and those of others demonstrate an aggravation of the childhood obesity epidemic [7, 11], the actual scope of the problem might be even larger than previously reported. Children with overweight and obesity included in these studies mostly participated in lifestyle interventions. Despite this, they showed a significant increase in the BMI z -score during the COVID-19 pandemic. Children with overweight and obesity in the general population may not have access to or receive lifestyle intervention, possibly making these children without guidance more vulnerable to the challenging conditions of a lockdown. These at-risk children may demonstrate a comparable or even greater increase in the BMI z -score during the COVID-19 pandemic. Furthermore, the increase in weight might be larger than reported by parents as parents often underestimate the weight status of their child [30]. A recent meta-analysis supports this hypothesis, reporting substantial body weight gain and significantly elevated BMI z -scores in healthy children during lockdowns, compared to before the pandemic [31].
The association of immigration background and the parental educational level with BMI z -score change found in this study emphasizes the role of family factors in weight management of children during unexpected situations such as lockdowns. Parental education, immigration background, home environment, and parenting style are known to predict weight-related behaviors in children [13, 32]. Therefore, not only during a possible new lockdown situation but also in other challenging situations in children's daily life, it is important to pay attention to these factors and identify vulnerable groups who require additional support. Besides the aforementioned immutable factors, other factors that could affect lifestyle habits in children with overweight and obesity during crisis situations might be at play. Further research is needed to identify these factors in depth. These data would not only provide knowledge about family risk factors during the pandemic but also provide valuable information for optimization of lifestyle interventions for children with overweight and obesity in case of unexpected life events after the pandemic.
A major strength and novelty of this study is the collection of both subjectively and objectively measured data in children of all weight categories, early in the COVID-19 pandemic. Although body weight and height in cohort A were self-reported and therefore prone to subjectivity and possible inconsistencies, it yields important information that could not have been obtained another way. National regulations did not allow for weight monitoring at outpatient clinics during lockdown. The resultshighlight the importance of (regular) anthropometric monitoring by healthcare professionals as parental monitoring might not be accurate. A limitation of this study could be the higher proportion of parents with a high education level in cohort A, which might have introduced some selection bias. Also, the number of children with overweight who already received guidance through a lifestyle intervention was high. Another limitation could be the small sample size and relatively short timeframe between pre- and post-BMI z -scores in the objectively measured data. However, it is telling that even considering this, our data clearly demonstrate health risks for this vulnerable population.
Conclusions
Our study describes both self-perceived and objectively measured accelerated weight gain in children with overweight and obesity during the COVID-19 pandemic and is the first study investigating the role of previously perceived lifestyle intervention. These findings represent an evolving vicious circle, in which the COVID-19 pandemic and the childhood obesity pandemic meet and reinforce each other, putting the (future) health of these children at risk through increasing prevalence of comorbidities such as nonalcoholic fatty liver disease, diabetes type 2, and cardiovascular disease. However, our results also indicate that prolonged participation in a multidisciplinary lifestyle intervention can prevent weight gain during unexpected situations, providing possibilities for the designs of current and future lifestyle interventions. Furthermore, it underlines the importance of strong support of vulnerable populations during crises like this pandemic and pleads for the acceleration of wide implementation of lifestyle interventions for children. With the pandemic ongoing, it is essential that awareness for the need of a healthy lifestyle of children increases among parents and healthcare providers, and pitfalls unique to the current situation are addressed to ensure the future health of children. Further research is planned to evaluate long-term effects of the COVID-19 pandemic on lifestyle of children with overweight and obesity. More qualitative insight in factors influencing the lifestyle of children, such as home environment, daily structure, and parental support and coping strategies during and after the COVID-19 pandemic will be obtained.
Statement of Ethics
Data of the COLC-study (cohort A) were obtained within local regulations of the hospital and Medical Ethical Committee and the Kijk op Overgewicht study (METC 13-4-130, Clinicaltrial.gov (NCT02091544)). Ethical approval for the COLC-study was provided by the Medical Ethics Committee of the Maastricht University Medical Centre+ (METC2020-1330-A-1, Clinicaltrial.gov NCT04411511). Written informed consent was obtained from all the participants and their parents or legal guardians where appropriate. For cohort B, data were obtained within local regulations of the hospital. The Medical Ethics Committee of the Maastricht University Medical Centre stated that this research did not fall under the scope of the Medical Research Involving Human Subjects Act (WMO), and therefore, no ethical approval was needed (METC2022-3105).
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Judith Lubrecht, Lisanne Arayess, Marijn Hesselink, Gabrielle ten Velde, and Anita C.E. Vreugdenhil designed the study. Judith Lubrecht, Lisanne Arayess, Arieke Janse, Ines von Rosentiel, Edgar G.A.H. van Mil, Marjoke Verweij, and Anita C.E. Vreugdenhil contributed to data collection. Judith Lubrecht, Lisanne Arayess, and Dorien Reijnders analyzed and interpreted the data and wrote the manuscript. Anita C.E. Vreugdenhil has primary responsibility for the final content. All the authors read and approved the final version of the manuscript for publication.
Data Availability Statement
The datasets generated and analyzed during this study are not publicly available as participants in this study did not give consent to do so. Data can be made available from the corresponding author through data sharing agreements on request.
Acknowledgments
The authors would like to acknowledge all involved children and parents for their participation and M.L. Swanink for her contribution to data extraction from patients' files from the Centre for Overweight Adolescent and Children's Healthcare.
References
- 1.Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28((8)):1382–5. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity. 2020;28((6)):1008–9. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9((4)):302–12. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll N, Sadowski A, Laila A, Hruska V, Nixon M, Ma DWL, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income canadian families with young children. Nutrients. 2020;12((8)):2352. doi: 10.3390/nu12082352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Hippel PT, Workman J. From kindergarten through second grade, U.S. children's obesity prevalence grows only during summer vacations. Obesity. 2016;24((11)):2296–300. doi: 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- 6.Vinker-Shuster M, Grossman ES, Yeshayahu Y. Increased weight gain of children during the COVID-19 lockdown. Isr Med Assoc J. 2021;23((4)):219–22. [PubMed] [Google Scholar]
- 7.Beck AL, Huang JC, Lendzion L, Fernandez A, Martinez S. Weight gain during the COVID-19 pandemic in a high-risk cohort of children in San Francisco, CA. Child Obes. 2022;18((2)):143–6. doi: 10.1089/chi.2021.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vogel M, Geserick M, Gausche R, Beger C, Poulain T, Meigen C, et al. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes. 2022;46((1)):144–52. doi: 10.1038/s41366-021-00968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weaver RG, Hunt ET, Armstrong B, Beets MW, Brazendale K, Turner-McGrievy G, et al. COVID-19 leads to accelerated increases in children's BMI z-score gain: an interrupted time-series study. Am J Prev Med. 2021;61((4)):e161–9. doi: 10.1016/j.amepre.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azoulay E, Yackobovitch-Gavan M, Yaacov H, Gilboa I, Lopez A, Sheppes T, et al. Weight status and body composition dynamics in children and adolescents during the COVID-19 pandemic. Front Pediatr. 2021;9:707773. doi: 10.3389/fped.2021.707773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stavridou A, Kapsali E, Panagouli E, Thirios A, Polychronis K, Bacopoulou F, et al. Obesity in children and adolescents during COVID-19 pandemic. Children. 2021;8((2)):135. doi: 10.3390/children8020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ten Velde G, Lubrecht J, Arayess L, van Loo C, Hesselink M, Reijnders D, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: pre-, during- and post-school closures. Pediatr Obes. 2021;16((9)):e12779. doi: 10.1111/ijpo.12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dannemann A, Ernert A, Rucker P, Babitsch B, Wiegand S. [The influence of migration background and parental education on childhood obesity and the metabolic syndrome] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011;54((5)):636–41. doi: 10.1007/s00103-011-1258-5. [DOI] [PubMed] [Google Scholar]
- 14.Nederlands Centrum voor Jeugdgezondheid . JGZ richtlijn: Overgewicht. 2012. Available from https://www.ncj.nl/richtlijnen/alle-richtlijnen/richtlijn/overgewicht Accessed April 1, 2022. [Google Scholar]
- 15.Iftekhar EN, Priesemann V, Balling R, Bauer S, Beutels P, Calero Valdez A, et al. A look into the future of the COVID-19 pandemic in Europe: an expert consultation. Lancet Reg Health Eur. 2021;8:100185. doi: 10.1016/j.lanepe.2021.100185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Umer A, Kelley GA, Cottrell LE, Giacobbi P, Jr, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17((1)):683. doi: 10.1186/s12889-017-4691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karnebeek K, Thapar S, Willeboordse M, van Schayck OCP, Vreugdenhil ACE. Comorbidities in primary versus secondary school children with obesity and responsiveness to lifestyle intervention. J Clin Endocrinol Metab. 2019:jc.2018–02318. doi: 10.1210/jc.2018-02318. [DOI] [PubMed] [Google Scholar]
- 18.Rijks J, Karnebeek K, van Dijk JW, Dorenbos E, Gerver WJ, Stouthart P, et al. Glycaemic profiles of children with overweight and obesity in free-living conditions in association with cardiometabolic risk. Sci Rep. 2016;6:31892. doi: 10.1038/srep31892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rijks JM, Plat J, Dorenbos E, Penders B, Gerver WM, Vreugdenhil ACE. Association of TSH with cardiovascular disease risk in overweight and obese children during lifestyle intervention. J Clin Endocrinol Metab. 2017;102((6)):2051–8. doi: 10.1210/jc.2016-3057. [DOI] [PubMed] [Google Scholar]
- 20.Rijks JM, Plat J, Mensink RP, Dorenbos E, Buurman WA, Vreugdenhil AC. Children with morbid obesity benefit equally as children with overweight and obesity from an ongoing care program. J Clin Endocrinol Metab. 2015;100((9)):3572–80. doi: 10.1210/jc.2015-1444. [DOI] [PubMed] [Google Scholar]
- 21.Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102((3)):709–57. doi: 10.1210/jc.2016-2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hernández-Garduño E. Comorbidities that predict acute respiratory syndrome coronavirus 2 test positivity in Mexican children: a case-control study. Pediatr Obes. 2020;16:e12740. doi: 10.1111/ijpo.12740. [DOI] [PubMed] [Google Scholar]
- 23.Appelhans BM, French SA, Martin MA, Lui K, Janssen I. Attenuated efficacy of pediatric obesity treatment during the COVID-19 pandemic. Obesity. 2021;30((1)):45–9. doi: 10.1002/oby.23313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.TNO Growth calculator for youth healthcare in the Netherlands. 2020. Available from https://tnochildhealthstatistics.shinyapps.io/JGZRichtlijnLengtegroei/ Accessed January 18, 2022.
- 25.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7((4)):284–94. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 26.Ministerie van Volksgezondheid Overgewicht > cijfers & context > huidige situatie >Overgewicht kinderen. 2020. Available from https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-context/huidige-situatie#node-overgewicht-kinderen (Accessed January 18, 2022)
- 27.Nederlands Jeugdinstituut Cijfers over overgewicht. 2022. Available from https://www.nji.nl/cijfers/overgewicht#:∼:text=In%202020%20had%2013%2C2,procent%20en%2014%2C7%20procent (Accessed April 1, 2022)
- 28.Bell LM, Byrne S, Thompson A, Ratnam N, Blair E, Bulsara M, et al. Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. J Clin Endocrinol Metab. 2007;92((2)):517–22. doi: 10.1210/jc.2006-1714. [DOI] [PubMed] [Google Scholar]
- 29.Welling MS, Abawi O, van den Eynde E, van Rossum EFC, Halberstadt J, Brandsma AE, et al. Impact of the COVID-19 pandemic and related lockdown measures on lifestyle behaviors and well-being in children and adolescents with severe obesity. Obes Facts. 2022;15((2)):186–96. doi: 10.1159/000520718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruiter ELM, Saat J, Molleman GRM, Fransen GAJ, van der Velden K, van Jaarsveld CHM, et al. Parents' underestimation of their child's weight status. Moderating factors and change over time: a cross-sectional study. PloS one. 2020;15((1)):e0227761. doi: 10.1371/journal.pone.0227761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang THCY, Chen WY, Chen CY, Hsu WY, Chou Y, Chang YH. Weight gain associated with COVID-19 lockdown in children and adolescents: a systematic review and meta-analysis. Nutrients. 2021;13((10)):3668. doi: 10.3390/nu13103668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehdizadeh A, Nematy M, Vatanparast H, Khadem-Rezaiyan M, Emadzadeh M. Impact of parent engagement in childhood obesity prevention interventions on anthropometric indices among preschool children: a systematic review. Child Obes. 2020;16((1)):3–19. doi: 10.1089/chi.2019.0103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during this study are not publicly available as participants in this study did not give consent to do so. Data can be made available from the corresponding author through data sharing agreements on request.