Abstract
Introduction
Lymphoepithelial cysts (LECs) are extremely uncommon disorders with pancreatic affection. It is predominant in middle-aged men and may be located in any portion of the pancreas. Differential diagnosis with malignant conditions is difficult.
Case presentation
A 53-year-old woman with abdominal pain and cystic lesion involving pancreas managed thorugh laparoscopic excision and colecistectomy due to chronic cholecystitis.
Discussion and conclusion
LECs are a type of true cysts that may occur in any portion of the pancreas, most common sites are the tail and body, with unclear pathogenesis. Accuracy in diagnosis with proper image investigation is necessary to separate surgical cases from conservatively managed.
Keywords: Lymphoepithelial cyst, Pancreas, Laparoscopy, Abdominal pain
Highlights
-
•
Lymphoepithelial cysts are uncommon conditions with pancreatic affection.
-
•
Pancreatic lymphoepithelial cysts are benign cysts with higher predominance in middle-aged men (4:1).
-
•
It may affect any portion of the pancreas, however the tail or body are the most common sets.
-
•
Its diagnosis it is only possible through histopathological analysis and neoplasms must be included as differential diagnosis.
1. Introduction
Lymphoepithelial cysts (LECs) are rare benign pancreatic lesions and account for approximately less than 0.5% of all cystic manifestations of the pancreas. There is no difference in frequency of LECs related with pancreatic head, body or tail and it is not possible to differ from other types of cystic lesions, including neoplasms [[1], [2], [3]].
There is a belief of LECs predominance in middle-aged men, however several cases have been reported in women. Their presentation may be as unilocular or multilocular lesion and located in any part of the pancreas [1,3].
LECs are benign lesions without malignant potential and its diagnosis confirmation is only possible through histopathological analysis. High suspicious and imaging investigation are fundamental for intervention [1,4].
We report a case of 53-year-old woman with pancreatic cyst affecting second duodenal portion and the biliary tract, surgically managed through laparoscopy with cyst excision and cholecystectomy.
2. Case presentation
A 53-year-old Brazilian woman first attended to her medical appointment in the Oncologic and General Surgery due to pain in right flank with pelvic irradiation. An abdominal ultrasound evidenced cystic image in upper abdomen located between head of the pancreas and gallbladder measuring 6.6 × 3.5 × 5.9 cm.
She reported worsened of the pain after feeding and denied any drug history or allergies. In her previous pathological history, she reported lipoma exeresis, cesareans, eye surgery and hemorrhoidectomy. A family history of lymphoma and skin cancer were stated. Other comorbidities and drug allergy were denied.
At first examination, the patient was stable, afebrile, acyanotic and anicteric, vital signs in normal values and physical exam with plan, flaccid abdomen, painful in right hypochondrium palpation with no peritoneal irritation.
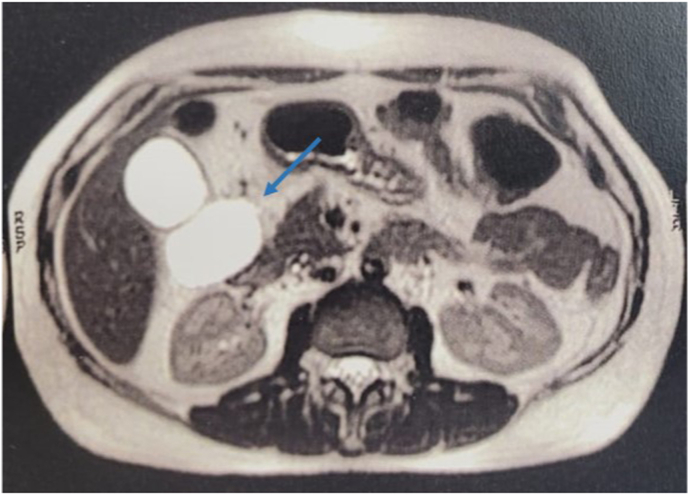
She was submitted to an abdominal and pelvic magnetic resonance (MRI) that revealed long shaped cystic formation with thin walls and no septations (Fig. 1). Its content was homogenous liquid in contact with gallbladder, duodedum second part and uncinated process of the pancreas, measuring 6.5 × 2.9 × 5.6 cm.
Fig. 1.
Axial abdominal MRI showing hypersigned image in pancreatic topography (blue arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
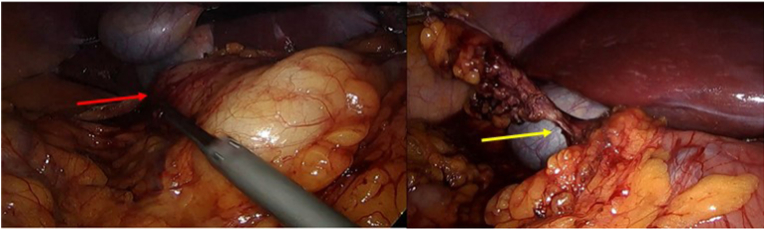
Surgical intervention through laparoscopy was first choice treatment with cyst excision and cholecystectomy due to intermittent pain in right hypochondrium performed by digestive tract surgeons and general surgeons. Intra-operatory findings were presence of cystic lesion originated in uncinated process of the pancreas and measuring approximately 12 cm with clear liquid content (Fig. 2A). Kocher maneuver was performed in the cholecystectomy with Sonicision clamp followed by cyst dissection and removal. The cyst was connected to the head of the pancreas by a peduncle (Fig. 2B) and a linear clamp was used to separate it during cyst resection. Blake drain was positioned in the right hypochondrium. She was submitted to a new MRI after surgery (Fig. 3).
Fig. 2.
A. Intra-operatory image showing cystic lesion (red arrow).B. Cystic lesion pulled revealing peduncule formation connecting it to the head of the pancreas (yellow arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
Post-operative MRI.
Histopathological analysis revealed lymphoepithelial cyst of the pancreas associated with smooth biliary congestion and chronic cholecystitis with cholesterolosis. In first post-operative day, the patient reported intense headache and one emetic episode with improvement after medication. She accepted oral diet and evolved feverless. Immune depression or autoimmune conditions were not stated before or even after procedure. Blake drain presented 30 mL of serosanguineous liquid. She was discharged two days after surgery. The follow-up remained for one year, with drain removal in the seventh post-operative day. She evolved asymptomatic since last appointment.
3. Discussion
Pancreatic lymphoepithelial cysts are benign cysts affecting predominantly middle-aged men in a proportion of 4:1 and may occur in any portion of the pancreas, most common in the tail or body [[1], [2], [3],5]. Our case presents a female patient, rarer than usual, with affection of the uncinated process of the pancreas.
Pancreactic cysts can be classified into true cysts, pseudocysts and cystic neoplasms with no differential in preoperative presentation. LECs are a type of true cysts and its content usually presents as white colored, which is compatible with our case [6].
Its pathogenesis is still undertermined with several hypotheses such as squamous metaplasia of pancreatic ducts and epithelial remant in lymphnodes. Due to its rarity and recent reports in literature, there is a low characterization of the lesion, however keratinized epithelium with lymphoid tissue and dense material are some histological features [4,7].
Literature estimates that 50% of LECs cases are incidental diagnosis. Meanwhile, symptomatic patients evidenced abdominal pain, nausea, vomiting, weight loss and diarrhea [7,8]. In our case, the patient presented only with abdominopelvic pain worsened after food ingestion.
Imaging investigation of pancreatic cystic lesions included computed tomography (CT) or magnetic resonance imaging (MRI). Ultrasonography may mislead diagnosis while CT or MRI are better to bound the lesion and characterize it from unilocular or mutilocular and determine its content as liquid or solid. MRI usually presents LECs with hypointensity on T1-weighted images and hyperintensity on T2-weighted images [1,3,9]. Due to cyst extension in our case and involvement of adjacents structures such as biliary system and duodenum, preoperative findings in MRI suggested its origin from duodenum and only in intraoperatory was possible to characterize it as from the uncinated process of the pancreas.
Fine-needle aspiration (FNA) biopsy with cytological analysis is a current option for differential diagnosis of LEC and avoidance of surgery. However, sensitivity and specificity can be decreased due to lack of cytopathologic material and presence of mucin or high level tumor markers, respectively, which may lead to an incorrect diagnosis [1,4,7].
Preoperative diagnosis based on clinical and image presentation is difficult due to lack of knowledge about the lesion and differential from malignant lesions. Surgical excision and histopathological analysis is the gold standard for LECs diagnosis. Differential diagnosis includes other benign lesions such as dermoid cyst or neoplasms, such as serous or mucinous cystic neoplasms and in our case may include duodenal duplication in cystic and non-communicating form due to MRI report [2,4,10].
Asymptomatic LECs are managed conservatively, surgery is indicated in symptomatic patients and when malignancy cannot be excluded. Surgical resection through laparoscopy is well-indicated for these cases with excellent patient recovery. Endocoscopic ultrasound FNA has been reported in successfully management of LECs in symtopmatic patients with lumen occlusion by metal stent [4,7,11,12].
This case report is being reported in line with the SCARE 2020 criteria [13].
4. Conclusion
LECs are rare benign disorders with high difficult differential diagnosis with malignant conditions. High suspicious and proper investigation through image exams and cytological analysis are fundamental for diagnosis and management. Accuracy in diagnosis is necessary to avoid unneeded surgical intervention.
4.1. Patient perspective
The patient reported in the follow-up she was grateful for the problem solution after surgery and that he could go back to her activities without any of previous difficulties.
Ethical approval
This study was exempt from ethnical approval.
Sources of funding for your research
This paper did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Aline Pereira da Costa: study concept, data collection, writing the paper.
Daniel Lourenço Lira: study concept and data collection.
Higino Felipe Figueiredo: study concept and data collection.
Matheus Alecrim Alexandre: study concept and data analysis.
Gustavo Lopes de Castro: study concept, data collection, writing the paper and design.
Jozyel Castro Cláudio: writing the paper and design.
Registration of research studies
Name of the registry:
Unique Identifying number or registration ID:
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
Each named author has no conflict of interest, financial or otherwise.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104117.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Groot V.P., Thakker S.S., Gemenetzis G., et al. Lessons learned from 29 lymphoepithelial cysts of the pancreas: institutional experience and review of the literature. HPB. 2018;20(7):612–620. doi: 10.1016/j.hpb.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Adsay N.V., Hasteh F., Cheng J.D., Bejarano P.A., Lauwers G.Y., Batts K.P., et al. Lymphoepithelial cysts of the pancreas: a report of 12 cases and a review of the literature. Mod. Pathol. 2002;15:492–501. doi: 10.1038/modpathol.3880553. [DOI] [PubMed] [Google Scholar]
- 3.Namba Y., Oshita A., Nishisaka T., et al. Lymphoepithelial cyst of the pancreas: a case report and summary of imaging features of pancreatic cysts. Int J Surg Case Rep. 2019;55:192–195. doi: 10.1016/j.ijscr.2019.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arumugam Prabhu& Fletcher, Natalie Kyriakides, Charis & Mears Lisa, Kocher Hemant. Lymphoepithelial cyst of the pancreas. Case Reports in Gastroenterology. 2016 doi: 10.1159/000445373. 10. 181-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdelkader A., Hunt B., Hartley C.P., Panarelli N.C., Giorgadze T. Cystic lesions of the pancreas: differential diagnosis and cytologic-histologic correlation. ArchPatholLab Med. 2020;144(1):47–61. doi: 10.5858/arpa.2019-0308-RA. [DOI] [PubMed] [Google Scholar]
- 6.Ryu D.H., Sung R.H., Kang M.H., Choi J.W. Lymphoepithelial cyst of the pancreas mimicking malignant cystic tumor: report of a case. Korean J. Hepatobiliary Surg. 2015;19:129–132. doi: 10.14701/kjhbps.2015.19.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capitanich P., Iovaldi M.L., Medrano M., et al. Lymphoepithelial cysts of the pancreas: case report and review of the literature. J. Gastrointest. Surg. 2004;8(3):342–345. doi: 10.1016/j.gassur.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Strapko A., Botash R., Murthy U., Landas S. Lymphoepithelial cyst of the pancreas: a case report and review of the literature. Dig. Dis. Sci. 1998;43:870–874. doi: 10.1023/a:1018842820499. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto K., Fujimoto K., Matsushiro T. Lymphoepithelial cyst of the pancreas: a case report. Gastroenterol. Jpn. 1990;25:758–761. doi: 10.1007/BF02779192. [DOI] [PubMed] [Google Scholar]
- 10.Clemente G., Sarno G., De Rose A.M., et al. Lymphoepithelial cyst of the pancreas: case report and review of the literature. Acta GastroenterolBelg. 2011;74(2):343–346. [PubMed] [Google Scholar]
- 11.Chowdhry M., Bilal M., Shah H., Clanton J., Singh S. Large lymphoepithelial cyst of pancreas: a rare entity managed using lumen-apposing metal stent-case report and review of the literature. Clin J Gastroenterol. 2019;12(6):609–614. doi: 10.1007/s12328-019-00982-y. [DOI] [PubMed] [Google Scholar]
- 12.Komura T., Kagaya T., Orita N., et al. Imaging features and pathological evaluation by EUS-FNA enable conservative management in patient of lymphoepithelial cyst of the pancreas: a case report. Clin J Gastroenterol. 2021;14(1):370–374. doi: 10.1007/s12328-020-01240-2. [DOI] [PubMed] [Google Scholar]
- 13.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAseREport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.