Objectives
The COVID-19 pandemic has placed unprecedented strain on healthcare systems and may have consequential impacts on patient safety incidents (PSIs). The primary objective of this study was to examine the impact of the COVID-19 pandemic on PSIs reported in Niagara Health.
Methods
Flexible Farrington models were used to retrospectively detect weeks from January to September 2020 where PSI counts were significantly above expected counts. Incident counts were adjusted to weekly inpatient-days. Outcomes included overall incident numbers, incidents by category, and incidents by ward type.
Results
The overall number of PSIs across Niagara Health did not increase during the first wave of the COVID-19 pandemic. However, significant increases in falls were observed, suggesting that other types of incidents decreased. Falls increased by 75% from February to March 2020, coinciding with the onset of the first wave of the pandemic. Further investigation by unit type revealed that the number of falls increased specifically on internal medicine and complex continuing care wards.
Conclusions
Despite no observed changes in overall number, significant composition shifts in PSIs occurred during the first wave of the COVID-19 pandemic, with increased falls on internal medicine and complex continuing care wards. Possible explanations include restrictions on patient visitation, reduced patient contact/supervision, and/or personal protective equipment requirements. Providers should maintain a particularly high vigilance for patient falls during pandemic outbreaks, and hospitals should consider targeting resources to higher-risk locations. The results of this study reinforce the need for ongoing pandemic PSI monitoring and rapidly adaptive responses to new patient safety concerns.
Key Words: COVID-19, pandemic, infectious disease, outbreak, incident reporting systems, patient safety incidents, falls, falls prevention, internal medicine, geriatrics, complex continuing care, personal protective equipment, patient safety
Nearly 20 years ago, the U.S. Institute of Medicine’s Too Err Is Human and the English Department of Health’s An Organization With a Memory demonstrated the prevalence and impact of medical errors within healthcare systems.1,2 Unfortunately, decades later, patient safety incidents (PSIs) continually plague healthcare organizations globally. In 2017, the Organization for Economic Cooperation and Development noted that 1 in every 10 patient encounters with the healthcare system results in patient harm, and that PSIs constitute about 14% of the global disease burden, comparable to diseases such as tuberculosis and malaria.3 In Canada, PSIs were estimated to be the third leading cause of death after cancer and heart disease, with less than 28,000 deaths in 2013.4
Data on the occurrence, frequency, types, causes, and clinical outcomes of PSIs are crucial for prevention.5 Recently, healthcare organizations have focused on incident reporting systems (IRSs) as a means of detecting and preventing PSIs. Incident reporting systems are typically voluntary, anonymous, nonpunitive, and confidential electronic systems that rely on real-time data from health providers directly involved with the incidents.5–7 Incident reporting systems report PSIs as well as “near misses” and “no-harm” events, and can paint a comprehensive picture regarding both actual and potential patient harm.7 Governments and healthcare organizations around the world have established their own IRSs. For example, the National Reporting and Learning System in the United Kingdom, the Advanced Incident Monitoring System in Australia, and the Danish Patient Safety Database in Denmark.7–12 In Ontario, all hospitals are required to establish IRSs to analyze critical incidents, and act to avoid or reduce the risk of future similar incidents.9,13
There are a myriad of patient-, provider-, institution-, and system-associated factors that influence the frequency and nature of PSIs. One particularly relevant factor includes outbreaks of infectious disease, which poses unique challenges for hospitals and intensive care units.14,15 The pandemic of severe acute respiratory syndrome–associated coronavirus 2, otherwise known as COVID-19, has massively stressed contemporary healthcare systems globally.16,17 Resulting alterations in staffing levels, patient-staff interactions, and the provision of care may have consequential impacts on PSIs. Understanding COVID-19–associated PSIs may help prevent future incidents during subsequent waves of the pandemic, may reveal valuable information about incidents of concern that occur during more mundane ward-level outbreaks of infectious pathogens, and may inform unique prevention strategies.
The primary objective of this study is to examine the evolving impact of the COVID-19 pandemic on PSIs, including characterizing the most frequent pandemic-associated PSIs and comparing them to prepandemic conditions.
METHODS
Institutional Background
This study was conducted within the Niagara Health (NH) system. Niagara Health consists of 5 community hospital sites across a semirural area of southeastern Ontario and serves a population of approximately 500,000. As of 2016, residents 65 years and older accounted for 21.4% of the population, compared with 16.7% and 16.9% of residents 65 years and older in Ontario and Canada, respectively.18 The NH system consists of a tertiary care center in St Catharines, 2 community hospitals in Niagara Falls and Welland, and 2 hospitals in Port Colborne and Fort Erie with long-term care wards and urgent care centers, but no other acute care beds. In 2017 to 2018, NH logged 34,846 inpatient admissions and less than 200,000 emergency/urgent care visits.19
As with most other hospital systems in Canada, NH service delivery was impacted by the COVID-19 pandemic. The first case of COVID-19 in the Niagara region was documented on March 13, 2020, shortly after the World Health Organization declared the pandemic on March 11.20,21 As of March 17, NH paused elective surgeries and nonemergent ambulatory procedures to increase capacity in the event of a surge in patient demand.22 On March 19, a no-visitors policy was implemented, thereby restricting the presence of family/other caregivers with admitted patients unless under compassionate circumstances.23
Data
Two sets of data were used to evaluate whether case counts for PSIs were above an expected level. Because of the nature of the data, research ethics board approval was granted, with exemption from a full review. The first data set consisted of all logged PSIs in NH from January 2014 to September 2020, with most of the analysis focused on data from 2018 to 2020. The second data set examined all logged PSIs in NH from January to September 2020—the early months of the COVID-19 pandemic encompassing the “first wave,” which began March 2020. The incident types for 2020 are detailed in Table 1A of Appendix A, http://links.lww.com/JPS/A461. The data are aggregated by the week of occurrence, and because of the rarity of most incidents, they are further aggregated to the top 4 incidents and all other incidents. Categories include falls, behavior/security/safety, medication/fluid errors, care/service coordination incidents, and other incidents. Incidents were examined for the entire system, for each hospital within the system, and for ward type where the incidents occurred. Ward types included emergency departments, inpatient medicine, inpatient surgery, critical care, and complex continuing care wards. The type and reason(s) logged for each PSI in the falls category were also specifically examined.
The onset of the COVID-19 pandemic coincided with many changes in NH’s service delivery. Elective and nonambulatory procedures were canceled; patients were worried about being exposed to COVID-19 by presenting to hospital, and as such, there was significantly less demand for patient services. A weekly time series suggested that the overall number of safety incidents may have decreased during the March 2020 first wave (Fig. 1A). To control for large decreases in inpatient demand (Fig. 2A), which may have impacted the number of PSIs during the pandemic period, the total number of inpatient-days was aggregated to the week.
FIGURE 1.
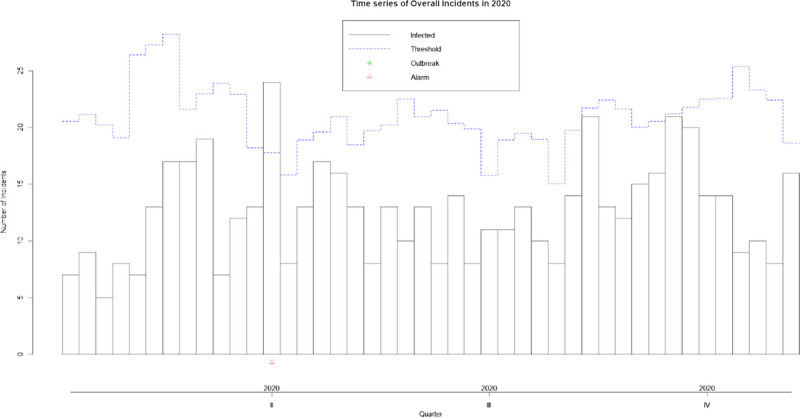
Overall number of PSIs reported in NH from January to September 2020. There was a single weekly alarm triggered at the outset of the second quarter.
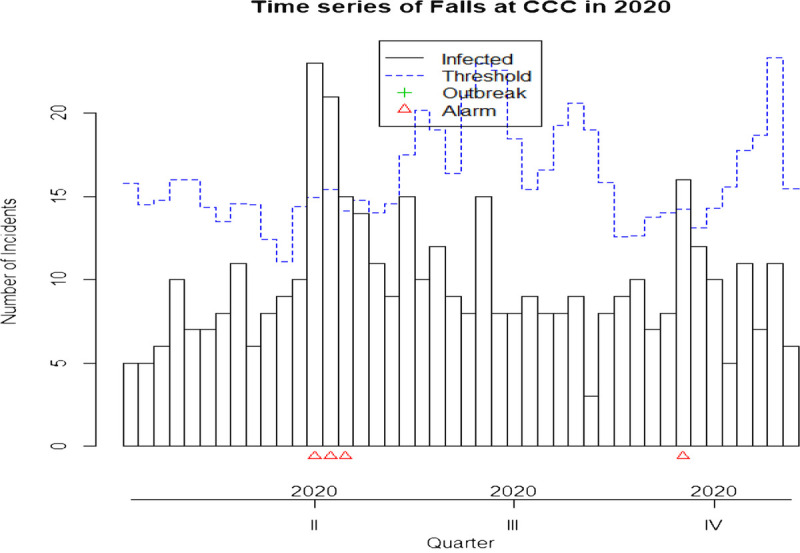
FIGURE 2.
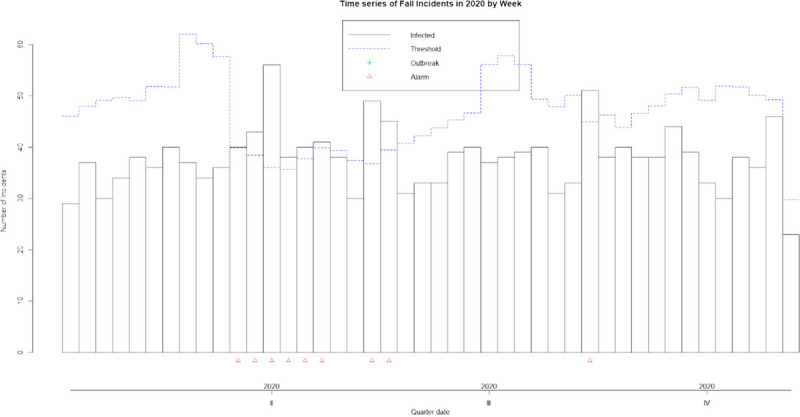
Number of reported fall incidents in NH from January to September 2020. There was a sustained outbreak of falls that began just before the onset of the second quarter and persisted for 6 weeks.
Statistical Strategy
This study used a counterfactual strategy that has become popularized in estimating excess mortality during the COVID-19 pandemic. Excess incidents were calculated using the Farrington flexible algorithm, which detects time intervals where observed incident counts are significantly above a threshold of expected incident counts.24 Further details regarding the Farrington flexible models and statistical strategies used are contained in Appendix B, http://links.lww.com/JPS/A462. The counterfactual “expected” number of weekly PSIs was based on data from 2018 and 2019. Incident counts from January to September 2020 were compared with these expected counts, representing the first wave of the COVID-19 pandemic. Outcomes included the overall incident numbers, incidents by category, and incidents by ward type. Incident counts were adjusted for the weekly number of inpatient-days to control for the decrease in patient services that occurred during this time period.
Primary outcomes of interest were alarms and “outbreaks” of incidents. An alarm was triggered when weekly PSI counts were above the expected level of incidents based on the 2018 through 2019 data. An “outbreak” of sustained alarms was considered to have occurred when 3 continuous weeks of alarms were triggered, or 3 of 4 weeks were tagged with alarms.
RESULTS
Over the period of observation from January 2018 to September 2020, a total of 9146 PSIs were logged across the 5 NH sites. This included 5956 during the prepandemic period of January 2018 to December 2019, and 3190 during the pandemic period of January 2020 to September 2020. The largest category of PSIs was falls, which accounted for 2444 and 1359 incidents in the prepandemic and pandemic periods, respectively. More details on the categories of incidents are contained in Supplementary Table 1A, http://links.lww.com/JPS/A461.
COVID-19 impacts on the overall number of safety incidents across NH during the period of January 2020 to September 2020 were first examined. Farrington flexible models did not demonstrate sustained outbreaks of incidents at NH, and only one alarm was triggered at the beginning of the second quarter of 2020. Although this coincided with the onset of the first wave, it did not meet the threshold for an outbreak (Fig. 1).
The apparent lack of change in the overall number of PSIs, however, masked significant changes in incident composition. Significant increases in falls were observed, and this coincided with the onset of the first wave. A sustained outbreak of falls occurred during the last 2 weeks of the first quarter of 2020 and persisted for a total of 6 weeks (Fig. 2). This was in part because of an actual increase in the number of falls, but also because there were far fewer inpatient days at risk of falls, which lowered the threshold to trigger an alarm. Otherwise, Farrington models did not demonstrate similar outbreaks or sustained periods of incident alarms for any other incident type(s). They also did not demonstrate similar persistent outbreaks for overall incidents at individual hospitals within NH. This suggests that, although the number of fall incidents increased with the onset of the COVID-19 pandemic, the number of other incidents decreased, resulting in an overall similar weekly rate of incidents.
From February to March 2020, the total number of falls increased to 140 from 82. The increase in falls was concentrated in one specific category type—falls from a wheelchair. The number of falls from a wheelchair increased by 86%, to 41 events from 22 in February 2020. This accounted for 33% of the overall increase in falls. The increase in falls from wheelchair persisted for a further 3 months. During the March to May 2020 period, smaller increases in falls from beds without railings and unwitnessed falls were documented, but these were still nowhere near the rise observed in falls from a wheelchair.
The ward type(s) where PSIs occurred further speaks to the heterogeneity of composition changes that occurred during the first wave of the COVID-19 pandemic. Increases in the overall number of incidents occurred on medicine wards (Fig. 3) and in emergency departments, but not on other types of wards. Falls, in particular, increased on medicine wards during this period, suggesting that falls were the source of increased overall safety incidents observed in this area (Fig. 4). Fall incidents were increased on complex continuing care wards as well, although with no accompanying increase in the overall number of PSIs (Fig. 5). Altogether, these data suggest that an increase in the number of fall incidents on medicine wards drove large increases in overall incident numbers at the outset of the COVID-19 pandemic.
FIGURE 3.
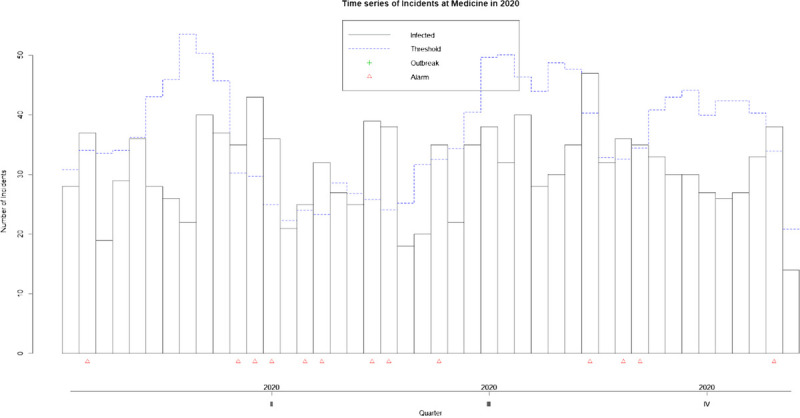
Overall number of PSIs reported on NH’s internal medicine wards from January to September 2020. There was a sustained outbreak of incidents that began just before the onset of the second quarter and persisted for 6 weeks.
FIGURE 4.
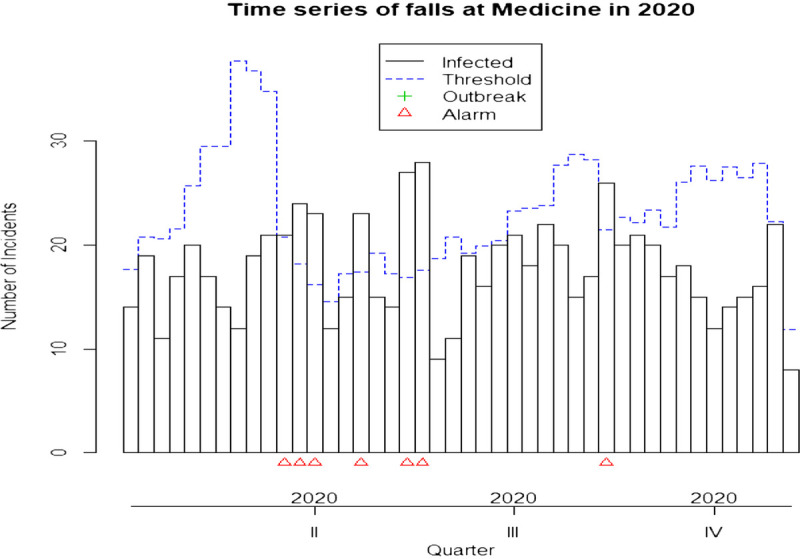
Number of reported fall incidents on NH’s internal medicine wards from January to September 2020. A sustained outbreak of falls began just before the onset of the second quarter and persisted for 8 weeks.
FIGURE 5.
Number of reported fall incidents on NH’s complex continuing care wards from January to September 2020. A sustained outbreak of falls began just before the onset of the second quarter and persisted for 3 weeks.
DISCUSSION
The COVID-19 pandemic has added much stress to existing healthcare systems, and exam of NH’s reported PSIs during the early months of the pandemic revealed several important findings. During the first wave of the COVID-19 pandemic, there was no apparent increase in the total number of safety incidents after adjusting for an approximate 25% reduction in total inpatient days (Fig. 1). However, this apparent lack of difference masked large composition shifts in the safety events actually occurring. Among the 5 most common IRS complaints examined, significant increases in the number of reported falls were discovered at the onset of the pandemic, especially falls from wheelchairs (Fig. 2). Although Farrington models are not designed to detect decreases in events, the rise in falls without an increase in overall events suggests that the frequency of other PSI events decreased compared with prepandemic conditions. Further investigation by unit type revealed that the number of falls increased specifically on internal medicine and complex continuing care wards during the same time period, with internal medicine wards reporting an increased overall number of PSIs as a result (Figs. 3, 4, 5). Altogether, these data suggest that increased falls on primarily internal medicine and complex continuing care wards drove significant increases in the number of reported falls overall during the first wave of the COVID-19 pandemic.
There are no published studies comparing PSIs and IRS data before versus during the first wave of the COVID-19 pandemic. However, current patient safety literature regards falls as the most frequently reported adverse events in adult inpatient settings, and they have long been an area of concern because of their detrimental effects and economic impact.25–27 More than 400 independent risk factors for falls have previously been identified. Some are particularly relevant to the large increases in falls observed on NH’s internal medicine and complex continuing care wards, as these patients often suffer the most consistent intrinsic falls risk factors. These include advanced age (>85 years), gait instability, agitation and/or confusion, and adverse (particularly psychotropic) drug reactions, among others.26–28
Beyond these intrinsic falls risk factors, the COVID-19 pandemic is suspected to have altered additional extrinsic and environmental risk factors that made these usually high-risk patients even more likely to fall. Within the NH environment, one identified potential contributor includes the no-visitor policy, which restricted family members and caregivers from attending to the bedside of at-risk patients. Amplified infection control measures, including more closed doors and room-sequestered patients, may also have contributed by reducing available lines of sight and timely access to patients, thereby reducing identification of and intervention in “near-fall” events. Similarly, personal protective equipment (PPE) requirements may have further deterred care providers from routinely checking in on patients, again reducing identification of and intervention in near-fall events. These possibilities may, however, be less likely given that unwitnessed falls did not comprise the majority of increased falls. A final possibility implicates time delays with the donning and doffing of PPE, which when done carefully takes roughly 3 to 5 minutes.29–32 When falls were threatened, PPE requirements may have prevented care providers from being able to intervene on their patients in time. Ultimately, it is challenging, if not impossible, to attempt to quantify the relative contributions of 400 different risk factors in assessing falls causality in the setting of the COVID-19 pandemic. However, it could be possible to prospectively intervene on a few likely causes in a local environment in a quality improvement model, then evaluate the impact.
Although the exact underlying falls mechanisms may be unclear, the results of this study demonstrate that the COVID-19 pandemic increased falls in NH. The increase in falls did not translate into increases in the overall number of PSIs even after controlling for a steep drop in inpatient visits. Although the data do not inform on which type(s) of PSIs declined, they do suggest that the pandemic led to reductions in other incidents, and this bears further investigation. If policymakers are only interested in how the pandemic has impacted the number of incidents, the investigators cannot say there has been any overall increase. Instead, the relative impact on incidents depends on the composition shift of falls and whether falls are weighted as more concerning or consequential than other incidents. These results also have some bearing on policy interventions to reduce adverse outcomes such as the spread of infection, as they may perversely affect PSIs. If it is the case that PPE requirements or other infection control procedures are implicated, future outbreaks—even at the ward level—may predispose patients to falls. Providers should then maintain a high vigilance for patient falls occurring during such episodes, whether due to outbreaks of COVID-19 or other infectious pathogens.
This study was limited by the use of ward-week level data, which is lacking in patient-specific details. This may be of particular concern given the altered patient presentations and admissions that occurred during the outset of the COVID-19 pandemic. As patient volumes decreased, it is likely that there were selection effects as the healthiest patients avoided hospitals/admissions. There were also specific directives given to physicians to try and avoid admissions to prevent additional nosocomial COVID-19 transmission. Although this study suggests that infection prevention procedures may have contributed to the observed increase in falls, it is possible that more particularly fall-prone patients were admitted to hospital compared with prepandemic patient populations. These same selection processes may also have led to decreases in other types of incidents. A similar concern is the inherently selective nature of incident reporting, as the only way a PSI gets logged is if a staff member self-reports. If there was any change in the threshold for reporting during the pandemic, changes in the reported incidents might be observed without changes in the true number of incidents. Finally, the statistical strategy used to detect changes in PSIs during the pandemic further limited the study, as the Farrington is designed to detect increases but not decreases in events. As a result, decreases in other nonfall safety incidents could not be detected but rather only inferred, as there was no major increase in the number of incidents overall.
Additional investigations beyond the administrative-level data analyzed in this study are warranted to further explore potential factors associated with the increased falls observed during the COVID-19 pandemic. These could include patient-level analyses (morbidity indices, frailty scores, medication polypharmacy, etc), and ward-level analyses (burden of infectious illness, staffing levels, PPE supply and practices, visitor restrictions, other infection control measures, etc). Information from such explorations could inform falls prevention strategies in future infection outbreaks.
CONCLUSIONS
In conclusion, the results of this investigation suggest that the COVID-19 pandemic impacted PSIs via composition shifts in incidents. Within NH, an increase in falls was observed without a concomitant increase in the overall number of incidents, suggesting an off-setting reduction in other nonfall incidents. Patients on internal medicine and complex continuing care wards were particularly susceptible to falls during the first wave. As the pandemic continues, hospitals may consider targeting resources to these locations specifically, with a particular focus on falls prevention through modification of both intrinsic and extrinsic/environmental factors. This is especially important because falls place immense economic and resource burdens on already stressed healthcare systems and, on an individual basis at the very least, are thought never to be without harm.27,28,33 Finally, the results of this investigation reinforce the need for ongoing pandemic PSI monitoring and rapidly adaptive responses to new patient safety concerns.
Footnotes
The authors disclose no conflict of interest.
The authors did not receive funding to facilitate the completion of this study.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
Contributor Information
Stephenson Strobel, Email: sbs296@cornell.edu.
Virginia Pullar, Email: Virginia.Pullar@niagarahealth.on.ca.
Pooja Senthil, Email: poojasenthil19@gmail.com.
Suneel Upadhye, Email: suneel_upadhye@hotmail.com.
Ekta Khemani, Email: ektakhemani@gmail.com.
REFERENCES
- 1.Institute of Medicine . To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000. doi: 10.17226/9728. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health . An Organisation With a Memory: Report of an Expert Group on Learning From Adverse Events in the NHS Chaired by the Chief Medical Officer. London, England: The Stationary Office; 2000. [Google Scholar]
- 3.Slawomirski L, Auraaen A, Klazinga N. The Economics of Patient Safety: Strengthening a Value-Based Approach to Reducing Patient Harm at a National Level. Paris, France: Organisation for Economic Co-operation and Development; 2017. [Google Scholar]
- 4.Canadian Patient Safety Institute . Strengthening Commitment for Improvement Together: A Policy Framework for Patient Safety. Edmonton, AB, Canada; 2019. [Google Scholar]
- 5.Simon A Lee RC Cooke DL, et al. Institutional Medical Incident Reporting Systems: A Review. Edmonton, AB, Canada: Alberta Heritage Foundation for Medical Research; 2005. [Google Scholar]
- 6.Ramírez E Martín A Villán Y, et al. Effectiveness and limitations of an incident-reporting system analyzed by local clinical safety leaders in a tertiary hospital: prospective evaluation through real-time observations of patient safety incidents. Medicine. 2018;97:e12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stavropoulou C, Doherty C, Tosey P. How effective are incident-reporting systems for improving patient safety? A systematic literature review. Milbank Q. 2015;93:826–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan B, Cochrane D. Measuring Patient Harm in Canadian Hospitals: What Can Be Done to Improve Patient Safety? Ottawa, ON, Canada: Canadian Institute for Health Information, Canadian Patient Safety Institute; 2016. [Google Scholar]
- 9.Boucaud S, Dorschner D. Patient safety incident reporting: current trends and gaps within the Canadian Health system. Healthc Q. 2016;18:66–72. [DOI] [PubMed] [Google Scholar]
- 10.Gregory D. Adverse Health Event Management: International and Canadian Practices. St. John’s, NL, Canada: Task Force on Adverse Health Events Background Documents Volume II: Additional Reports; 2008. [Google Scholar]
- 11.Sendlhofer G Schweppe P Sprincnik U, et al. Deployment of Critical Incident Reporting System (CIRS) in public Styrian hospitals: a five year perspective. BMC Health Serv Res. 2019;19:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Health System Improvement . Commentary on National Quarterly Dataset Summary of Incidents Reported to the National Reporting and Learning System July to September 2016. England, United Kingdom: National Health System; 2017. [Google Scholar]
- 13.Hamilton M, Ma J. Ontario Hospital Critical Incidents Related to Medications or IV Fluids Analysis Report: January to December 2013. Toronto, ON, Canada: Institute for Safe Medication Practices Canada; 2014. [Google Scholar]
- 14.Kain T, Fowler R. Preparing intensive care for the next pandemic influenza. Crit Care. 2019;23:337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maves RC, Jamros CM, Smith AG. Intensive care unit preparedness during pandemics and other biological threats. Crit Care Clin. 2019;35:609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Center for Immunization and Respiratory Diseases, Division of Viral Diseases . Severe acute respiratory syndrome: SARS basics fact sheet. Ctr Dis Control Prev. 2017. Available at: https://www.cdc.gov/sars/about/fs-sars.html. Accessed March 31, 2021. [Google Scholar]
- 17.WHO Team, Health Emergencies Preparedness and Response . Q&A on Coronaviruses (COVID-19). Geneva, Switzerland: World Health Organization; 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses. Accessed March 31, 2021. [Google Scholar]
- 18.Benner A. Niagara Aging Population Booming. Niagara Falls Review [Newspaper on the Internet]. 2017. Available at: https://www.niagarafallsreview.ca/news/niagara-region/2017/05/03/niagara-aging-population-booming.html. Accessed March 31, 2021.
- 19.Niagara Health . I am Niagara Health: Annual Report 2017–2018. [Internet]. Accessed 2021 April 13 from https://www.niagarahealth.on.ca/site/annualreport17-18.
- 20.Niagara Region [Internet] . COVID-19 Statistics in Niagara. Thorold, ON: Niagara Region. Available at: https://www.niagararegion.ca/health/covid-19/statistics/statistics.aspx. Accessed March 31, 2021. [Google Scholar]
- 21.The Canadian Press . Grim anniversary: a timeline of one year of COVID-19. CTV News [Newspaper on the Internet]. 2021. Available at: https://www.ctvnews.ca/health/coronavirus/grim-anniversary-a-timeline-of-one-year-of-covid-19-1.5280617. Accessed April 13, 2021.
- 22.Niagara Health . News and Updates from Niagara Health. Niagara Health postponing elective procedures as part of COVID-19 response. [Internet] 2020 March 16. Available at: https://www.niagarahealth.on.ca/site/news/2020/03/16/niagara-health-postponing-elective-procedures-as-part-of-covid-19-response. Accessed April 12, 2021.
- 23.Niagara Health . News and Updates from Niagara Health. No hospital visitors permitted effective Thursday, March 19, 8 p.m. [Internet]. 2020. Available at: https://www.niagarahealth.on.ca/site/news/2020/03/19/no-hospital-visitors-permitted-effective-thursday-march-19-8-pm. Accessed April 13, 2021.
- 24.Farrington CP Andrews NJ Beale AJ, et al. A statistical algorithm for the early detection of outbreaks of infectious disease. J R Statist Soc A. 1996;159:547–563. doi: 10.2307/2983331. [DOI] [Google Scholar]
- 25.Registered Nurses’ Association of Ontario . Clinical Best Practice Guidelines: Preventing Falls and Reducing Injury From Falls. 3rd ed. Toronto, ON, Canada: Registered Nurses’ Association of Ontario; 2017. [Google Scholar]
- 26.Currie L. Chapter 10: Fall and Injury Prevention. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses [e-book] vol. 1. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008:195–250. Available at: https://www.ncbi.nlm.nih.gov/books/NBK2653/pdf/Bookshelf_NBK2653.pdf. Accessed March 31, 2021. [PubMed] [Google Scholar]
- 27.Morris R, O’Riordan S. Prevention of falls in hospital. Clin Med (Lond). 2017;17:360–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oliver D Daly F Martin FC, et al. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33:122–130. [DOI] [PubMed] [Google Scholar]
- 29.Public Health Ontario . Putting on Full PPE [Internet Video]. 2017. Available at: https://www.youtube.com/watch?v=s2z1uM1fXN8. Accessed March 31, 2021.
- 30.Public Health Ontario . Taking off Full PPE [Internet Video]. 2017. Available at: https://www.youtube.com/watch?v=crGlUX3_4DA. Accessed 2021 March 31.
- 31.Centers for Disease Control and Prevention (CDC) . Demonstration of donning (putting on) personal protective equipment (PPE) [Internet Video]. 2020. Available at: https://www.youtube.com/watch?v=H4jQUBAlBrI&feature=youtu.be. Accessed March 31, 2021.
- 32.Centers for Disease Control and Prevention (CDC) . Demonstration of doffing (taking off) personal protective equipment (PPE) [Internet Video]. 2020. Available at: https://www.youtube.com/watch?v=PQxOc13DxvQ&feature=youtu.be. Accessed March 31, 2021.
- 33.Miake-Lye IM, Hempel S, Ganz DA. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):390–396. [DOI] [PubMed] [Google Scholar]


