Abstract
Background
The prevalence and paradigm of antenatal heart disease are contrasting between high-income, industrialized, and low- and middle-income countries. In this systematic review, we report the prevalence of heart disease and its spectrum in pregnant women of South Asia.
Methods
We searched through different electronic databases (PubMed, Google-scholar, Embase, Cochrane Library) to locate relevant articles. Studies with sufficient data that met our inclusion criteria were included. Two reviewers independently screened the articles. Discrepancies were resolved by other reviewers. Subsequently, data extraction was done using a standardized form and quality assessment of studies using the Joanna Briggs Institute tool. Meta-analysis was done using R software.
Results
After various stages of screening 25 studies were included in the final quantitative synthesis. The pooled prevalence of heart disease among pregnant women was 1.46% (95% CI 0.99–2.01). Among those with heart disease, 70.25% (95% CI 64.87–75.38) had Rheumatic heart disease and 18.10% (95% CI 14.39–22.12) had congenital heart disease. The pooled prevalence of preterm labor and delivery among pregnant women with heart disease was 17.63% (95% CI 12.18–23.80). Similarly, the pooled maternal and fetal mortality rates were 26.14 (95% CI 12.47–43.55) and 50.48 (95% CI 29.59–75.83) per 1000 pregnant women with heart disease respectively.
Conclusion
As pregnancy, itself is a prolonged state of physiologic stress, heart disease further adds to the risk both for the mother and fetus. Having such a high prevalence, efforts must be made to detect and closely monitor the condition antenatally, and decisions should be made according to the clinical conditions of the patient.
Keywords: Pregnancy, Heart disease, Rheumatic heart disease, South Asia
Abbreviations: RHD, Rheumatic Heart Disease; CHD, Congenital Heart Disease
Highlights
-
•
The paradigm of antenatal heart disease are contrasting between high-income countries, and low- and middle-income countries.
-
•
Pooled prevalence of heart disease among pregnant women is 1.46%, most having rheumatic heart disease.
-
•
Efforts should be made to prevent RHD by early detection of ARF and RHD prophylaxis of patient with ARF.
1. Introduction
Pregnancy and the peripartum period are recognized as prolonged physiological stress on the cardiovascular system [1,2]. Although most cardiac conditions are well tolerated during pregnancy with favorable outcomes, some cardiac conditions have significant maternal and fetal morbidity and mortality. The majority of women with heart disease can successfully undergo pregnancy in western countries, owing to early diagnosis and treatment of congenital heart diseases during infancy and childhood and good antenatal and obstetric care during pregnancy [1].
The prevalence and paradigm of antenatal heart disease are contrasting between high-income, industrialized, and low- and middle-income countries [3]. Congenital heart disease (CHD) is the most common in western countries, while Rheumatic heart disease (RHD) is the most common in low- and middle-income countries, accounting for up to 88% to 90% of cases [4]. However, the prevalence of RHD has decreased as healthcare coverage has increased, and the ratio of RHD to CHD has decreased from 10:1 to 3:1 in developing countries [5].
Rheumatic heart disease, a sequela of acute rheumatic fever, has afflicted countries with emerging and developing economies with the highest prevalence in India, China, Pakistan, Indonesia, and the Democratic Republic of Congo where poverty, overcrowding, and poor sanitation are pervasive [3,4]. RHD is endemic in 20 nations, with the majority of cases occurring in women of childbearing age [6].
In low and middle-income countries of Asia and Africa, rheumatic mitral stenosis, mitral regurgitation, and prior surgical mitral valve repair accounted for up to 3/4th of maternal heart disease. Mitral stenosis is usually poorly tolerated in pregnancy, and it is the leading cardiac cause of maternal mortality in the developing world [7].
Cardiac disease complicating pregnancy is a major non-obstetric and an ‘indirect’ cause of maternal mortality, as it is unrelated to any complication of the pregnancy itself [6]. The two most common adverse cardiac complications in pregnancy are heart failure and arrhythmia which may lead to maternal mortality [8]. Prematurity, low birth weight, and death are expected adverse neonatal outcomes [3].
In this systematic review, we review articles reporting the spectrum of heart disease prevalence in pregnant women of South Asia. We try to find out the pooled prevalence of heart disease in pregnancy, the percentage of rheumatic and congenital heart disease in those patients, and the mortality rate of mother and fetus or neonate in pregnancy with heart disease. We summarize the epidemiology of feto-maternal adverse outcomes in pregnant women with heart disease but not the interventions. The region, South Asia, was chosen as the site of study as no review has tried to summarize the prevalence of this condition in this part of the world. Further due to low socio-economic status, poor hygiene, unavailability of quality health services, and other factors, the spectrum of heart disease is different than in the developed world. So our meta-analysis tries to find out the actual prevalence of rheumatic heart disease and congenital heart disease in heart diseased pregnant women. These results thus obtained can help clinicians to know the epidemiology of the condition in our part of the world and screen and manage high-risk populations which may lead to better maternal and fetal prognosis.
2. Methods
The review protocol, with a comprehensive methodology, inclusion criteria, exclusion criteria, search strategy, and review questions, was registered in Research Registry UIN. (Registration Number: reviewregistry1399) This study was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [44]. The study was conceptualized (PS, SK, and SB) and the research question was defined (PS, SK, SB). A study protocol for our systematic review and meta-analysis was built (PS, SK, SB, AG). PubMed, EMBASE, and Google Scholar Library were searched to identify relevant studies published. Items used for search included “heart disease”, “pregnancy”, “prevalence or outcome”, “Nepal or India or Pakistan or Afghanistan or Srilanka or Maldives or Bhutan or Bangladesh or South Asia”. The search strategy used is given as a supplementary file in Supplementary Content 1.
No language restrictions were applied, and translations were obtained. Only human studies were included. Reference lists in each paper were further searched for any additional relevant and missing articles. Eligible study types were cross-sectional prospective or retrospective studies or cohort studies describing the type of heart disease in pregnant women with heart disease. Case reports and series were excluded. Conference abstracts, posters, and unpublished materials were not included. Other criteria of exclusion included articles published before the year 2000, and studies conducted in countries outside South Asia.
Two reviewers (AM and SLB) thoroughly analyzed the title and abstract to assess the suitability of the inclusion of the studies. Full texts of included studies were again reviewed by two reviewers (PB, ASN). Differences in opinion were sorted out by mutual discussion and a common consensus was obtained with the help of a third reviewer (PS and SK). A log of rejected studies was maintained. Quality assessment of the studies was done by two authors (RS, SB) using Joanna Briggs Institute Critical Appraisal tools for Prevalence Studies and AMSTAR 2: a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions [45]. It consists of nine yes/no questions that determine if the key components of an observational study are present or not in that study.
Data were extracted from each included article by two reviewers (RS, AG). From the individual study, extracted information included study characteristics (title, year of publication, authors, time period, and study design), population characteristics (number of pregnant women with heart disease and type of heart disease in those patients), and outcomes (frequency of preterm labor and delivery, maternal mortality and fetal or perinatal mortality).
The primary outcomes of this study were the mean pooled prevalence of heart disease and its spectrum, maternal and fetal or perinatal mortality in patients with heart disease. The event rate of maternal mortality, preterm labor and delivery, and fetal or perinatal mortality was expressed as the proportion of the total number of pregnancies with heart disease. Rates were reported per pregnancy or per 1000 pregnancies to maintain consistency across outcomes from previously published literature. The heterogeneity across each effect size was evaluated with the I2 statistic and visual plot. When I2 was less than 50%, a fixed-effect model was used and when I2 was >50%, DerSimonian, and Laird random-effects model was used for meta-analysis. A possible effect of sampling error was assessed using the 95% confidence interval (CI) around risk estimates. The statistical software used for the meta-analysis was R version 4.0.3.
3. Results
3.1. Study selection
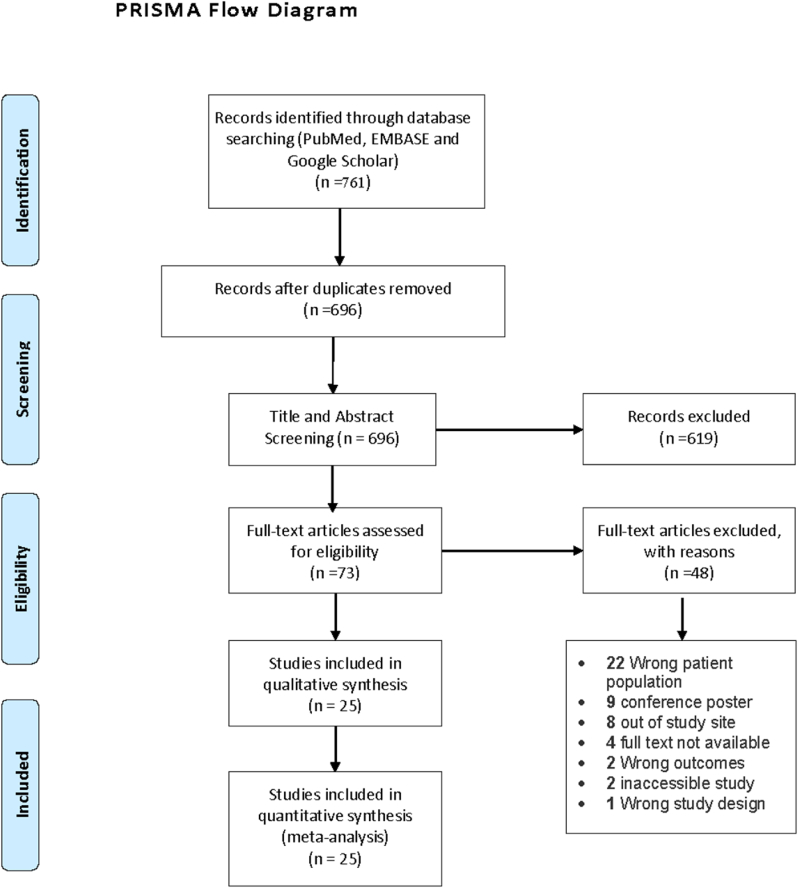
A total of 761 articles were obtained after a literature search of major databases and a reference list of obtained articles. Four hundred thirty-four articles were obtained from EMBASE, 246 from PubMed, 77 from google scholar, and four from reference search for missing articles. After the removal of 65 duplicates, 696 articles were eligible for the title and abstract screening. Seventy-three articles qualified for full-text review and 25 articles were included for qualitative and quantitative synthesis of the systematic review and meta-analysis. The PRISMA flow diagram (see Fig. 1) depicts the study retrieval process used.
Fig. 1.
PRISMA Flow diagram.
3.2. Study characteristics
A total of 25 studies from South Asia were included in the study, from five different countries. A total of 17 studies reported the prevalence of heart disease among pregnant women. Similarly, only 23 studies each reported fetal and maternal mortality. Only the studies conducted in South Asian countries were included and we were able to obtain eligible studies from India, Nepal, Pakistan, Bangladesh, and Srilanka. No studies were obtained from Afghanistan, Maldives, and Bangladesh based on the inclusion criteria. All patients with confirmed pregnancy with heart disease in various hospitals were the study subjects. The characteristic of individual studies is provided in Table 1.
Table 1.
Study Characteristic table.
| Author | Year of study | Country | Study design | Total number of deliveries | Mean age (years) | Pregnant women with Heart disease |
|---|---|---|---|---|---|---|
| Abbasi et al. [9] | 2017 | Bangladesh | Cross sectional | N/A | N/A | 51 |
| Abhilashi et al. [10] | 2018 | India | Retrospective | N/A | N/A | 41 |
| Akhtar et al. [11] | 2011 | Bangladesh | Cross sectional | 1054 | N/A | 54 |
| Asghar et al. [12] | 2005 | Pakistan | Cross sectional | 5100 | N/A | 50 |
| Bhatla et al. [13] | 2003 | India | Retrospective | 9365 | 25.66 ± 3.90 | 293 |
| Chhetri et al. [14] | 2014 | Nepal | Prospective | 9463 | 25 ± 5 | 53 |
| Gore et al. [15] | 2016 | India | Cohort | N/A | N/A | 390 |
| Haider et al. [16] | 2014 | Pakistan | Cross sectional | N/A | N/A | 29 |
| Joshi et al. [17] | 2015 | India | Retrospective | N/A | N/A | 42 |
| Kaluarachchi et al. [18] | 2020 | Srilanka | Retrospective | 26056 | N/A | 248 |
| Kanwar et al. [19] | 2018 | India | Prospective observational | 21000 | 25.33 ± 3.3 | 71 |
| Khursheed et al. [20] | 2015 | India | Retrospective | N/A | N/A | 132 |
| Laxmikantha et al. [21] | 2019 | India | Cross sectional | 2558 | N/A | 110 |
| Mahalakshmi et al. [22] | 2016 | India | Retrospective | 8072 | N/A | 62 |
| Mohan et al. [23] | 2020 | India | Retrospective | 23900 | 25 | 116 |
| Parpillewar et al. [24] | 2020 | India | Cross sectional | 11554 | N/A | 127 |
| Patil et al. [25] | 2014 | India | Prospective | 6404 | N/A | 60 |
| Patne et al. [26] | 2016 | India | Prospective | 8140 | N/A | 71 |
| Rangaswamy et al. [27] | 2016 | India | Retrospective | 31160 | N/A | 52 |
| Salam et al. [28] | 2017 | India | Cross sectional | 2093 | N/A | 90 |
| Sen et al. [29] | 2014 | India | Prospective | N/A | N/A | 40 |
| Sharma et al. [30] | 2018 | India | Prospective observational | 1301 | N/A | 35 |
| Subbaiah et al. [31] | 2013 | India | Retrospective | 2639 | 26.9 ± 4.09 | 100 |
| Waheed et al. [32] | 2012 | Pakistan | Cross-sectional | N/A | N/A | 52 |
| Yasmeen et al. [33] | 2011 | Pakistan | Cross-sectional | 7000 | N/A | 40 |
N/A = Not available.
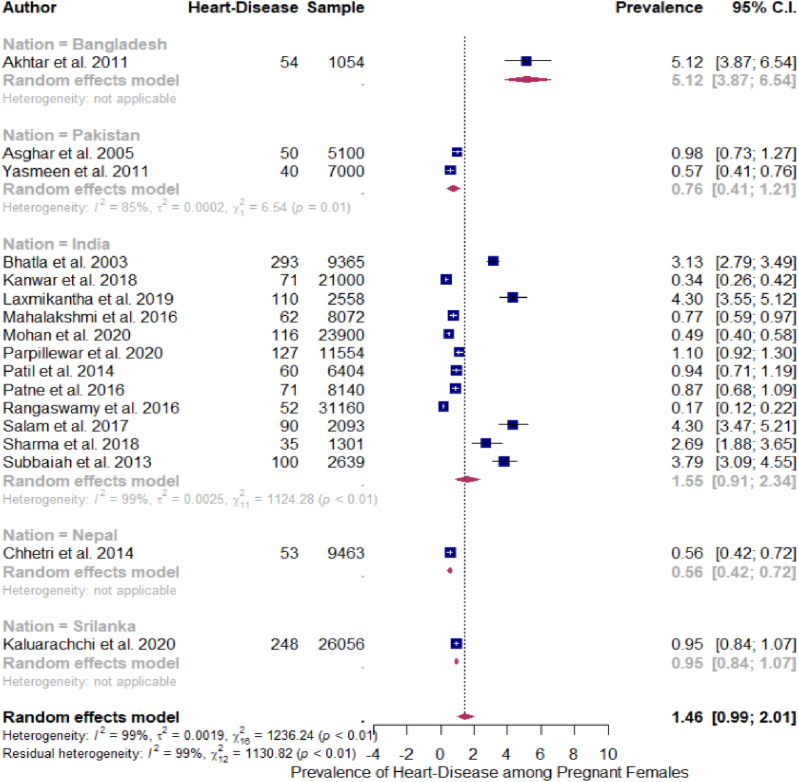
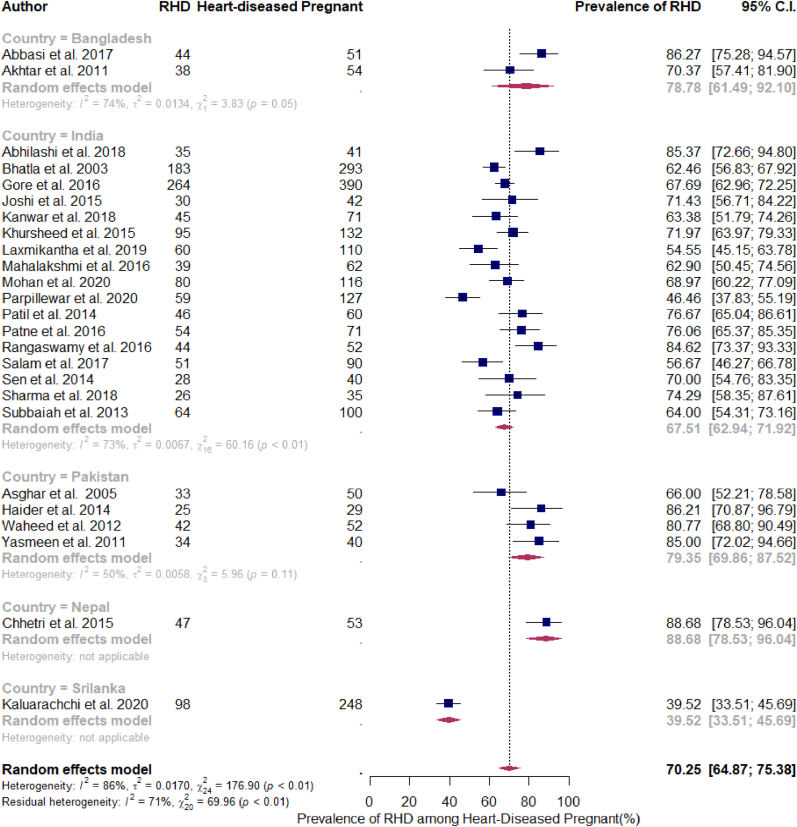
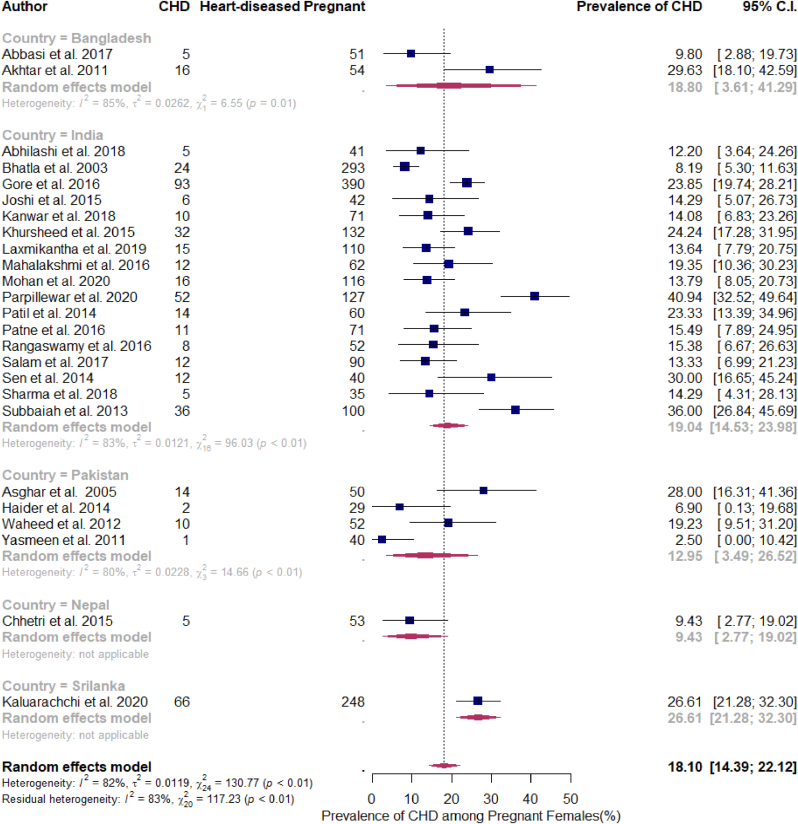
3.3. Pooled prevalence
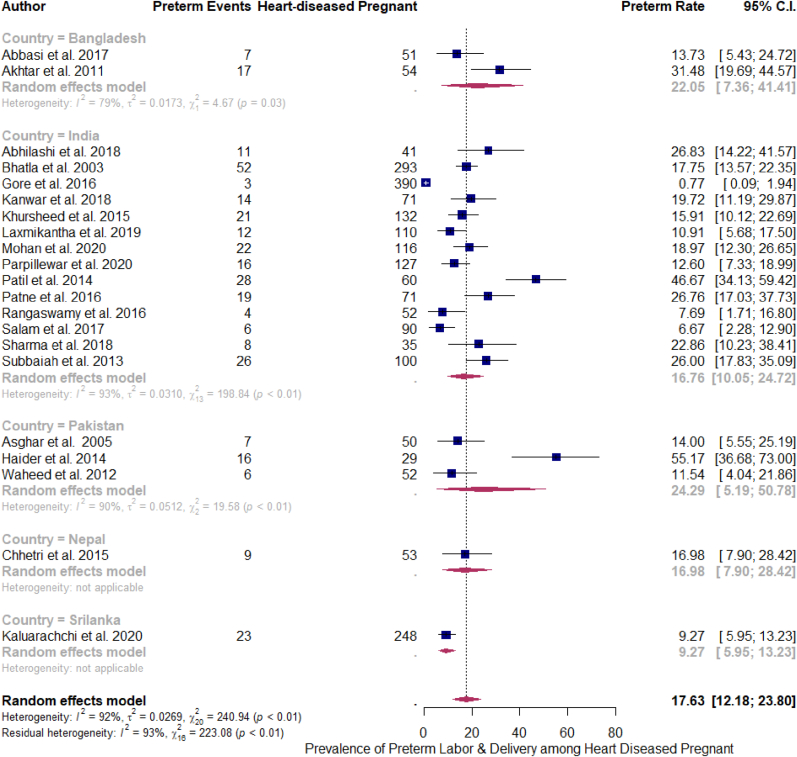
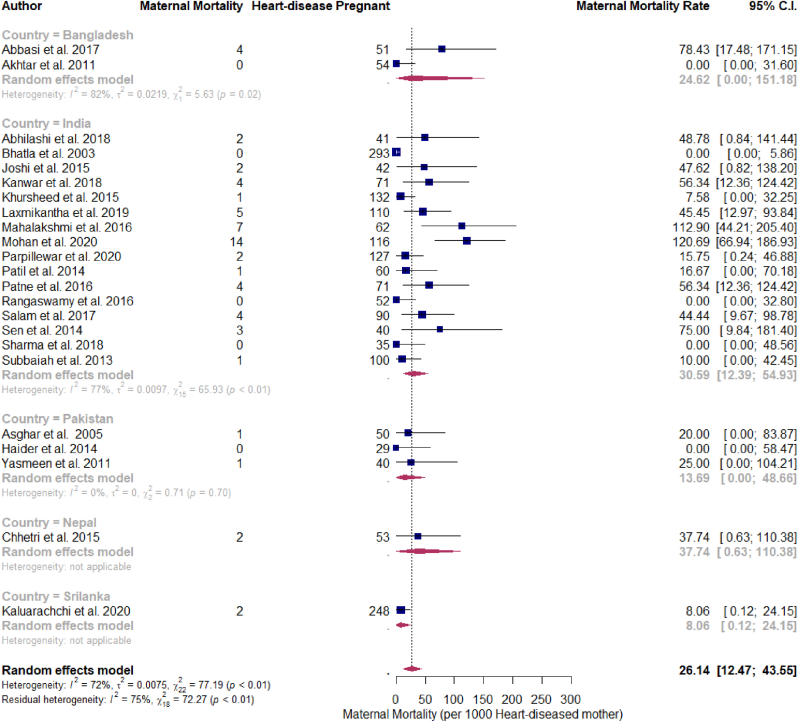
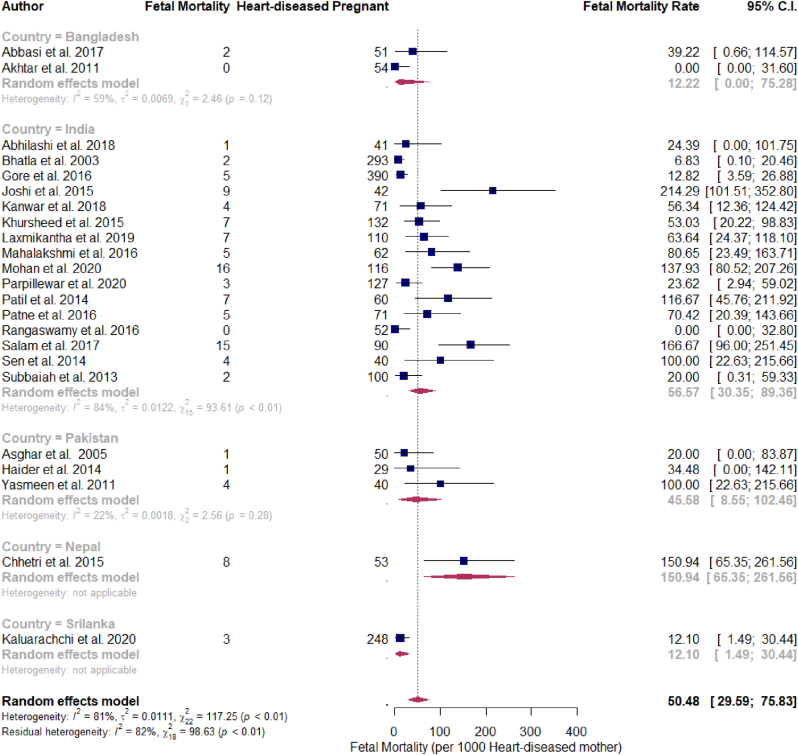
The pooled prevalence of heart disease among pregnant women from the 17 studies which reported it came out to be 1.46% (95% CI 0.99–2.01). However, there was severe heterogeneity among the studies (I2 = 99%) (Fig. 2). Among the pregnant women with heart disease, the pooled prevalence of Rheumatic Heart Disease (RHD) was found to be 70.25% (95% CI 64.87–75.38) (Fig. 3) and that of congenital heart disease (CHD) was 18.10% (95% CI 14.39–22.12) (Fig. 4). The pooled prevalence of preterm labor and delivery among pregnant women with heart disease was 17.63% (95% CI 12.18–23.80) (Fig. 5). Similarly, the pooled maternal and fetal mortality rate was 26.14 (95% CI 12.47–43.55) per 1000 pregnant women with heart disease (Fig. 6) and 50.48 (95% CI 29.59–75.83) (Fig. 7) per 1000 pregnant women with heart disease respectively. The pooled estimates of events in pregnancy with heart disease are summarized in Table 2.
Fig. 2.
Prevalence of heart disease among pregnant women.
Fig. 3.
Prevalence of RHD among the heart disease in pregnancy.
Fig. 4.
Prevalence of CHD among heart disease in pregnancy.
Fig. 5.
Prevalence of Preterm Labor and delivery among pregnant women with heart disease.
Fig. 6.
Pooled prevalence of maternal mortality per 1000 pregnancies with heart disease.
Fig. 7.
Pooled prevalence of fetal mortality per 1000 pregnancies with heart disease.
Table 2.
Pooled Estimates of Event Rates in Pregnancy with heart disease.
| Outcomes | Number of Studies | Pooled Event Rate | 95% CI | I 2 Estimate (%) |
|---|---|---|---|---|
| Pregnancy with heart disease | 17 [[11], [12], [13], [14],18,19,[21], [22], [23], [24], [25], [26], [27], [28],30,31,33] | 1.46 | 0.99–2.01 | 99 |
| Preterm labor and delivery among mother with heart disease | 21 [[9], [10], [11], [12], [13], [14], [15],[17], [18], [19], [20],[22], [23], [24], [25], [26], [27],[29], [30], [31],33] | 17.63 | 12.18–23.8 | 92 |
| Maternal mortality among mother with heart disease | 23 [[9], [10], [11], [12], [13], [14],[16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31],33] | 26.14/1000 | 12.47–43.55/1000 | 72 |
| Fetal or perinatal mortality in baby of mother with heart disease | 23 [[9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29],31,33] | 50.48/1000 | 29.59–75.83/1000 | 81 |
3.4. Subgroup and sensitivity
Sensitivity analysis was done using the leave one study out function in R which showed no major difference in the heterogeneity (supplementary file Supplementary Content 3). To access the confounder influencing heterogeneity, we used nation and study design as covariates. Subgroup analysis was done on the basis of the nation which showed the maximum prevalence of heart disease in pregnancy in Bangladesh (5.12%; 95% CI 3.87–6.54) and minimum in Nepal (0.56%; 95% CI 0.42–0.72). There were not sufficient studies from Srilanka, Nepal, and Pakistan and no studies from Afghanistan, Bhutan, and Maldives targeting populations that matched our criteria to be included in the study. And on the basis of years, there was a significant decline in the prevalence of heart disease among pregnant women from 1.8% to 1.24% between 2015-2020 and 2000–2015.
3.5. Methodological quality
A Kappa value of 0.579 was obtained which indicates moderate agreement between the two authors for assessment of the methodological quality of the included study using the JBI scale. The table showing quality assessment is given in the supplementary file Supplementary Content 2. Also, the AMSTAR 2 checklist for risk of bias assessment is provided in the supplementary file.
3.6. Publication bias
Funnel plot came out to be asymmetric and on eggers testing using mixed-effects meta-regression model it was significant for funnel plot asymmetry. (supplementary file Supplementary Content 4).
4. Discussion
In this systematic review and meta-analysis, 25 studies from South Asia, involving pregnant women with heart disease were included. To the best of our knowledge, this is the first comprehensive meta-analysis to assess the prevalence of heart disease, cause of heart disease, and maternal and fetal or perinatal outcome in this population. We showed that the prevalence of heart disease among pregnant women is 1.46%. Among the people with heart disease in this population, RHD (70.25%) carried a significant proportion followed by CHD (18.10%). Other heart diseases in pregnancy were not included in the quantitative synthesis of data as these two diseases carried the highest burden. The pooled prevalence of preterm labor and delivery in pregnancy with heart disease was 17.63%. Maternal mortality and fetal or perinatal mortality was found to be 26.14 and 50.48 per 1000 pregnancy with heart disease respectively. These findings help understand the burden of the condition and its associated adverse effect on fetal and maternal outcomes.
In pregnancy, there are major hemodynamic alterations like an increase in blood volume, stroke volume, and reduction in systemic vascular resistance, which are necessary to meet progressively increasing feto-maternal needs [34]. A diseased heart may not be able to cope with the increased demand and complications may ensue. These suggest that the epidemiology of heart disease in pregnancy be known.
As documented in the Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK (MBRRACE-UK) report, maternal heart disease complicating pregnancies is increasing [35]. It is now the most common cause of maternal death in the United Kingdom and the United States of America [35,36]. In the context of countries with low per capita income, heart disease-related deaths occur at an early age, typically in events like pregnancy [37]. The high prevalence of heart disease along with maternal mortality is also seen in our study.
The global pooled prevalence of RHD is 21.1 per 1,000. It is estimated that in 2015, RHD may have affected 31.4 million individuals worldwide [38]. Among these cases, 99% were mainly from endemic regions which were mostly low- and middle-income countries with a prevalence of 4.44 per 100,000 population. This is more than the prevalence of 3.4 per 100,000 population in non-endemic countries, the majority of which were high-income [39]. These findings could signify that the true prevalence of RHD in pregnancy is high and this high prevalence is significantly associated with maternal and fetal/perinatal prognosis. The rates of prematurity and stillbirth in newborns of pregnant women with rheumatic heart diseases are 20%–30% and 1%–3% respectively [40]. The majority of our study population had rheumatic heart disease and these data are similar to the one depicted in our study.
It is reported that the prevalence of preterm birth is 5–18% [41,42] and maternal mortality in pregnancy with heart disease is higher than in pregnancy without heart disease [43]. Our study also shows a high prevalence of maternal mortality in patients with heart disease. Also, these findings suggest that maternal mortality in pregnancy with heart disease is high in South Asia than in other regions [35,36].
Pregnancy itself is a physiological stress state and heart disease further adds risk to both mother and fetus. In the study region i.e. South Asia, most of the countries are low-income and the World Health Organization and the World Heart Federation have called for a 25% reduction in mortality because of cardiovascular causes, including RHD, by 2025 [39]. The efforts might reduce the burden of heart disease in pregnancy and reduce the risk to both fetus and mother.
The limitations of our study are it could not address some countries of the region as there were no studies that qualified the inclusion criteria. Also due to variability in the study population because of the wide spectrum of heart disease, there can be bias present in the study. We did not take into consideration the NYHA staging of patients with heart disease. Although we included studies published after 2000, some studies also included pregnancies with heart disease from before 2000.
5. Conclusion
Heart disease in pregnancy is a high-risk state for both mother and fetus. In pregnancies with heart disease, both the service provider and the patient should be extra cautious. Efforts must be made to detect and closely monitor the condition antenatally, and decisions should be made according to the clinical conditions of the patient to minimize the risk imposed by heart disease during pregnancy. The high prevalence of RHD in mothers with heart disease indicates the high burdens of this in the region and prevention of RHD should be done through early detection of Acute Rheumatic Fever (ARF) and secondary prophylaxis for RHD in patients with ARF.
Ethical approval
None.
Source of funding
No funding was received for this study.
Author contribution
Conceptualization: PS, SK and SB, research question defined (PS, SK, SB), study protocol built: PS, SK, SB, AG, Title and abstract review: AM, SLB, Full Text review: PB, ASN, Third reviewer: PS, SK,Data extraction: RS, AG, Analysis: PS, SK, Manuscript writing and review: all authors.
Trail registry number
None.
Guarantor
SK is the guarantor of the study.
Data availability
All data are available upon reasonable request to the corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None declared.
Acknowledgments
We would like to acknowledge Dr. Kundan Raj Pandey and Dr. Suman Rimal for their valuable support in manuscript proofreading.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104293.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Heart disease in pregnancy. - PDF Download Free [Internet]. docksci.com. 2021 May 17. https://docksci.com/heart-disease-in-pregnancy_5a461a33d64ab27b3b3ec368.html
- 2.Cardiovascular physiology of pregnancy | circulation. 2021 May 17. https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.114.009029 [internet]
- 3.Rheumatic heart disease in pregnancy: global challenges and clear opportunities - PubMed [internet] 2021 May 17. https://pubmed.ncbi.nlm.nih.gov/29459467/ [DOI] [PubMed]
- 4.Watkins D.A., Johnson C.O., Colquhoun S.M., Karthikeyan G., Beaton A., Bukhman G., et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N. Engl. J. Med. 2017;377(8):713–722. doi: 10.1056/NEJMoa1603693. [DOI] [PubMed] [Google Scholar]
- 5.Stangl V., Schad J., Gossing G., Borges A., Baumann G., Stangl K. Maternal heart disease and pregnancy outcome: a single-centre experience. Eur. J. Heart Fail. 2008;10(9):855–860. doi: 10.1016/j.ejheart.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Anthony J., Sliwa K. Decompensated heart failure in pregnancy. Card. Fail. Rev. 2016 May;2(1):20–26. doi: 10.15420/cfr.2015:24:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen Manh T., Bui Van N., Le Thi H., Vo Hoang L., Nguyen Si Anh H., Trinh Thi Thu H., et al. Pregnancy with heart disease: maternal outcomes and risk factors for fetal growth restriction. Int J Environ Res Public Health [Internet] 2019 Jun;(12):16. doi: 10.3390/ijerph16122075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6616620/ [cited 2021 May 17] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mogos M.F., Piano M.R., McFarlin B.L., Salemi J.L., Liese K.L., Briller J.E. Heart failure in pregnant women: a concern across the pregnancy continuum. Circ Heart Fail. 2018 Jan;(1):11. doi: 10.1161/CIRCHEARTFAILURE.117.004005. e004005. [DOI] [PubMed] [Google Scholar]
- 9.Abbasi S., Siddiqua S.F., Rijvi S., Akhtar S., Haque B., Jesmin S. Study of maternal and fetal outcome in pregnancy with heart disease. Anwer Khan Mod. Med. Coll. J. 2017;8(2):112–116. [Google Scholar]
- 10.Abhilashi K, Tiwary B, Sinha A, Kiran S, Parvina P, Prasad D. Epidemiology and maternal and fetal outcome of heart disease during pregnancy: a tertiary care center experience. Congenit. Heart Dis.. 5:12–1.
- 11.Akhtar N., Sultana T., Sayeeda S., Parveen T., Begum F. A study on pattern of heart disease and maternal and fetal outcome of pregnancy in a tertiary level hospital. Univ. Heart J. 2015;11(1):36–41. [Google Scholar]
- 12.Asghar F., Kokab H. Evaluation and outcome of pregnancy complicated by heart disease. J. Pakistan Med. Assoc. 2005;55(10):416–419. [PubMed] [Google Scholar]
- 13.Bhatla N., Lal S., Behera G., Kriplani A., Mittal S., Agarwal N., et al. Cardiac disease in pregnancy. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2003 Aug;82(2):153–159. doi: 10.1016/s0020-7292(03)00159-0. [DOI] [PubMed] [Google Scholar]
- 14.Chhetri S., Shrestha N.R., Pilgrim T. Pregnancy complicated by heart disease in Nepal. Glob Heart. 2014;9(1):e39–40. doi: 10.1136/heartasia-2013-010396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gore S., Warade S., Bramhapurikar R. A study to assess cardiac diseases in pregnancy and pregnancy outcome. Int J Reprod Contracept Obstet Gynecol. 2017 Feb 3;5(9):2960–2963. [Google Scholar]
- 16.Haider S., Shaheen R. To find out maternal and fetal outcome of cardiac disease in pregnancy. Pak J Med Health Sci. 2014;8(3):559–561. [Google Scholar]
- 17.Joshi G., Joshi S.C., Jha S.K., Singh Y., Joshi A. Maternal heart disease and pregnancy outcome: findings from a retrospective cohort in a tertiary care government hospital in Haldwani. Nainital. Niger J Cardiol. 2015;12(2):120. [Google Scholar]
- 18.Kaluarachchi A., Senanayake H., Wjeyaratne C., Jayawardane I., Ranaweera A., Rishard M., et al. Maternal heart disease and pregnancy outcome: experience of a single unit in a tertiary care hospital in Sri Lanka. Sri Lanka J Obstet Gynaecol. 2020;(1):42. [Google Scholar]
- 19.Kanwar R., Sharma M., Marwah S., Mittal P., Kumari N. Heart disease in pregnancy-evaluation of spectrum, association of predictors with obstetric outcome and need for comprehensive medical care. J. Clin. Diagn. Res. 2018;(1):12. [Google Scholar]
- 20.Khursheed R., Tabasum A., Zargar B. Maternal and fetal outcome in pregnancies complicated with maternal cardiac diseases: experience at a tertiary care hospital. Internet J Gynecol Obstet [Internet] 2015;19(1) https://www.embase.com/search/results?subaction=viewrecord&id=L605616982&from=export [Google Scholar]
- 21.Laxmikantha G, Parvathi B, Begum S. A Prospective Study of Heart Disease in Pregnancy and its Effect on Maternal Outcome.
- 22.Mahalakshmi G., Nirmala P., Shravanya K. Evaluation of pregnancy outcome in heart disease complicating pregnancy. J. Evol. Med. Dent. Sci. 2016;5(43):2657–2661. [Google Scholar]
- 23.Mohan A., Mohan U., Singla R., Mittal P., Pandey D., Bharti R. Feto–maternal outcome in pregnancy with Heart Disease: a tertiary care centre experience. MOJ Womens Health. 2020;9(2):59–62. [Google Scholar]
- 24.Parpillewar M.B., Prashanthi S., Fidvi J.I. Study of maternal and foetal outcome of pregnancy complicated with heart disease at a tertiary care centre. Indian Obstet Gynaecol. 2020;10(2) [Google Scholar]
- 25.Patil V., Bhingare P., Murthy B. Evaluation of maternal and foetal outcome of pregnancy with heart disease with special reference to surgically corrected heart diseases. Int J Sci Res Publ. 2014:184. [Google Scholar]
- 26.Patne SV, Tungikar S, Shinde A. Study of Maternal and Neonatal Outcome in Pregnancy with Heart Disease.
- 27.Rangaswamy M., Ramachandra P. 2016. Pregnancy with Cardiac Disease: a Retrospective Five Year Study in a Teaching Hospital. Int J Reprod Contracept Obstet Gynecol; pp. 1589–1592. [Google Scholar]
- 28.Salam S., Mushtaq S., Mohi-ud-Din K., Gul I., Ali A. Maternal and fetal outcome in pregnancy with heart disease in tertiary care hospital in India. Int J Reprod Contracept Obstet Gynecol. 2017 Aug 28;6(9):3947–3951. [Google Scholar]
- 29.Sen M., Bhattacharyya P., Chowdhury N. Pregnancy with heart disease–fetomaternal outcome. J. Evol. Med. Dent. Sci. 2014;3(5):1178–1184. [Google Scholar]
- 30.Sharma P., Malik R., Pandit N. Risk factors in pregnancy with heart disease and their co-relation with adverse feto-maternal outcome. Int J Reprod Contracept Obstet Gynecol. 2018;7(3):1136. [Google Scholar]
- 31.Subbaiah M., Sharma V., Kumar S., Rajeshwari S., Kothari S.S., Roy K.K., et al. Heart disease in pregnancy: cardiac and obstetric outcomes. Arch. Gynecol. Obstet. 2013;288(1):23–27. doi: 10.1007/s00404-013-2730-2. [DOI] [PubMed] [Google Scholar]
- 32.Waheed K., Sajjad N., Riaz U., Ejaz S., Malik M. Frequency of maternal complications in pregnancy with cardiac disease. Pak J Med Health Sci. 2012;6(3):613–615. [Google Scholar]
- 33.Yasmeen N., Aleem M., Iqbal N. Feto-maternal outcome in patients with cardiac disease in pregnancy. Pak J Med Health Sci. 2011;5(4):748–751. [Google Scholar]
- 34.Albakri A. Heart failure in pregnancy: a review of clinical status and meta-analysis of diagnosis and medication safety. Med Clin Arch [Internet]. 2019 [cited. 2021 May 11;3(1) https://www.oatext.com/heart-failure-in-pregnancy-a-review-of-clinical-status-and-meta-analysis-of-diagnosis-and-medication-safety.php [Google Scholar]
- 35.Knight M., Tuffnell D., Kenyon S., Shakespeare J., Gray R., Kurinczuk J.J. Confidential Enquiries into Maternal Deaths and Morbidity 2009-13. National Perinatal Epidemiology Unit. University of Oxford; 2015. Saving lives, improving mothers' care: surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland. [Google Scholar]
- 36.Pregnancy mortality surveillance system | maternal and infant health | CDC. 2020. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm [internet], [cited 2021 May 11.
- 37.Vos T., Flaxman A.D., Naghavi M., Lozano R., Michaud C., Ezzati M., et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marijon E., Celermajer D.S., Jouven X. Rheumatic heart disease-an iceberg in tropical waters. N. Engl. J. Med. 2017;377(8):780–781. doi: 10.1056/NEJMe1705840. [DOI] [PubMed] [Google Scholar]
- 39.Watkins D.A., Johnson C.O., Colquhoun S.M., Karthikeyan G., Beaton A., Bukhman G., et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N. Engl. J. Med. 2017;377(8):713–722. doi: 10.1056/NEJMoa1603693. [DOI] [PubMed] [Google Scholar]
- 40.Michael A. Prospective cohort study compares effect of corrected and uncorrected rheumatic heart valve of pregnant women on maternal and fetal outcomes. clinicaltrials.gov. 2017 Jan https://clinicaltrials.gov/ct2/show/NCT03029117 [internet] [cited 2021 May 11]. Report No.: NCT03029117. Available from: [Google Scholar]
- 41.Wagura P., Wasunna A., Laving A., Wamalwa D., Ng’ang’a P. Prevalence and factors associated with preterm birth at kenyatta national hospital. BMC Pregnancy Childbirth. 2018 Apr 19;18(1):107. doi: 10.1186/s12884-018-1740-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Preterm birth. 2021 May 11. https://www.who.int/news-room/fact-sheets/detail/preterm-birth
- 43.Maternal mortality rates and statistics [Internet]. Unicef data [cited 2021 May 11]. Available from: https://data.unicef.org/topic/maternal-health/maternal-mortality/.
- 44.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 45.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017 Sep 21:358. doi: 10.1136/bmj.j4008. https://www.bmj.com/content/358/bmj.j4008 [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available upon reasonable request to the corresponding author.