Abstract
Introduction
and Importance: Williams Syndrome (WS) is a well-recognized genetic disorder characterized by multi-system clinical manifestations. However, there are very rare gastrointestinal complications associated with patients with Williams Syndrome. We report the first transverse colon volvulus (TCV) case in an adult with pre-diagnosed Williams Syndrome.
Case presentation
We report a case of a 22-year-old South Asian adult who presented with complaints of generalized progressive abdominal pain, distension, bilious vomiting, and constipation. Detailed history, physical examination, and radiological investigations confirmed the diagnosis of transverse colon volvulus. A subtotal colectomy with end-to-end anastomosis was done.
Conclusion
Patients with Williams Syndrome can develop rare gastrointestinal complications like transverse colon volvulus due to congenital/physiological predisposing factors. It is a surgical emergency and should be diagnosed and managed optimally. In addition, physicians should keep TCV in differential diagnoses while dealing with patients of Williams Syndrome presenting with acute or subacute abdominal pain.
Keywords: Williams syndrome, Congenital, Constipation, Volvulus, Transverse colon volvulus, Case report
Highlights
-
•
There are very rare gastrointestinal complications associated with patients with Williams Syndrome.
-
•
This case report bridges a void in the existing medical literature regarding the gastrointestinal complications of Williams Syndrome.
-
•
Physicians should keep TCV in differential diagnoses while dealing with patients of Williams Syndrome presenting with acute or subacute abdominal pain.
1. Background
Williams Syndrome (WS) is a well-recognized, multi-system genetic disorder characterized by facial anomalies described as elfin faces, cognitive dysfunction, growth abnormalities, congenital heart defects, and other very rare manifestations [1]. Most (90%) of the cases of WS occur due to deletion at chromosome 7q11.23, which also includes the elastin gene [2]. The frequency of WS has been estimated to be 1 in 20,000 births, with most of the patients with a normal life expectancy [3]. Diagnosis of Williams Syndrome is mainly clinical, but detecting genetic abnormality by fluorescence in situ hybridization (FISH) aids in the diagnosis [2]. Existing literature has delineated the common clinical manifestations of this uncommon disorder [1]. However, there are very rare presentations associated with patients with Williams Syndrome. These include musculoskeletal abnormalities, underdeveloped thyroid gland, ophthalmological anomalies, and gastrointestinal (GI) disorders [1]. The gastrointestinal manifestations of WS range from feeding problems, vomiting, and constipation in infants to recurrent abdominal pain, diverticulitis, and GI perforation [4]. Cases of chronic constipation, celiac disease, diverticulitis, and other GI complications have been reported [[5], [6], [7]]. We report the first transverse colon volvulus (TCV) case in an adult with pre-diagnosed Williams Syndrome. Transverse colon volvulus itself is a rare GI disorder and constitutes about 0.2–0.3% of all the large bowel obstructions [8]. Our case report bridges a void in the existing medical literature regarding the gastrointestinal complications of Williams Syndrome. This case report has been reported in line with the SCARE 2020 criteria [9].
2. Case presentation
A 22-year-old gentleman presented in surgical emergency with complaints of generalized progressive abdominal pain, distension, bilious vomiting, and constipation from four days. According to the patient, the intensity of the pain was 8/10. The patient was diagnosed with Williams Syndrome at the age of six years. Past medical history was significant for recurrent episodes of constipation, supra-valvular aortic stenosis, and recurrent urinary tract infections (UTIs). His family members were also interviewed for an elaborative history. According to his mother, the patient was suffering from severe constipation, later diagnosed as chronic constipation syndrome. His stool sample included medium-sized, separate, hard lumps of fecal matter. There were only two to three episodes of defecation per week, with straining and an incomplete sensation of evacuation after every episode. There was no history of trauma or prior surgical intervention. Family history was negative for Williams Syndrome or any other genetic disorder. He denied any complaints of fever, cough, body aches, and shortness of breath.
On presentation to the emergency department, the pulse rate was 78 beats/min, blood pressure was 130/80 mmHg, respiratory rate was 22/min, and oxygen saturation was 96%. The patient was dehydrated and irritable. General physical examination revealed a typical “elfin” face with bulged forehead, dental malocclusion, and a short nose with a tipped appearance. His speech and auditory senses were normal. The psychiatric evaluation revealed mild cognitive decline. On systemic examination, generalized distension was found, more marked under the right subcostal region. Percussion note was tympanic. On auscultation, no bowel sounds were heard. A digital rectal examination demonstrated an empty rectal vault without an intraluminal mass. The patient was non-alcoholic, non-smoker, and never abused drugs. Keeping the past history of the patient in mind, the associated disorders, and acute presentation, our differential diagnosis included diverticulitis, pancreatitis, and GI perforation. The patient was managed conservatively at that time.
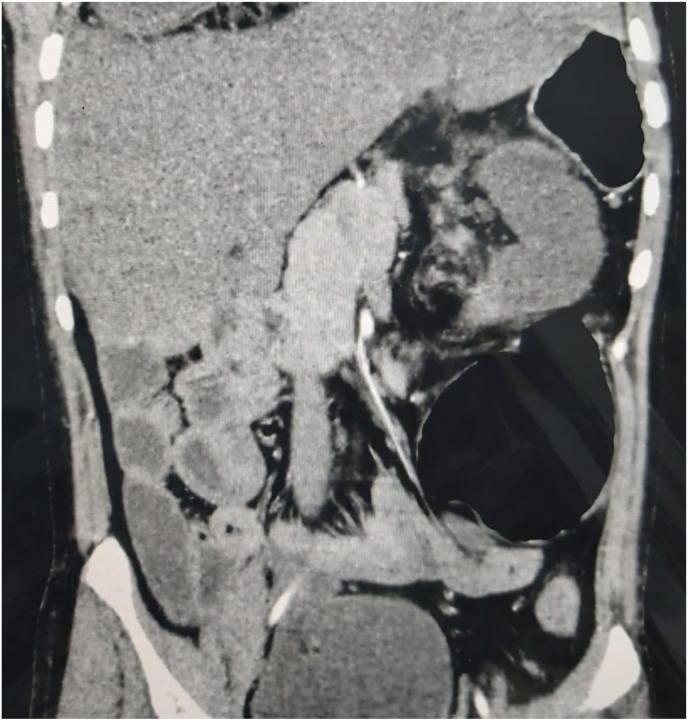
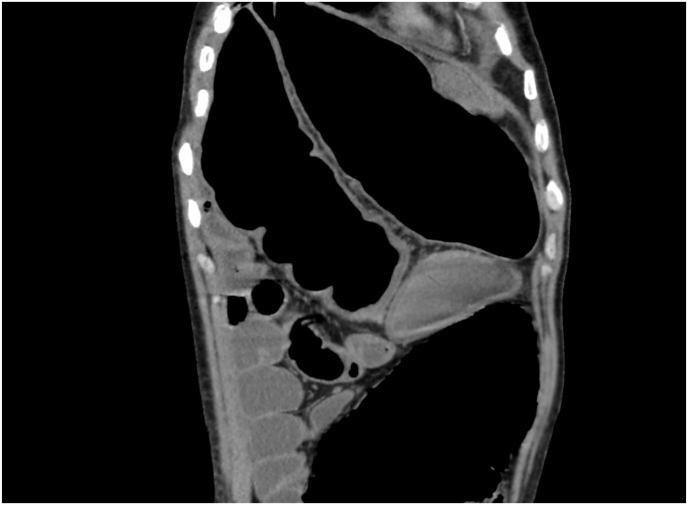
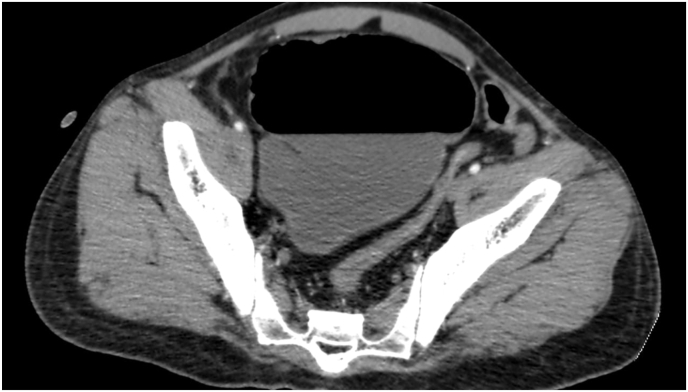
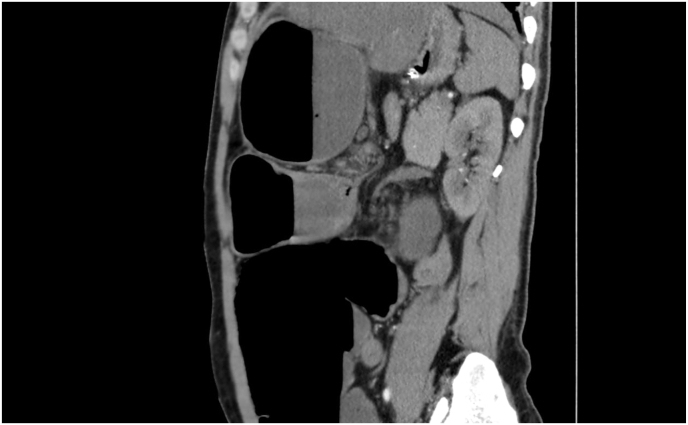
Laboratory workup included complete blood count, liver function tests, renal parameters, serum amylase and lipase, serum electrolytes, and clotting profile. All were in the normal reference range. Computed tomography (CT scan) abdomen with intravenous contrast was also done, which revealed twisting of the transverse mesocolon and transverse colon at the splenic flexure, acting as a transitional point to the moderately dilated transverse colon, ascending colon, and cecum (Fig. 1). A large gas-filled bowel loop in the upper abdomen, pointing to the right upper quadrant, was also observed (Fig. 2). Descending and sigmoid colon was collapsed (Fig. 3). It also showed converging short mesentery and twisting mesenteric vessels with dilated anteriorly located loops of the large bowel (Fig. 4).
Fig. 1.
Coronal abdominal computed tomography (CT) scan imaging during porto-venous phase showing large bowel dilation with a twist in the mesentry giving evidence of volvulus.
Fig. 2.
Coronal abdominal computed tomography (CT) scan imaging during porto-venous phase showing a gas filled large bowel loop located in upper abdomen, pointing to right upper quadrant.
Fig. 3.
Axial post contrast computed tomography (CT) scan abdomen showing collapsed sigmoid and descending colon, revealed point of obstruction proximal to it.
Fig. 4.
Sagittal computed tomography (CT) scan of abdomen showing converged and twisted mesenteric vessels with dilated anteriorly located loops of large bowel.
Based on clinical and radiological investigations, a provisional diagnosis of transverse colon volvulus was made. Being an unusual presentation of a rare disorder, a specialist board of general surgeons, anesthesiologists, and cardiovascular surgeons was called. A decision to proceed with the laparotomy under very cautious and expert-informed anesthesia was made. Endoscopic correction of the volvulus was not done due to the risk of recurrence as it was a complex case with a lot of comorbidities. Laparotomy confirmed the diagnosis of transverse colon volvulus. A markedly dilated mid-transverse colon with 180° anticlockwise twist was found lying under the right subcostal area. A short mesentery with normal hepatic and splenic angle fixation was observed. There was no evidence of ischemia of the involved segment. The volvulus was untwisted. Both colonic flexures were found very restrictive. A subtotal colectomy with end-to-end anastomosis was done. The patient did not develop any postoperative complications and was discharged after two weeks of laparotomy. The discharge protocol included specialized wound care, prescription antibiotics, and pain killers as needed. We followed up with the patient fourteen days after discharge. There were no active complaints. All the examination was normal with properly healing wound.
3. Discussion
We reported a case of a patient with pre-diagnosed Williams Syndrome presenting with generalized abdominal pain, later diagnosed as transverse colon volvulus. Intraoperatively, the transverse colon was mobile with an increased length. However, there was no sign of malignancy. Existing literature has reported various cases of gastrointestinal complications of the Williams Syndrome [5,6]. This is the first-ever reported transverse colon volvulus in a patient with Williams Syndrome.
Volvulus is defined as an axial rotation of the bowel upon its mesentery. It can involve the stomach, small bowel, or large bowel. Large bowel volvulus is an important, uncommon cause of large bowel obstruction [9]. Due to its long mesentery and narrow mesenteric base, the sigmoid colon is the commonest part of the colon to twist. The transverse colon rarely twists, probably due to its fixation at each flexure [10]. We can identify past surgical procedures causing coalescence or bowel malrotation, neoplasia, pregnancies, and congenital errors such as intestinal malrotation with an abnormal fixation of the posterior abdominal wall [10,11]. Moreover, chronic constipation can also lead to the occurrence of transverse colon volvulus by causing its excessive and abnormal elongation [12].
In our case, the patient had a congenitally short mesentery with a normal fixation on both hepatic and splenic angles. It was well established in radiological investigations and intra-operatively. Medina et al. reported that anatomical or congenital defects of mesentery constitute the most important risk factors for the development of transverse colon volvulus [13]. However, our patient also had chronic constipation syndrome, a predisposing factor for the development of TCV, which led to the elongation of the colon and motility issues [12,13].
Surgical resection constitutes the treatment of choice to prevent recurrence [12]. However, after previous resection and primary anastomosis, the incidence of recurrent volvulus varies between 22 and 36%. Therefore, some authors prefer considering a subtotal colectomy in the case of megacolon instead of a partial colectomy of the involved intestinal segment [14]. It is done with or without primary anastomosis depending on the aspect of the colon, the existence or not of peritonitis, and the comorbidities of the patient [14].
Though rare, the development of transverse colon volvulus can occur in patients with Williams Syndrome due to congenital/physiological predisposing factors. Physicians should keep TCV in the differential diagnoses of acute or sub-acute GI disorders in patients with Williams Syndrome. We suggest that the complaint of constipation in patients with WS should be dealt with special care as it can lead to various GI complications. A complete workup for the diagnosis and pre-operative care of the patient should be done. In addition, the surgeons should consider subtotal colectomy to avoid recurrent development of the volvulus, as the patients with WS can develop fatal complications due to anesthesia [[15], [16]]. Finally, we believe that further studies are required to appreciate this association between the development of the Williams Syndrome and underlying pathophysiology.
Our study has certain limitations. First, we could not collect the results of genetic testing done in the patient's childhood for the diagnosis of Williams Syndrome. Second, we could not obtain the patient's magnetic resonance imaging (MRI) due to clinical circumstances. Our case signifies the multidisciplinary team approach for the optimal diagnosis and critical management of such unique manifestations of rare genetic disorders.
4. Conclusion
Patients with Williams Syndrome can develop rare gastrointestinal complications like transverse colon volvulus due to congenital/physiological predisposing factors. It is a surgical emergency and should be diagnosed and managed optimally. In addition, physicians should keep TCV in differential diagnoses while dealing with patients of Williams Syndrome presenting with acute or subacute abdominal pain.
List of abbreviations
WS: Williams Syndrome.
FISH: Fluorescence in situ hybridization.
GI: Gastrointestinal.
UTI: Urinary tract infection.
CT: Computed tomography.
TCV: Transverse Colon Volvulus.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Informed consent was also taken from the patient's kin, his mother in this case. A copy of the written consents is available for review by the Editor-in-Chief of this journal.
Availability of data and materials
Not applicable.
Ethical approval
Nishtar Medical University and Hospital, Multan.
0000-NMU-0077.
Sources of funding
No funding was received for this case report.
Author contributions
SY conceived and designed the study. SY and ZS were responsible for data collection and acquisition of data. ZS, MAM, and HM analyzed and/or interpreted the data. HM and MAM performed the literature review. SY, ZS, and HM wrote the initial manuscript. MAM and HM critically revised the manuscript. All authors have approved the final manuscript.
Trail registry number
1. Name of the registry: NA.
2. Unique Identifying number or registration ID: NA.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
Guarantor
Dr Hamza Maqsood.
Nishtar Medical University.
And Hospital, Multan, Pakistan.
Phone: +923168435531.
Email address: hamzamaqsood381@gmail.com.
Provenance and peer review
Not commissioned, externally peer reviewed.
Annals of medicine and surgery
The following information is required for submission. Please note that failure to respond to these questions/statements will mean your submission will be returned. If you have nothing to declare in any of these categories then this should be stated.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Declaration of competing interest
No conflict of interest.
Acknowledgment
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104310.
Contributor Information
Shifa Younus, Email: shifa.sheikh166@gmail.com.
Zainab Sadiq, Email: znbsdq3@live.com.
Muhammad Ali Momin, Email: m.alimomin51@gmail.com.
Hamza Maqsood, Email: hamzamaqsood381@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Amenta S., Sofocleous C., Kolialexi A., et al. Clinical manifestations and molecular investigation of 50 patients with Williams syndrome in the Greek population. Pediatr. Res. 2005;57(6):789–795. doi: 10.1203/01.PDR.0000157675.06850.68. [DOI] [PubMed] [Google Scholar]
- 2.Zamani H., Babazadeh K., Fattahi S., Mokhtari-Esbuie F. Williams-Beuren's syndrome: a case report. Case Rep Med. 2012;2012 doi: 10.1155/2012/585726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burn J. Williams syndrome. J. Med. Genet. 1986;23(5):389–395. doi: 10.1136/jmg.23.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris C.A., Demsey S.A., Leonard C.O., Dilts C., Blackburn B.L. Natural history of Williams syndrome: physical characteristics. J. Pediatr. 1988;113(2):318–326. doi: 10.1016/s0022-3476(88)80272-5. [DOI] [PubMed] [Google Scholar]
- 5.Mıhçı E., Nur B.G., Berker-Karaüzüm S., Yılmaz A., Artan R. Celiac disease in patients with Williams-Beuren syndrome. Turk. J. Pediatr. 2015;57(6):599–604. doi: 10.1136/jmg.38.11.767. [DOI] [PubMed] [Google Scholar]
- 6.Stagi S., Lapi E., Chiarelli F., de Martino M. Incidence of diverticular disease and complicated diverticular disease in young patients with Williams syndrome. Pediatr. Surg. Int. 2010;26(9):943–944. doi: 10.1007/s00383-010-2666-6. [DOI] [PubMed] [Google Scholar]
- 7.Partsch C.J., Siebert R., Caliebe A., Gosch A., Wessel A., Pankau R. Sigmoid diverticulitis in patients with Williams-Beuren syndrome: relatively high prevalence and high complication rate in young adults with the syndrome. Am. J. Med. Genet. 2005;137(1):52–54. doi: 10.1002/ajmg.a.30865. [DOI] [PubMed] [Google Scholar]
- 8.Lepage-Saucier M., Tang A., Billiard J.S., Murphy-Lavallée J., Lepanto L. Small and large bowel volvulus: clues to early recognition and complications. Eur. J. Radiol. 2010;74(1):60–66. doi: 10.1016/j.ejrad.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: Updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Kerry R.L., Ransom H.K. Volvulus of the colon. Arch. Surg. 1969;99(2):215–222. doi: 10.1001/archsurg.1969.01340140087013. [DOI] [PubMed] [Google Scholar]
- 11.Tobinaga S., Morinaga A., Sajima S., Kanazawa N., Yoshida T. Transverse to descending colon volvulus and megacolon with mesenterium commune: report of a case. Surg. Today. 2004;34(10):875–877. doi: 10.1007/s00595-004-2808-3. [DOI] [PubMed] [Google Scholar]
- 12.Deshmukh S.N., Maske A.N., Deshpande A.P., Shende S.P. Transverse colon volvulus with chilaiditis syndrome. Indian J. Surg. 2010;72(4):347–349. doi: 10.1007/s12262-010-0130-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casamayor Franco M.C., Gracia Solanas J.A., Artigas Marco C., Bielsa Rodrigo M.A., Martínez Díez M. Intestinal occlusion secondary to transverse colon volvulus. Rev. Esp. Enferm. Dig. 2005;97(12):914–915. doi: 10.4321/s1130-01082005001200008. [DOI] [PubMed] [Google Scholar]
- 14.Medina V., Alarcó A., Meneses M., et al. Vólvulo de colon transverso: una causa poco frecuente de obstrucción intestinal [Volvulus of the transverse colon: a rare cause of intestinal obstruction] Rev. Esp. Enferm. Dig. 1994;86(3):683–685. [PubMed] [Google Scholar]
- 15.Booij K.A., Tanis P.J., van Gulik T.M., Gouma D.J. Recurrent volvulus of the transverse colon after sigmoid resection. Int. J. Colorectal Dis. 2009;24(4):471–472. doi: 10.1007/s00384-008-0565-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matisoff A.J., Olivieri L., Schwartz J.M., Deutsch N. Risk assessment and anesthetic management of patients with Williams syndrome: a comprehensive review. Paediatr. Anaesth. 2015;25(12):1207–1215. doi: 10.1111/pan.12775. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.