Summary
Background
Extreme heat exposure can lead to premature death. Climate change is expected to increase the frequency, intensity, and duration of extreme heat events, resulting in many additional heat-related deaths globally, as well as changing the nature of extreme cold events. At the same time, vulnerability to extreme heat has decreased over time, probably due to a combination of physiological, behavioural, infrastructural, and technological adaptations. We aimed to account for these changes in vulnerability and avoid overstated projections for temperature-related mortality. We used the historical observed decrease in vulnerability to improve future mortality estimates.
Methods
We used historical mortality and temperature data from 208 US cities to quantify how observed changes in vulnerability from 1973 to 2013 affected projections of temperature-related mortality under various climate scenarios. We used geographically structured meta-regression to characterise the relationship between temperature and mortality for these urban populations over the specified time period. We then used the fitted relationships to project mortality under future climate conditions.
Findings
Between Oct 26, 2018, and March 9, 2020, we established that differences in vulnerability to temperature were geographically structured. Vulnerability decreased over time in most areas. US mortalities projected from a 2°C increase in mean temperature decreased by more than 97% when using 2003–13 data compared with 1973–82 data. However, these benefits declined with increasing temperatures, with a 6°C increase showing only an 84% decline in projected mortality based on 2003–13 data.
Interpretation
Even after accounting for adaptation, the projected effects of climate change on premature mortality constitute a substantial public health risk. Our work suggests large increases in temperature will require additional mitigation to avoid excess mortality from heat events, even in areas with high air conditioning coverage in place.
Introduction
Extreme temperatures can overwhelm the body’s ability to regulate its internal temperature, increasing the frequency and severity of acute and chronic health effects, including mortality.1–4 Climate change is causing an increase in the frequency of extreme heat events, reducing the frequency of extreme cold events, increasing mean temperature, and increasing temperature variability.5–7 Estimates of the net effect of climate change on temperature related mortality yield large numbers globally using multiple methodologies.3,8–10
Studies finding a relationship between changes in all-cause mortality to temperature have found that vulnerability varies over space and time, and can be mitigated through physiological acclimatisation, increased air-conditioning availability, or social programmes such as cooling centres, which provide air-conditioned spaces for those in need, as well as outreach to and monitoring of individuals who are vulnerable to extreme heat.3 A better understanding of the role of geographical and temporal adaptation trends (adaptation being defined here as a reduction in the response to temperature from earlier time periods to later ones; this operational definition makes no assumptions about mechanisms) will improve estimates of future temperature-attributable mortality. However, few attempts have been made to incorporate adaptation in projections of temperature-attributable human health outcomes in possible future climates. The analogue city approach replaces one city’s vulnerability profile with the profile from a second city whose temperature matches the projected temperature from the first city.11,12 Alternatively, projections can be made assuming temperature thresholds used in the mortality functions will increase over time at some rate less than or equal to the rate of warming.13–15 Petkova and colleagues used historical trends in relative risks at each temperature threshold to project future relative risks, with two possible future bounding conditions depending on optimistic or pessimistic projections of maximum adaptation.16 One study addressed future vulnerability by projecting the effect of increased air-conditioning prevalence.17 Approaches published since 2017 have applied more sophisticated techniques to control for lagged temperatures and seasonal variation in response curves, or incorporating economic factors in vulnerability estimates.16,18,19
In this Article, we applied multiple analytical approaches to use observed adaptation trends to project future effects of climate change on temperature-related mortality in the USA. Our approach assumes that the observed reductions in vulnerability to extreme temperatures over time are a proxy for adaptation, without necessarily identifying the adaptive mechanism. We analysed effects at mean levels of US warming from 1–6°C, in 1°C increments, for 208 cities clustered into nine regions.
Methods
Study design and response curve development
We related historical mortality to temperature with data from 208 cities (appendix pp 3–4) located in the contiguous United States aligned with the work of Nordio and colleagues.2 We obtained death certificates from the US Centers for Disease Control and Prevention’s National Center for Health Statistics from 1973–2006 (appendix pp 3–4). To extend these data, death records from 2006 to 2013 were acquired from individual state departments of public health; missing data thus occur more commonly for the latest time period (2003–13), but cities were included for every year possible (appendix pp 3–5). After assembling data from these sources, we aggregated the death certificates into daily counts of deaths from all-natural causes for all counties associated with each of the 208 cities.
These cities were grouped into nine clusters, adapted from cluster analyses by Nordio and colleagues and Schwartz and colleagues, based on the similarity of their climates (figure 1).2,20 As projected temperatures were available as minimum and maximum daily temperature, we defined temperature as the mean of the daily minimum and maximum temperature values from the bias-corrected and downscaled hydrometeorological dataset.21,22 We selected gridded points within the urban areas for each city, and calculated the mean daily minimum and maximum temperature values over those points to provide a single value for mean temperature on each day in each city in the historical time period. We then fit historical exposure response functions (ERFs) for each city relating the daily death counts with the constructed mean daily temperature measure.
Figure 1:
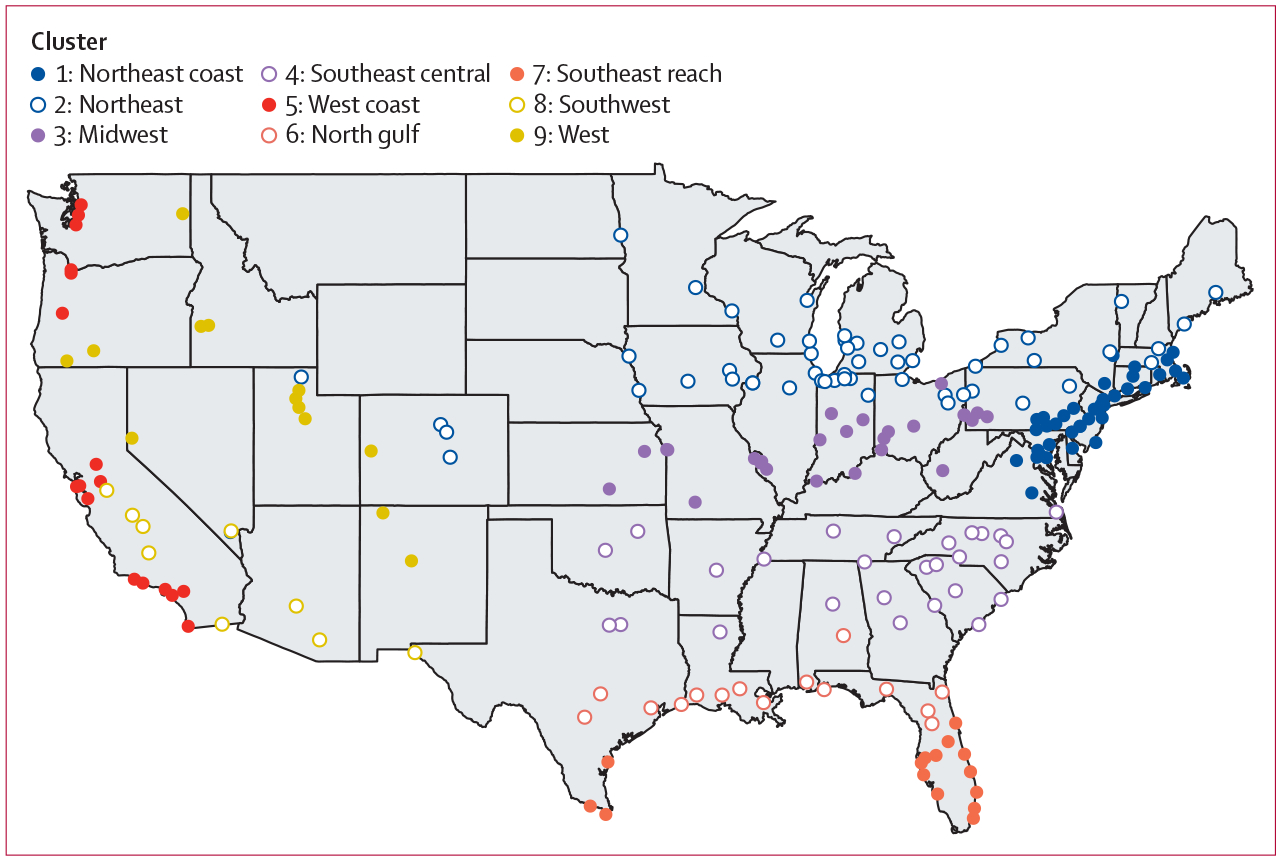
City locations by cluster
To quantify adaptation trends, we fit ERFs separately in four time periods (1973–82, 1983–92, 1993–2002, and 2003–13). The regressions defining the ERFs included terms for both the daily (lag 0) and the 5-day moving average of daily mean temperature. The 5-day moving average generally captures cold-related mortality, while lag 0 generally captures heat effects.2,18,23 However, because heatwaves over several days can also result in increased mortality, 5-day moving average was included as a predictor across the range of temperatures.
We did this analysis in two stages to produce meta-smoothed spline coefficients for mortality due to lag 0 (βt0) and 5-day moving average (βt5) temperatures for each cluster in each of the four time periods. We did cluster-based analysis and adjustment to account for different exposure histories and trends that might have moderated historical relationships between mortality and temperature (appendix p 2).
Identifying adaptation predictors of dose-response changes
To identify and describe mechanisms of adaptation, and to incorporate adaptation into projections of climate-related mortality, we first did meta-regressions to identify possible predictors. We also ran projections based on each of the historical periods for 1°C to 6°C increase from the 1986–2005 baseline period. We related these projections to the proposed predictors.
To examine which factors could potentially modify the mortality-temperature association and result in adaptation, we also undertook meta-regressions for the fitted lag 0 and 5-day moving average terms for each cluster to establish whether city-specific characteristics could explain some of the temporal and spatial differences in exposure-response functions. These meta-regressions included terms for air-conditioning coverage, winter and summer mean temperatures, total population in a relevant year for each time period (1970, 1980, 1990, and 2000), and population aged 65 years or older.2 We normalised population and demographic values to the mean values for each cluster. We obtained data for the total city population and calculated the percentage of people aged 65 years or older using data from the US Census Bureau. We estimated the percentage of households in each city with central air conditioning using data from the American Housing Survey of the US Census Bureau. We calculated the mean and variance of the daily warm season (May to October) temperature for each city using previously published data.21,22 We compared models to identify the predictors most important for explaining the ERF in each cluster,24 using measures of heterogeneity among cities within clusters (Cochran’s Q and I2) along with the Akaike Information Criterion and Bayesian Information Criterion.
Projections of temperature-related mortality
We projected future temperature-related mortality using downscaled and bias-corrected Localised Constructed Analog datasets for Representative Concentration Pathway 8.5 for six global climate models chosen for concordance with previous studies and to encompass a broad range of warming scenarios.25–28 For each model, we selected time periods with projections averaging a 1–6°C change from the 1986–2005 baseline period (appendix p 9). The baseline period was selected for consistency with other climate impact studies published since 2017.22,29,30 We calculated the mean of the projected daily minimum and maximum temperatures for all urban points within each city to produce daily mean temperature values.
We used the cluster-specific meta-smoothed spline coefficients (βt0 and βt5) from each time period to calculate relative risk, attributable risk (AR), and attributable mortality (AN) in the future.16 AN is calculated as the AR of mortality due to temperature on a given day, multiplied by the mean day-of-year mortality over the last time period from the historical dataset.18 We calculated ARt0 to ARt5 and AN for each projected mean daily temperature in 11-year periods around the central year for each climate model at a given temperature change in US temperature (Δ°C, appendix p 9). We did the same calculations for temperatures in the fourth time period (2003–13) to produce a hindcast mortality estimate based on day and year of the temperature:
| 1 |
| 2 |
| 3 |
| 4 |
| 5 |
The hindcast modelled mortality for the 2003–13 time period through the same method used to project future mortality.
For consistency across cities and alignment with the previous analysis by Nordio and colleagues,2 the splines were centred at 15·6°C during the model fitting and meta-smoothing stages, and the resulting AR and AN were relative to this temperature. To calculate the change in mortality due to the projected Δ°C, we subtracted the mean hindcast day-of-year AN from the projected day-of-year AN for each city and model (equations 4–5). For mapping and estimation, we produced projections using the fitted spline for the final time period. To examine the effects of adaptation over time, we also produced projections using the fitted splines for each of the other historical time periods. We corrected all projections using the hindcast from the final time period to allow comparison.
Role of the funding source
The funder of the study had no role in data collection or in performing the data analysis. MCS, a member of the funding agency, participated in analysis, design, and manuscript development, and the funding agency reviewed the manuscript for accuracy and clarity before submission for publication.
Results
Between Oct 26, 2018, and March 9, 2020, we established that differences in vulnerability to temperature were geographically structured. Fitted ERF for the daily mean temperature (lag 0) and the 5-day moving average differed among time periods and geographical clusters in the historical data (figures 1, 2). Most clusters showed evidence of adaptation over time, especially relative to the earliest periods. For example, in cluster 1, the increase in mortality due to temperature in 1973–82 is much higher than the response to temperature in 2003–13 (figure 3, appendix p 12). Generally, the lag 0 ERFs are largest at high temperatures, whereas the 5-day moving average ERFs are largest at the cold extremes. The summed ERF is then high at either extreme, except for the southeast central region in which the lag 0 ERF plateaus at the highest temperatures.
Figure 2: Fitted exposure response functions for total relative risk, the sum of lag 0, and 5-day moving average terms.
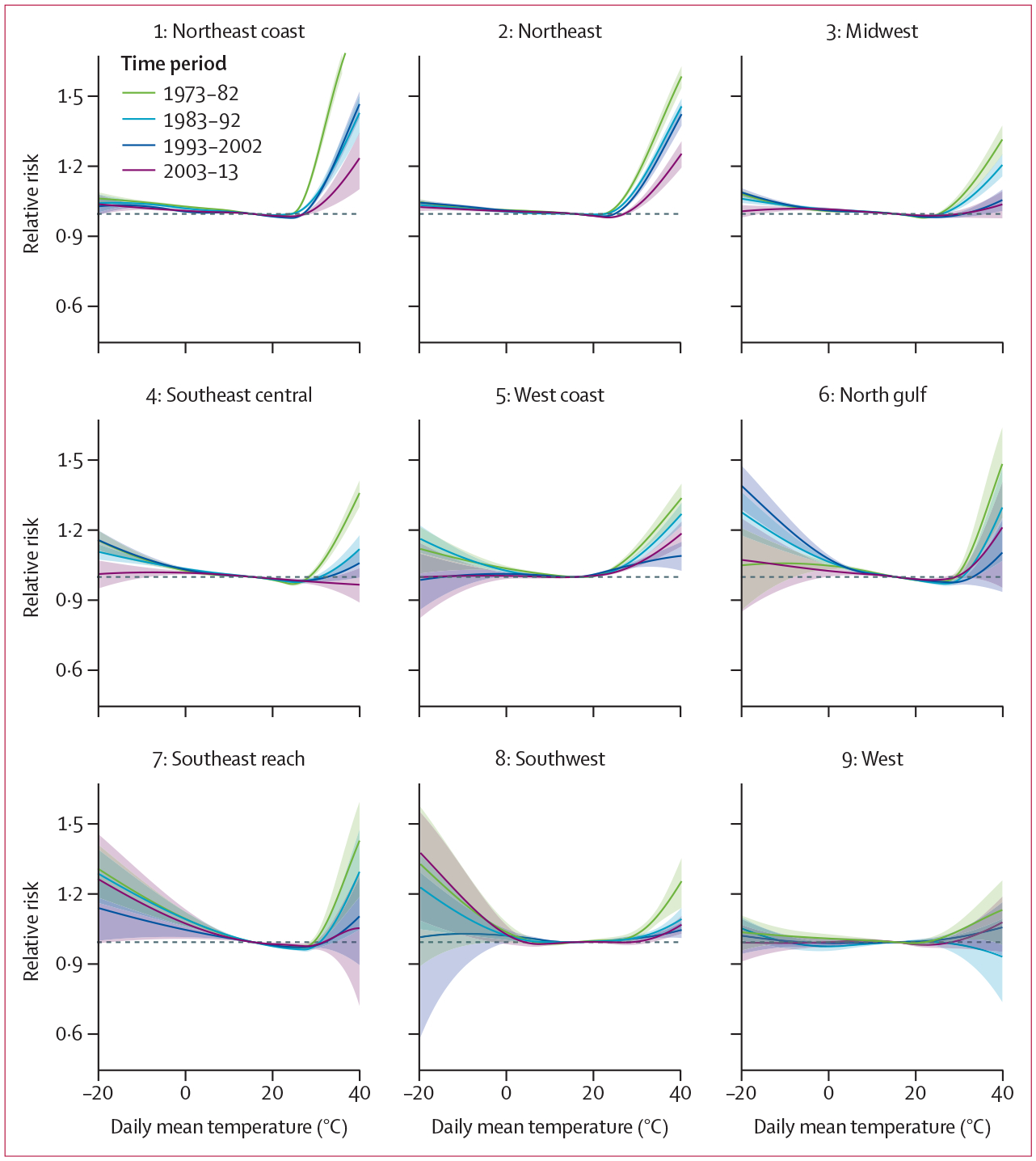
Data shown for all time periods by cluster with the 66% confidence interval around the exposure response function. The horizontal dotted line indicates a relative risk of 1.
Figure 3: Change in attributable risk relative to hindcast at a change of 3°C in relation to seasons and historical time period used in fitting exposure response functions.
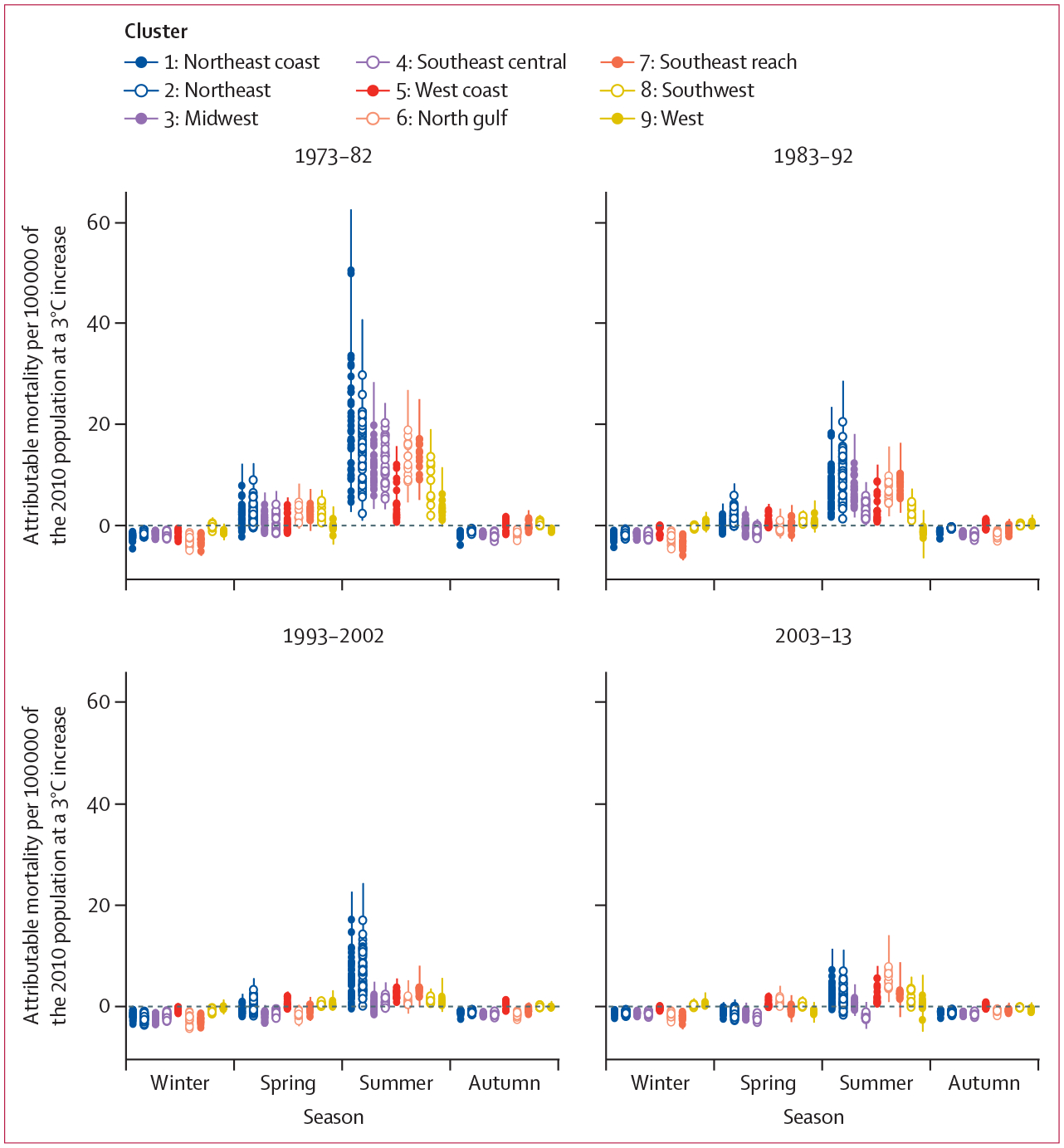
Points represent the central estimate for each city, and whiskers represent the 66% CI around those estimates. Within each season, points are arranged from cluster 1 (left) to cluster 9 (right). Winter was considered as December to February; spring was considered as March to June; summer was considered as July to September; and autumn was considered as October to November, as typical in the northern hemisphere.
Regarding meta-regression, overall no set of predictors explained adaptation entirely across clusters. Unlike the work by Nordio and colleagues,2 we fit ERFs separately for each geographical region. Because the resulting functions had differing numbers of knots, these ERFs could not be simply included in an overall meta-regression. Heterogeneity among cities within each cluster, as indicated by Cochran’s Q and I2, were often reduced by the addition of predictor variables, particularly air conditioning and seasonal mean temperatures (appendix p 9). However, the small number of cities included in each individual cluster analysis, the low variation in some of the predictors within clusters, and tight correlations among some predictor variables resulted in unstable predictions. Because this analysis did not result in clear predictors that could be easily used to estimate ERF under maximum adaptation for each cluster in the future, we also used the fourth time period fit for each cluster as an approximation of projected mortality under a high-adaptation scenario, even without identifying the precise predictors of adaptation.
We projected mortality by degree Celsius of warming using the fitted ERF for each time period and cluster. A reduction in vulnerability to temperature was evident from 1973 to 2013 (table, figures 3, 4, appendix p 14), with the greatest decrease in vulnerability occuring during the warmest months (July to September; figure 3) and in earlier time periods (table, appendix p 14). The effect of heat on increasing mortality is greatly reduced in the 2003–13 fitted dose-response relationship (figure 3, appendix p 14). The change in vulnerability over time leads to large differences in projected mortality under increasing mean temperature; for 3°C scenarios, the reduction in projected mortality between ERF fit on 1973–82 data and 2003–13 data is close to 23 000 deaths, if the population was held constant at 2010 levels in all 208 cities.
Table:
Change in mortality attributable to temperature based on the 2010 population for 208 cities in the USA
| Attributable mortality projected minus hindcast | 66% CI | |
|---|---|---|
| 2°C increase | ||
| 1973–82 | 12 396 | 5923 to 18 549 |
| 1983–92 | 4727 | 859 to 8407 |
| 1993–2002 | 1550 | −1417 to 4377 |
| 2003–13 | 299 | −2438 to 3056 |
| 3°C increase | ||
| 1973–82 | 24 378 | 14 476 to 33 796 |
| 1983–92 | 9760 | 3545 to 15 574 |
| 1993–2002 | 4222 | −350 to 8582 |
| 2003–13 | 1590 | −3025 to 6172 |
| 4°C increase | ||
| 1973–82 | 38 489 | 23 901 to 53 219 |
| 1983–92 | 16 143 | 7640 to 24 563 |
| 1993–2002 | 8289 | 1756 to 14 625 |
| 2003–13 | 3767 | −2948 to 10 455 |
| 5°C increase | ||
| 1973–82 | 56 210 | 34 908 to 77 166 |
| 1983–92 | 24 666 | 12 156 to 37 199 |
| 1993–2002 | 14 134 | 4190 to 23 771 |
| 2003–13 | 7000 | −2639 to 16 718 |
| 6°C increase | ||
| 1973–82 | 90 025 | 69 093 to 111 695 |
| 1983–92 | 41 982 | 26 922 to 56 822 |
| 1993–2002 | 26 700 | 15 419 to 38 086 |
| 2003–13 | 14 610 | 1307 to 28 028 |
Mortality estimates are based on exposure response function for each of the four historical time periods. The greatest reductions in expected mortality due to temperature increase appear to have occurred between the 1970s and 1980s. See appendix p 14 for a graphical representation of the projections in this table.
Figure 4: Projected change in attributable risk at 3°C for each cluster showing the estimated air-conditioning coverage and mean summer temperature for the historical period in which the exposure response functions were fitted.
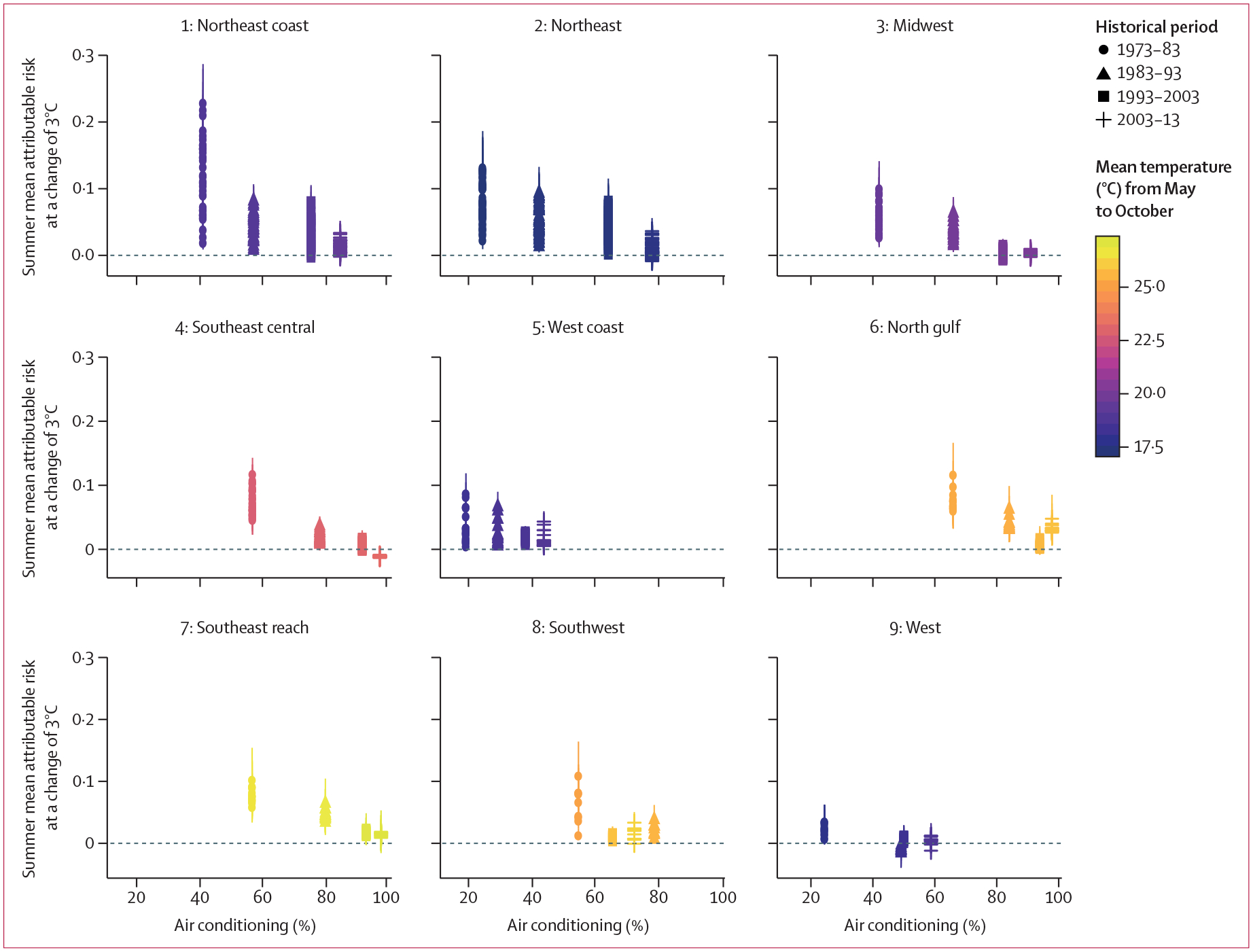
Point colour represents mean summer temperature (°C), with similar colours showing little change in mean temperature.
Cluster 4 has mortality reductions in all seasons. This result is due in part to the plateau in the lag 0 ERF at the high end of the temperature range: however, it is also consistent with the large uncertainties at the temperature extremes (figure 2). The overall pattern of mortality increase by cluster is the same at all temperature ranges, but at 6°C increase results in a doubling of temperature-attributable mortality in multiple clusters (appendix p 14).
In projections based on the 2003–13 ERF, year-round mortality is further offset by reductions in winter mortality in most clusters, as well as spring (March to June) and autumn (October to November) in some clusters (figure 3). The highest increases in summer mortality are seen in northeastern clusters 1 and 2; and in cluster 6, the northern gulf area (figure 3, 5).
Figure 5: Total change in mortality due to temperature increase (°C) compared with the hindcast attributable mortality.
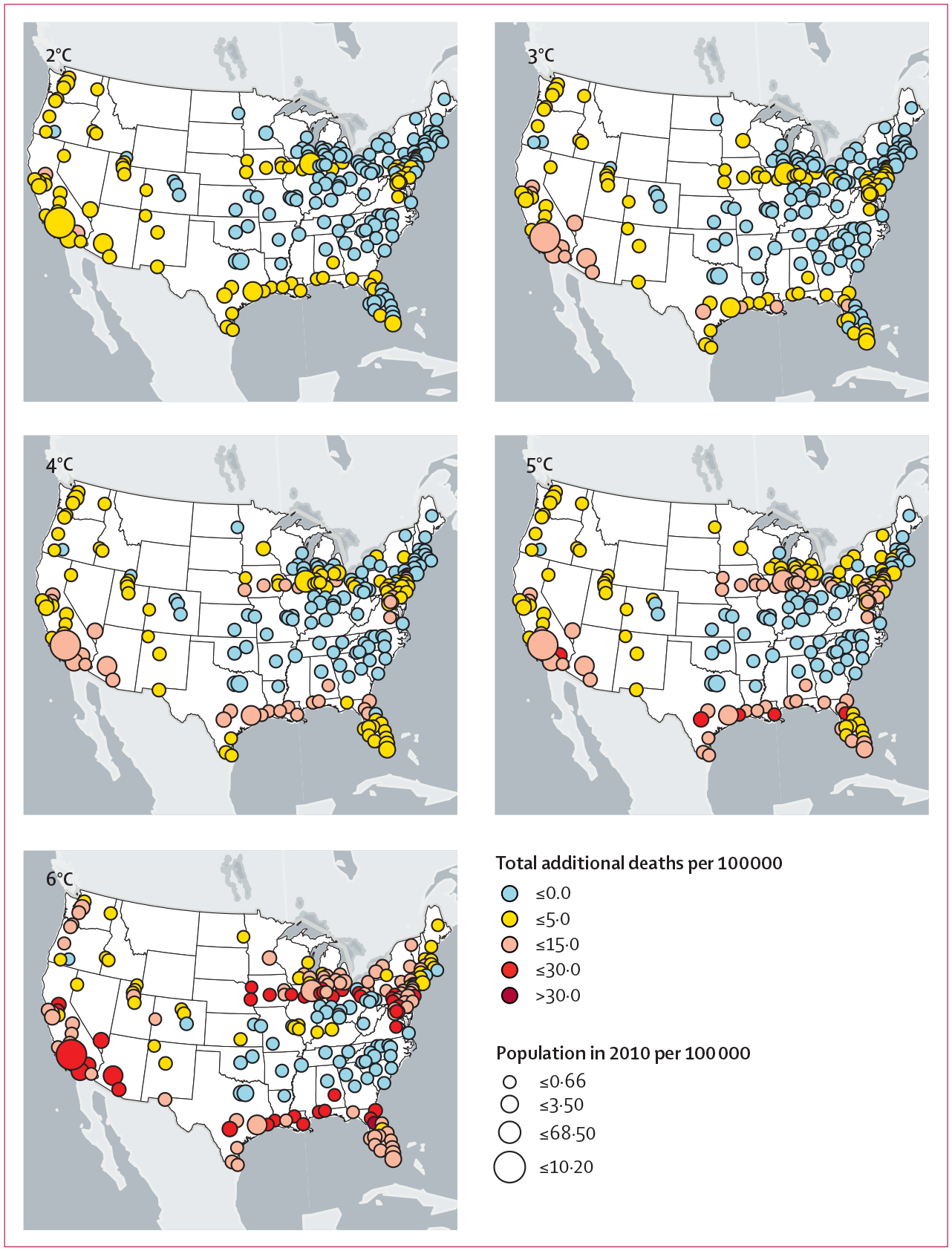
Temperature increases (°C) will be reached within the range of years listed in the appendix (p 9), depending on the global climate model referenced. The 1°C map is not shown because it overlaps with the period used for fitting for most of the global climate models.
Again, the within-cluster meta-regressions did not conclusively show that air conditioning affected the ERF shape (appendix p 9). However, if air-conditioning coverage was responsible for the reduction in summer heat-related mortality over previous time periods, additional reductions in vulnerability to summer heat-related mortality might be small, particularly in the warmest regions (figure 4) where air conditioning is already nearly universally present in households. As expected, air-conditioning coverage in the historical time period did not affect projected differences for the winter AR (appendix p 15). Additionally, the size of the population aged 65 years or older does not appear to greatly increase the AN projections for summer mortality, although it might slightly increase winter mortality (appendix pp 16–17). For projections shown in figure 5, we relied on spline fits from the 2003–13 time period.
Discussion
Past estimates of the net effect of climate change on temperature-related mortality have yielded large numbers, both globally and in the USA; however, few of these studies accounted for actual and potential changes in vulnerability.1–3 We found that temperature extremes for both heat and cold increase mortality rates. Further, we identified evidence of adaptation to heat over a historical period from 1973 to 2013, and used this evidence to inform projections of mortality under future climate models.
Previous efforts to project future temperature-related health effects in a changing climate followed a typical health effect assessment methodology combining empirically based ERFs with future temperature projections and population estimates.2,3,8–10 A limitation of these studies was their ability to account for potential adaptation over time. Since 2017, studies have begun to address this limitation with approaches that account for ways in which historically observed trends in decreasing ERFs might change in the future, particularly through adaptive capacity.16,31 This study accounted for these changes up to 2013.
Consistent with previous studies, we identified reductions in heat-related mortality from 1973 to 2013 in 208 US cities. We observed the largest reductions in heat-related mortality across time between the 1973–82 and the 1983–92 time periods (figure 2, appendix p 12), with lower but continued reductions between each subsequent time period. Trends appeared for most of the USA, but varied across the nine climate zones, with evidence suggesting in some regions, such as the northern gulf coast, that either adaptation measures have reached their limit or are being offset by increases in vulnerability (eg, due to an increasing proportion of the population being aged 65 years or older, appendix p 17). Although the 208 cities in the analysis hold almost 60% of the total US population, these trends are likely to be different in smaller cities or rural areas.
Evidence is growing of reductions in vulnerability to heat-related mortality over time.1 Various mechanisms for this adaptation have been proposed. Hondula and colleagues presented four groupings of adaptive behaviour, namely physiological, behavioural, infrastructural, and technological.32 Increased prevalence of air conditioning in hot regions and, over time, nationwide might explain both geographical and temporal adaptation trends of reduced population vulnerability to heat; however, evidence in support of this idea remains mixed.17 This study found that reductions in vulnerability to heat observed in the ERF for each cluster over time could not be entirely explained by available data for air conditioning, age, or changes in seasonal mean temperatures, which is similar to findings of previous authors.33 However, data for air conditioning use among some of the populations at greatest risk for heat-related death (eg, older adults and individuals with low incomes) are not available; thus, we cannot draw firm conclusions about this factor. Past research has, however, shown that even with access to air conditioning, vulnerable populations might elect not to use it during extreme temperatures out of concern for the associated electrical bills.1,31,34 We did not examine the effects of poverty, living situation, or chronic disease on outcomes due to the insufficient data with which to make statistically significant conclusions; however, changes in populations experiencing such added stressors could greatly increase their vulnerability. Further study with focused datasets that link income and energy cost to air conditioning use would better address such issues. We also did not consider the effects of humidity or heatwave conditions other than those identified in the 5-day moving average, which have been shown to affect heat-related mortality in multiple countries.35
The evidence for adaptive capacity has been based, in part, on current, well established geographical differences in ERFs related to prevailing climate. Specifically, heat related mortality effects are lower in the warmer southern regions of the USA than the more northern locations.3,36 This general difference might reflect a combination of physiological adaptation, changing behaviour patterns, and differences in infrastructure, including air conditioning, building design, and construction materials.1,31,32 Our findings suggest that decreased winter mortality in some regions could drive reductions in overall annual temperature-related mortality under the scenarios with the smallest mean increases in temperature (figure 3). This finding was particularly true in warmer areas, such as Florida, but was evident in colder areas such as the northeast as well. However, as in previous studies, we might have overestimated cold-related mortality by not completely controlling for other winter season contributors to mortality that could masquerade as cold-temperature effects, such as influenza and limited daylight hours. Cold extremes generally show more uncertainty in the temperature-mortality relationship than heat extremes (figure 2). This uncertainty could be due to confounding seasonal effects such as influenza, reduced daylight hours, and a longer temporal lag between a given cold event and related mortality.33,37 Additionally, with further temperature increases, any reduction in mortality in the winter is more than exceeded by warm-weather mortality increases in most regions.
In general, as temperatures increase with climate change, we project that deaths due to heat are likely to outweigh decreases in cold-related mortality in most of the studied US locations. At increases of 4°C, national-level reductions in cold-related mortality were outweighed by increases in mortality due to heat. At increases of 6°C, we projected much larger increases in mortality in most regions. Cluster 4, the southeast central region of the country, had a central estimate ERF to temperature that was fairly flat at higher temperatures, and even trended slightly downward. This trend of flat or declining ERF at high temperatures resulted in projected decreases with increasing temperatures in cluster 4, although CIs around projections encompassed zero. In general, we expect the 5-day moving average term to flatten or trend back upward with temperature, and to contribute less to mortality at higher temperatures, which occurred for most clusters. The unusual curve fit in cluster 4 might have been caused by fitting the lag 0 term concurrently with the 5-day moving average term, without sufficiently accounting for differences in relationships that might occur with seasonal changes. Schwartz and colleagues fit each month separately, and this approach, or an approach accounting for interactive effects of season, could clarify the relationship.20 By contrast, clusters 6 and 8 in the northern gulf of Mexico and the southernmost tips of Florida and Texas showed substantial increases in mortality due to heat at the hottest temperatures.
Uncertainty around the estimated ERFs at temperatures greater than those observed historically, or which have not been frequently observed in previous years, poses a challenge for accurate projections. Multiple strategies have been used, including assuming that the projected mortality rates are constant at temperatures higher than those used to determine the observed relationship of temperature and mortality.15 The approach we chose fixes the temperature response curve to a log-linear extension of the interior portion of the curve beyond the highest temperatures used in the historical analysis. This method has the benefit of identifying the last-observed portion of the trend, but does not resolve the issue of uncertainty. Additional data and an improved understanding of the predictors that might drive the fit of the curve, specifically close attention to demographics and living or working circumstances, are likely to improve future estimates. An additional strategy that might be useful for other studies would be to treat historical period as an additional variable. This strategy might improve power and reduce uncertainty in regions of the curve with more consistent temperature measurements over time.
Estimating both the anticipated risks of climate change and the degree to which communities can prepare for temperature increases to reduce the risk of mortality in their populations can inform public policy in multiple ways. As has been shown previously, we found that adaptation to climate change over time has occurred throughout the USA. Even so, increased mortality due to future warming temperatures is probable in many regions, particularly those areas where further adaptation might not be possible. In addition, if warming happens quickly, adaptation might not occur quickly enough to reduce vulnerability. This study highlights the potential for adaptation at the local level to minimise the effects of global change, as well as the fact that at higher levels of climate change there could be limits to further adaptation.
Supplementary Material
Research in context.
Evidence before this study
We considered peer-reviewed primary and review articles focused on characterising effects of extreme temperatures on historical mortality, estimating mortality under future climate change, and evidence of adaptation to climate change in human populations. We relied on knowledge of the existing literature and databases and searched Google Scholar and PubMed. Search terms from database inception up until June 1, 2020, included “climate change”, “extreme temperatures”, “mortality”, “vulnerability”, “adaptation”, “climate adaptation”, “vulnerable populations”, “demographics”, “air conditioning”, “global climate model”, “heat-related mortality”, “cold-related mortality”, and “cooling centers”. All identified sources had English language versions, and literature included international studies. These sources could be biased towards researchers in North America and Europe, and towards findings that show evidence of adaptation and changes in mortality with extreme temperatures.
Added value of this study
Our study estimates mortality due to extreme temperatures under projected temperatures from six global climate models while accounting for changes in vulnerability to temperature over time. Previous studies have also found evidence of adaptation to climate change. Our study characterised this pattern based on newly available mortality data from 2006 to 2013, and offered methods to characterise the limits of adaptation in addressing mortality due to extreme temperatures.
Implications of all the available evidence
This study provides evidence of reduction in vulnerability through adaptations such as improved public notification systems and cooling centres, which provide air conditioning to those in need. However, the results suggest that increased mortality due to climate change is probable in many regions, particularly in regions that have already enacted substantial changes to reduce mortality due to extreme temperatures. These findings have implications for public policy, highlighting the importance of both mitigation to reduce future warming and continued investment in adaptive measures, such as social outreach programmes, to reduce the impact of that warming.
Acknowledgments
We thank Alexis St Juliana, Joel Smith, Victoria Aragon, Sara Sokolinksi, Diane Callow, Erin Miles, and Justin Stein of Abt Associates for preparing supporting figures, helpful review comments, and submitting the final manuscript. The US Environmental Protection Agency provided funding for this research through contract EP-BPA-18-H-0011 and order number 68HE0H18F0184 with Abt Associates. The preparation of the manuscript was also supported with Abt Associates internal funds. The paper was improved by presentation at Abt Associates’ Work in Progress Seminar (March 26, 2020; online) and comments received as a part of that process. The views expressed in this document are solely those of the authors and do not necessarily reflect those of their affiliated institutions, including the US Environmental Protection Agency.
Funding
The US Environmental Protection Agency and Abt Associates.
Footnotes
Declaration of interests
We declare no competing interests.
For the Science Hub see https://doi.org/10.23719/1520971
See Online for appendix
Data sharing
Mortality data from 2006 to 2013 were obtained from state health departments and had to be destroyed at the end of the relevant data use agreements. Those data are available from the respective US state health departments upon completion of data use agreements with each department. All other data are publicly available with no restrictions. Processed de-identified datasets used in analytical work as well as analytical code and supporting documentation will be made available on the Environmental Protection Agency’s Science Hub. Author approval is not required for use.
References
- 1.Kinney LP. Temporal trends in heat-related mortality: implications for future projections. Atmosphere 2018; 9: 409. [Google Scholar]
- 2.Nordio F, Zanobetti A, Colicino E, Kloog I, Schwartz J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ Int 2015; 81: 80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarofim M, Saha S, Hawkins M, et al. 2: Temperature-related death and illness. The impacts of climate change on human health in the United States: a scientific assessment. US Global Change Research Program: Washington, DC, 2016. https://health2016.globalchange.gov/low/ClimateHealth2016_02_Temperature_small.pdf (accessed March 18, 2021). [Google Scholar]
- 4.McMichael AJ, Wilkinson P, Kovats RS, et al. International study of temperature, heat and urban mortality: the ‘ISOTHURM’ project. Int J Epidemiol 2008; 37: 1121–31. [DOI] [PubMed] [Google Scholar]
- 5.Bathiany S, Dakos V, Scheffer M, Lenton TM. Climate models predict increasing temperature variability in poor countries. Sci Adv 2018; 4: eaar5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayhoe K, Wuebbles DJ, Easterling DR, et al. Our changing climate. Impacts, risks, and adaptation in the United States: Fourth National Climate Assessment Washington, DC. Washington DC: US Global Change Research Program, 2018. [Google Scholar]
- 7.Kornhuber K, Coumou D, Vogel E, et al. Amplified Rossby waves enhance risk of concurrent heatwaves in major breadbasket regions. Nat Clim Chang 2020; 10: 48–53. [Google Scholar]
- 8.Gasparrini A, Guo Y, Sera F, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health 2017; 1: e360–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morefield PE, Fann N, Grambsch A, Raich W, Weaver CP. Heat-related health impacts under scenarios of climate and population change. 2018; 15: 2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanderson M, Arbuthnott K, Kovats S, Hajat S, Falloon P. The use of climate information to estimate future mortality from high ambient temperature: a systematic literature review. PLoS One 2017; 12: e0180369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knowlton K, Lynn B, Goldberg RA, et al. Projecting heat-related mortality impacts under a changing climate in the New York City region. Am J Public Health 2007; 97: 2028–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mills D, Schwartz J, Lee M, et al. Climate change impacts on extreme temperature mortality in select metropolitan areas in the United States. Clim Change 2015; 131: 83–95. [Google Scholar]
- 13.Gosling SN, Lowe JA, McGregor GR, Pelling M, Malamud BD. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Clim Change 2009; 92: 299–341. [Google Scholar]
- 14.Watkiss P, Hunt A, Blyth W, Dyszynski J. The use of new economic decision support tools for adaptation assessment: a review of methods and applications, towards guidance on applicability. Clim Change 2015; 132: 401–16. [Google Scholar]
- 15.Gosling SN, Hondula DM, Bunker A, et al. Adaptation to climate change: a comparative analysis of modeling methods for heat-related mortality. Environ Health Perspect 2017; 125: 087008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petkova EP, Vink JK, Horton RM, et al. Towards more comprehensive projections of urban heat-related mortality: estimates for New York City under multiple population, adaptation, and climate scenarios. Environ Health Perspect 2017; 125: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostro B, Rauch S, Green S. Quantifying the health impacts of future changes in temperature in California. Environ Res 2011; 111: 1258–64. [DOI] [PubMed] [Google Scholar]
- 18.Vicedo-Cabrera AM, Sera F, Gasparrini A. Hands-on tutorial on a modeling framework for projections of climate change impacts on health. Epidemiology 2019; 30: 321–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carleton T, Delgado M, Greenstone M, et al. Valuing the global mortality consequences of climate change accounting for adaptation costs and benefits. Becker Friedman Institute for Economics 2018; 54: 2018–51. [Google Scholar]
- 20.Schwartz JD, Lee M, Kinney PL, et al. Projections of temperature-attributable premature deaths in 209 U.S. cities using a cluster-based Poisson approach. Environ Health 2015; 14: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Livneh B, Bohn TJ, Pierce DW, et al. A spatially comprehensive, meteorological data set for Mexico, the U.S., and southern Canada (NCEI Accession 0129374). NOAA National Centers for Environmental Information. 10.7289/v5x34vf6 (accessed March 18, 2021). [DOI] [Google Scholar]
- 22.Wobus C, Zarakas C, Malek P, et al. Reframing future risks of extreme heat in the United States. Earths Futur 2018; 6: 1323–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braga ALF, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect 2002; 110: 859–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gasparrini A, Armstrong B, Kenward MG. Multivariate meta analysis for non-linear and other multi-parameter associations. Stat Med 2012; 31: 3821–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pierce DW, Cayan DR, Thrasher BL. Statistical downscaling using localized constructed analogs (LOCA). J Hydrometeorol 2014; 15: 2558–85. [Google Scholar]
- 26.University of California San Diego. LOCA statistical downscaling. Scripps Institution of Oceanography. 2017. http://loca.ucsd.edu/ (accessed April 16, 2021).
- 27.Lay CR, Mills D, Belova A, et al. Emergency department visits and ambient temperature: evaluating the connection and projecting future outcomes. Geohealth 2018; 2: 182–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belova A, Mills D, Hall R, et al. Impacts of increasing temperature on the future incidence of West Nile neuroinvasive disease in the United States. Am J Clim Change 2017; 6: 166–216. [Google Scholar]
- 29.Wobus C, Zheng P, Stein J, et al. Projecting changes in expected annual damages from riverine flooding in the United States. Earths Futur 2019; 7: 516–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US Global Change Research Program. Climate Science Special Report: Fourth National Climate Assessment. 2017. https://data.globalchange.gov/report/climate-science-special-report (accessed April 16, 2021).
- 31.Vicedo-Cabrera AM, Sera F, Guo Y, et al. A multi-country analysis on potential adaptive mechanisms to cold and heat in a changing climate. Environ Int 2018; 111: 239–46. [DOI] [PubMed] [Google Scholar]
- 32.Hondula DM, Balling RC Jr, Vanos JK, Georgescu M. Rising temperatures, human health, and the role of adaptation. Curr Clim Change Rep 2015; 1: 144–54. [Google Scholar]
- 33.Kinney PL, Schwartz J, Pascal M, et al. Winter season mortality: will climate warming bring benefits? Environ Res Lett 2015; 10: 064016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayrhuber EA, Dückers MLA, Wallner P, et al. Vulnerability to heatwaves and implications for public health interventions—a scoping review. Environ Res 2018; 166: 42–54. [DOI] [PubMed] [Google Scholar]
- 35.Armstrong B, Sera F, Vicedo-Cabrera AM, et al. The role of humidity in associations of high temperature with mortality: a multicountry, multicity study. Environ Health Perspect 2019; 127: 97007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 2002; 155: 80–87. [DOI] [PubMed] [Google Scholar]
- 37.Arbuthnott K, Hajat S, Heaviside C, Vardoulakis S. What is cold-related mortality? A multi-disciplinary perspective to inform climate change impact assessments. Environ Int 2018; 121: 119–29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Mortality data from 2006 to 2013 were obtained from state health departments and had to be destroyed at the end of the relevant data use agreements. Those data are available from the respective US state health departments upon completion of data use agreements with each department. All other data are publicly available with no restrictions. Processed de-identified datasets used in analytical work as well as analytical code and supporting documentation will be made available on the Environmental Protection Agency’s Science Hub. Author approval is not required for use.


