Background
Psychological safety—the belief that it is safe to speak up—is vital amid uncertainty, but its relationship to feeling heard is not well understood.
Purpose
The aims of this study were (a) to measure feeling heard and (b) to assess how psychological safety and feeling heard relate to one another as well as to burnout, worsening burnout, and adaptation during uncertainty.
Methodology
We conducted a cross-sectional survey of emergency department staff and clinicians (response rate = 52%; analytic N = 241) in July 2020. The survey measured psychological safety, feeling heard, overall burnout, worsening burnout, and perceived process adaptation during the COVID-19 crisis. We assessed descriptive statistics and construct measurement properties, and we assessed relationships among the variables using generalized structural equation modeling.
Results
Psychological safety and feeling heard demonstrated acceptable measurement properties and were correlated at r = .54. Levels of feeling heard were lower on average than psychological safety. Psychological safety and feeling heard were both statistically significantly associated with lower burnout and greater process adaptation. Only psychological safety exhibited a statistically significant relationship with less worsening burnout during crisis. We found evidence that feeling heard mediates psychological safety’s relationship to burnout and process adaptation.
Conclusion
Psychological safety is important but not sufficient for feeling heard. Feeling heard may help mitigate burnout and enable adaptation during uncertainty.
Practice Implications
For health care leaders, expanding beyond psychological safety to also establish a feeling of being heard may further reduce burnout and improve care processes.
Key words: Burnout, crisis, psychological safety
The complexity, uncertainty, and high stakes of health care make it vital that clinicians and staff can speak up with questions and ideas, admit mistakes, and ask for help when needed. Psychological safety—the belief that it is safe to take interpersonal risks such as by speaking up—is thus particularly salient in health care environments (Edmondson et al., 2016; O’Donovan & McAuliffe, 2020; Rosenbaum, 2019). By enabling issues to surface that otherwise might remain unexplored, psychological safety can spark learning and help teams improve, which is highly desirable in health care delivery (Tucker et al., 2007). Numerous studies have documented this value in various contexts; for instance, psychological safety can improve teamwork in intensive care units (Diabes et al., 2020), facilitate technology implementation in operating rooms (Edmondson, 2003; Edmondson et al., 2001), enhance care timeliness in primary care (Nembhard et al., 2015), and reduce emotional exhaustion among clinicians (Rathert et al., 2020).
However, feeling safe to speak up is not equivalent to feeling heard. Employees, especially those with lower status roles, often speak up only to be shot down, preventing valuable ideas from reaching implementation and causing frustration among staff (Satterstrom et al., 2021). Feeling heard—which we define as the belief that the content of one’s voiced ideas or questions will be recognized and responded to—may be complementary to feeling psychologically safe, but it has not been adequately accounted for in research and practice. Although feeling heard has been recognized as worth measuring and addressing for patients (e.g., Gramling et al., 2016), it has not been widely applied regarding clinicians and staff. If clinicians and staff feel safe to share their ideas and questions but simultaneously believe that their efforts to speak up will go unrecognized and unaddressed, there may be consequences both for individuals’ emotional exhaustion and burnout at work, as well as for their ability to materially improve the work processes in which they engage. Understanding the phenomenon of feeling heard and how it relates to psychological safety, clinician experience, and process adaptation is thus vital for health care organizations.
Psychological safety and feeling heard are particularly important to understand in work environments facing uncertainty, where burnout and the need to adapt are especially salient. In its original conceptualization, psychological safety was seen as a critical means of mitigating anxiety and facilitating information flow during uncertainty and change (Schein & Bennis, 1965). Individuals are more likely to withhold information when they are not confident in it, even if the uncertain information is important—a problematic tendency that psychological safety mitigates (Siemsen et al., 2009). Beyond informational benefits, psychological safety offers value for individual worker experience and stress when facing uncertainty; for example, research studying health care workers during the early COVID-19 pandemic in China found psychological safety to protect against distress over time (Ahmed et al., 2021). Feeling heard may be similarly relevant amid uncertainty and crisis, as high pressures and anxieties might amplify the importance of feeling that one’s concerns will be taken seriously.
In this study, we examine psychological safety and feeling heard in a deeply uncertain, high-pressure environment: emergency departments (EDs) during the early, greatly uncertain phase of the COVID-19 crisis. High rates of burnout were recorded among emergency medicine personnel even early in the pandemic (Rodriguez et al., 2021), and because the ED was on the frontline of care during COVID-19, clinicians and staff had to rapidly and proactively adapt care processes amid great uncertainty (Stark et al., 2020). These factors make emergency medicine during COVID-19 a practically important and theoretically interesting setting in which to understand how psychological safety and feeling heard relate to one another and how, if at all, they are associated with burnout and adaptation amid uncertainty.
Theory
To conceptualize why psychological safety and feeling heard may be particularly relevant for burnout during periods of high uncertainty, we draw on conservation of resources theory (Hobfoll, 1989, 2001), which has been applied to worker burnout both within and outside health care (Williams et al., 2019). Conservation of resources theory suggests that employees experience stress when resources are lost or prevented from growing such that employees’ ability to meet their job demands is threatened and, when experienced chronically, leads to burnout (Hobfoll & Freedy, 1993). For instance, nurses experience stress when they face time pressure and long hours that make it difficult for them to complete patient care tasks or find time for nonwork activities (Prapanjaroensin et al., 2017). This can lead to rational but problematic behaviors as workers try to strategically address resource shortages. For example, physicians might respond to inadequate time for patient care by “stealing” time from other areas of their lives that would otherwise be resource replenishing, such as activities outside work and social interaction (Rathert et al., 2018).
Resource conservation is particularly helpful for conceptualizing burnout during periods of crisis and uncertainty because of the sudden and extreme resource depletion imposed by turmoil. For frontline clinicians and staff during the COVID-19 pandemic, resources prone to depletion include task time as caseloads reached capacity, material protection as personal protective equipment stores were depleted, social networks as workers were redeployed to makeshift COVID-19 units with unfamiliar team members, and regenerative time as workers avoided loved ones in fear of bringing COVID-19 home from the hospital. Facing such sudden and multipronged resource depletion, workers seeking to recover resources or stymie their loss as much as possible would need to ask questions and raise their concerns to managers and leaders who control the resources they need, such as staffing arrangements, mask deployment, time off, or information about rapidly changing care protocols. These conditions are likely to make the ability to speak up—and to have one’s ideas be heard—particularly salient.
Speaking up is facilitated by a climate of psychological safety, in which people have a shared belief that it is safe to take interpersonal risks such that they will not be punished for asking questions, admitting mistakes, or seeking help (Edmondson, 1999; Edmondson & Lei, 2014; Schein & Bennis, 1965). Past research has established the importance of individuals’ experience of psychological safety for individual outcomes, for example, finding positive relationships to engagement and creativity at work (Gong et al., 2012; Siemsen et al., 2009). Although these concepts are conceptually related to burnout, literature rigorously associating psychological safety and burnout in health care has been lacking, prompting recent calls for more (Swendiman et al., 2019) and new studies exploring their relationship (Rathert et al., 2020). Consistent with this recent research, we hypothesize that psychological safety is associated with less overall burnout, and given the intensification of resource depletion amid great uncertainty, we further hypothesize that psychological safety is associated with less worsening burnout during crisis.
In addition, we hypothesize that psychological safety is related to greater process adaptation during crisis. We define process adaptation as the adjusting of work processes to become more suited to the environment. This is an important complementary concept to burnout in the context of COVID-19 because the uncertainty inherent to the pandemic caused challenges not only for worker burnout but also a need for new processes for delivering care, particularly in emergency medicine where care protocols changed rapidly and new personal protective equipment rules substantively altered care delivery (Hayirli et al., 2021; Stark et al., 2020). In this challenging context, the ability to speak up and be heard is likely related to the ability to better adapt processes because new ideas are more likely to surface at the point of care, where process problems are evident. Indeed, at its core, the employee voice that is encouraged by psychological safety is about the discretionary offering of constructive ideas for improving organizational functioning (Hirschman, 1970; Morrison, 2011).
Research has documented barriers that prevent new process adaptation ideas from surfacing from employees and related implications for performance, such as strong professional hierarchies that constrain speaking up (Nembhard & Edmondson, 2006) and the tendency for people to withhold information about which they are uncertain (Siemsen et al., 2009). Research has also shown that health care workers are less likely to report near-miss events when they have high harm potential, which leads, ironically, to failing to learn about the most important opportunities for prevention (Jung et al., 2021). Psychological safety and team members’ speaking up have been associated with the ability to adapt amid uncertainty such as in new technology implementation in surgery (Edmondson, 2003) and amid the uncertain environments of intensive care units (Tucker et al., 2007). However, although psychological safety has been documented as important for adaptation amid uncertainty, it has not been explored under the intense uncertainty of a crisis context, and the related role of feeling heard for process adaptation has remained unexplored.
Hypothesis 1. Psychological safety is negatively associated with burnout (H1a) and worsening burnout (H1b) and is positively associated with process adaptation (H1c) amid uncertainty.
Nonetheless, the underlying tenets of conservation of resources theory suggest that psychological safety, though helpful, is only part of the equation. At its core, psychological safety enables people to speak up with concerns, questions, and requests for help and that should increase the likelihood that people feel heard and responded to. Indeed, we hypothesize that psychological safety is associated with greater feelings of being heard.
Hypothesis 2. Psychological safety is associated with greater feelings of being heard (H2).
However, psychological safety does not guarantee feeling heard, with implications for burnout and adaptation. Raising concerns, questions, and ideas is not without cost; it requires time and effort, which are often scarce resources during periods of crisis. If workers raising their voices feel they are neglected or ignored, their resources may ultimately be more depleted rather than less. Past research in related areas lends support to this notion. For instance, qualitative research among nurses shows that individuals’ assessments of whether and how their messages are received by managers is important for their work satisfaction (Garon, 2012). Research on process improvement teams in health care documents how people who voice their ideas in meetings but perpetually feel they are not heard can become frustrated—even leading them to quit (Satterstrom et al., 2021). Feeling heard may thus be vital for reducing burnout directly, and it may also be a conduit through which psychological safety affects burnout indirectly.
We hypothesize similarly for feeling heard and process adaptation. From a conservation of resources perspective, if individuals feel safe to raise ideas but believe they will not be heard, they may strategically choose to withhold their ideas to conserve their time and effort. This notion is supported by research showing that individuals are more likely to speak up when they perceive that their idea will have greater impact (Sherf et al., 2021). When individuals withhold their ideas, opportunities for learning and improvement are lost. Indeed, actual process improvement requires that new ideas about processes be heard and addressed. We hypothesize that feeling heard is associated with greater process adaptation during crisis and that feeling heard partially mediates the relationship of psychological safety and process adaptation.
Hypothesis 3. Feeling heard is negatively associated with burnout (H3a) and worsening burnout (H3b) and positively associated with process adaptation (H3c) amid uncertainty.
Hypothesis 4. Feeling heard partially mediates the relationship of psychological safety and (H4a) burnout, (H4b) worsening burnout, and (H4c) process adaptation.
Figure 1 displays the conceptual framework of hypothesized relationships among psychological safety, feeling heard, burnout, worsening burnout, and adaptation.
Figure 1.
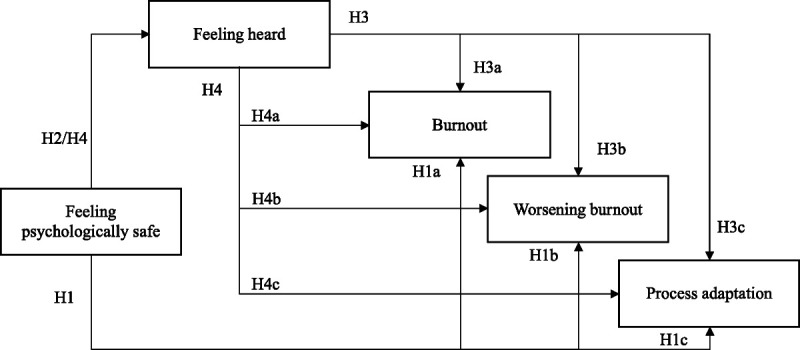
Conceptual framework depicting hypothesized relationships among psychological safety, feeling heard, burnout, worsening burnout, and process adaptation.
Methods
Survey Sampling and Administration
To minimize response burden during the already burdensome COVID-19 pandemic, we sampled clinicians and staff in two large general EDs affiliated with an academic medical center in California (other EDs in the system were excluded because they were pediatric-focused). The survey was administered to the following clinician and staff roles: attending physicians, residents and fellows, advanced practice providers including physician assistants and nurse practitioners, registered nurses, pharmacists, respiratory therapists, greeters, technicians, and social workers. Guided by expert input, we focused on these roles as most central to providing acute unscheduled medical care, a method of focused role-based selection that has been used when measuring psychological safety and related constructs in other health care settings (see Diabes et al., 2020). The two EDs from which the sample was drawn had similar operational responses to the COVID-19 pandemic, as policies were set centrally; they also had similar structural contexts, as they were part of the same organization. Although one ED’s hospital provided highly specialized quaternary-level medical care whereas the other served as a safety-net hospital and trauma center, the clinician and staff survey responses analyzed in this article were similar in both settings. The study was approved by institutional review boards at the Harvard T. H. Chan School of Public Health and the University of California San Francisco.
The final sample frame included 635 clinicians and staff (375 at one site and 269 at the other). We fielded the survey from June 29 to July 28, 2020 online in English via Qualtrics. During the weeks that the survey was in the field, the COVID-19 case count in the county ranged from 3,561 to 6,505, as compared to a high of 2,320 and low of 108 during the first 2 months of the pandemic. The survey took about 10 minutes to complete. Respondents received a $5 gift card for participating. We received 328 responses, for a response rate of 52%. For descriptive statistics, we excluded 87 respondents who did not answer a majority of relevant questions for an analytic sample of 241 respondents.
Table 1 presents analytic sample characteristics. There was representation across multiple roles: 31.5% of respondents were attendings, residents/fellows, or advanced practice providers; 49.0% were registered nurses; and 18.3% were in other roles (pharmacists, respiratory therapists, social workers, and greeters). This distribution of roles was similar to the distribution of roles in the units we studied (e.g., 33.5% in the unit were attendings, resident/fellows, or advanced practice providers, as compared to the 31.5% in our sample). A majority of respondents had tenure in their ED of more than 5 years (54.8%); 33.6% were male, and 54.4% were White.
Table 1.
Analytic sample characteristics (N = 241)
| Characteristics | n (%) |
|---|---|
| Gender | |
| Female | 138 (57.3) |
| Male | 81 (33.6) |
| Nonbinary | 2 (0.8) |
| Prefer not to answer | 20 (8.3) |
| Race | |
| White | 131 (54.4) |
| Black | 15 (6.2) |
| Asian/Hawaiian/Pacific Islander | 39 (16.2) |
| Other | 15 (6.2) |
| Prefer not to answer | 41 (17) |
| Ethnicity | |
| Hispanic | 28 (11.6) |
| Not Hispanic | 190 (78.8) |
| Prefer not to answer | 23 (9.5) |
| Role | |
| Attending, resident/fellow, advanced practice provider | 76 (31.5) |
| Registered nurse | 118 (49.0) |
| Other: pharmacist, respiratory therapist, social worker, greeter | 44 (18.3) |
| No response | 3 (1.2) |
| Age, mean (SD) | 39.3 (8.9) |
| Tenure | |
| Less than 2 years | 44 (18.3) |
| 2–5 years | 64 (26.6) |
| More than 5 years | 132 (54.8) |
| Site | |
| Hospital 1 | 146 (60.6) |
| Hospital 2 | 95 (39.4) |
Survey Development
We developed the survey based on past research pertaining to psychological experience at work. The survey was part of a broader study of staff and clinician experience during the COVID-19 pandemic. For this study, we focused on two domain constructs as predictor variables (psychological safety and feeling heard) and three outcome variables (burnout, worsening burnout during the crisis, and process adaptation). Measures were adapted from previously developed instruments, with wording modifications for appropriateness in the ED setting (see the Measures section); we selected the most relevant subset of items from existing scales to further minimize response burden. We conducted confirmatory factor analysis to assess the psychometric properties of the adapted, previously validated measures. The survey was cognitively tested with three organizational insiders, and wording was modified for clarity.
Measures
We used three items to measure psychological safety adapted for the ED (Edmondson, 1999; Nembhard & Edmondson, 2006), asking “in this ED” whether “People are comfortable checking with each other if they have questions about the right way to do something,” “People are able to bring up problems and tough issues,” and “If you make a mistake, it is often held against you”—the last of which was reverse-coded in analysis to address its negative framing.
Although psychological safety is often measured as a collective team-level concept (Edmondson, 1999), because we were interested in individuals’ experience of psychological safety as it related to individual experience of feeling heard, we measured and operationalized psychological safety at the individual level from the respondent’s perspective. Items were each measured on 5-point Likert scales, and we created domain scores by averaging these three items.
To measure feeling heard, we adapted three items pertaining to individuals’ experience of feeling heard, drawn from a broader scale used in psychology research to measure one’s personal sense of power at work (Anderson et al., 2012). The three items that focus on feeling heard that we selected for our research included “I can get them to listen to what I say,” “Even if I voice my views, my views have little sway” (reverse-coded), and “My ideas and opinions are often ignored” (reverse-coded). Respondents answered these questions in reference to ED leadership. As with the psychological safety domain items, these items were each measured on 5-point Likert scales, and we created domain scores by averaging the three items.
We used three measures as outcome variables: burnout, worsening burnout, and adaptation. Burnout was measured with a validated, nonproprietary single-item burnout scale (Dolan et al., 2015) that was built upon the emotional exhaustion scale of the original Maslach Burnout Inventory (Maslach & Jackson, 1981; Worley et al., 2008). We focus on emotional exhaustion rather than the depersonalization and reduced personal accomplishment aspects of Maslach’s three-part burnout definition because of the primacy of emotional exhaustion in an acute crisis. The scale ranged from 1 = “I enjoy my work. I have no symptoms of burnout” to 5 = “I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help.” To measure worsening burnout during crisis, we asked “Compared to your level of burnout prior to COVID-19, to what extent is your current level of burnout, worse, improved, or the same?” answered on a 5-point scale, where 1 = gotten much better and 5 = gotten much worse. For process adaptation, we used the following statement: “We’ve invented new ways of providing care to adapt to this crisis,” measured with a 5-point Likert agreement scale.
Analyses
We conducted descriptive analyses with the survey data, examining univariate and bivariate statistics for each measure. We conducted confirmatory factor analysis to assess the usage of the items for psychological safety and feeling heard as constructs, and we assessed the relationships between the constructs descriptively. To assess the relationships of psychological safety and feeling heard to one another and to burnout, worsening burnout, and adaptation during crisis, we used generalized structural equation modeling. To estimate the relationship between the two mean-based domain constructs (feeling heard and psychological safety), we used a linear function based on the Gaussian distribution. To estimate the relationships between these constructs and the ordinal 5-point observed outcome measures, we modeled using the ordered logit family link function. To estimate standard errors, we used 10,000 bootstrapped replications.
To assess the potential for common method bias in the survey measures, we performed a Harman test and did not find strong evidence for bias (33.9% common variance). We also conducted sensitivity analyses including various demographic characteristics (gender, race, and ethnicity) and status characteristics (role and tenure), none of which substantively altered the results (available upon request). In addition, we conducted sensitivity analysis allowing correlation between the outcomes, which did not materially alter standard errors or coefficients. Calculating standard errors using the delta method did not meaningfully differ from bootstrapped estimates. Statistical analyses were performed with Stata 15.1.
Results
Table 2 displays descriptive statistics for the variables of interest. The mean for the psychological safety domain was higher than the mean for the feeling heard domain (3.83 vs. 3.15, respectively), although both were less than four, which correlates qualitatively to not agreeing that either was felt. Confirmatory factor analysis supported the psychometric properties of both the psychological safety and feeling heard measures (CFI = .94, TDI = .88, RMSEA = .15, SRMR = .09), although the RMSEA was somewhat elevated. Model fit with the two domains was superior to model fit with one domain, including all items pertaining to psychological safety and feeling heard, with worse fit statistics for the one domain model (CFI = .82, TLI = .70; RMSEA = .24; SRMR = .12). The domain alphas were .72 for psychological safety and .88 for feeling heard. Psychological safety and feeling heard were statistically significantly correlated at r = .54.
Table 2.
Measure descriptives: N, mean, standard deviation, alpha, and correlations
| Measures | N | Mean | SD | α | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|---|---|
| 1. Psychological safety | 240 | 3.83 | 0.79 | 0.72 | 1.00 | |||
| 2. Feeling heard | 239 | 3.15 | 1.01 | 0.88 | .54* | 1.00 | ||
| 3. Burnout | 239 | 2.28 | 0.89 | n/a | −.23* | −.32* | 1.00 | |
| 4. Worsening burnout | 239 | 3.56 | 0.97 | n/a | −.16* | −.15* | .36* | 1.00 |
| 5. Adaptation | 241 | 4.00 | 0.84 | n/a | .34* | .44* | −.16* | −.11 |
Note. SD = standard deviation.
*p < .05.
The mean of the burnout scale was 2.28, which corresponds qualitatively with being between occasionally feeling under stress and definitely burning out; 32.07% reported definitely burning out, experiencing symptoms of burnout that won’t go away, or feeling completely burned out. The mean of the worsening burnout scale was 3.56. Worsening burnout was correlated with overall burnout at r = .36.
Table 3 presents results from generalized structural equation modeling, indicating direct, indirect, and total path coefficients. We found support for H1a, H1b, and H1c: Psychological safety had a statistically significant and negative total effect on burnout (b = −0.55, p < .01, odds ratio [OR] = 0.58) and worsening burnout (b = −0.37, p < .05, OR = 0.69) and a positive significant total effect on process adaptation (b = 0.99, p < .001, OR = 2.68). These coefficients represent log odds. Using ORs, these findings can be interpreted as follows: a one-unit increase in psychological safety is associated with 2.68 times greater odds of reporting more process adaptation.
Table 3.
Generalized structural equation model path coefficients (N = 239)
| Path | Related hypotheses | Path coefficients (unstandardized) | ||
|---|---|---|---|---|
| Direct | Indirect | Total | ||
| Psychological safety ➔ Feeling heard ➔ Burnout | H1a/H4a | −0.17 | −0.38*** | −0.55** |
| Psychological safety ➔ Feeling heard ➔ Worsening burnout | H1b/H4b | −0.26 | −0.11 | −0.37* |
| Psychological safety ➔ Feeling heard ➔ Process adaptation | H1c/H4c | 0.42 | 0.56** | 0.99*** |
| Psychological safety ➔ Feeling heard | H2 | 0.69*** | — | 0.69*** |
| Feeling heard ➔ Burnout | H3a | −0.55*** | — | −0.55*** |
| Feeling heard ➔ Worsening burnout | H3b | −0.16 | — | −0.16 |
| Feeling heard ➔ Process adaptation | H3c | 0.82** | — | 0.82** |
*p < .05. **p < .01. ***p < .001.
As hypothesized (H2), psychological safety had a statistically significant and positive relationship with feeling heard (b = 0.69, p < .001). This linear coefficient can be interpreted as a 1-point increase in psychological safety being associated with a 0.69-point increase in feeling heard.
Analysis indicated support for the hypotheses pertaining to the direct effect of feeling heard on burnout and process adaptation (H3a and H3c, respectively). The coefficient for the relationship between feeling heard and burnout (b = −0.55, p < .001, OR = 0.58) can be interpreted as a 1-unit increase in feeling heard being associated with a 42% reduction in perceived burnout. We did not find support for the hypothesized relationship between feeling heard and less worsening burnout (H3b).
We also found support for H4a and H4c, with statistically significant indirect paths from psychological safety through feeling heard for both burnout and process adaptation. We did not find support for a mediating relationship with feeling heard when using worsening burnout as the outcome (H4b).
Discussion
Our findings point to the importance of conceptualizing, measuring, and assessing psychological safety and feeling heard as distinct constructs. Although psychological safety is widely accepted as an important factor in health care delivery (Rosenbaum, 2019), the phenomenon of feeling heard has received little attention. Our data linking feeling heard to lower burnout and greater process adaptation, even while accounting for psychological safety, suggest that the belief that one will be heard is important for clinicians and staff—worth measuring in research and addressing in practice.
Our findings indicating distinction between psychological safety and feeling heard suggest that, in some work environments, people who feel free to speak up may simultaneously believe their voice will not be recognized or responded to. Furthermore, our regression results suggest that feeling heard has unique importance for both burnout and adaptation. Much has been said about the importance of burnout in health care contexts (Shanafelt et al., 2019), and our findings lend further support to the hypothesized relationship between psychological safety and lower burnout in health care (Rathert et al., 2020; Swendiman et al., 2019). However, our findings also indicate that feeling heard is strongly associated with lower burnout as well, even when accounting for psychological safety. This accords with conservation of resources theory, which conceptualizes how burnout is caused by resource depletion (Hobfoll, 1989; Williams et al., 2019), highlighting how efforts to speak up to mitigate burnout may backfire if the speaker feels unheard—because speaking up uses time and effort, and those resources are likely to be particularly scarce during periods of great uncertainty. Qualitative research has documented that people feel frustrated when their ideas are dismissed or ignored at work (Satterstrom et al., 2021). Because speaking into a void may be discouraging, distressing, and further resource-depleting, feeling heard might be vital for reducing burnout.
However, we also found that psychological safety was a statistically significant predictor of less worsening burnout as the COVID-19 crisis unfolded, whereas feeling heard was not. This finding might relate to the concept of loss spirals in conservation of resources theory. Loss spirals refer to the compounding of resource loss over time as initial losses spur future losses and it becomes increasingly difficult to recover from such losses as they accumulate (Hobfoll & Freedy, 1993). For clinicians and staff experiencing loss spirals as the pandemic wore on, the resource-using act of speaking up with ideas to be heard may have become eclipsed in importance by the first-order problem of feeling psychologically protected, particularly as fear and anxiety rose. For instance, during the time of our data collection, stories were circulating widely of clinicians throughout the United States who were fired for raising concerns about limited personal protective equipment (Scheiber & Rosenthal, 2020). It is possible these troubling examples shifted some individuals’ experience from a status quo of feeling relatively safe to a sudden concern that speaking up would be risky and contentious. Future research to explore both psychological safety and feeling heard and their relationships to uncertainty, especially longitudinally, is well warranted.
It is our hope that this study prompts future efforts to refine the measures and explore their relationships to other variables. Although our new measure of feeling heard was adapted from a validated source and indicated promising measurement properties for early exploration, future efforts to fully develop a robust construct for use in broader research are warranted. In addition, although we measured the individual experience of feeling heard, it is possible that, like psychological safety (Edmondson & Lei, 2014), feeling heard could be operationalized as a team-level climate variable, which would enable exploration of how feeling heard operates at a team or work unit level. Being heard may also be measured from different vantage points—from the employee’s perception of feeling heard to the manager or teammates’ perceptions of hearing them. Research has found that employees and managers can have different impressions of how much an employee speaks up—and that there are negative outcomes when employees overestimate their level of speaking up relative to their managers’ perception (Burris et al., 2013). This suggests that differences in employee and manager perceptions of hearing might be fruitfully explored.
Differences in individuals’ experience of feeling heard by occupational role may also be particularly important for future research. A steep professionally based power gradient has been documented in past research on psychological safety, whereby individuals with less power (e.g., nurses) report lower psychological safety than those with higher power, such as physicians (Nembhard & Edmondson, 2006). A similar pattern may exist for feeling heard, with potentially important implications. For instance, research on global conflict resolution has found that, for lower power group members, feeling heard is associated with positive attitude change, but simply expressing one’s perspective is not—whereas by contrast, for higher power groups, expressing one’s perspective alone is sufficient for attitude change (Bruneau & Saxe, 2012). Such a finding suggests that feeling heard may have uniquely important potential for improving the experience and attitudes of lower power group members, such as nurses, who may often feel unheard.
It is vital that future efforts in research and practice seek to understand how feeling heard is generated. Research on psychological safety has found that leaders are vital to fostering a climate of speaking up through being inclusive (Nembhard & Edmondson, 2006)—and it is likely that leaders have a role to play in generating a feeling of being heard. However, the dimensions of establishing such a feeling may be distinct; for instance, to what extent do voiced ideas have to be responded to with words versus action to establish a feeling of being heard? It is possible that simple interventions may foster feeling heard, even without action. For example, research has shown that “conversational receptiveness”—the use of language to communicate one’s willingness to thoughtfully engage with opposing views—can be reliably fostered by adopting language that expresses receptiveness (Yeomans et al., 2020). However, it is also possible that certain types of ideas come with greater expectations for how they are met; for instance, while raising an issue that is a “nice to have” might be met sufficiently with verbal receptiveness, an issue that is core to someone’s values might carry expectations for action. Qualitative efforts to unpack this phenomenon could support future efforts to intervene for improvement.
Future research can also explore application to other settings and other historical moments. Because of the potentially heightened importance of both psychological safety and feeling heard during times of great uncertainty, we chose to study these factors during the COVID-19 pandemic. Our finding that feeling heard was related strongly to general burnout is suggestive that perhaps these relationships may also unfold under more typical circumstances. Indeed, the uncertainty and fast pace of care in emergency medicine (Faraj & Xiao, 2006) may be sufficient to make feeling heard salient in this context regardless of extenuating crisis circumstances. Indeed, psychological safety has been noted for its relevance in health care well before the pandemic (Eppich, 2015), and feeling heard may have similarly broad application.
This study has the following limitations. First, it is cross-sectional and not causal. Second, generalizability is limited. Although this study represents a diverse array of roles, it draws from two EDs that are part of one broader health system and that may have similar organizational cultures. Moreover, these data were collected during a pandemic. In addition, although we conducted sensitivity analysis to control for role and found our findings to be consistent, our sample size did not support role-specific estimates for each variable. Third, the predictor and outcome measures were drawn from the same survey, with potential for common method bias. To investigate the presence of this bias, we used the Harman test and did not find evidence of strong bias. Moreover, the relative differences across the psychological safety and feeling heard would be notable even in the presence of common method bias, as one would expect any common method bias for both variables to occur in the same direction (i.e., biasing the correlation upward rather than down). Fourth, we rely on self-report for all psychological constructs, which introduces potential for measurement error.
Practice Implications
The concept of psychological safety has made it into the lexicon of many health care leaders today, and the importance of speaking up without fear is increasingly recognized in medicine (Rosenbaum, 2019). This is vital progress, but our findings suggest that there is much more for health care leaders to do. Consider a nurse with 30 years of experience who is unafraid to speak up but who feels it is futile to do so because rejection or avoidance is the likely response. Even a well-intentioned leader familiar with the concept of psychological safety might mistake this nurse’s comfort with speaking for a sign that they are in fact contributing the ideas they have. Our research suggests this would be a costly mistake—and, also, that it may be a common one. Because feeling heard is strongly associated with less burnout and greater adaptation, leaders who help workers feel heard may build a more resilient workforce, such that setbacks can be overcome and periods of great uncertainty weathered.
Ensuring that workers feel heard is challenging, especially because resources are inherently limited and not all good ideas can be put into practice. If it is pursued through simply saying yes to all requests, it will likely be unsustainable—but through practices such as humility in inquiry (Schein, 2013) and transparency in decision-making (Li et al., 2021), leaders may be able to say yes a bit more and to say no better. A first step might be to include feeling heard as a managerial goal that is discussed and checked in on explicitly. For instance, many health care delivery organizations include measures of psychological safety on their annual provider surveys. Measuring feeling heard, reporting back on it, and using the data to spark a discussion about who feels heard—and who does not—might spur additional insight about why and what might be done to improve. Furthermore, incorporating aspects of feeling heard into training and coaching—and modeling the desired behaviors among top leadership—may help shift toward a climate where listening is seen as an expectation of management and where leaders find tactics for listening to be available and encouraged. As uncertainty and stress are likely to remain fixtures of health care delivery, leaders who help people feel heard can offer a vital asset to their organizations and the patients they serve.
Footnotes
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Tuna C. Hayirli, Email: thayirli@hbs.edu.
Aditi Bhanja, Email: abhanja@hsph.harvard.edu.
Nicholas Stark, Email: Nicholas.Stark@ucsf.edu.
James Hardy, Email: James.Hardy@ucsf.edu.
Christopher R. Peabody, Email: Christopher.Peabody@ucsf.edu.
References
- Ahmed F. Zhao F. Faraz N. A., & Qin Y. J. (2021). How inclusive leadership paves way for psychological well-being of employees during trauma and crisis: A three-wave longitudinal mediation study. Journal of Advanced Nursing, 77(2), 819–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C. John O. P., & Keltner D. (2012). The personal sense of power. Journal of Personality, 80(2), 313–344. [DOI] [PubMed] [Google Scholar]
- Bruneau E. G., & Saxe R. (2012). The power of being heard: The benefits of “perspective-giving” in the context of intergroup conflict. Journal of Experimental Social Psychology, 48(4), 855–866. [Google Scholar]
- Burris E. R. Detert J. R., & Romney A. C. (2013). Speaking up vs. being heard: The disagreement around and outcomes of employee voice. Organization Science, 24(1), 22–38. [Google Scholar]
- Diabes M. Ervin J. N. Davis B. S. Rak K. J. Cohen T. R. Weingart L. R., & Kahn J. M. (2020). Psychological safety in intensive care unit rounding teams. Annals of the American Thoracic Society, 18(6), 1027–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan E. D. Mohr D. Lempa M. Joos S. Fihn S. D. Nelson K. M., & Helfrich C. D. (2015). Using a single item to measure burnout in primary care staff: A psychometric evaluation. Journal of General Internal Medicine, 30(5), 582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmondson A. C. (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350–383. [Google Scholar]
- Edmondson A. C. (2003). Speaking up in the operating room: How team leaders promote learning in interdisciplinary action teams. Journal of Management Studies, 40(6), 1419–1452. [Google Scholar]
- Edmondson A. C. Bohmer R. M., & Pisano G. P. (2001). Disrupted routines: Team learning and new technology implementation in hospitals. Administrative Science Quarterly, 46(4), 685–716. [Google Scholar]
- Edmondson A. C. Higgins M. Singer S., & Weiner J. (2016). Understanding psychological safety in health care and education organizations: A comparative perspective. Research in Human Development, 13(1), 65–83. [Google Scholar]
- Edmondson A. C., & Lei Z. (2014). Psychological safety: The history, renaissance, and future of an interpersonal construct. Annual Review of Organizational Psychology and Organizational Behavior, 1(1), 23–43. [Google Scholar]
- Eppich W. (2015). “Speaking up” for patient safety in the pediatric emergency department. Clinical Pediatric Emergency Medicine, 16(2), 83–89. [Google Scholar]
- Faraj S., & Xiao Y. (2006). Coordination in fast-response organizations. Management Science, 52(8), 1155–1169. [Google Scholar]
- Garon M. (2012). Speaking up, being heard: Registered nurses’ perceptions of workplace communication. Journal of Nursing Management, 20, 361–371. [DOI] [PubMed] [Google Scholar]
- Gong Y. Cheung S. Y. Wang M., & Huang J. C. (2012). Unfolding the proactive process for creativity: Integration of the employee proactivity, information exchange, and psychological safety perspectives. Journal of Management, 38(5), 1611–1633. [Google Scholar]
- Gramling R. Stanek S. Ladwig S. Gajary-Coots E. Cimino J. Anderson W. Norton S. A. Aslakson R. A. Ast K. Elk R. Garner K. K. Gramling R. Grudzen C. Kamal A. H. Lamba S. LeBlanc T. W. Rhodes R. L. Roeland E. Schulman-Green D., … Unroe K. T. (2016). Feeling heard and understood: A patient-reported quality measure for the inpatient palliative care setting. Journal of Pain and Symptom Management, 51(2), 150–154. [DOI] [PubMed] [Google Scholar]
- Hayirli T. C. Stark N. Bhanja A. Hardy J. Peabody C. R., & Kerrissey M. J. (2021). Masked and distanced: A qualitative study of how personal protective equipment and distancing affect teamwork in emergency care. International Journal for Quality in Health Care, 33(2), mzab069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschman A. O. (1970). Exit, voice, and loyalty: Responses to decline in firms, organizations, and states. Harvard University Press. [Google Scholar]
- Hobfoll S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44, 513–524. [DOI] [PubMed] [Google Scholar]
- Hobfoll S. E. (2001). The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Applied Psychology, 50(3), 337–421. [Google Scholar]
- Hobfoll S. E., & Freedy J. (1993). Conservation of resources: A general stress theory applied to burnout. In Schaufeli W. B. Maslach C., & Marek T. (Eds.), Professional burnout: Recent developments in research and theory : (pp. 115–129). CRC Press. [Google Scholar]
- Jung O. S. Kundu P. Edmondson A. C. Hegde J. Agazaryan N. Steinberg M., & Raldow A. (2021). Resilience vs. vulnerability: Psychological safety and reporting of near misses with varying proximity to harm in radiation oncology. Joint Commission Journal on Quality and Patient Safety, 47(1), 15–22. [DOI] [PubMed] [Google Scholar]
- Li J.-Y. Sun R. Tao W., & Lee Y. (2021). Employee coping with organizational change in the face of a pandemic: The role of transparent internal communication. Public Relations Review, 47, e101984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C., & Jackson S. E. (1981). The measurement of experienced burnout. Journal of Organizational Behavior, 2(2), 99–113. [Google Scholar]
- Morrison E. W. (2011). Employee voice behavior: Integration and directions for future research. Academy of Management Annals, 5(1), 373–412. [Google Scholar]
- Nembhard I. M., & Edmondson A. C. (2006). Making it safe: The effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. Journal of Organizational Behavior, 27, 941–966. [Google Scholar]
- Nembhard I. M. Yuan C. T. Shabanova V., & Cleary P. D. (2015). The relationship between voice climate and patients’ experience of timely care in primary care clinics. Health Care Management Review, 40(2), 104–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donovan R., & McAuliffe E. (2020). A systematic review of factors that enable psychological safety in healthcare teams. International Journal for Quality in Health Care, 32(4), 240–250. [DOI] [PubMed] [Google Scholar]
- Prapanjaroensin A. Patrician P. A., & Vance D. E. (2017). Conservation of resources theory in nurse burnout and patient safety. Journal of Advanced Nursing, 73(11), 2558–2565. [DOI] [PubMed] [Google Scholar]
- Rathert C. Ishqaidef G., & Porter T. H. (2020). Caring work environments and clinician emotional exhaustion: Empirical test of an exploratory model. Health Care Management Review, 47(1), 58–65. [DOI] [PubMed] [Google Scholar]
- Rathert C. Williams E. S., & Linhart H. (2018). Evidence for the quadruple aim: A systematic review of the literature on physician burnout and patient outcomes. Medical Care, 56(12), 976–984. [DOI] [PubMed] [Google Scholar]
- Rodriguez R. M. Montoy J. Hoth K. F. Talan D. A. Harland K. K. Eyck P. T. Mower W. Krishnadasan A. Santibanez S., & Mohr N., Project COVERED Emergency Department Network (2021). Symptoms of anxiety, burnout, and PTSD and the mitigation effect of serologic testing in emergency department personnel during the COVID-19 pandemic. Annals of Emergency Medicine, 78(1), 35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum L. (2019). Cursed by knowledge—Building a culture of psychological safety. New England Journal of Medicine, 380(8), 786–790. [DOI] [PubMed] [Google Scholar]
- Satterstrom P. Kerrissey M., & DiBenigno J. (2021). The voice cultivation process: How team members can help upward voice live on to implementation. Administrative Science Quarterly, 66(2), 380–425. [Google Scholar]
- Scheiber N., & Rosenthal B. M. (2020, April 9). Nurses and doctors speaking out on safety now risk their job. The New York Times. New York, NY. https://www.nytimes.com/2020/04/09/business/coronavirus-health-workers-speak-out.html. [Google Scholar]
- Schein E. H. (2013). Humble inquiry: The gentle art of asking instead of telling. Berrett-Koehler. [Google Scholar]
- Schein E. H., & Bennis W. G. (1965). Personal and organizational change through group methods. Wiley. [Google Scholar]
- Shanafelt T. D. West C. P. Sinsky C. Trockel M. Tutty M. Satele D. V. Carlasare L. E., & Dyrbye L. N. (2019). Changes in burnout and satisfaction with work-life integration in physicians and the general U.S. working population between 2011 and 2017. Mayo Clinic Proceedings, 94(9), 1681–1694. [DOI] [PubMed] [Google Scholar]
- Sherf E. N. Parke M. R., & Isaakyan S. (2021). Distinguishing voice and silence at work: Unique relationships with perceived impact, psychological safety, and burnout. Academy of Management Journal, 64(1), 114–148. [Google Scholar]
- Siemsen E. Roth A. V. Balasubramanian S., & Anand G. (2009). The influence of psychological safety and confidence in knowledge on employee knowledge sharing. Manufacturing & Service Operations Management, 11(3), 429–447. [Google Scholar]
- Stark N. Kerrissey M. Grade M. Berrean B., & Peabody C. (2020). Streamlining care in crisis: Rapid creation and implementation of a digital support tool for COVID-19. The Western Journal of Emergency Medicine, 21(5), 1095–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendiman R. A. Edmondson A. C., & Mahmoud N. N. (2019). Burnout in surgery viewed through the lens of psychological safety. Annals of Surgery, 269(2), 234–235. [DOI] [PubMed] [Google Scholar]
- Tucker A. L. Nembhard I. M., & Edmondson A. C. (2007). Implementing new practices: An empirical study of organizational learning in hospital intensive care units. Management Science, 53(6), 894–907. [Google Scholar]
- Williams E. S. Rathert C., & Buttigieg S. C. (2019). The personal and professional consequences of physician burnout: A systematic review of the literature. Medical Care Research and Review, 77(5), 371–386. [DOI] [PubMed] [Google Scholar]
- Worley J. A. Vassar M. Wheeler D. L., & Barnes L. L. B. (2008). Factor structure of scores from the Maslach Burnout Inventory: A review and meta-analysis of 45 exploratory and confirmatory factor-analytic studies. Educational and Psychological Measurement, 68(5), 797–823. [Google Scholar]
- Yeomans M. Minson J. Collins H. Chen F., & Gino F. (2020). Conversational receptiveness: Improving engagement with opposing views. Organizational Behavior and Human Decision Processes, 160, 131–148. [Google Scholar]


