Abstract
We compared outcomes at 3 community hospitals before and after switching from in-person to a Tele-ID group from an academic medical center. Compared to in-person, Tele-ID received significantly more consultations with similar outcomes for length of hospital stay, transfers, readmission, and mortality. Tele-ID is a suitable alternative for community settings.
Keywords: community hospital, critical access hospitals, infectious diseases, telehealth, telemedicine
The majority of United States counties have no access to infectious diseases (ID) specialty care [1]. Small community hospitals have traditionally had difficulty attracting and retaining ID specialists. Importantly, ID specialty services have been shown to improve patient outcomes [2–6]. Without specialist care, hospitals have to transfer patients to tertiary facilities to access ID consultants, which could impact care and community hospital revenue.
Telemedicine can expand access to ID specialists [7, 8]. Adoption of standalone or adjunct Tele-ID services has reduced length of stay (LOS), readmissions, and mortality and improved patient satisfaction in both inpatient and outpatient settings [9–19]. However, limited data have been reported on directly comparing inpatient Tele-ID to an in-person ID service in community settings where the lack of access to ID expertise is greatest [20]. To fill this knowledge gap, we report our analyses comparing Tele-ID services at community hospitals with prior in-person ID care.
METHODS
University of Pittsburgh Medical Center (UPMC) is a large healthcare organization based in Pittsburgh, Pennsylvania. The system has 40 hospitals across Pennsylvania, Maryland, and New York. Three UPMC hospitals were included in the current study: Hospital 1 is the largest with 216 licensed beds, followed by hospitals 2 and 3 with 122 and 106 licensed beds, respectively. All 3 hospitals are in northwestern Pennsylvania with county populations ranging from 6000 to 300 000. The cumulative driving time between all 3 hospitals is 1 hour and 40 minutes.
We performed a retrospective medical record review comparing outcomes of patients evaluated by in-person versus Tele-ID care. The in-person group consisted of all patients seen by the local physician between 1 January 2018 and 30 June 2018. The Tele-ID group consisted of all patients seen by a UPMC Tele-ID physician between 1 July 2018 and 30 December 2018. Data were extracted from the electronic medical record (EMR) for each population including sex, race, age, body mass index, and Charlson Comorbidity Index at the time of consultation. Key study outcomes included the total number of unique patient encounters, the total hospital LOS and LOS after ID consult, discharge to home, transfers to tertiary centers, ID-related hospital readmission, and mortality. Postdischarge mortality was captured through the health system’s access to the Social Security database. Specific ID diagnoses for each unique patient encounter were tabulated. All statistical significance analyses were performed with the Mann-Whitney U test using Microsoft Excel and R software. The study did not require institutional review board approval as it was approved by the UPMC quality improvement committee (Project ID 2046: Assessing the Quality and Outcomes of the Infectious Diseases Services Provided via telemedicine within the UPMC Healthcare System).
RESULTS
Description of ID Consultation Structure
Before July 2018, all 3 hospitals were serviced by a single, independent, full-time ID physician who traveled daily between the sites. Following the departure of this physician on 30 June 2018, the 3 hospitals implemented Tele-ID consultations through the Division of Infectious Diseases of UPMC. Given the distance, location, and prior implementation of Tele-ID at other UPMC hospitals [21], a fully remote Tele-ID service was executed on 1 July 2018. One full-time equivalent Tele-ID physician, from a pool of 8 rotating ID physicians, was assigned to cover the 3 hospitals. The Tele-ID physician placed notes and orders in the local EMR. The Tele-ID physician provided live audio-video visits, electronic consults (e-consults), and telephonic physician-to-physician consults. Live initial and follow-up consultations were conducted with the assistance of a tele-presenter registered nurse (RN) at each site during weekdays. The RN was trained on Health Insurance Portability and Accountability Act–compliant telecommunications equipment and on conducting a comprehensive physical examination including the utilization of a high-definition portable camera and a Bluetooth-enabled stethoscope to allow auscultation. Hospital 1 had a dedicated RN to assist all telemedicine services (ID, endocrinology, pulmonary, and neurology), while hospitals 2 and 3 had an RN assigned for Tele-ID up to 2 hours per day. E-consults constituted reviewing the EMR, occasional discussion with the in-hospital primary care team, and providing a detailed consultation note. Telephonic physician-to-physician consultations were available 24/7, but live visits and e-consults were only completed during the weekdays. The Tele-ID physician decided on a case-by-case basis whether to evaluate the patient using a live visit or an e-consult. Postdischarge, the in-person group was followed by the local ID physician at an independent clinic. For the Tele-ID group, patients discharged on intravenous antibiotics were followed by a central outpatient parenteral antibiotic team. They were seen by the same pool of ID physicians either in-person in Pittsburgh or at a satellite clinic utilizing live audio-video software with a tele-presenter.
Outcomes
A total of 642 unique patient encounters occurred across the in-person and Tele-ID groups during the study period (Table 1). Data from hospitals 2 and 3 were combined as both shared a common EMR. In the Tele-ID group, most consults were live, except for 8 initial e-consults and 34 unique encounters with at least 1 follow-up e-consult. Patients were predominantly White (89.3%) with a slight female majority (54.2%). The average age of the population was 67.0 years and the average body mass index was 32.4 kg/m2. The average Charlson Comorbidity Index was 5.9 in the in-person group and 6.4 in the Tele-ID group.
Table 1.
Characteristics and Outcomes of the Study Population
| Characteristic or Outcome | Hospital 1 | Hospitals 2 and 3 | Overall | ||
|---|---|---|---|---|---|
| In-Person ID | Tele-ID | In-Person ID | Tele-ID | ||
| Patient characteristics | |||||
| No. of encounters | 147 | 239 | 104 | 152 | 642 |
| No. of initial E-consults | 0 | 8 | 0 | 0 | 8 |
| White race | 126 (85.7) | 205 (85.8) | 97 (93.2) | 145 (95.4) | 573 (89.3) |
| Female sex | 74 (50.3) | 141 (59.0) | 54 (51.9) | 79 (51.9) | 348 (54.2) |
| Average age, y | 67.4 | 66.7 | 66.5 | 67.3 | 67.0 |
| Average BMI, kg/m2 | 31.5 | 30.9 | 32.6 | 34.7 | 32.4 |
| Average CCI | 5.4 | 5.8 | 6.4 | 7.0 | 6.2 |
| Patient outcomes (in-person vs Tele-ID) | |||||
| Encounters | 147 | 239 | 104 | 152 | P = .018 |
| LOS after ID consult, d | 4.6 | 4.4 | 3.6 | 3.5 | P = .945 |
| Total hospital LOS, d | 7.8 | 7.5 | 6.5 | 6.4 | P = .654 |
| ID-related readmissions at 30 d | 12 (8.2) | 7 (2.9) | 4 (3.8) | 3 (2.0) | P = .072 |
| Transfer to tertiary center | 17 (11.6) | 23 (9.6) | 16 (15.4) | 17 (11.2) | P = .301 |
| Discharge to homea | 63 (42.9) | 121 (50.6) | 64 (61.5) | 95 (62.5) | P = .333 |
| Death within 30 d of discharge | 5 (3.4) | 9 (3.8) | 3 (2.9) | 5 (3.3) | P = .979 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: BMI, body mass index; CCI, Charlson Comorbidity Index; ID, infectious diseases; LOS, length of stay.
There were 80 discharges to skilled nursing facilities for the in-person group (60 at hospital 1; 20 at hospitals 2 and 3) and 119 for the Tele-ID group (85 at hospital 1; 34 at hospitals 2 and 3). There were 9 discharges to hospice for the in-person group (6 at hospital 1; 3 at hospitals 2 and 3) and 7 for the Tele-ID group (3 at hospital 1; 4 at hospitals 2 and 3).
The total number of encounters seen by the Tele-ID group was significantly greater than the in-person group (251 vs 391; P = .018; Table 1). The average LOS following the initial ID consult was 4.1 days for in-person (4.6 days at hospital 1; 3.6 days at hospital 2 and 3) and 3.9 days for Tele-ID (4.4 days for hospital 1; 3.5 days for hospital 2 and 3) (P = .945). The average total hospital LOS was 7.2 days for in-person (7.8 days at hospital 1; 6.5 days at hospital 2 and 3) and 7.0 days for Tele-ID (7.5 days for hospital 1; 6.4 days at hospitals 2 and 3) (P = .654). There were 16 ID-related readmissions at 30 days for in-person (12 at hospital 1; 4 at hospitals 2 and 3) and 10 for Tele-ID (7 at hospital 1; 3 at hospitals 2 and 3) (P = .072). There were 33 transfers to tertiary centers for in-person (17 at hospital 1; 16 at hospitals 2 and 3) and 40 for Tele-ID (23 at hospital 1; 17 at hospitals 2 and 3) (P = .301). The in-person group had 12 ID-related transfers and Tele-ID had 5. Reasons for ID transfers included need for surgical specialty evaluation or a diagnostic modality unavailable at the originating hospital. There were 127 discharges to home for the in-person group (63 at hospital 1; 64 at hospitals 2 and 3) and 216 for the Tele-ID group (121 at hospital 1; 95 at hospitals 2 and 3) (P = .333). There was a total of 8 deaths within 30 days of discharge in the in-person group and 14 deaths in the Tele-ID group (P = .979).
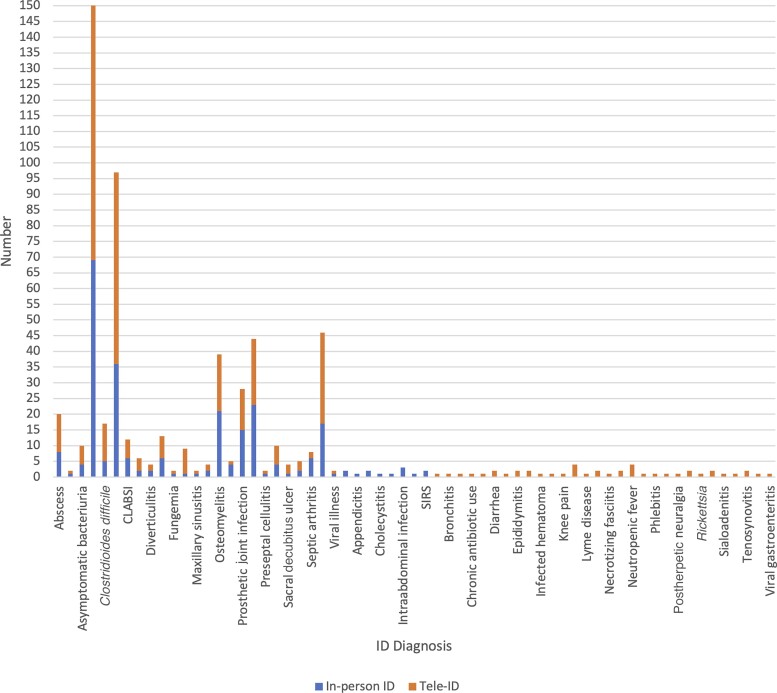
The most common ID diagnosis in both groups was bacteremia. A wider range of ID diagnoses were made in the Tele-ID group (Figure 1). Antimicrobial usage at all 3 sites for all hospital encounters was 984 days of therapy per 1000 patient-days (DOT/1000 PD) during the in-person ID period and 938 DOT/1000 PD during the Tele-ID period, which was a 4.7% decrease (P = .12).
Figure 1.
Wider variety of infectious diseases (ID) diagnoses by Tele-ID service. Abbreviations: CLABSI, central line–associated bloodstream infection; ID, infectious diseases; SIRS, systemic inflammatory response syndrome.
DISCUSSION
This is the first study comparing inpatient outcomes between in-person ID versus Tele-ID at the same hospitals. This comparison shows that outcomes are similar between the 2 groups, despite a significantly greater number of consults performed by Tele-ID. As a result of the higher number of encounters, Tele-ID saw more medically complex patients with more diverse ID diagnoses.
The greater number of consults seen by Tele-ID suggests improved productivity compared with in-person care, possibly because of travel time elimination. Although not statistically significant, the Tele-ID group showed a trend toward shorter LOS, less frequent ID-related readmissions at 30 days and transfers to tertiary centers, more frequent discharges to home, and low mortality within 30 days of discharge. The less frequent transfers allowed patients to remain in care in their local community and for hospitals to receive full reimbursement for the hospitalization. Two concerns about Tele-ID include possible missed diagnosis and increased antibiotic usage compared to in-person care. The data from this study suggest the opposite: Tele-ID physicians were able to make a broader range of ID diagnoses and there was no increase in antimicrobial usage.
There are limitations to this study. The sample size in both groups is limited because of the small size of the community hospitals and the low overall volume of patients needing ID consultation. Larger studies comparing in-person to Tele-ID care will be needed. There is also the possibility of a temporal bias because the calendar dates of the study groups differ, although there was no time gap between the transition from in-person to Tele-ID care.
In conclusion, although there can be technical, physical, and financial challenges in implementing telemedicine services, the results of this initial study suggest that Tele-ID can be an effective alternative to in-person ID consultation in areas where in-person ID expertise is not available.
Contributor Information
Nupur Gupta, Division of Infectious Diseases, Department of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA.
J Ryan Bariola, Division of Infectious Diseases, Department of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA.
John W Mellors, Division of Infectious Diseases, Department of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA.
Rima C Abdel-Massih, Division of Infectious Diseases, Department of Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA; Infectious Disease Connect, Inc, Pittsburgh, Pennsylvania, USA.
Notes
Author contributions. All authors contributed equally to this work.
Acknowledgments. The authors thank Keith Oelkers and Shannon Overly for their assistance with statistical analysis.
Patient consent. Patient written consent was not obtained as it was deemed not applicable. The design of the work was approved by the UPMC quality improvement committee (Project ID 2046).
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Walensky RP, McQuillen DP, Shahbazi S, Goodson JD. Where is the ID in COVID-19? Ann Intern Med 2020; 173:587–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Butt AA, Al Kaabi N, Saifuddin M, et al. . Impact of infectious diseases team consultation on antimicrobial use, length of stay and mortality. Am J Med Sci 2015; 350:191–4. [DOI] [PubMed] [Google Scholar]
- 3. Schmitt S, MacIntyre AT, Bleasdale SC, et al. . Early infectious diseases specialty intervention is associated with shorter hospital stays and lower readmission rates: a retrospective cohort study. Clin Infect Dis 2019; 68:239–46. [DOI] [PubMed] [Google Scholar]
- 4. McQuillen DP, MacIntyre AT. The value that infectious diseases physicians bring to the healthcare system. J Infect Dis 2017; 216(Suppl 5):S588–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schmitt S, McQuillen DP, Nahass R, et al. . Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis 2014; 58:22–8. [DOI] [PubMed] [Google Scholar]
- 6. Hamandi B, Husain S, Humar A, Papadimitropoulos EA. Impact of infectious disease consultation on the clinical and economic outcomes of solid organ transplant recipients admitted for infectious complications. Clin Infect Dis 2014; 59:1074–82. [DOI] [PubMed] [Google Scholar]
- 7. Abdel-Massih RC, Mellors JW. Telemedicine and infectious diseases practice: a leap forward or a step back? Open Forum Infect Dis 2019; 6:ofz196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Young JD, Abdel-Massih RC, Herchline T, et al. . Infectious Diseases Society of America position statement on telehealth and telemedicine as applied to the practice of infectious diseases. Clin Infect Dis 2019; 68:1437–43. [DOI] [PubMed] [Google Scholar]
- 9. Burnham JP, Fritz SA, Yaeger LH, Colditz GA. Telemedicine infectious diseases consultations and clinical outcomes: a systematic review. Open Forum Infect Dis 2019; 6:ofz517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Monkowski D, Rhodes LV, Templer S, et al. . A retrospective cohort study to assess the impact of an inpatient infectious disease telemedicine consultation service on hospital and patient outcomes. Clin Infect Dis 2020; 70:763–70. [DOI] [PubMed] [Google Scholar]
- 11. Parmar P, Mackie D, Varghese S, Cooper S. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis 2014; 60:1084–94. [DOI] [PubMed] [Google Scholar]
- 12. Tande AJ, Berbari EF, Ramar P, et al. . Association of a remotely offered infectious diseases eConsult service with improved clinical outcomes. Open Forum Infect Dis 2020; 7:ofaa003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Strymish J, Gupte G, Afable MK, et al. . Electronic consultations (e-consults): advancing infectious disease care in a large Veterans Affairs healthcare system. Clin Infect Dis 2017; 64:1123–5. [DOI] [PubMed] [Google Scholar]
- 14. Young JD, Patel M, Badowski M, et al. . Improved virologic suppression with HIV subspecialty care in a large prison system using telemedicine: an observational study with historical controls. Clin Infect Dis 2014; 59:123–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. León A, Cáceres C, Fernández E, et al. . A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: a randomized study. PLoS One 2011; 6:e14515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mashru J, Kirlew M, Saginur R, Schreiber YS. Management of infectious diseases in remote northwestern Ontario with telemedicine videoconference consultations. J Telemed Telecare 2017; 23:83–7. [DOI] [PubMed] [Google Scholar]
- 17. Sheridan KR, Abdel-Massih RC, Gupta N, Mellors JW. Tele-OPAT outcomes at two community hospitals [abstract 627]. In: IDWeek, Virtual, 21–25 October 2020. [Google Scholar]
- 18. Evers EC, Fritz SA, Colditz GA, Burnham JP. Perceptions of telemedicine and costs incurred by a visit to a general infectious diseases clinic: a survey. Open Forum Infect Dis 2022; 9:ofab661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open 2021; 4:e2136405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Younus F, Girio-Herrera L, Barrueto F, Ahmed Z, Zimand P. Tele-infectious disease consultation produces equivalent outcomes as in-person consultation [abstract 1638]. In: IDWeek, San Francisco, CA, 3–7 October 2018.
- 21. Gupta N, Sanghvi AB, Mellors JW, Abdel-Massih R. Six-year longitudinal analysis of an inpatient infectious diseases telemedicine service at a community hospital [abstract 124]. In: IDWeek, Virtual, 21–25 October 2020.