Abstract
Genital warts are caused by several strains of Human Papilloma Viruses. Although asymptomatic in most cases, they can be psychologically and physically distressing for patients. Recently, intralesional immunotherapy using different antigens—such as Bacille Calmette–Guerin vaccine, candida antigen and measles, mumps, and rubella (MMR) vaccine—have shown promising efficacy in the treatment of genital warts. We report two cases in Omani males who presented to the Dermatology Department at Barka Polyclinic with recalcitrant genital warts that resolved completely with intralesional injection of the MMR vaccine.
Keywords: Genital Warts, Immunotherapy, Measles-Mumps-Rubella Vaccine, Venereal Warts, Oman
Genital warts, also known as anogenital warts and condylomata acuminata, are fleshy growths affecting the genital and anal area and are caused by the human papilloma viruses (HPVs). More than 200 HPV subtypes have been identified, with HPV subtypes 6 and 11 being considered low risk, while subtypes HPV 16 and 18 are considered high risk as they are associated with cervical dysplasia.1 Genital warts are transmitted through sexual contact; however, vertical transmission and autoinoculation have also been reported.2,3
The treatments for genital warts focus on removing the warty growths, rather than eradicating the virus. Many treatment modalities are available, including topical agents (e.g. imiquimod ointment), destructive methods (e.g. cryotherapy or lasers) and immunomodulators (e.g. interferons). Recently, immunotherapy with intralesional agents such as the measles, mumps and rubella (MMR) vaccine, purified protein derivative (PPD) and the Bacillus Calmette-Guérin (BCG) vaccine have been shown to be efficient with good tolerability in the treatment of warts, especially refractory ones.4 We report two cases of recalcitrant genital warts that were treated successfully with intralesional immunotherapy using the MMR vaccine, along with a literature review for the use of this treatment method on genital warts.
Case One
A 23-year-old male patient presented to the Dermatology Department at Barka Polyclinic in 2020 with multiple papules over the groin area lasting for more than two months. He noted that the lesions were increasing in size.
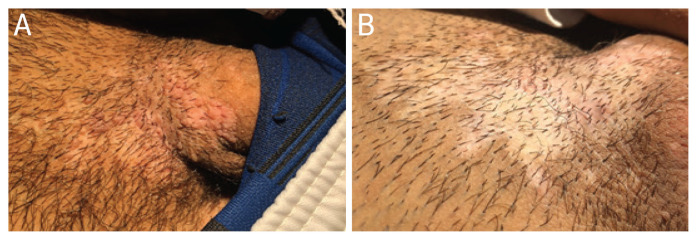
Upon examination, there were multiple skin-colored flat and verrucous papules coalescing into plaques over the pubic area and shaft of the penis [Figure 1A]. The Koebner phenomenon was also observed, since some of the lesions appeared in a linear fashion due to hair removal with a razor. Laboratory investigations were negative for human immunodeficiency virus (HIV), venereal disease research laboratory (VDRL) test, treponema pallidum hemagglutination (TPHA), hepatitis C and hepatitis B surface antigen. The patient was diagnosed with genital warts based on the typical clinical presentation.
Figure 1.
A: A 23-year-old male patient with genital warts before treatment with an intralesional measles, mumps and rubella injection. B: Affected area after the fourth session of immunotherapy showing complete regression with post-inflammatory hypopigmentation.
A plan of treatment was discussed with the patient and he agreed to try cryotherapy at two-week intervals with KOH 5% solution application at home twice daily. After six sessions, there was no significant improvement and so the patient was offered ablative radiofrequency. Two sessions were performed one month apart; however, there was a recurrence after a few weeks. Finally, an intralesional MMR injection was offered considering prior vaccination with MMR as per the national programme. The two biggest warts were chosen to be injected with 0.3 mL of MMR solution (M-M-R® II 0.5 mL vial, Merck Sharp & Dohme Corp., New Jersey, USA), once every two weeks with no other modalities of treatment. A total of four sessions were required to achieve complete resolution of the warts without any reported side effects [Figure 1B]. To enhance the efficacy, the patient was given two sessions of cryotherapy after the third session of intralesional MRR injection. There was no recurrence on follow-up after three and six months.
Case Two
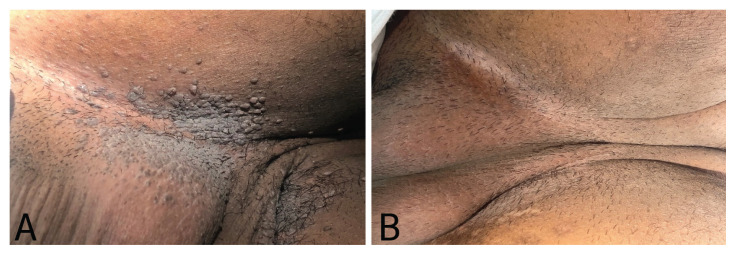
A 25-year-old male patient presented to the Dermatology Department at Barka Polyclinic in 2020 with extensive anogenital warts for more than 18 months [Figure 2A]. He was seen in different skin clinics and had received multiple treatments, including topical imiquimod cream 5%, cryotherapy sessions, electrocautery and radiofrequency treatments with no successful results as the warts were reoccurring.
Figure 2.
A: A 25-year-old male patient with extensive genital warts. B: Complete resolution after seven sessions of intralesional measles, mumps and rubella injection.
The patient was counselled on potential treatment using immunotherapy via MMR injections as he was already vaccinated with the same as per the national programme and he agreed to proceed with the immunotherapy. Prior to the injection, he was tested for HIV, HBsAg, hepatitis C virus, antinuclear antibodies test, TPHA and VDRL, which were all negative. The patient was given a total of seven sessions of MMR injections (Merck Sharp & Dohme Corp.), two weeks apart, with four sites injected in each session and 0.3 mL of MMR per site. In addition, the patient started cryotherapy after the third session of MMR injections, once every two weeks, receiving a total of five sessions. The patient had significant improvement after completing the course of treatment with no reported side effects [Figure 2B]. There was no recurrence on follow-up at eight weeks and most of the inflammation marks were resolved.
The authors have obtained patient consent prior to publication. The patients have given their consent for the use of their images and other clinical information for publication purposes.
Discussion
Several treatments for genital warts are available, including medical agents (e.g. imiquimod cream and podophyllotoxin), destructive methods (e.g. cryotherapy, electrocautery and lasers) or surgical excision. These options are limited by a high rate of recurrence and side effects, such as pain and scarring.5 Immunotherapy is becoming more popular for the treatment of warts, especially for genital and refractory warts.4 Commonly used agents include the MMR vaccine, PPD, the BCG vaccine and the Candida antigen. Among these, the MMR vaccine and PPD have been shown to be the most effective in achieving complete primary and long-term recovery, reducing the recurrence rate at the same site compared with cryotherapy and other immunotherapeutic modalities.6 Additionally, combining intralesional immunotherapy with a destructive method may enhance the efficacy and reduce treatment duration.6 There are no clear guidelines on when to use immunotherapy; however, it is generally used on extensive, recurrent and refractory warts in difficult to treat areas, such as the periungual area.4
The exact mechanism of intralesional immunotherapy is not entirely understood. A postulated mode of action includes the release of different immunoregulatory cytokines such as interleukins 2 and 12 and interferon-c that stimulate a strong immune response against HPV.7 Furthermore, antigen injection is associated with proliferation of peripheral blood mononuclear cells that promotes T-helper 1 cytokine responses to eradicate HPV-infected cells.8 It is used to treat genital warts at a dose of 0.3 to 0.5 mL injected into the biggest wart at three week intervals.
To date, there are no randomised clinical trials evaluating the efficacy of intralesional MMR vaccines in the treatment of genital warts nor clear guidelines as to when to use them. A review of the literature showed a dearth of research evaluating the use of MMR vaccines to treat genital warts [Table 1]. In an open-label study, Sharma et al. evaluated the use of the MMR vaccine on 35 patients using a 0.5 mL dose given at three week intervals.9 The treatment response rate was nearly 98% after a period of nine weeks. Meena et al. reported two cases of genital warts that had an excellent response to a 0.5 mL intralesional injection of the MMR vaccine at a similar interval.10 Side effects were minimal and temporary, however, with flu-like symptoms being the most common side effect reported from studies of intralesional MMR vaccines to treat extra-genital warts.11 In the current cases, a slightly higher dose (0.6 mL and 1.2 mL, respectively) of the MMR vaccine was used, as the patients had extensive bilateral warts. A combination with a destructive method (i.e. cryotherapy) was also utilised to enhance the resolution of stubborn lesions.
Table 1.
Summary of published literature on the use of intralesional measles, mumps and rubella for genital warts
| Study type | No. of patients | Dose and number of MMR sessions | Combination treatment used | Results | Side effects | |
|---|---|---|---|---|---|---|
| Meena et al.9 | Case report | 2 | 0.5 mL into biggest wart every three weeks | - | Complete response for the 1st patient after two sessions, 2nd patient had almost complete response after a single session | Pain during procedure |
| Sharma et al.8 | Open label study | 35 | 0.5 mL into biggest wart every three weeks for a maximum of three injections | - | 98% improvement at nine weeks | Swelling following injection (18.2%) |
| Present cases | Case report | 2 | Case one: Total of 0.6 mL of MMR every two weeks Case two: total of 1.2 mL of MMR every two weeks |
Cryotherapy | Complete resolution after four and seven sessions for patients one and two, respectively | - |
MMR = measles, mumps and rubella.
Intralesional MMR vaccine is currently not routinely used for genital warts. The present cases along with the previously reported cases draw attention to the need for further randomised clinical trials to establish the potential role of MMR vaccine immunotherapy in the management of anogenital warts. Compared with current modalities of treatments, the MMR vaccine offers low recurrence, less side effects and an easy-to-use therapeutic method.
Conclusion
Intralesional immunotherapy with the MMR vaccine seems to be a safe and effective treatment modality for recalcitrant genital warts and can save the patients and doctors a long treatment time, noted using other methods. Further large sample studies are needed to establish this modality of treatment for genital warts.
ACKNOWLEDGEMENT
The authors would like to thank the patients for giving consent to publish the cases.
Footnotes
AUTHORS’ CONTRIBUTIONS
AQ and FF were involved in the literature review process. AQ drafted the manuscript. FF contributed with the evaluation of the cases. Both authors approved the final version of the manuscript.
References
- 1.Tyring SK. Human papillomavirus infections: Epidemiology, pathogenesis, and host immune response. J Am Acad Dermatol. 2000;43:S18–26. doi: 10.1067/mjd.2000.107807. [DOI] [PubMed] [Google Scholar]
- 2.Mayeaux EJ, Jr, Dunton C. Modern management of external genital warts. J Low Genit Tract Dis. 2008;12:185–92. doi: 10.1097/LGT.0b013e31815dd4b4. [DOI] [PubMed] [Google Scholar]
- 3.Hernandez BY, Shvetsov YB, Goodman MT, Wilkens L, Thompson P, Zhu X, et al. Genital and extra-genital warts increase the risk of asymptomatic genital human papillomavirus infection in men. Sex Transm Infect. 2011;87:391–5. doi: 10.1136/sti.2010.048876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thappa DM, Chiramel MJ. Evolving role of immunotherapy in the treatment of refractory warts. Indian Dermatol Online J. 2016;7:364–70. doi: 10.4103/2229-5178.190487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bacelieri R, Johnson SM. Cutaneous warts: an evidence-based approach to therapy. Am Fam Physician. 2005;72:647–52. [PubMed] [Google Scholar]
- 6.Salman S, Ahmed MS, Ibrahim AM, Mattar OM, El-Shirbiny H, Sarsik S, et al. Intralesional immunotherapy for the treatment of warts: A network meta-analysis. J Am Acad Dermatol. 2019;80:922–30e4. doi: 10.1016/j.jaad.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 7.King M, Johnson SM, Horn TD. Intralesional immunotherapy for genital warts. Arch Dermatol. 2005;141:1606–7. doi: 10.1001/archderm.141.12.1606. [DOI] [PubMed] [Google Scholar]
- 8.Horn TD, Johnson SM, Helm RM, Roberson PK. Intralesional immunotherapy of warts with mumps, Candida, and Trichophyton skin test antigens: A single-blinded, randomized, and controlled trial. Arch Dermatol. 2005;141:589–94. doi: 10.1001/archderm.141.5.589. [DOI] [PubMed] [Google Scholar]
- 9.Sharma S, Agarwal S. Intralesional Immunotherapy with Measles Mumps Rubella Vaccine for the Treatment of Anogenital Warts: An Open-label Study. J Clin Aesthet Dermatol. 2020;13:40–4. [PMC free article] [PubMed] [Google Scholar]
- 10.Meena D, Sharma S, Chauhan P. Measles, mumps, and rubella vaccine in genital warts: A case report of two patients. Indian J Sex Transm Dis AIDS. 2018;39:133–5. doi: 10.4103/ijstd.IJSTD_44_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nofal A, Nofal E, Yosef A, Nofal H. Treatment of recalcitrant warts with intralesional measles, mumps, and rubella vaccine: a promising approach. Int J Dermatol. 2015;54:667–71. doi: 10.1111/ijd.12480. [DOI] [PubMed] [Google Scholar]