Abstract
Psychological research consistently demonstrates that affect can play an important role in decision-making across a broad range of contexts. Despite this, the role of affect in clinical reasoning and medical decision-making has received relatively little attention. Integrating the affect, social cognition, and patient safety literatures can provide new insights that promise to advance our understanding of clinical reasoning and lay the foundation for novel interventions to reduce diagnostic errors and improve patient safety. In this paper, we briefly review the ways in which psychologists differentiate various types of affect. We then consider existing research examining the influence of both positive and negative affect on clinical reasoning and diagnosis. Finally, we introduce an empirically supported theoretical framework from social psychology that explains the cognitive processes by which these effects emerge and demonstrates that cognitive interventions can alter these processes. Such interventions, if adapted to a medical context, hold great promise for reducing errors that emerge from faulty thinking when healthcare providers experience different affective responses.
Keywords: affect, affective biases, clinical reasoning, information processing
Introduction
Diagnostic error is a serious public health concern. It is estimated that every person in the United States is likely to experience at least one diagnostic error in their lifetime – some with devastating and debilitating consequences [1]. Given the prevalence and severity of diagnostic error, there is a critical need for effective interventions that reduce its frequency [1]. To develop such interventions, it is essential that we understand the causes that can underlie diagnostic error.
In investigating these causes, some researchers have drawn from the psychological literature. Patient safety experts have theorized that diagnostic errors often result from differences in how physicians think, which has led them to apply a dual process model of reasoning [1, 2]. This conceptualization maintains that people process information using two parallel, interactive systems: a fast, heuristic system 1 and a slow, deliberative system 2 [3], [4], [5], [6]. System 1 is driven by pattern recognition and relies on the use of mental shortcuts; system 2 is driven by rational processes and relies on the use of reason and logic [3, 4, 7, 8].
Given that many diagnostic errors appear to be due to cognitive failures rather than lack of knowledge, dual process models posit that diagnostic errors result from overreliance on system 1 and under reliance on system 2 processing [2, 9]. In this sense, diagnostic errors are fundamentally a problem of thinking [10, 11]. Some scholars have argued that these thinking problems can be addressed by identifying the specific cognitive heuristics that lead providers to make diagnostic errors, and then devising effective strategies to counter or “debias” the effects of these heuristics [2, 9].
While considerable progress has since been made in understanding the cognitive roots of diagnostic errors [10, 12], this approach often leaves out a key factor known to influence a broad array of judgments and decisions: affect [12], [13], [14], [15]. Decades of research in social psychology and cognitive neuroscience have converged on the conclusion that decisions and judgments are derived from the interplay between thinking and feeling [16, 17], and that affective feelings are generally adaptive as they assists in complex decision-making processes [17, 18]. In fact, damage to the amygdala – one brain region implicated in affective processing – often leaves patients incapable of making decisions [13, 19]. Though this well-established body of research shows that affect influences reasoning [20, 21], relatively little is known about the influence of affect on clinical reasoning specifically [10, 12, 14, 15, 22].
It is reasonable to assume that affect influences clinical reasoning, as patients themselves can elicit emotions among providers throughout the medical care and treatment process. Over four decades ago, Groves [23] wrote about taking care of “hateful patients” – those who are considered “difficult” and evoke significant negative reactions among physicians. He urged physicians not to avoid such patients, but to try to better understand and manage them. A decade later, Smith and Zimney [24] used a survey to assess the degree of emotion that highly experienced internists felt in a variety of situations with patients. The situations that elicited the strongest emotional reactions involved disrespectful and critical patients, those who express anger toward the physician, those who attempt to control the interaction, and those who want tests or drugs (especially narcotics) that the physician thinks are unnecessary.
More recently, Croskerry et al. [10, 12] brought attention to the issue of physicians’ feelings, insisting that healthcare providers are not immune to emotional influences and therefore must work to avoid being biased by their emotional experiences. It is important to note, however, that feelings themselves are not inherently “bad.” In fact, most models of affect in psychology recognize that affect is quite adaptive in everyday life and typically leads to the right decisions and conclusions. Physicians, for example, frequently rely on subtle feelings when assessing patients, and these often lead to diagnostic success [25]. But when physicians over rely on their intuition or feelings in contexts that call for a more analytical and systematic approach, biases and misdiagnoses can result [8, 12].
In this paper, we first resolve some of the confusion regarding what affect is and then present commonly accepted views within the social cognitive and affective sciences. We briefly review the way in which psychologists identify different types of affect, after which we consider extant research examining the influence of affect and affective contexts on patient safety, diagnosis, and clinical reasoning. Finally, we introduce an empirically supported theoretical framework from social psychology that not only explains the cognitive processes by which these effects emerge, but also demonstrates that cognitive interventions can alter these processes. Such interventions, if adapted to a medical context, hold great promise for reducing errors that emerge from faulty thinking when healthcare providers experience different affective responses.
The nature and function of affect
Although affective experiences are highly ubiquitous in our everyday lives, research investigating both the nature of these experiences and their function is remarkably complex. Indeed, even the ways in which types of affect are differentiated reflect this complexity, and the failure to specify what one means by “affect” may contribute to confusion around what affect is and what affect does both in the healthcare domain and more generally. As we will discuss, this has implications for our understanding of how affect is likely to influence reasoning and decision-making.
Affect is a general, umbrella term that refers to how much things are valued. In other words, affect is about the “goodness” or “badness” of things or people as they are related to us [20, 21, 26, 27]. For example, an elderly patient may trigger positive affect in a physician if the patient reminds the physician of her grandmother, but this same patient may trigger negative affect in another physician if the patient reminds her of someone who has done harm to her. Both types of affect are adaptive responses to one’s environment and thus, neither is inherently good or bad; it depends on the context in which the affect is experienced.
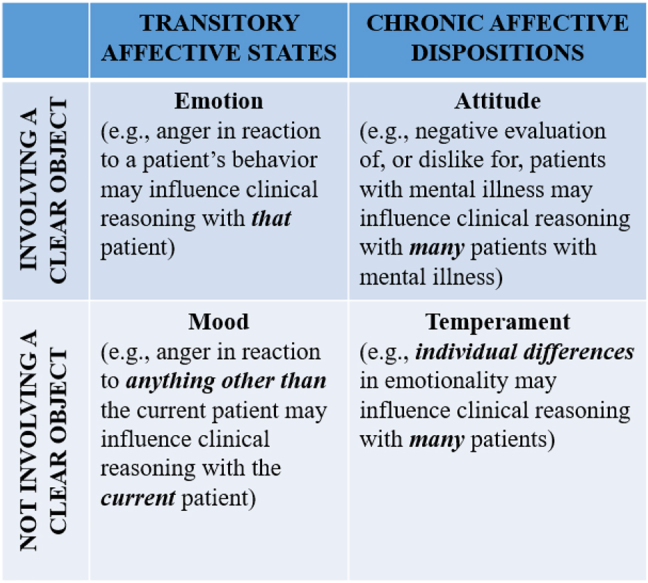
As a general umbrella term, affect subsumes a broad range of affective experiences, which can be divided into temperament, attitude, emotion, and mood [20, 28] (see Table 1). They can be distinguished by whether they are long-term dispositions vs. short-term states and by whether they involve a clear object [20]. For example, temperament and attitude are long-term, affective dispositions that are relatively diffuse. As such, temperament and attitudes can have broad impacts on patients and/or clinical reasoning. Emotions and moods, on the other hand, are affective states; they are transitory reactions to specific individuals or situations (i.e., “objects”). Attitudes and emotions arise in response to a clear, specific object (e.g., a patient); temperaments and moods are diffuse affective conditions that do not involve clear objects [20, 28]. Table 1 depicts these similarities and differences, along with the implications that each type of affect can have for patients. Not recognizing the different types of affect could potentially impede progress in this field by casting too large a net on “affective influences” when the different types of affect could be better studied with different methods and may call for different interventions.
Table 1:
Different types of affective experiences.
Affect functions to convey information about our evaluations of experiences [21, 26, 29, 30]. In turn, affect influences what we think, or our evaluations and judgments of an object or person. For example, if a physician experiences positive affect toward elderly people in general (i.e., a positive attitude), then when he meets an elderly patient, he will cast the patient in a more positive and favorable light, and perhaps pay more attention to their clinical presentation. Conversely, if the same physician holds a negative attitude toward elderly people, he will likely cast the patient in a more negative and unfavorable light, possibly allocating less time to their diagnosis (e.g., premature closure) [31]. In addition, different types of affect can interact, such that the physician’s overall attitude towards elderly individuals might result in a different emotional reaction depending on the physician’s general temperament or the patient’s current mood. For example, research demonstrates that physician burnout (a chronic and diffuse affective condition) can intensify the effects of physician mood on their clinical behaviors with patients [32].
In addition to directly swaying judgment, affect also influences how we arrive at a judgment – that is how we think [20, 21, 30]. Positive affect – such as happiness and feelings of satisfaction – sends us a signal that our current way of making decisions is working well and indicates that we can continue whatever information processing approach (e.g., system 1 or 2) we are currently relying upon. Negative affect – particularly fear, anxiety, and sadness – sends us a signal or warning that our current way of making decisions is problematic, thereby prompting us to change our information processing strategy to better adapt to the circumstances [20, 33]. Importantly, anger is a notable exception. Anger, by virtue of being driven by a sense of certainty and confidence, sends us confirming signals on our current decision-making strategies, much like positive affect does. As we will describe later, it is critically important that anger tends to promote heuristic processing and stereotyping [34] (i.e., system 1 processing), as this carries implications for clinical reasoning [31, 35]. Before reviewing research in social psychology relevant to the process by which affect influences thinking, we first examine existent scholarship investigating the influence of affect on clinical reasoning.
Affective influence on clinical reasoning
Although little research has investigated the influence of physicians’ affective experiences on diagnostic reasoning, patient safety scholars have generated thoughtful hypotheses based on research from social and cognitive psychology. For example, some have suggested that positive affect may facilitate the processing of clinical information [36, 37]. Others have suggested that negative affect may diminish the cognitive resources available to physicians to process information carefully [38], possibly leading to disengagement from patients [32]. In the following sections, we review key findings related to the less researched topic of positive affect and then move on to negative affect, which has received more research attention. We conclude the section with a description on the broader influence of affective clinical contexts.
The influence of positive affect on clinical reasoning
Some research suggests that positive affect may facilitate the processing of clinical information, thereby making clinical reasoning more efficient. For example, Isen, Rosenzweig, and Young [39] found that medical students who completed a positive affect induction (compared to those in a control condition) made clinical judgments more quickly in a clinical problem solving task, were more likely to go beyond the assigned task to consider potential diagnoses of the other hypothetical patients in the study, and showed more signs of holistic and integrative thinking when evaluating patients by consulting different kinds of information (e.g., age, occupation, smoking status). These findings suggest that positive affect may both facilitate and broaden the scope of processing, increasing the likelihood of a correct clinical judgment.
In a subsequent study examining the effect of positive affect on clinical reasoning [37], internists were randomly assigned to either a control condition, a condition in which they read a humanistic statement on medicine, or a positive affect condition in which they received a small package of candy (an established means of eliciting positive affect in the emotion literature). Participants then read a case about a patient with hepatitis and were required to think aloud (i.e., verbalize their reasoning) while making a diagnosis. Compared to the control and humanistic statement-reading conditions, participants in the positive affect condition arrived at the correct diagnosis faster, indicating greater efficiency in processing clinical information. They also showed the least amount of anchoring (i.e., overreliance on the first part of information received) in their reasoning, indicating a broader information processing scope.
Crane et al. [36] directly tested the influence of positive affect on information processing scope in a simulation study examining fixation on patient case information among anesthetists. Practicing anesthesiologists rated the frequency with which they experienced positive and negative affect over the past three days, received a simulated patient’s case history, and provided a general anesthetic to allow wound debridement. Physicians’ performance while providing general anesthesia during the simulation were video-recorded and later coded by independent coders to determine the amount of “fixation” in their reasoning. Fixation was operationalized as the extent to which an anesthesiologist focused on a single aspect of the case to the exclusion of other relevant and important information – a tendency that has been linked to medical errors, and in more severe cases, patient death [36]. Results showed that anesthesiologists who reported more frequent positive affect in the three days prior to the study showed less fixation and were quicker to detect changes in the patient’s condition and initiate necessary interventions. These findings, although correlational, suggest that positive affect is associated with a broadened processing scope, allowing physicians to be more flexible in their clinical processing to consider multiple sources of information [36].
Although this research seems to suggest unequivocal benefits of positive affect on clinical reasoning and diagnosis, this relationship may not always be so straightforward. For example, positive affect towards patients may lead providers to over-test and over-treat patients, and may reduce a provider’s belief that a patient has a serious illness [35, 40]. Thus, future work is needed to clearly articulate the conditions in which positive affect is helpful vs. harmful to clinical decision-making and patient safety.
The influence of negative affect on clinical reasoning
While research demonstrates that positive affect can facilitate the processing of clinical information, studies suggest that negative affect – particularly anger, frustration, or irritation – may hinder it. For instance, Mamede and colleagues [38] examined internal medicine residents’ diagnostic accuracy and time to diagnose in response to written clinical vignettes of two types. Half of the vignettes involved “neutral” patients and the other half described “disruptive,” difficult patients. When responding to vignettes involving difficult (vs. neutral) patients, residents made more diagnostic errors, reported fewer clinical results, and recalled more patient behaviors. The authors suggest that the patients’ disruptive behaviors may have elicited negative emotions in the residents, who may have diverted mental resources to process these behaviors, which consequently lowered diagnostic accuracy. While this explanation is consistent with research in the social cognition literature, future research is needed to evaluate this hypothesis directly.
Negative affect can alter clinical reasoning by restricting physicians’ information processing scope. In a study investigating the effects of acute stress on clinical reasoning, researchers randomly assigned senior medical students to either a high or a low stress condition and asked them to provide medical consultation for simulated ambulatory patients [41]. Although there was no difference between conditions in diagnostic accuracy and students’ explanations for the main diagnosis, students in the high stress condition scored lower on their explanation for the differential diagnosis, suggesting that stress might have constricted reasoning scope when establishing a differential diagnosis [41].
Negative affect may also impact the diagnostic process by leading physicians to interact less with their patients. In a survey of family physicians examining the effects of mood states on physicians’ behaviors during physician-patient interactions, Kushnir and colleagues [32] found that when in a negative mood, physicians talked less to their patients, wrote more prescriptions, ordered more tests, and made more referrals to specialists. Conversely, when physicians were in a good mood, they talked longer to their patients, wrote fewer prescriptions, and made fewer referrals for tests and to specialists. These mood effects were found to be intensified by physician burnout; high burnout made unhappy physicians talk even less to their patients, prescribe even more medications, and make more referrals compared to their low-burnout-counterparts. Although it is impossible to determine whether mood states causally influenced physicians’ behaviors without random assignment, these results suggest that negative moods might lower the quality of physician-patient interaction, which can lead to diagnostic and other errors.
Researchers have also considered specific patient populations who tend to elicit negative affect, which is often due to negative attitudes or stigma that providers hold toward these patients. For example, individuals with mental illness experience a significant mortality gap and suffer from considerable healthcare disparities and rates of diagnostic errors [1, 42, 43]. This is partly due to these patients’ physical symptoms sometimes being attributed to psychological causes, an error known as diagnostic overshadowing [44, 45]. Two qualitative studies found that negative and stigmatizing attitudes held by physicians and nurses toward patients with mental illness are among the leading factors that contribute to diagnostic overshadowing [44, 45]. In a large-scale qualitative study that we recently conducted, we found that emergency providers repeatedly identified patients with psychiatric conditions and/or substance use disorders as the most challenging populations that elicited negative emotions among providers [31]. Moreover, some providers acknowledged these negative emotions had deleterious impacts on patient care; for example, providers acknowledged that they would spend less time with these patients or order tests that allowed for quicker discharge, which they recognized might lead to diagnostic errors.
In a second study with emergency medicine providers, we directly elicited provider emotions by having them recall their own recent patient encounters. Specifically, they described an encounter with a patient who (1) elicited negative emotions, specifically anger, (2) elicited positive emotions, specifically satisfaction, and (3) had a mental health condition. After each description, providers reported their emotional reactions and engagement levels during the encounter. We found that providers reported highly negative emotions in both the angry and mental health patient encounters, compared to the positive patient encounters. Moreover, these negative emotions were associated with lower levels of provider engagement. In a subsequent analysis of the impact of negative emotions on clinical reasoning and decision-making, providers reported that negative emotions elicited by angry and mental health patients led them to provide suboptimal care and treatment to those patients [35].
In addition to patients with mental illness, there are numerous other patient populations that providers may hold negative attitudes toward and who may elicit negative emotions that can adversely impact care. For example, healthcare disparities among various racial and ethnic minority populations are well-established and are due, at least in part, to affective factors [46]. Further, it is worth noting that providers’ own identities can readily interact with those of a patient in unique ways. For example, a Jewish ED physician may be emotionally triggered by a patient who arrives in his ED covered in Nazi tattoos, whereas a non-Jewish physician may be significantly less affected [47].
The affective influence of clinical contexts
Clinical contexts, like other social contexts, are inherently affective [31, 48, 49]. As such, they exert influence on the individuals who occupy them (e.g., physicians, patients, colleagues, families) and these individuals can reciprocally impact each other. This, in turn can shape clinical outcomes. Research has demonstrated a clear, unambiguous link between negative clinical contexts – characterized by rudeness and incivility – and clinical reasoning and performance. For example, Riskin and colleagues [50], in a randomized controlled trial, found that rude comments (from an external expert) given to neonatal intensive care unit (NICU) team members significantly disrupted their clinical reasoning, resulting in much less information sharing during diagnosis, which in turn led to a deterioration in diagnostic performance. Similar deterioration resulting from rudeness was also observed in their performance of clinical procedures (e.g., resuscitation).
In a follow-up study, Riskin and colleagues [51] varied the source of rudeness from colleagues to patients and shifted the recipient of rudeness (from individual NICU members to teams) and examined the extent to which rudeness impacted team-level processes and clinical outcomes. Results showed that rude remarks from patients’ families not only disrupted team processes (e.g., workload sharing, helping), but also distorted the quality of the team’s therapeutic performance (e.g., intervention performance).
These experimental results correspond well with our qualitative investigation on the emotional experiences of emergency department healthcare providers [31], in which we found that providers frequently identified patients, colleagues, and characteristics of the overall hospital and healthcare systems as sources of negative emotions, which they perceived to have a deleterious impact on their ability to deliver quality care.
Insights from social psychology: the Affect-as-Cognitive-Feedback Model
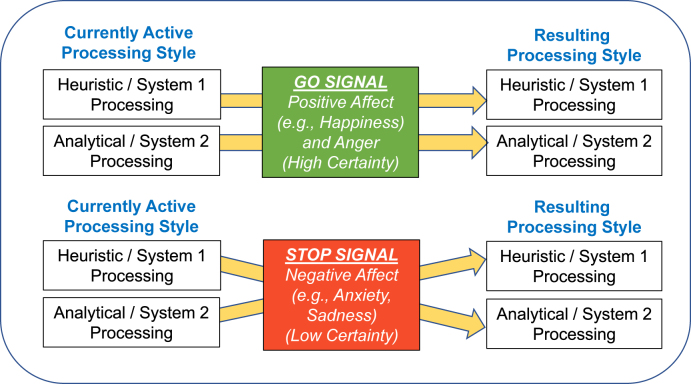
The findings reviewed above are consistent with the Affect-as-Cognitive-Feedback Model — a prominent model in the social psychology literature that explains how affect influences decision-making by providing feedback about our decisions and how we process information [20, 28, 30, 33]. As described earlier, affect is typically highly adaptive and serves a signaling function that orients individuals and directs their behaviors [52]. Positive feelings provide favorable feedback and an accompanying feeling of confidence (i.e., certainty) in one’s decision-making approach and decisions, whereas negative affect (excluding anger) provides unfavorable feedback and an accompanying lack of confidence (i.e., uncertainty). This feedback leads individuals to either accept (in the case of positive affect) or reject (in the case most negative affect) their decisions and the information processing style used to reach them – often implicitly and non-consciously [20, 26, 29, 30, 33].
Figure 1 depicts the Affect-as-Cognitive-Feedback Model. Specifically, as shown in the top of Figure 1, positive affect and anger act as a “go” signal that confers value on and confidence in whatever information or processing style is currently active and promotes the use of that information or processing style. Given that heuristic/system 1 processing is usually dominant by default and therefore is typically currently active [20, 21, 30, 33, 34], these emotions tend to promote this processing style.
Figure 1:
The Affect-as-Cognitive-Feedback Model.
Although positive affect and anger often function similarly based on research reported in the broad affect and social cognition literatures, in the clinical context, these emotions seem to exhibit differential properties with respect to information processing. As we have reviewed in an earlier section, positive affect has been found to facilitate and broaden information processing, allowing physicians to be more flexible in reasoning to consider multiple sources of information, thereby improving the likelihood of arriving at a correct diagnosis [36, 37, 39]. On the other hand, anger, frustration, and irritation appear to have little or no adaptive value in the diagnostic process. These emotions can enhance stereotype-use [53] and reliance on other heuristics [54, 55] including premature closure (e.g., failing to consider a full differential diagnosis), anchoring (e.g., incorrectly assuming a patient’s presenting condition is due to one cause), and other biases associated with diagnostic error [31, 32, 35, 45].
As shown in the bottom of Figure 1, with the exception of anger, other types of negative affect act as a “stop” signal that alerts people to potential problems with their decisions or their currently active processing style, therefore leading them to consider alternative decisions or switch decision-making styles altogether [30, 33]. For example, in clinical decision-making, anxiety signals to the healthcare provider that their typical default system 1 processing may be problematic or inaccurate, prompting them to slow down to reconsider the case at hand or to zoom in and focus on a challenging, puzzling issue (thereby activating system 2 processing) [36, 37, 48]. Thus, anxiety can transform a default system 1 processor into a system 2 processor. Indeed, moderate levels of anxiety can promote better performance and decision-making [56, 57]. In our research conducted outside of the clinical context, we find that experimentally inducing low to moderate levels of anxiety/fear in individuals leads them to process information in a relatively detailed and analytical manner [20, 21, 30, 33, 34, 54]. However, high levels of anxiety/fear can reduce individuals’ ability to engage in these more effortful thought processes and can lead to narrowing of attention, increased attention to threat, and limited attentional resources [58] – all making analytical thought more effortful and less likely.
Although system 1 processing is often active by default, note that the Affect-as-Cognitive-Feedback Model also explains how affect influences thinking under conditions in which more analytical/system 2 processing may be chronically active – as is the case for individuals with anxiety disorders or autism [59, 60]. Further, research demonstrates that dominant default thinking styles differ across cultures [61]. Thus, based on individual difference variables, cultural variables, and perhaps other factors, the influences of affect will be reverse of those already described. Future research is needed to better understand the factors that underlie differences in default thinking styles.
Valence vs. discrete emotion approaches
Although emotion research has tended to take a valence-based approach (positive vs. negative affect), research demonstrates that emotions can have more specific effects on judgment and processing when moving beyond valence to consider the characteristics of more specific or discrete emotions. Much of this work focuses on the inherent appraisal tendencies of emotions. Appraisal tendencies are prototypical cognitive features and processes that characterize each emotion [62]. For example, in addition to valence, emotions can be categorized by the extent to which they convey a sense of personal control (vs. lack thereof), a sense of certainty (vs. uncertainty), or a sense of self- vs. other-responsibility (i.e., whether the self or others should be responsible or blamed for what happened).
Appraisal-tendency theory argues that it is not just the valence of emotions that influences judgment and processing, the inherent appraisal tendencies of emotions can also have an impact [62]. Although emotions of the same valence (e.g., happy and proud, or sad and fearful) tend to generate similar effects, when emotions of the same valence differ on important appraisal dimensions, they tend to produce different results [62, 63]. A notable contrast is between shame and anger, both of which are negative in valence but differ along the dimension of self- vs. other-responsibility. Shame is characterized by a high sense of self-responsibility; whereas anger is characterized by a high sense of other-responsibility. Thus, shameful people tend to blame themselves for what happened whereas angry people tend to do the opposite [62]. This may have direct implications in clinical contexts especially with respect to actions or decisions that led to undesirable health outcomes (e.g., a medical error or misdiagnosis).
The Affect-as-Cognitive-Feedback Model is compatible with both the valence and appraisal-tendency approaches in its premise that affect or emotions provide feedback concerning value on one’s judgment [20]. Although positive emotions tend to provide positive value (e.g., happiness), and negative emotions negative value (e.g., fear), appraisal tendencies of some negative emotions also convey positive value, for example, anger is characterized by a high sense of certainty and control. In this way, this model incorporates both approaches by not restricting itself exclusively to just one type of input (be it valence or appraisal-tendency)—a characteristic that contributes to its potentially broad applications in the field of clinical decision-making.
Section summary
The Affect-as-Cognitive-Feedback Model brings a unified, tested theoretical framework with rich empirical support (for a detailed review, see ref. [20]) to the field of clinical decision-making. Not only can it explain past findings with respect to the influence of affect in clinical contexts, it can also generate specific, testable hypotheses (see next section) on when affect is likely to influence clinical decision-making and how. Seen in this perspective, the Affect-as-Cognitive-Feedback framework has arrived at a timely junction as it has the ability to establish a common ground on which stranded research programs can be joined by elucidating, conceptually, the intricate and sometimes puzzling relationship between cognition and affect.
Recommendations and research opportunities for altering adverse influences of affect on clinical reasoning and diagnostic error
Beyond its theoretical implications, the Affect-as-Cognitive-Feedback Model suggests several interventions to reduce the negative impact that affect may have on clinical reasoning and diagnostic error. The effects that we reviewed are not inevitable. Fortunately, the influence of affect on cognitive processing is highly malleable and easily altered. Research in social cognition demonstrates that cognitively priming a specific information processing style (e.g., heuristic/system 1 or analytical/system 2 processing) activates procedural knowledge (i.e., a content-free way of how to process information) that carries over to reliably influence how subsequent information is processed. Indeed, research demonstrates that simple experimental manipulations can quickly turn heuristic/system 1 processors into analytical/system 2 processors. The goal is to change one’s default information processing style from heuristic to analytic; this can be done via well-established cognitive priming methods.
For example, researchers frequently use a Navon letter task [64] in which participants view a series of letter displays (see example, Figure 2). Participants instructed to identify small letters (“T”) process information in a subsequent unrelated task more analytically than those instructed to identify the large letter (“H”). Isbell and colleagues [34] showed that anger-induced, “H”-primed participants employed greater heuristic, categorical (i.e., system 1) processing on a subsequent task designed to assess self-concept, whereas those “T”-primed used more analytical, concrete (i.e., system 2) processing.
Figure 2:
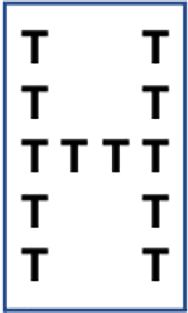
Navon letter task.
Although very much in the testing and research phase, such findings may have clinical applications. That is, to the extent that specific types of patients reliably elicit particular affective reactions in providers [35], it may be possible to build strategies for priming providers to process information more carefully (e.g., via system 2) into electronic health records, for example, for specific types of patients. Such interventions may also be tailored to specific providers based on different providers’ unique emotional triggers. This is an area of considerable research opportunity.
A second potential intervention in line with the Affect-as-Cognitive-Feedback Model focuses on another strategy for changing the effects of emotions. Simply changing what emotions are attributed to changes the effects of those emotion on judgements and decision-making [21, 30]. For example, if a clinician attributes their anger during an encounter with a patient with mental illness to something external to the patient (e.g., lack of psychological support or resources in the community), then the provider might engage in a reasoning process that is less biased by anger (and the system 1 processing that anger typically promotes), as the target of the anger has shifted from the patient to something else. In this way, the simple act of attributing one’s feelings to something other than the task at hand (i.e., evaluating the patient) changes the relevance of those feelings to the task, and thereby changes their influence on the task [35].
Finally, interventions that alter providers’ emotional experiences directly via specific emotion regulation strategies are effective in reducing adverse effects of emotions on decisions. Research demonstrates that cognitive reappraisal – thinking about different aspects of an emotional situation – can directly alter one’s emotional experience [65], [66], [67]. For example, rather than focusing on the frustrating aspects of an encounter with an angry patient, a provider may direct their attention to other aspects of the situation, such as the staff’s helpful efforts to assist the patient and provider. By changing one’s focus of attention in this way, emotions change, and their effects on clinical reasoning (i.e., overconfidence, premature closure) should similarly be altered [35]. Research demonstrates that emotional awareness and regulation skills can be developed and enhanced via emotional intelligence training interventions [68, 69], which we along with others [70], [71], [72], [73], [74] recommend be a part of medical training.
Concluding remarks
In medicine, it has long been assumed that decision-making is largely, if not entirely, cognitive [12, 14, 22]. When diagnostic errors happen, they are very often thought to be the result of faulty thinking. Hence, the solution for these errors is to think better. Part of this assumption is appropriate: determining a diagnosis is a cognitive task, and many biases can induce errors in decisions [2, 9]. However, affect can also play a major role in the diagnostic process, as it does in any of our thinking and decision-making. Indeed, decades of research in social and cognitive psychology suggest that it plays a major role in shaping our thinking and decision-making (for reviews, see refs. [20, 21]).
In this paper, we reviewed evidence demonstrating the strong influence of feelings on thinking. We also considered extant research findings related to the influence of affect on clinical reasoning. We maintain that although affect is generally adaptive and typically leads to the right decisions, it can negatively influence decision-making in the clinical context. Therefore, in order to lay an empirical foundation for the development and testing of interventions that can mitigate negative influences of affect on clinical reasoning and diagnosis, we issue an imperative call for more research. Drawing on a large body of scholarly work in social psychology, including the Affect-as-Cognitive-Feedback Model, we propose developing and testing interventions to combat the negative impact of emotions and other affective experiences on clinical decision-making, which will reduce diagnostic errors and improve clinical reasoning. By integrating the literature on patient safety with those in social cognitive and affective science, there is an abundance of opportunities to make new discoveries that will have the power to significantly reduce diagnostic errors and improve patient safety. To realize this potential, interdisciplinary collaborations are urgently needed and strongly encouraged.
Footnotes
Research funding: This research was funded by Agency for Healthcare Research and Quality, Grant # 5R01HS025752 awarded to Linda M. Isbell.
Author contributions: All authors contributed to the development and writing of this manuscript, and have accepted responsibility for the entire content of this manuscript and approved its submission.
Competing interests: Authors state no conflict of interest.
Informed consent: Not applicable.
Ethical approval: Not applicable.
References
- 1.Institute of Medicine . Improving diagnosis in health care. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 2.Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ Theory Pract. 2009;14(1 Suppl):27–35. doi: 10.1007/s10459-009-9182-2. [DOI] [PubMed] [Google Scholar]
- 3.Epstein S. Integration of the cognitive and the psychodynamic unconscious. Am Psychol. 1994;49:709–24. doi: 10.1037/0003-066x.49.8.709. [DOI] [PubMed] [Google Scholar]
- 4.Epstein S. Advanced personality. New York, NY, US: Plenum Press; 1998. Cognitive-experiential self-theory; pp. 211–38. [Google Scholar]
- 5.Epstein S, Pacini R, Denes-Raj V, Heier H. Individual differences in intuitive–experiential and analytical–rational thinking styles. J Pers Soc Psychol. 1996;71:390–405. doi: 10.1037/0022-3514.71.2.390. [DOI] [PubMed] [Google Scholar]
- 6.Tversky A, Kahneman D. Extensional versus intuitive reasoning: the conjunction fallacy in probability judgment. Psychol Rev. 1983;90:293–315. doi: 10.1037/0033-295x.90.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Croskerry P. ED cognition: any decision by anyone at any time. Can J Emerg Med. 2014;16:13–9. doi: 10.2310/8000.2013.131053. [DOI] [PubMed] [Google Scholar]
- 8.Kahneman D. Thinking, fast and slow. New York, NY: Farrar, Straus and Giroux; 2011. p. 499. [Google Scholar]
- 9.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78:775–80. doi: 10.1097/00001888-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Croskerry P, Abbass AA, Wu AW. How doctors feel: affective issues in patients’ safety. Lancet. 2008;372:1205–6. doi: 10.1016/s0140-6736(08)61500-7. [DOI] [PubMed] [Google Scholar]
- 11.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165:1493. doi: 10.1001/archinte.165.13.1493. [DOI] [PubMed] [Google Scholar]
- 12.Croskerry P, Abbass A, Wu AW. Emotional influences in patient safety. J Patient Saf. 2010;6:199–205. doi: 10.1097/pts.0b013e3181f6c01a. [DOI] [PubMed] [Google Scholar]
- 13.Damasio A. Descartes’ error: emotion, reason, and the human brain. New York, NY: Putnam Publishing; 1994. p. 336. [Google Scholar]
- 14.Heyhoe J, Birks Y, Harrison R, O’Hara JK, Cracknell A, Lawton R. The role of emotion in patient safety: are we brave enough to scratch beneath the surface? J R Soc Med. 2016;109:52–8. doi: 10.1177/0141076815620614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LeBlanc VR, McConnell MM, Monteiro SD. Predictable chaos: a review of the effects of emotions on attention, memory and decision making. Adv Health Sci Educ. 2015;20:265–82. doi: 10.1007/s10459-014-9516-6. [DOI] [PubMed] [Google Scholar]
- 16.Loewenstein G, Lerner JS. The role of affect in decision making. In: Davidson RJ, Scherer KR, Goldsmith HH, editors. Handbook of affective sciences. Oxford; New York: Oxford University Press; 2003. [Google Scholar]
- 17.De Martino B, Kumaran D, Seymour B, Dolan RJ. Frames, biases, and rational decision-making in the human brain. Science. 2006;313:684–7. doi: 10.1126/science.1128356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham WA, Brosch T. Motivational salience: amygdala tuning from traits, needs, values, and goals. Curr Dir Psychol Sci. 2012;21:54–9. doi: 10.1177/0963721411430832. [DOI] [Google Scholar]
- 19.Gupta R, Koscik TR, Bechara A, Tranel D. The amygdala and decision-making. Neuropsychologia. 2011;49:760–6. doi: 10.1016/j.neuropsychologia.2010.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huntsinger JR, Isbell LM, Clore GL. The affective control of thought: malleable, not fixed. Psychol Rev. 2014;121:600–18. doi: 10.1037/a0037669. [DOI] [PubMed] [Google Scholar]
- 21.Isbell LM, Lair EC. Moods, emotions, and evaluations as information. In: Carlston D, editor. The Oxford Handbook of Social Cognition. New York, NY: Oxford University Press; 2013. pp. 435–62. [Google Scholar]
- 22.Kozlowski D, Hutchinson M, Hurley J, Rowley J, Sutherland J. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ. 2017;17:1–13. doi: 10.1186/s12909-017-1089-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Groves JE. Taking care of the hateful patient. N Engl J Med. 1978;298:883–7. doi: 10.1056/nejm197804202981605. [DOI] [PubMed] [Google Scholar]
- 24.Smith RC, Zimny GH. Physicians’ emotional reactions to patients. Psychosomatics. 1988;29:392–7. doi: 10.1016/s0033-3182(88)72339-7. [DOI] [PubMed] [Google Scholar]
- 25.Norman GR, Eva KW. Diagnostic error and clinical reasoning. Med Educ. 2010;44:94–100. doi: 10.1111/j.1365-2923.2009.03507.x. [DOI] [PubMed] [Google Scholar]
- 26.Clore GL, Huntsinger JR. How emotions inform judgment and regulate thought. Trends Cognit Sci. 2007;11:393–9. doi: 10.1016/j.tics.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quigley KS, Lindquist KA, Barrett LF. Inducing and measuring emotion and affect: tips, tricks, and secrets. In: Reis H, Judd C, editors. Handbook of research methods in personality and social psychology. New York, NY: Oxfod University Press; 2014. [Google Scholar]
- 28.Clore GL, Wyer RS, Dienes B, Gasper K, Gohm C, Isbell L. Theories of mood and cognition: a user’s guidebook. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2001. Affective feelings as feedback: some cognitive consequences; pp. 27–62. [Google Scholar]
- 29.Clore GL, Huntsinger JR. How the object of affect guides its impact. Emot Rev. 2009;1:39–54. doi: 10.1177/1754073908097185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Isbell LM, Lair EC, Rovenpor DR. Affect-as-information about processing styles: a cognitive malleability approach. Soc Personal Psychol Compass. 2013;7:93–114. doi: 10.1111/spc3.12010. [DOI] [Google Scholar]
- 31.Isbell LM, Boudreaux ED, Chimowitz H, Liu G, Cyr E, Kimball E. What do emergency department physicians and nurses feel? A qualitative study of emotions, triggers, regulation strategies, and effects on patient care. BMJ Qual Saf. 2020;29:815–25. doi: 10.1136/bmjqs-2019-010179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kushnir T, Kushnir J, Sarel A, Cohen AH. Exploring physician perceptions of the impact of emotions on behaviour during interactions with patients. Fam Pract. 2011;28:75–81. doi: 10.1093/fampra/cmq070. [DOI] [PubMed] [Google Scholar]
- 33.Isbell LM, Lair EC, Rovenpor DR. The impact of affect on out-group judgments depends on dominant information-processing styles: evidence from incidental and integral affect paradigms. Pers Soc Psychol Bull. 2016;42:485–97. doi: 10.1177/0146167216634061. [DOI] [PubMed] [Google Scholar]
- 34.Isbell LM, Rovenpor DR, Lair EC. The impact of negative emotions on self-concept abstraction depends on accessible information processing styles. Emotion. 2016;16:1040–9. doi: 10.1037/emo0000193. [DOI] [PubMed] [Google Scholar]
- 35.Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety. BMJ Qual Saf. 2020;29:803–14. doi: 10.1136/bmjqs-2019-010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crane MF, Brouwers S, Forrest K, Tan S, Loveday T, Wiggins MW, et al. Positive affect is associated with reduced fixation in a realistic medical simulation. Hum Factors. 2017;59:821–32. doi: 10.1177/0018720817695191. [DOI] [PubMed] [Google Scholar]
- 37.Estrada CA, Isen AM, Young MJ. Positive affect facilitates integration of information and decreases anchoring in reasoning among physicians. Organ Behav Hum Decis Process. 1997;72:117–35. doi: 10.1006/obhd.1997.2734. [DOI] [Google Scholar]
- 38.Mamede S, Gog TV, Schuit SCE, den Berge KV, Daele PLAV, Bueving H, et al. Why patients’ disruptive behaviours impair diagnostic reasoning: a randomised experiment. BMJ Qual Saf. 2016;26:13–8. doi: 10.1136/bmjqs-2015-005065. [DOI] [PubMed] [Google Scholar]
- 39.Isen AM, Rosenzweig AS, Young MJ. The influence of positive affect on clinical problem solving. Med Decis Making. 1991;11:221–7. doi: 10.1177/0272989x9101100313. [DOI] [PubMed] [Google Scholar]
- 40.Mayer JD, Gaschke YN, Braveman DL, Evans TW. Mood-congruent judgment is a general effect. J Pers Soc Psychol. 1992;63:119–32. doi: 10.1037/0022-3514.63.1.119. [DOI] [Google Scholar]
- 41.Pottier P, Dejoie T, Hardouin JB, Le Loupp AG, Planchon B, Bonnaud A, et al. Effect of stress on clinical reasoning during simulated ambulatory consultations. Med Teach. 2013;35:472–80. doi: 10.3109/0142159x.2013.774336. [DOI] [PubMed] [Google Scholar]
- 42.McGinty EE, Baller J, Azrin ST, Juliano-Bult D, Daumit GL. Quality of medical care for persons with serious mental illness: a comprehensive review. Schizophr Res. 2015;165:227–35. doi: 10.1016/j.schres.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sullivan G, Han X, Moore S, Kotrla K. Disparities in hospitalization for diabetes among persons with and without Co-occurring mental disorders. Psychiatr Serv. 2006;57:1126–31. doi: 10.1176/ps.2006.57.8.1126. [DOI] [PubMed] [Google Scholar]
- 44.Shefer G, Henderson C, Howard LM, Murray J, Thornicroft G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms--a qualitative study. PLoS One. 2014;9:e111682. doi: 10.1371/journal.pone.0111682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Nieuwenhuizen A, Henderson C, Kassam A, Graham T, Murray J, Howard LM, et al. Emergency department staff views and experiences on diagnostic overshadowing related to people with mental illness. Epidemiol Psychiatr Sci. 2013;22:255–62. doi: 10.1017/s2045796012000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Institute of Medicine . Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 47.Nichols T. The pandemic was already testing me. Then a man covered in Nazi tattoos showed up in my ER. . [1 Dec 2021]. https://www.washingtonpost.com/opinions/2020/12/05/taylor-nichols-er-patient-nazi-tattoo/ [Online] Available from. Accessed.
- 48.Heyhoe J. Affective and cognitive influences on decision making in healthcare. Leeds: University of Leeds; 2013. Ph.D. Dissertation. [Google Scholar]
- 49.Heyhoe J, Lawton R. Social emotion and patient safety: an important and understudied intersection. BMJ Qual Saf. 2020;29:1–2. doi: 10.1136/bmjqs-2019-010795. [DOI] [PubMed] [Google Scholar]
- 50.Riskin A, Erez A, Foulk TA, Kugelman A, Gover A, Shoris I, et al. The impact of rudeness on medical team performance: a randomized trial. Pediatrics. 2015;136:487–95. doi: 10.1542/peds.2015-1385. [DOI] [PubMed] [Google Scholar]
- 51.Riskin A, Erez A, Foulk TA, Riskin-Geuz KS, Ziv A, Sela R, et al. Rudeness and medical team performance. Pediatrics. 2017;139:e20162305. doi: 10.1542/peds.2016-2305. [DOI] [PubMed] [Google Scholar]
- 52.Frijda NH. The emotions. Paris, France: Cambridge University Press; 1986. [Google Scholar]
- 53.Bodenhausen GV, Sheppard LA, Kramer GP. Negative affect and social judgment: the differential impact of anger and sadness. Eur J Soc Psychol. 1994;24:45–62. doi: 10.1002/ejsp.2420240104. [DOI] [Google Scholar]
- 54.Parker MT, Isbell LM. How I vote depends on how I feel: the differential impact of anger and fear on political information processing. Psychol Sci. 2010;21:548–50. doi: 10.1177/0956797610364006. [DOI] [PubMed] [Google Scholar]
- 55.Small DA, Lerner JS. Emotional policy: personal sadness and anger shape judgments about a welfare case. Polit Psychol. 2008;29:149–68. doi: 10.1111/j.1467-9221.2008.00621.x. [DOI] [Google Scholar]
- 56.Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit formation. J Comp Neurol Psychol. 1908;18:459–82. doi: 10.1002/cne.920180503. [DOI] [Google Scholar]
- 57.Hebb DO. Drives and the C. N. S. (conceptual nervous system) Psychol Rev. 1955;62:243–54. doi: 10.1037/h0041823. [DOI] [PubMed] [Google Scholar]
- 58.MacLeod C, Mathews A. Anxiety and the allocation of attention to threat. Q J Exp Psychol Sect A. 1988;40:653–70. doi: 10.1080/14640748808402292. [DOI] [PubMed] [Google Scholar]
- 59.Mikulincer M, Kedem P, Paz D. Anxiety and categorization—1. The structure and boundaries of mental categories. Pers Indiv Differ. 1990;11:805–14. doi: 10.1016/0191-8869(90)90189-x. [DOI] [Google Scholar]
- 60.Wang L, Mottron L, Peng D, Berthiaume C, Dawson M. Local bias and local-to-global interference without global deficit: a robust finding in autism under various conditions of attention, exposure time, and visual angle. Cogn Neuropsychol. 2007;24:550–74. doi: 10.1080/13546800701417096. [DOI] [PubMed] [Google Scholar]
- 61.Koo M, Clore GL, Kim J, Choi I. Affective facilitation and inhibition of cultural influences on reasoning. Cognit Emot. 2012;26:680–9. doi: 10.1080/02699931.2011.613920. [DOI] [PubMed] [Google Scholar]
- 62.Lerner JS, Keltner D. Beyond valence: toward a model of emotion-specific influences on judgement and choice. Cognit Emot. 2000;14:473–93. doi: 10.1080/026999300402763. [DOI] [Google Scholar]
- 63.Lerner JS, Keltner D. Fear, anger, and risk. J Pers Soc Psychol. 2001;81:146–59. doi: 10.1037/0022-3514.81.1.146. [DOI] [PubMed] [Google Scholar]
- 64.Navon D. Forest before trees: the precedence of global features in visual perception. Cognit Psychol. 1977;9:353–83. doi: 10.1016/0010-0285(77)90012-3. [DOI] [Google Scholar]
- 65.Gross JJ. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol. 1998;74:224–37. doi: 10.1037/0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- 66.Gross JJ. Handbook of emotion regulation. 2nd ed. New York, NY, US: Guilford Press; 2014. Emotion regulation: conceptual and empirical foundations; pp. 3–20. [Google Scholar]
- 67.Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq. 2015;26:1–26. doi: 10.1080/1047840x.2014.940781. [DOI] [Google Scholar]
- 68.Hodzic S, Scharfen J, Ripoll P, Holling H, Zenasni F. How efficient are emotional intelligence trainings: a meta-analysis. Emot Rev. 2018;10:138–48. doi: 10.1177/1754073917708613. [DOI] [Google Scholar]
- 69.Mattingly V, Kraiger K. Can emotional intelligence be trained? A meta-analytical investigation. Hum Resour Manag Rev. 2019;29:140–55. doi: 10.1016/j.hrmr.2018.03.002. [DOI] [Google Scholar]
- 70.Bourgeon L, Bensalah M, Vacher A, Ardouin J-C, Debien B. Role of emotional competence in residents’ simulated emergency care performance: a mixed-methods study. BMJ Qual Saf. 2016;25:364–71. doi: 10.1136/bmjqs-2015-004032. [DOI] [PubMed] [Google Scholar]
- 71.Nightingale S, Spiby H, Sheen K, Slade P. The impact of emotional intelligence in health care professionals on caring behaviour towards patients in clinical and long-term care settings: findings from an integrative review. Int J Nurs Stud. 2018;80:106–17. doi: 10.1016/j.ijnurstu.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 72.Shouhed D, Beni C, Manguso N, IsHak WW, Gewertz BL. Association of emotional intelligence with malpractice claims: a review. JAMA Surg. 2019;154:250–6. doi: 10.1001/jamasurg.2018.5065. [DOI] [PubMed] [Google Scholar]
- 73.Mintle LS, Greer CF, Russo LE. Longitudinal assessment of medical student emotional intelligence over preclinical training. J Am Osteopath Assoc. 2019;119:236–42. doi: 10.7556/jaoa.2019.039. [DOI] [PubMed] [Google Scholar]
- 74.Taylor C, Farver C, Stoller JK. Perspective: can emotional intelligence training serve as an alternative approach to teaching professionalism to residents? Acad Med. 2011;86:1551. doi: 10.1097/acm.0b013e318235aa76. [DOI] [PubMed] [Google Scholar]