Abstract
Purpose
Incomplete reperfusion after mechanical thrombectomy (MT) is associated with a poor outcome. Rescue therapy would potentially benefit some patients with an expanded treatment in cerebral ischemia score (eTICI) 2b50/2b67 reperfusion but also harbors increased risks. The relative benefits of eTICI 2c/3 over eTICI 2b50/67 in clinically important subpopulations were analyzed.
Methods
Retrospective analysis of our institutional database for all patients with occlusion of the intracranial internal carotid artery (ICA) or the M1/M2 segment undergoing MT and final reperfusion of ≥eTICI 2b50 (903 patients). The heterogeneity in subgroups of different time metrics, age, National Institutes of Health Stroke Scale (NIHSS), number of retrieval attempts, Alberta Stroke Programme Early CT Score (ASPECTS) and site of occlusion using interaction terms (pi) was analyzed.
Results
The presence of eTICI 2c/3 was associated with better outcomes in most subgroups. Time metrics showed no interaction of eTICI 2c/3 over eTICI 2b50/2b67 and clinical outcomes (onset to reperfusion pi = 0.77, puncture to reperfusion pi = 0.65, onset to puncture pi = 0.63). An eTICI 2c/3 had less consistent association with mRS ≤2 in older patients (>82 years, pi = 0.038) and patients with either lower NIHSS (≤9) or very high NIHSS (>19, pi = 0.01). Regarding occlusion sites, the beneficial effect of eTICI 2c/3 was absent for occlusions in the M2 segments (aOR 0.73, 95% confidence interval [CI] 0.33–1.59, pi = 0.018).
Conclusion
Beneficial effect of eTICI 2c/3 over eTICI 2b50/2b67 only decreased in older patients, M2-occlusions and patients with either low or very high NIHSS. Improving eTICI 2b50/2b67 to eTICI 2c/3 in those subgroups may be more often futile.
Supplementary Information
The online version of this article (10.1007/s00062-021-01131-0) contains supplementary material, which is available to authorized users.
Keywords: Ischemic stroke, Mechanical thrombectomy, Cerebral vessel occlusion, Risk factors, Stent retriever
Introduction
The association of better clinical outcomes and reduced long-term mortality with increased reperfusion quality of mechanical thrombectomy is well established [1–8]. A modified thrombolysis in cerebral infarction (mTICI) score of mTICI 2b and above (i.e. more than 50% reperfusion of the initially hypoperfused territory) has traditionally been considered successful [9]; however, mTICI 2b covers a wide range of reperfusion and the refined expanded treatment in cerebral ischemia (eTICI) scale subdivides it into eTICI 2b50 (50–66% reperfusion), eTICI 2b67 (67–89%) and eTICI 2c (near-complete, 90–99%). Accordingly, near complete (eTICI 2c) and complete (eTICI 3) reperfusion were associated with better clinical outcomes than eTICI 2b50/2b67 reperfusion [1, 10].
It remains less clear which patients with intraprocedural eTICI 2b50/2b67 reperfusion would benefit from rescue therapy and in which patients additional retrieval attempts may be futile/unnecessary and expose patients to unnecessary risks [11]. Recent work indicated that time metrics (particularly time from groin puncture to reperfusion) play a critical role in the effectiveness of complete reperfusion [12].
With the intention to explore a potential heterogeneity of the relative benefits of eTICI 2c/3 over eTICI 2b50/2b67, we analyzed outcome differences across different reperfusion grades in clinically important subpopulations.
Material and Methods
Study Population
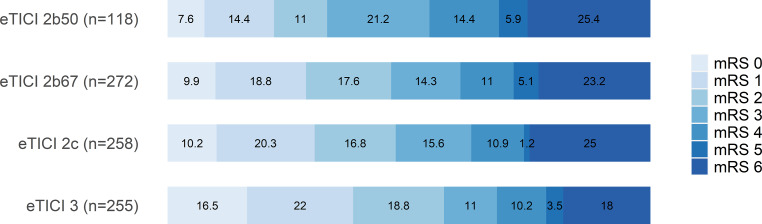
We performed a retrospective analysis of our institutional database including all patients with occlusion of the intracranial internal carotid artery (ICA) or the M1/M2 segment, undergoing endovascular stroke treatment and final reperfusion degree of ≥50% (≥eTICI 2b50) between 1st January 2010 and 31st December 2018. Patients with incomplete/insufficient angiographic documentation of preinterventional and postinterventional digital subtraction angiography (DSA) runs as well as incomplete clinical history were excluded (Fig. 1).
Fig. 1.
Flowchart showing the patient selection procedure
Image Analysis
The thrombolysis in cerebral infarction (TICI) scale visually estimates the grade of reperfusion of the initially hypoperfused territory (target downstream territory [TDT]), represented as restored antegrade capillary blush on DSA [13]. To assess the grade of reperfusion, we used the eTICI scale which makes the following distinctions: eTICI 0 (no reperfusion), eTICI 1 (thrombus reduction without any reperfusion of distal arteries), eTICI 2a (<50% reperfusion), eTICI 2b50 (50–66% reperfusion), eTICI 2b67 (67–89% reperfusion), eTICI 2c (near complete reperfusion, 90–99%), and eTICI 3 (100%) [1].
In the first step, three neuroradiologists independently evaluated the eTICI scores for 142 randomly selected patients based on preprocedural and postprocedural DSA runs, with both an anterior-posterior and a lateral projection. They were blinded to other clinical, imaging, and outcome data. Since good interrater reliability was achieved, the remaining cases (n = 761/903) were evaluated independently by core laboratory judication in the same fashion.
Collateral status was graded by two neuroradiologists based on the preinterventional DSA runs, blinded to all clinical and outcome information. Collaterals were graded according to the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) scale: 0—No collaterals visible to ischemic site, 1—Slow collaterals to the periphery of ischemic site, with persistence of some of the defect, 2—Rapid collaterals to the periphery of ischemic site, with persistence of some of the defect, and to only a portion of the ischemic territory, 3—Collaterals with slow but complete angiographic blood flow of the ischemic bed by the late venous phase, 4—Complete and rapid collateral blood flow to the vascular bed in the entire ischemic territory by retrograde perfusion [14].
Statistical Analysis
Baseline and outcome parameters between the groups were compared using the Kruskal-Wallis test for continuous variables or the Fisher’s exact test for categorical variables. Data are displayed as median (interquartile range [IQR]) and n (%) if not otherwise specified.
Interrater reliability was assessed using Krippendorff’s alpha for multiple raters. Krippendorff’s alpha is a coefficient representing the interrater reliability for any number of raters and any kind of variables. Values were interpreted as follows: 0 = poor; 0.01–0.20 = slight; 0.21–0.40 = fair; 0.41–0.60 = moderate; 0.61–0.80 = substantial and 0.81–1.0 = almost perfect agreement.
The distribution of clinical outcomes (mRS at 90 days after the intervention) for each eTICI was depicted graphically. Furthermore, binary logistic regression modeling was performed to assess the association of eTICI and clinical outcome (dichotomized into mRS ≤2 = good outcome versus mRS >2 = poor outcome [15]) and to account for potential prespecified confounders based on the literature (age, sex, NIHSS on admission, number of retrieval attempts, site of intracranial occlusion, general anesthesia, time from onset to groin puncture and ASPECTS).
The cases were then grouped into eTICI 2b50/2b67 and eTICI 2c/3. A multiplicative interaction term (eTICI*variable) was used to test for interaction with the following variables: continuous time metrics (onset to reperfusion time, puncture to reperfusion time and onset to puncture time), age on admission, NIHSS on admission, number of retrieval attempts, ASPECTS, ASITN/SIR DSA collateral score and site of occlusion.
To assess heterogeneity, subgroups were defined based on their quartiles for time metrics, age, and NIHSS; for ASPECTS as 0–4, 5–7, and 8–10 [16]; for collaterals ASITN/SIR 0/1, 2, and 3/4 (due to the small number of cases with ASITN/SIR 0 and 4, respectively); and for the number of retrieval attempts as 1, 2, and ≥3. Finally, marginal effects were plotted for time metrics and age as well as point estimates for ASPECTS.
All statistical analyses were conducted using R (Version 4.0.2, R Foundation for Statistical Computing, Vienna, Austria) [17]. A two-tailed p-value of <0.05 was considered statistically significant.
Results
Population
A total of 903 patients with occlusion of the intracranial ICA or M1/M2 segments (median age 75 years, IQR 63–82 years, 51% female) were included. Baseline characteristics are shown in Table 1. Group sizes were almost balanced, only the eTICI 2b50 group was smaller. With higher degrees of reperfusion, there was a trend towards shorter time from symptom onset to groin puncture (eTICI 2b50 median 250.5 min (IQR 175.5–383.5 min), eTICI 2b67 median 238.5 min (IQR 170–355.25 min), eTICI 2c median 233.5 min (IQR 168–358.75 min), eTICI 3 median 213 min (IQR 154–313 min), overall p = 0.03) and a lower number of retrieval attempts (overall p < 0.001). Patients with NIHSS ≤9 presented with better collaterals (median ASITN/SIR 3, IQR 2–4) than patients with NIHSS 10–19 (median ASITN/SIR 1, IQR 1–2, p < 0.001) and consequently, patients with NIHSS ≥20 had worse collaterals (median ASITN/SIR 1, IQR 1–2) than patients with NIHSS 10–19 (p < 0.001) (Suppl. Table I). Except for a higher proportion of current/history of smoking in the eTICI 2b67 population, the groups were well balanced regarding risk factors and stroke etiology.
Table 1.
Patient characteristics overall and stratified by eTICI scores
| All (N = 903) | eTICI 2b50 (n = 118) | eTICI 2b67 (n = 272) | eTICI 2c (n = 258) | eTICI 3 (n = 255) | p | |
|---|---|---|---|---|---|---|
| Age (years) | 75 (63–82) | 74 (60.25–83) | 75 (63.75–81) | 73 (62–82) | 76 (64–83.5) | 0.37 |
| Sex (female) | 464 (51.4) | 70 (59.3) | 131 (48.2) | 136 (52.7) | 127 (49.8) | 0.21 |
| Admission NIHSS | 15 (9–19) | 15 (10–19) | 15 (9.75–20) | 15 (9–20) | 15 (9.5–19) | 0.78 |
| Admission imaging modality (MRI) | 481 (53.3) | 78 (66.1) | 134 (49.3) | 128 (49.6) | 141 (55.3) | 0.01* |
| Admission ASPECTS | 8 (6–9) | 7 (6–9) | 8 (7–9) | 8 (6–9) | 8 (7–9) | 0.02* |
| Onset to puncture (min) | 232 (165.5–350) | 250.5 (175.5–383.5) | 238.5 (170–355.25) | 233.5 (168–358.75) | 213 (154–313) | 0.03* |
| Number of retrieval attempts | <0.001*** | |||||
| 1 | 527 (58.4) | 46 (39.0) | 140 (51.5) | 165 (64.0) | 176 (69.0) | |
| 2 | 208 (23) | 36 (30.5) | 78 (28.7) | 48 (18.6) | 46 (18.0) | |
| ≥3 | 168 (18.6) | 36 (30.5) | 54 (19.9) | 45 (17.4) | 33 (12.9) | |
| Site of intracranial occlusion | 0.33 | |||||
| Intracranial ICA | 36 (4) | 1 (0.8) | 17 (6.2) | 11 (4.3) | 7 (2.7) | |
| T or L occlusion of ICA | 210 (23.3) | 23 (19.5) | 57 (21.0) | 67 (26.0) | 63 (24.7) | |
| M1 | 514 (56.9) | 65 (55.1) | 162 (59.6) | 145 (56.2) | 142 (55.7) | |
| M2 | 143 (15.8) | 29 (24.6) | 36 (13.2) | 35 (13.6) | 43 (16.9) | |
| ASITN/SIR DSA collateral score | 0.156 | |||||
| 0 | 61 (6.8) | 8 (6.8) | 22 (8.1) | 14 (5.4) | 17 (6.7) | |
| 1 | 355 (39.3) | 41 (34.7) | 99 (36.4) | 99 (38.4) | 116 (45.5) | |
| 2 | 250 (27.7) | 34 (28.8) | 78 (28.7) | 83 (32.2) | 55 (21.6) | |
| 3 | 221 (24.5) | 33 (28.0) | 69 (25.4) | 54 (20.9) | 65 (25.5) | |
| 4 | 16 (1.8) | 2 (1.7) | 4 (1.5) | 8 (3.1) | 2 (0.8) | |
| Intubation narcosis | 640 (70.9) | 82 (69.5) | 193 (71.0) | 188 (72.9) | 177 (69.4) | 0.83 |
| 3‑month mRS ≤2 | 434 (48.1) | 39 (33.1) | 126 (46.3) | 123 (47.7) | 146 (57.3) | <0.001*** |
| Risk factors | ||||||
| Diabetes | 148 (16.4) | 19 (16.1) | 42 (15.5) | 42 (16.3) | 45 (17.6) | 0.93 |
| Arterial hypertension | 638 (70.7) | 80 (67.8) | 197 (72.7) | 176 (68.2) | 185 (72.5) | 0.53 |
| Dyslipidemia | 513 (56.9) | 64 (54.7) | 157 (57.7) | 137 (53.1) | 155 (60.8) | 0.34 |
| Smoking history | 209 (23.3) | 27 (22.9) | 79 (29.4) | 53 (20.5) | 50 (19.8) | 0.04* |
| Previous stroke | 114 (12.6) | 18 (15.3) | 39 (14.3) | 26 (10.1) | 31 (12.2) | 0.39 |
| Coronary heart disease | 184 (20.5) | 20 (16.9) | 53 (19.6) | 47 (18.3) | 64 (25.2) | 0.15 |
| Stroke cause | 0.14 | |||||
| Atherosclerosis | 97 (10.8) | 11 (9.3) | 36 (13.3) | 30 (11.6) | 20 (7.9) | |
| Cardioembolic | 407 (45.2) | 42 (35.6) | 126 (46.5) | 111 (43.0) | 128 (50.4) | |
| Other, determined etiology | 56 (6.2) | 11 (9.3) | 14 (5.2) | 17 (6.6) | 14 (5.5) | |
| Undetermined etiology | 341 (37.8) | 54 (45.8) | 95 (35.1) | 100 (38.8) | 92 (36.2) | |
| IVT bridging | 366 (40.5) | 43 (36.4) | 106 (39.0) | 102 (39.5) | 115 (45.1) | 0.33 |
Data are displayed as median (IQR) and n (%) if not otherwise specified
NIHSS National Institutes of Health Stroke Scale, ASPECTS Alberta Stroke Programme Early CT score, ICA internal carotid artery, mRS modified Rankin Scale, IVT intravenous thrombolysis, MRI magnetic resonance imaging, ASITN/SIR American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology, DSA digital subtraction angiography, eTICI expanded treatment in cerebral ischemia
*p < 0.05, ***p < 0.001
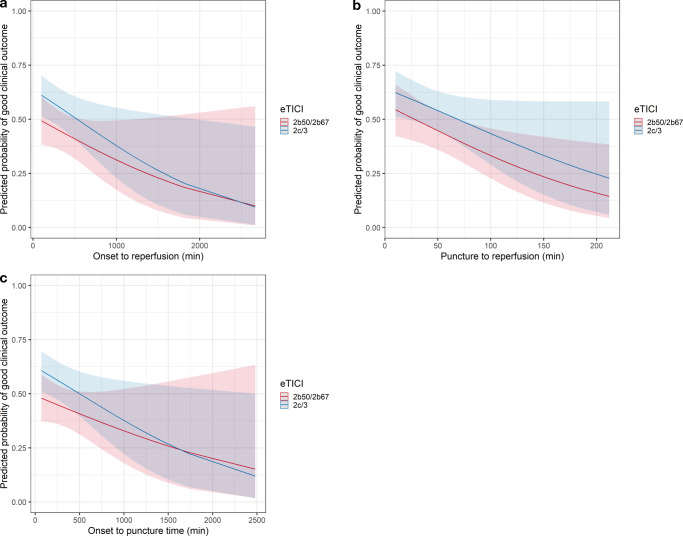
Degree of Reperfusion and Clinical Outcome
Higher degrees of eTICI were associated with mRS 90-day ≤2 (eTICI 2b50 as Reference, Table 2): eTICI 3 aOR 3.21 (95% CI 1.86–5.61), eTICI 2c aOR 1.91 (1.12–3.31), and eTICI 2b67 aOR 1.94 (1.14–3.33) (Fig. 2). Similarly, the proportion of patients with severe disability or death (mRS 5–6) decreased with higher eTICI scores, as did the proportion of patients with an intermediate level of disability (mRS 3–4).
Table 2.
Multivariable logistic regression model with adjusted odds ratios (aOR) for good clinical outcome (mRS90-day ≤2)
| Variable | aOR | 95% CI | p |
|---|---|---|---|
| Age on admission (per year) | 0.93 | 0.92–0.95 | <0.001*** |
| Male gender | 1.04 | 0.78–1.46 | 0.80 |
| NIHSS on admission (per point) | 0.92 | 0.9–0.95 | <0.001*** |
| ASPECTS | 1.33 | 1.22–1.46 | <0.001*** |
| Site of occlusion | |||
| Intracranial ICA | Reference | ||
| T or L occlusion of ICA | 1.09 | 0.46–2.43 | 0.83 |
| M1 | 1.45 | 0.63–3.13 | 0.36 |
| M2 | 1.06 | 0.42–2.42 | 0.90 |
| Intubation narcosis (yes) | 0.87 | 0.6–1.23 | 0.44 |
| Onset to puncture (per min) | 0.99 | 0.998–0.999 | 0.02* |
| Number of maneuvers | |||
| 1 | Reference | ||
| 2 | 0.64 | 0.45–0.96 | 0.02* |
| ≥3 | 0.65 | 0.43–0.99 | 0.049* |
| eTICI score | |||
| eTICI 2b50 | Reference | ||
| eTICI 2b67 | 1.94 | 1.14–3.33 | 0.02* |
| eTICI 2c | 1.91 | 1.12–3.31 | 0.02* |
| eTICI 3 | 3.21 | 1.86–5.61 | <0.001*** |
NIHSS National Institutes of Health Stroke Scale, ASPECTS Alberta Stroke Programme Early CT score, ICA internal carotid artery, eTICI expanded treatment in cerebral ischemia
*p < 0.05, ***p < 0.001
Fig. 2.
Percentage of patients with respective clinical outcome (mRS) 90 days after ischemic stroke, stratified by final eTICI scores
Interrater agreement among the 3 neuroradiologists for eTICI rating of 142 patients reached almost perfect agreement (Krippendorff’s alpha = 0.87, 95% CI 0.83–0.91).
Heterogeneity of the Association of TICI2c/3 and good Clinical Outcomes with Strata of Time Metrics
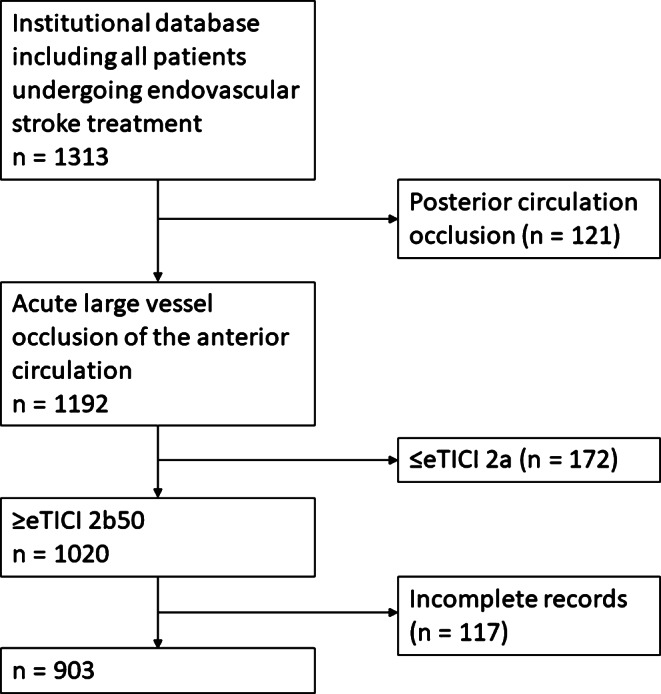
Time metrics as continuous variables showed no interaction with dichotomized eTICI scores (eTICI 2b50/2b67 vs. eTICI 2c/3; p for interaction: time from onset to reperfusion p = 0.77, time from groin puncture to reperfusion p = 0.65, time from onset to groin puncture p = 0.63). The adjusted odds ratios (aOR) for mRS 90-day ≤2 stratified by dichotomized eTICI scores slightly changed between different quartiles but showed no clear trend (Fig. 3).
Fig. 3.
Adjusted odds ratios (aOR) for eTICI 2c/3 reperfusion for good clinical outcome (mRS-90 day ≤2) according to various time course metrics and baseline characteristics. Adjusted odds ratios, 95% CI, and p-values for interaction are shown. Asterisk Exploratory p-values show interaction for age >82 years vs. ≤82 years, M2 occlusions vs. ICA/T/L/M1 occlusions, and NIHSS 10–19 vs. NIHSS ≤9/>19 pooled. CI confidence interval
The change of probability of a good clinical outcome (mRS-90d ≥2) over time courses stratified by dichotomized eTICI scores are shown in Fig. 4 and show stable superiority of eTICI 2c/3 over eTICI 2b50/2b67.
Fig. 4.
Predicted probabilities of good clinical outcome (mRS-90d ≤2) a on onset to reperfusion time, b on groin puncture to reperfusion time, c on onset to groin puncture time, stratified by eTICI, using multivariable logistic regression adjusted to age, sex, NIHSS on admission, number of retrieval attempts, site of intracranial occlusion, intubation narcosis, ASPECTS, and an multiplicative interaction term for each corresponding continuous time metric. The regression lines and 95% CI are shown
We also observed a decreasing proportion of patients with eTICI 2c/3 reperfusion with increasing time metrics, probably most striking in the subgroups of the puncture to reperfusion time: 185/264 (70.1%) patients achieved eTICI 2c/3 in the group with ≤28 min, 131/215 (60.9%) patients in the group with 29–40 min, 120/232 (51.7%) patients in the group with 41–65 min and only 77/192 (40.1%) patients in the group with >65 min.
Heterogeneity of the Association of TICI2c/3 and good Clinical Outcomes with Strata of Other Baseline Characteristics
Older age groups showed a trend towards decreasing beneficial effect of eTICI 2c/3 over eTICI 2b50/2b67 (p for interaction = 0.08), adjusted odds ratios for each quartile were as follows (Fig. 3): ≤62 years aOR 2.19 (95% CI 1.14–4.27), 63–73 years aOR 1.97 (95% CI 1.06–3.71), 74–82 years aOR 1.77 (95% CI 0.95–3.33), >82 aOR 0.68 (95% CI 0.3–1.51). There was a statistically significant interaction of effect when comparing the last quartile to the three others pooled (p = 0.038). These findings did not change substantially in a subanalysis including only patients with prestroke mRS ≤2 (n = 802, p for interaction = 0.09): ≤62 years aOR 2.06 (95% CI 1–4.23), 63–73 years aOR 2.24 (95% CI 1.11–4.59), 74–82 years aOR 1.95 (95% CI 1.01–3.84), and >82 years aOR 0.69 (95% CI 0.29–1.65).
There was no trend in change of beneficial effect of eTICI 2c/3 in quartiles of the number of retrieval attempts (p for interaction = 0.84) and no statistically significant interaction for NIHSS on admission when quartiles were handled as independent groups (p for interaction = 0.37). In patients with low NIHSS (≤9, aOR 1.16, 95% CI 0.63–2.14) and patients with high NIHSS (>19, aOR 1.15, 95% CI 0.52–2.6) however, eTICI 2c/3 had less impact on good clinical outcome as opposed to the middle groups (NIHSS 10–19, aOR 1.91, 95% CI 1.31–2.82, p for interaction = 0.01). In a further subgroup analysis of the low NIHSS group, patients with NIHSS ≤5 benefited less from eTICI 2c/3 (n = 103, aOR 0.34, 95% CI 0.11–1.03) than patients with NIHSS 6–9 (n = 133, aOR 2.08, 95% CI 0.9–4.93).
We found an increasing beneficial effect of eTICI 2c/3 with decreasing collateral scores (ASITN/SIR 3/4 aOR 0.99, 95% CI 0.53–1.82, ASITN/SIR 2 aOR 1.76, 95% CI 0.96–3.24 and ASITN/SIR 0/1 aOR 2.28, 95% CI 1.39–3.83, p for interaction 0.08).
There was no heterogeneity regarding the association of eTICI 2c/3 with good clinical outcomes across ASPECTS (Fig. 3). The point estimate of eTICI 2c/3 vs. eTICI 2b50/2b67 regarding good clinical outcomes was aOR 2.39 (95% CI 0.69–9.44) in ASPECTS 0–4 compared to a point estimate of aOR 1.82 (95% CI 1.02–3.28) and aOR 1.43 (95% CI 0.96–2.15) in ASPECTS 5–7 and 8–10, respectively (p for interaction = 0.26).
The change of probability of a good clinical outcome (mRS ≤2) over age (Fig. 5) and ASPECTS (Fig. 6) stratified by dichotomized eTICI scores again showed stable superiority of eTICI 2c/3 over eTICI 2b50/2b67 with the exception of older patients and patients with ASPECTS 10.
Fig. 5.
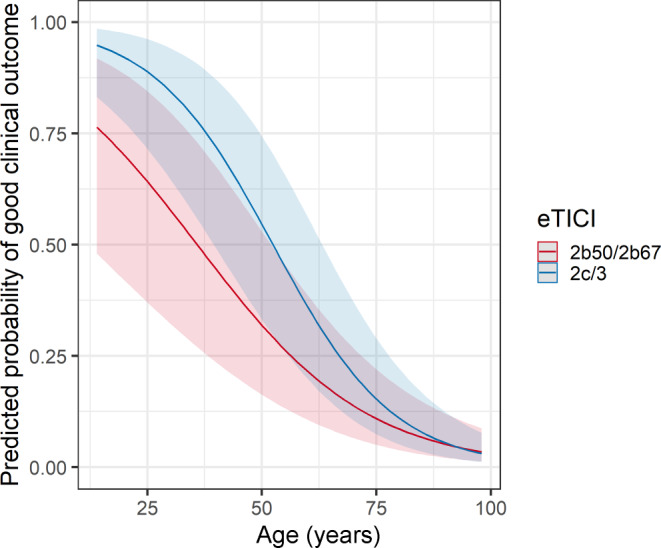
Predicted probabilities of good clinical outcome (mRS-90d ≤2) on age on admission, stratified by eTICI, using multivariable logistic regression adjusted to age, sex, NIHSS on admission, number of retrieval attempts, site of intracranial occlusion, intubation narcosis, ASPECTS, time from onset to puncture and a multiplicative interaction term for age. The regression lines and 95% CI are shown
Fig. 6.
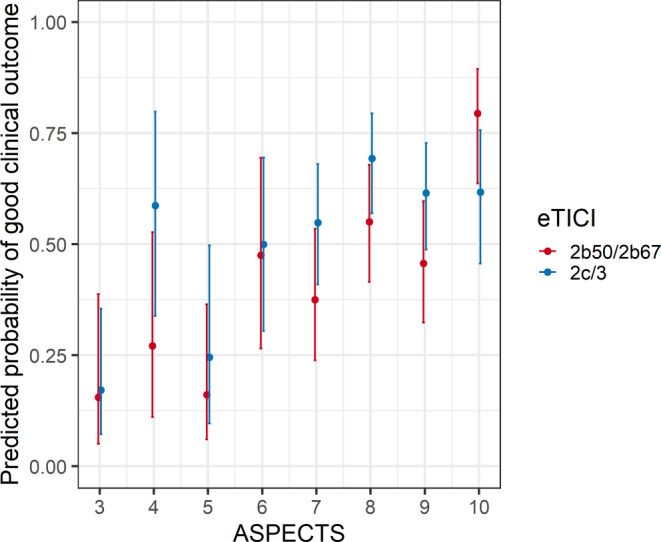
Predicted probabilities of good clinical outcome (mRS-90d ≤2) on ASPECTS, stratified by eTICI, using multivariable logistic regression adjusted to age, sex, NIHSS on admission, number of retrieval attempts, site of intracranial occlusion, intubation narcosis, ASPECTS, time from onset to puncture and a multiplicative interaction term for ASPECTS. The point estimates and 95% CI are shown
We found beneficial effects of eTICI 2c/3 in occlusions of the intracranial ICA/T or L occlusions (aOR 2.09, 95% CI 1.09–4.1) and of the M1 segments (aOR 1.64, 95% CI 1.06–2.54); however, this association was absent in patients with M2 occlusions (aOR 0.73, 95% CI 0.33–1.59, p for interaction vs. other occlusion sites pooled = 0.018).
Discussion
This study has the following main findings: 1) better eTICI scores were associated with better clinical outcomes across several subgroups, including a large range of early ischemic changes and various time courses, and 2) a decreasing beneficial effect of eTICI 2c/3 over eTICI 2b50/2b67 was only found in older patient groups, more distal occlusions and patients with either low or very high NIHSS.
Effect of near Complete/Complete Reperfusion in Subgroups
In line with previous work [1, 10], we found better outcomes for patients with ≥eTICI 2b67 reperfusion, when compared to patients with eTICI 2b50 reperfusion.
We did not find interactions of various time courses with clinical outcome after 90 days, contradicting the results of the study of Kitano et al. [12]. They found decreasing association of good clinical outcome of mTICI 3 reperfusion over mTICI 2b after ≥80 min puncture to reperfusion time. It should be noted that our quartiles were different, with the upper quartile being >65 min puncture to reperfusion time, indicating differences between the two cohorts; however, with prolonged time courses, we found overall decreasing beneficial effects of successful reperfusion and also a decreasing likelihood of eTICI 2c/3 reperfusion. These findings make it reasonable to assume that longer onset to admission and/or longer procedure times promote tissue infarction and worse clinical outcomes as described before [18–21].
We found a trend of decreasing beneficial effect of complete recanalization in older patient groups, with the biggest leap being in the group with patients older than 82 years. This phenomenon is well known and probably relies on multiple factors, such as higher prevalence of comorbidities, higher rates of polypharmacy, and reduced neuronal plasticity [22–24]. Moreover, there is generally a less stringent association of successful reperfusion, initial neurological improvement and mid-term functional outcome in older patients [25].
Another interesting finding is that patients with either low NIHSS (≤9) or very high NIHSS (>19) did not benefit from eTICI 2c/3 as much as the group with NIHSS 10–19. A possible explanation for this could be that patients presenting with low NIHSS were more likely to have good to excellent collateral status and patients presenting with very high NIHSS were more likely to have poor collateral status. Previous studies showed the association of adequate collaterals and good tissue outcome [26, 27] and our results are in line with these findings, as the difference of eTICI 2b50/2b67 to eTICI 2c/3 reperfusion did not play a crucial role in patients with adequate collaterals. Also in favor of this hypothesis, patients in our cohort with NIHSS ≤5 benefited less from eTICI 2c/3 than patients with NIHSS 6–9. On the other hand, patients with poor collaterals benefited significantly more from a final eTICI 2c/3 than patients with good to excellent collaterals, underlining the importance of complete or near complete reperfusion especially in patients with poor collaterals.
While a beneficial effect of eTICI 2c/3 on the mRS at 90 days was present in ICA/T and M1 occlusions, it was absent in M2 occlusions. Obviously, eTICI 2b50/2b67 perfusion deficits after M2 occlusions are significantly smaller compared to the range of possible perfusion deficits in eTICI 2b50/2b67 reperfusion after e.g. M1 occlusions. Other possible explanations are different collateral situations in medium vessel occlusions and smaller amounts of affected brain tissue and therefore having a lower probability to affect more eloquent brain areas. In this sense, reliable measurement of the volume of remaining hypoperfused tissue during mechanical thrombectomy (e.g. with flat-panel CT perfusion) could help in deciding whether to extend or discontinue the procedure.
Possible Implications on Patient Selection
Regarding extended mechanical thrombectomy for improving eTICI 2b50/2b67 to eTICI 2c/3, it is still not possible to draw clear boundaries for proper patient selection. In an individual case-based decision the operator may weigh in the likelihood of the improvement being clinically futile, which seems to occur more often in older patients, M2 occlusions and patients with either low or very high NIHSS.
Limitations
The retrospective analysis of data from a single center implicates limitations of our study and generalizability of our results on other cohorts has to be validated. Furthermore, we found shorter time from symptom onset to groin puncture and lower number of retrieval attempts in patients with higher degrees of reperfusion, possibly biasing our findings. While we have corrected for these confounders in all presented logistic regression analyses, there was high collinearity between these variables and the possibility of residual and hidden confounding remains.
The results of our study should be interpreted with caution. It is not clear whether secondary established eTICI 2c/3 (after initial eTICI 2b50/2b67 reperfusion) over eTICI 2b50/2b67 has the same beneficial effects as first pass eTICI 2c/3, but recent reports seem promising [28, 29]. On the other hand, a lack of benefit of primary eTICI 2c/3 reperfusion over eTICI 2b50/2b67 indicates little to no benefit in secondary established eTICI 2c/3 reperfusion.
A particular strength of our study is the consistent core laboratory judication of the eTICI scores of our large sample size.
Conclusion
The beneficial effect of eTICI 2c/3 over eTICI 2b50/2b67 was stable over various time metrics. It only decreased in older patient groups, M2 occlusions, patients with either low or very high NIHSS and patients with good to excellent collaterals. Improving eTICI 2b50/2b67 to eTICI 2c/3 in those subgroups may be more often futile, which should be acknowledged when making individualized decisions regarding potential improvements from eTICI 2b50/2b67 to eTICI 2c/3.
Supplementary Information
Acknowledgments
Funding
This study was supported by the Swiss Academy of Medical Sciences (SAMS) within the framework of the Young Talents in Clinical Research Program and grants provided by the Clinical Trials Unit Bern, University of Bern.
Author Contribution
Johannes Kaesmacher and Christoph Kurmann contributed to the study conception and design. Material preparation, data collection and analysis were performed by Christoph Kurmann, Johannes Kaesmacher, Eike Piechowiak, Tomas Dobrocky, Felix Zibold and Adnan Mujanovic. The first draft of the manuscript was written by Christoph Kurmann and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Conflict of interest
T.R. Meinel reports research support from the Bangerter Rhyner Foundation, Swiss National Foundation and the Swiss Heart Foundation. M. Arnold reports personal fees from Bayer, Bristol-Myers Squibb, Medtronic, Amgen, Daiichi Sankyo, Nestlé Health Sciences, Boehringer Ingelheim, and Covidien during the conduct of the study. U. Fischer reports grants during the conduct of the study from Medtronic, Stryker, and CSL Behring outside the submitted work. J. Gralla is a global principal investigator of STAR (Solitaire FR Thrombectomy for Acute Revascularisation), Clinical Event Committee member of the PROMISE study (Prospective, Multicenter, Observational, Single-Arm European Registry on the ACE Reperfusion Catheters and the Penumbra System in the Treatment of Acute Ischemic Stroke; Penumbra), and a principal investigator and consultant for the SWIFT DIRECT study (Solitaire With the Intention for Thrombectomy Plus Intravenous tPA Versus DIRECT Solitaire Stent-Retriever Thrombectomy in Acute Anterior Circulation Stroke; Medtronic) and receives Swiss National Science Foundation grants for magnetic resonance imaging in stroke. J. Kaesmacher reports grants from the Swiss Academy of Medical Sciences/Bangerter Foundation, Swiss Stroke Society, and Clinical Trial Unit Bern during the conduct of the study. C.C. Kurmann, A. Mujanovic, E.I. Piechowiak, T. Dobrocky, F. Zibold, M. Beyeler, J. Vynckier, D. Seiffge and P. Mordasini declare that they have no competing interests.
Ethical standards
This study was performed in line with the principles of the Declaration of Helsinki. Institutional Review Board approval was obtained. Consent to participate: written informed consent was obtained from all subjects (patients) in this study. Consent for publication: not applicable.
Footnotes
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code Availability
Not applicable.
References
- 1.Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, Mitchell PJ, van der Lugt A, Menon BK, San Román L, Campbell BC, Muir KW, Hill MD, Dippel DW, Saver JL, Demchuk AM, Dávalos A, White P, Brown S, Goyal M, HERMES Collaborators eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2019;11:433–438. doi: 10.1136/neurintsurg-2018-014127. [DOI] [PubMed] [Google Scholar]
- 2.Kaesmacher J, Dobrocky T, Heldner MR, Bellwald S, Mosimann PJ, Mordasini P, Bigi S, Arnold M, Gralla J, Fischer U. Systematic review and meta-analysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: success revisited. J Neurol Neurosurg Psychiatry. 2018;89:910–917. doi: 10.1136/jnnp-2017-317602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rizvi A, Seyedsaadat SM, Murad MH, Brinjikji W, Fitzgerald ST, Kadirvel R, Rabinstein AA, Kallmes DF. Redefining ‘success’: a systematic review and meta-analysis comparing outcomes between incomplete and complete revascularization. J Neurointerv Surg. 2019;11:9–13. doi: 10.1136/neurintsurg-2018-013950. [DOI] [PubMed] [Google Scholar]
- 4.Tung EL, McTaggart RA, Baird GL, Yaghi S, Hemendinger M, Dibiasio EL, Hidlay DT, Tung GA, Jayaraman MV. Rethinking Thrombolysis in Cerebral Infarction 2b: Which Thrombolysis in Cerebral Infarction Scales Best Define Near Complete Recanalization in the Modern Thrombectomy Era? Stroke. 2017;48:2488–2493. doi: 10.1161/STROKEAHA.117.017182. [DOI] [PubMed] [Google Scholar]
- 5.Almekhlafi MA, Mishra S, Desai JA, Nambiar V, Volny O, Goel A, Eesa M, Demchuk AM, Menon BK, Goyal M. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol. 2014;20:21–27. doi: 10.15274/INR-2014-10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal M, Fargen KM, Turk AS, Mocco J, Liebeskind DS, Frei D, Demchuk AM. 2C or not 2C: defining an improved revascularization grading scale and the need for standardization of angiography outcomes in stroke trials. J Neurointerv Surg. 2014;6:83–86. doi: 10.1136/neurintsurg-2013-010665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, Saleme S, Costalat V, Bracard S, Desal H, Mazighi M, Consoli A, Piotin M, Lapergue B, ASTER Trial Investigators Modified Thrombolysis in Cerebral Infarction 2C/Thrombolysis in Cerebral Infarction 3 Reperfusion Should Be the Aim of Mechanical Thrombectomy: Insights From the ASTER Trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization) Stroke. 2018;49:1189–1196. doi: 10.1161/STROKEAHA.118.020700. [DOI] [PubMed] [Google Scholar]
- 8.Beyeler M, Weber L, Kurmann CC, Piechowiak EII, Mosimann PJ, Zibold F, Meinel TR, Branca M, Goeldlin M, Pilgram-Pastor SM, Grunder L, Arnold M, Seiffge D, Meier R, Heldner MR, Dobrocky T, Mordasini P, Gralla J, Fischer U, Kaesmacher J. Association of reperfusion success and emboli in new territories with long term mortality after mechanical thrombectomy. J Neurointerv Surg. 2021 doi: 10.1136/neurintsurg-2021-017422. [DOI] [PubMed] [Google Scholar]
- 9.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–e418. doi: 10.1161/STROKEAHA.118.022606. [DOI] [PubMed] [Google Scholar]
- 10.Behme D, Tsogkas I, Colla R, Gera RG, Schregel K, Hesse AC, Maier IL, Liman J, Liebeskind DS, Psychogios MN. Validation of the extended thrombolysis in cerebral infarction score in a real world cohort. PLoS One. 2019;14:e0210334. doi: 10.1371/journal.pone.0210334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaesmacher J, Ospel JM, Meinel TR, Boulouis G, Goyal M, Campbell BCV, Fiehler J, Gralla J, Fischer U. Thrombolysis in Cerebral Infarction 2b Reperfusions: To Treat or to Stop? Stroke. 2020;51:3461–3471. doi: 10.1161/STROKEAHA.120.030157. [DOI] [PubMed] [Google Scholar]
- 12.Kitano T, Todo K, Yoshimura S, Uchida K, Yamagami H, Sakai N, Sakaguchi M, Nakamura H, Kishima H, Mochizuki H, Ezura M, Okada Y, Kitagawa K, Kimura K, Sasaki M, Tanahashi N, Toyoda K, Furui E, Matsumaru Y, Minematsu K, Morimoto T. Futile complete recanalization: patients characteristics and its time course. Sci Rep. 2020;10:4973. doi: 10.1038/s41598-020-61748-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BF, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS, Cerebral Angiographic Revascularization Grading (CARG) Collaborators. STIR Revascularization working group. STIR Thrombolysis in Cerebral Infarction (TICI) Task Force Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44:2650–2663. doi: 10.1161/STROKEAHA.113.001972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, Dillon W, Warach S, Broderick J, Tilley B, Sacks D, Technology Assessment Committee of the American Society of Interventional and Therapeutic Neuroradiology. Technology Assessment Committee of the Society of Interventional Radiology Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34:e109–e137. doi: 10.1161/01.STR.0000082721.62796.09. [DOI] [PubMed] [Google Scholar]
- 15.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, HERMES collaborators Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 16.Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F, THRACE investigators Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–1147. doi: 10.1016/S1474-4422(16)30177-6. [DOI] [PubMed] [Google Scholar]
- 17.R Core Team . A language and environment for statistical computing. R Foundation for Statistical Computing. 2019. [Google Scholar]
- 18.Kaesmacher J, Maamari B, Meinel TR, Piechowiak EI, Mosimann PJ, Mordasini P, Goeldlin M, Arnold M, Dobrocky T, Boeckh-Behrens T, Berndt M, Michel P, Requena M, Benali A, Pierot L, Mendes Pereira V, Boulouis G, Brehm A, Sporns PB, Ospel JM, Gralla J, Fischer U, BEYOND-SWIFT Investigators Effect of Pre- and In-Hospital Delay on Reperfusion in Acute Ischemic Stroke Mechanical Thrombectomy. Stroke. 2020;51:2934–2942. doi: 10.1161/STROKEAHA.120.030208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bourcier R, Goyal M, Liebeskind DS, Muir KW, Desal H, Siddiqui AH, Dippel DWJ, Majoie CB, van Zwam WH, Jovin TG, Levy EI, Mitchell PJ, Berkhemer OA, Davis SM, Derraz I, Donnan GA, Demchuk AM, van Oostenbrugge RJ, Kelly M, Roos YB, Jahan R, van der Lugt A, Sprengers M, Velasco S, Lycklama À Nijeholt GJ, Hassen BW, Burns P, Brown S, Chabert E, Krings T, Choe H, Weimar C, Campbell BCV, Ford GA, Ribo M, White P, Cloud GC, San Roman L, Davalos A, Naggara O, Hill MD, Bracard S, HERMES Trialists Collaboration Association of Time From Stroke Onset to Groin Puncture With Quality of Reperfusion After Mechanical Thrombectomy: A Meta-analysis of Individual Patient Data From 7 Randomized Clinical Trials. JAMA Neurol. 2019;76:405–411. doi: 10.1001/jamaneurol.2018.4510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meinel TR, Kaesmacher J, Mordasini P, Mosimann PJ, Jung S, Arnold M, Heldner MR, Michel P, Hajdu SD, Ribo M, Requena M, Maegerlein C, Friedrich B, Costalat V, Benali A, Pierot L, Gawlitza M, Schaafsma J, Pereira VM, Gralla J, Fischer U. Outcome, efficacy and safety of endovascular thrombectomy in ischaemic stroke according to time to reperfusion: data from a multicentre registry. Ther Adv Neurol Disord. 2019;12:1756286419835708. doi: 10.1177/1756286419835708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jahan R, Saver JL, Schwamm LH, Fonarow GC, Liang L, Matsouaka RA, Xian Y, Holmes DN, Peterson ED, Yavagal D, Smith EE. Association Between Time to Treatment With Endovascular Reperfusion Therapy and Outcomes in Patients With Acute Ischemic Stroke Treated in Clinical Practice. JAMA. 2019;322:252–263. doi: 10.1001/jama.2019.8286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaesmacher J, Ospel JM, Meinel TR, Boulouis G, Goyal M, Campbell BCV, Fiehler J, Gralla J, Fischer U. Thrombolysis in Cerebral Infarction 2b Reperfusions: To Treat or to Stop? Stroke. 2020;51:3461–3471. doi: 10.1161/STROKEAHA.120.030157. [DOI] [PubMed] [Google Scholar]
- 23.Alawieh A, Starke RM, Chatterjee AR, Turk A, De Leacy R, Rai AT, Fargen K, Kan P, Singh J, Vilella L, Nascimento FA, Dumont TM, McCarthy D, Spiotta AM. Outcomes of endovascular thrombectomy in the elderly: a ‘real-world’ multicenter study. J Neurointerv Surg. 2019;11:545–553. doi: 10.1136/neurintsurg-2018-014289. [DOI] [PubMed] [Google Scholar]
- 24.Saposnik G, Cote R, Phillips S, Gubitz G, Bayer N, Minuk J, Black S, Stroke Outcome Research Canada (SORCan) Working Group Stroke outcome in those over 80: a multicenter cohort study across Canada. Stroke. 2008;39:2310–2317. doi: 10.1161/STROKEAHA.107.511402. [DOI] [PubMed] [Google Scholar]
- 25.Kleine JF, Boeckh-Behrens T, Prothmann S, Zimmer C, Liebig T. Discrepancy between early neurological course and mid-term outcome in older stroke patients after mechanical thrombectomy. J Neurointerv Surg. 2016;8:671–676. doi: 10.1136/neurintsurg-2015-011702. [DOI] [PubMed] [Google Scholar]
- 26.Vagal A, Aviv R, Sucharew H, Reddy M, Hou Q, Michel P, Jovin T, Tomsick T, Wintermark M, Khatri P. Collateral Clock Is More Important Than Time Clock for Tissue Fate. Stroke. 2018;49:2102–2107. doi: 10.1161/STROKEAHA.118.021484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derraz I, Pou M, Labreuche J, Legrand L, Soize S, Tisserand M, Rosso C, Piotin M, Boulouis G, Oppenheim C, Naggara O, Bracard S, Clarençon F, Lapergue B, Bourcier R, ASTER and the THRACE Trials Investigators Clot Burden Score and Collateral Status and Their Impact on Functional Outcome in Acute Ischemic Stroke. AJNR Am J Neuroradiol. 2021;42:42–48. doi: 10.3174/ajnr.A6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russo R, Del Sette B, Mizutani K, Coskun O, Di Maria F, Lapergue B, Wang A, Bergui M, Rodesch G, Consoli A. Mechanical Thrombectomy in Distal Residual Occlusions of the Middle Cerebral Artery after Large Vessel Recanalization in Acute Stroke: 2b or not 2b? A Pragmatic Approach in Real-Life Scenarios. World Neurosurg. 2021;151:e793–e802. doi: 10.1016/j.wneu.2021.04.127. [DOI] [PubMed] [Google Scholar]
- 29.Kaesmacher J, Maegerlein C, Zibold F, Wunderlich S, Zimmer C, Friedrich B. Improving mTICI2b reperfusion to mTICI2c/3 reperfusions: A retrospective observational study assessing technical feasibility, safety and clinical efficacy. Eur Radiol. 2018;28:274–282. doi: 10.1007/s00330-017-4928-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.