Abstract
Introduction and importance
Brachiocephalic fistula, an arteriovenous fistula approach for hemodialysis in Chronic Kidney Disease patients, can cause various complications. Pseudoaneurysm in the venous end of the arteriovenous fistula is one of those unusual presentations, and can lead to the failure of vascular access.
Case presentation
We present a case of a 38-year-old female with pseudoaneurysm in the venous end of the left brachiocephalic fistula presenting as painless swelling for one month. Surgical management was done with excision followed by aneurysmorrhaphy.
Clinical discussion
The repair is associated with risks of arteriovenous fistula failure, thromboembolism, bleeding manifestation and graft rupture. Surgical correction should be done as early as possible with consideration of size, location, and available resources.
Conclusion
Venous pseudoaneurysm in a brachiocephalic fistula is an unusual complication which requires prompt surgical correction.
Keywords: Case report, Arteriovenous fistula, Hemodialysis, Pseudoaneurysm
Highlights
-
•
Pseudoaneurysm in the venous end of the brachiocephalic fistula is an unusual presentation.
-
•
Surgical repair of pseudoaneurysm is associated with more complications.
-
•
Case of successful surgical management of pseudoaneurysm by excision and aneurysmorrhaphy
1. Introduction
Hemodialysis treatment using vascular access is the most commonly used renal replacement therapy for patients with chronic kidney disease [1]. Brachiocephalic fistula is one of the approaches to placement of fistula for hemodialysis [1]. Venous pseudoaneurysm is a rare complication following arteriovenous fistula and is characterized by the formation of extravascular hematoma following vessel wall defect due to repeated needle puncture which can be diagnosed with help of Doppler ultrasonography and computed tomography (CT) angiogram [2], [3]. Pseudoaneurysm can occur due to any therapeutic or diagnostic vascular intervention, intravenous drug use, vascular trauma and infections [4].
Here we report a case of a 38-year-old female with venous pseudoaneurysm of left brachiocephalic fistula who presented to our tertiary care center and was treated with excision and aneurysmorrhaphy, which, based on literature review, is being reported for the first time from Nepal. This report highlights the identification and management of venous pseudoaneurysm amidst financial constraints and limited resources which is an emergent surgical problem. However, literatures on venous pseudoaneurysm remain scarce to this date which warrants the need for higher studies to identify the risk factors, guide prevention measures and ameliorate the management of this condition. The article has been written in line with SCARE Guideline 2020 [5].
2. Presentation of case
A 38-year-old female presented to Dhulikhel hospital with painless progressive swelling over the left upper arm for 1 month. She was a known case of hypertension and bilateral kidney failure under dialysis via brachiocephalic fistula with anastomosis in the cubital region for three years. On local examination, a soft non-tender pulsatile mass of 3 × 3 cm was present over the medial aspect of the left upper arm (Fig. 1). There were multiple marks due to repeated punctures during dialysis.
Fig. 1.
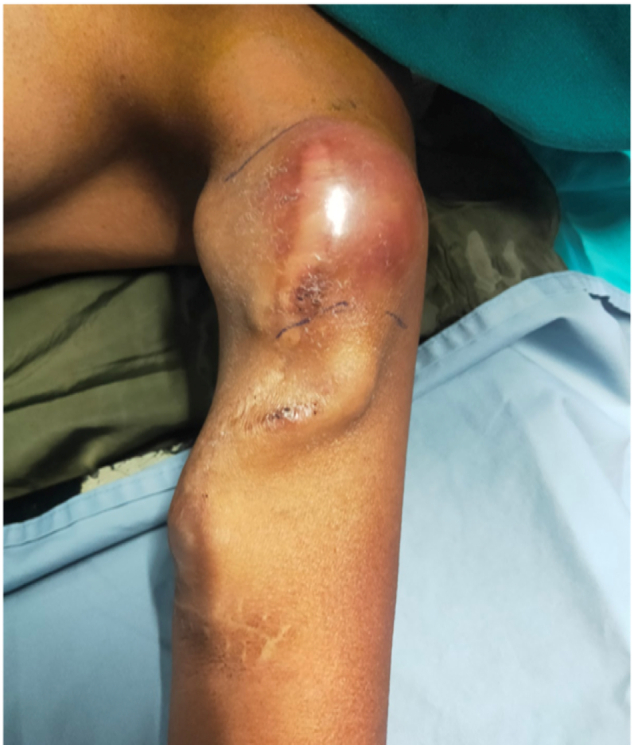
Swelling of 3 × 3 cm over the medial aspect of the left upper arm.
Preoperatively we did doppler ultrasonography which showed aneurysm originating from cephalic vein. The brachial artery was normal. The finding was consistent with the intraoperative picture. Thus we labelled the case as venous pseudoaneurysm.
Her laboratory workup was unremarkable and within the normal limits. However, serology revealed reactivity to HBsAg. Doppler ultrasonography revealed a pseudoaneurysm in the left arm of size 3 × 3 cm arising from the cephalic vein with typical Ying Yang sign. The brachial artery was normal.
Based on these findings, a diagnosis of brachiocephalic fistula with pseudoaneurysm was made.
As the pseudoaneurysm led to difficulty in cannulation, the patient was scheduled for surgical management by a team of experienced vascular surgeons. She underwent surgery for excision of pseudoaneurysm and repair under brachial plexus block. An incision was made of about 5 cm in the left cubital fossa. Brachial artery and cephalic vein were identified. Operative findings revealed a pseudoaneurysm of size 3 × 3 cm arising from the cephalic vein which confirmed diagnosis made by doppler ultrasonography. There was a rent of about 0.5 cm in the cephalic vein. Excision of the pseudoaneurysm was done and the rent in the cephalic vein was repaired. The residual cephalic vein was left in situ. However, during the postoperative period, thrombosis of the cephalic vein was noted after which the fistula could not be used for dialysis. A permanent catheter was kept for hemodialysis. No further complications were noted and the patient was discharged on the fifth postoperative day. The patient was then regularly followed up for 4 months with no new complaints (Fig. 2, Fig. 3, Fig. 4).
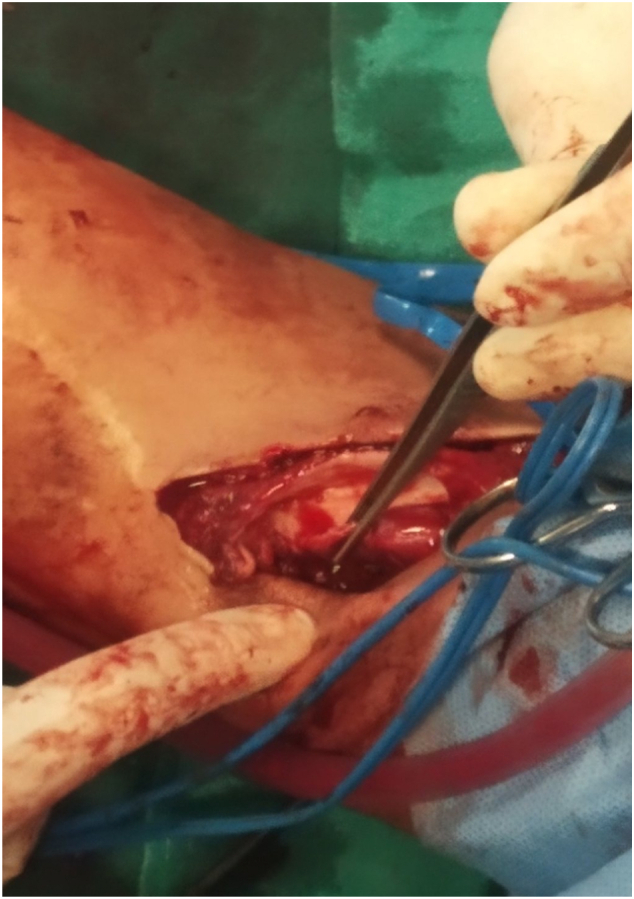
Fig. 2.

Pseudoaneurysm being visualized after incision of the skin and subcutaneous tissue.
Fig. 3.
Pseudoaneurysm during aneurysmorrhaphy.
Fig. 4.
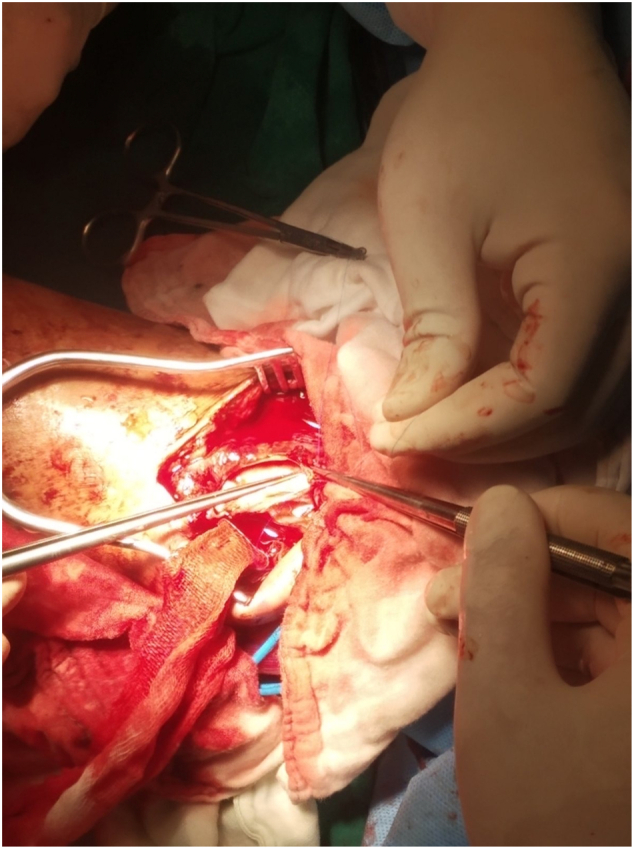
Pseudoaneurysm during aneurysmorrhaphy being closed.
3. Discussion
Hemodialysis patients require a fistula to function as a circuit to aid the kidney's function to filter blood. Though Arteriovenous fistula (AVF) is the preferred approach for vascular access, however, these are linked with frequent complications like thromboembolism, edema, cardiac failure, aneurysm and pseudoaneurysm [6]. Pseudoaneurysm results from a vessel wall defect which leads to persistent bqlood leaks forming extravascular hematoma without endothelial lining [7], [8]. It is a rare complication which has an incidence of 0.05 % to 0.5 % in all diagnostic and therapeutic puncture operations [9].
It is rarer in the venous system because it is a low-pressure circulation that doesn't usually favor hematoma formation [10]. In our case, the pseudoaneurysm was formed in the cephalic vein rather than the brachial artery. The creation of the brachiocephalic fistula could have led to an increased blood flow and thus increased blood pressure in the cephalic vein downstream to the fistula site which may have resulted in the pseudoaneurysm formation at sites of cannulation where the vessel walls were weak [2], [3]. Our patient had multiple marks over the swelling due to repeated cannulations and there were no signs of infection. So this pseudoaneurysm is traumatic cause rather than infective. Whereas aneurysm may form as a result of dilatation of weakened vessels involving all vessel walls following repeated needlings [11]. It may also form as a result of high blood flow through a vessel or due to abnormal hemodynamics following stenoses of the vessel [12]. Sequelae of pseudoaneurysm in arteriovenous fistula include rupture, limitation in cannulation, and necrotization of overlying skin with secondary infections [3]. As veins downstream of an AV fistula are constantly exposed to arterial pressure, hemorrhage can be critical in a venous pseudoaneurysm [10].
Venous pseudoaneurysm, being rare, lacks evidence-based treatment [13]. Treatment modalities for pseudoaneurysm should be selected considering the size, location, accessibility, aetiology and availability of vascular intervention facilities [14]. Therefore, depending on the case, conservative management by ultrasound-guided compression and thrombin injection, endovascular stent and surgery are the various commonly taken approaches for the management [15]. Covered-stent grafts have also recently been used to treat pseudoaneurysms in some selected cases, saving patients from the morbidity of the surgery [16]. But there may be problems in cannulation over a stent if treated endovascularly and there may be complications like stent fracture and migration [3], [17]. Stent graft is also expensive for patients in our setting.
As the patient presented late with large pseudoaneurysm, so surgical excision and repair were attempted considering the available resources. Surgical treatment is associated with significant morbidity and complications like arteriovenous fistula failure, bleeding, thrombosis, and graft rupture [17]. Despite these complications, where the advanced facilities are not available, the most common method of treatment is surgical repair [18]. This highlights the need for the prevention of aneurysms and pseudoaneurysms, especially in low-income countries where proper resources to treat them are lacking. There are very limited studies implicating poor cannulation technique, repeated single-site needling, postprocedural anticoagulant therapy and unsupervised dialysis catheter insertion as risk factors for the development of pseudoaneurysm [1], [4]. Use of buttonhole technique for cannulations, ensuring proper cannulation technique and rotation of cannulation site are some of the ways recommended by some studies for prevention of aneurysm and pseudoaneurysm in dialysis access [1], [19]. But there is a need for further studies to establish effective ways of prevention.
Even if the lesion might appear salvagable there are chances that the fistula might be thrombosed. Thus, aneurysmorraphy in pseudoaneurysm might not always have a favourable outcome.
4. Conclusion
A brachiocephalic fistula is an approach for hemodialysis patients with renal pathology. Among the various complications, pseudoaneurysm at the venous end is a rare complication encountered in patients with arteriovenous fistulas. The literature regarding the prevention and management of venous pseudoaneurysm in AV fistula is limited. So there is a need for further study to establish proper prevention and treatment in such cases.
Sources of funding
No sources of funding.
Ethical approval
Patient anonymity is maintained throughout this manuscript, and consent was obtained for publication from the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
AC: Manuscript preparation, edit and review.
SA: Manuscript preparation, edit and review.
RMK: Concept, manuscript edit and review, performed the surgery and guarantor.
AL: Data collection, Obtaining consent from the patient, Manuscript review.
SP: manuscript edit and review.
SB: manuscript preparation, edit and review.
Research registration
N/A.
Guarantor
Dr. Robin Man Karmacharya.
Unit Chief, Cardiothoracic and Vascular Surgery Unit.
Department of Surgery.
Dhulikhel Hospital.
Dhulikhel, Kavre.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
All authors declare that they have no conflicts of interest.
References
- 1.Vascular Access 2006 Work Group Clinical practice guidelines for vascular access. Am. J. Kidney Dis. 2006;48(Suppl 1):S176–S247. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 2.Une D., Nakanishi K., Shimizu S., et al. Cephalic vein pseudoaneurysm after blunt trauma in a patient with arteriovenous fistula for hemodialysis. Circ. Control. 2014;35:232–234. [Google Scholar]
- 3.Kershen L.M., Marichal D.A. Endovascular treatment of stent fracture and pseudoaneurysm formation in arteriovenous fistula dialysis access. Proc. 2013;26:47–49. doi: 10.1080/08998280.2013.11928916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaiswal L.S., Pandit N., Prasad J.N., et al. Pseudoaneurysm of peripheral arteries: our experience in a community-based hospital. Indian J. Vasc. Endovasc. Surg. 2019;6:102. [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Zibari G.B., Rohr M.S., Landreneau M.D., et al. Complications from permanent hemodialysis vascular access. Surgery. 1988;104:681–686. [PubMed] [Google Scholar]
- 7.Schatz I.J., Fine G. Venous aneurysms. N. Engl. J. Med. 1962;266:1310–1312. doi: 10.1056/NEJM196206212662505. [DOI] [PubMed] [Google Scholar]
- 8.Deşer S.B. Management of iatrogenic brachial artery pseudoaneurysm. Int.J. Cardiovasc. Acad. 2017;3:9–10. [Google Scholar]
- 9.Kresowik T.F., Khoury M.D., Miller B.V., et al. A prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplasty. J. Vasc. Surg. 1991;13:328–333. discussion 333–5. [PubMed] [Google Scholar]
- 10.Min S.I., Jung I.M., Chung J.K., et al. A nontraumatic, noniatrogenic pseudoaneurysm of the cephalic vein presenting as an upper arm mass. Ann. Vasc. Surg. 2008;22:575–578. doi: 10.1016/j.avsg.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Mudoni A., Cornacchiari M., Gallieni M., et al. Aneurysms and pseudoaneurysms in dialysis access. Clin. Kidney J. 2015;8:363–367. doi: 10.1093/ckj/sfv042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajput A., Rajan D.K., Simons M.E., et al. Venous aneurysms in autogenous hemodialysis fistulas: is there an association with venous outflow stenosis. J. Vasc. Access. 2013;14:126–130. doi: 10.5301/jva.5000111. [DOI] [PubMed] [Google Scholar]
- 13.Lyons W., Harfouche M., Lopez J. Conservative management of a traumatic common iliac venous pseudoaneurysm: a case report. J. Surg. Case Rep. 2017;2017 doi: 10.1093/jscr/rjx085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang A., Silberzweig J.E. Brachial artery pseudoaneurysms caused by inadvertent hemodialysis access needle punctures. Am. J. Kidney Dis. 2009;53:351–354. doi: 10.1053/j.ajkd.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Yildirim S., Nursal T.Z., Yildirim T., et al. Brachial artery pseudoaneurysm: a rare complication after haemodialysis therapy. Acta Chir. Belg. 2005;105:190–193. [PubMed] [Google Scholar]
- 16.Shah A.S., Valdes J., Charlton-Ouw K.M., et al. Endovascular treatment of hemodialysis access pseudoaneurysms. J. Vasc. Surg. 2012;55:1058–1062. doi: 10.1016/j.jvs.2011.10.126. [DOI] [PubMed] [Google Scholar]
- 17.Belli S., Parlakgumus A., Colakoglu T., et al. Surgical treatment modalities for complicated aneurysms and pseudoaneurysms of arteriovenous fistulas. J. Vasc. Access. 2012;13:438–445. doi: 10.5301/jva.5000077. [DOI] [PubMed] [Google Scholar]
- 18.Darbari A., Tandon S., Chandra G., et al. Post-traumatic peripheral arterial pseudoaneurysms: our experience. Indian J. Thoracic Cardiovasc. Surg. 2006;22:182–187. [Google Scholar]
- 19.van Loon M.M., Goovaerts T., Kessels A.G.H., et al. Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol. Dial. Transplant. 2010;25:225–230. doi: 10.1093/ndt/gfp420. [DOI] [PubMed] [Google Scholar]


