Abstract
A 50-year-old male underwent thoracic endovascular aortic repair (TEVAR) for distal arch traumatic aortic dissection. Following placement of a Najuta endograft (Kawasumi Laboratories, Inc., Tokyo, Japan) from zone 0 to zone 4, patency of the three vessels was confirmed. Later, the patient suddenly experienced complete intermittent loss of motor and sensory functions in the bilateral lower extremities. Contrast computed tomography (CT) findings indicated endograft stenosis. Following an additional TEVAR procedure, the paraparesis state was temporarily improved. Thereafter, he was readmitted due to congestive heart failure with intermittent paraparesis and contrast CT findings indicated endograft collapse. An emergency procedure for re-expansion of the collapsed endograft and urgent surgery for replacement of the aortic arch was successful. In cases with intermittent paraparesis, endograft collapse should be considered.
Keywords: Najuta endograft, Collapse, Paraparesis
Introduction
A rare, though well-known, complication of thoracic endovascular aortic repair (TEVAR) is thoracic endograft collapse, which is most often seen following treatment for traumatic aortic lesions. The majority of cases are asymptomatic, though such a collapse may induce reperfusion of the injured aortic segment or distal organ malperfusion, or both [1]. In the present case, symptomatic thoracic endograft collapse occurred 180 and 270 days following a TEVAR procedure for traumatic aortic dissection, which resulted in neurologic deficits in the bilateral lower extremities. Redo TEVAR was performed, followed by an open conversion procedure, which were successful.
Case report
A traumatic type B thoracic aortic dissection (DeBakey type III) occurred in a 50-year-old male after a falling accident 2 years prior. Routine follow-up chest computed tomography (CT) examination findings revealed a distal arch aortic dissecting aneurysm showing a tendency for expansion (maximum diameter increasing from 37 to 45 mm in a 6-month period). In coronary CT images, no evidence of stenosis was seen, while echocardiography showed good wall motion and no valvular pathology. Cerebral imaging of the cerebrovascular and neck vessels also provided no evidence of an anomaly or stenosis. Based on those findings, we recommended open arch surgery, though stent graft treatment was ultimately planned, even though it would be an off-label use, based on the strong desire of the patient. Preparations were made under the following conditions: (1) the stent graft device would be placed in a healthy zone landing site in the central area and (2) the operation would be changed to open thoracic surgery, if major complications occurred.
A TEVAR procedure was performed using a Najuta fenestrated endograft (Kawasumi Laboratories, Inc., Tokyo, Japan) in order to maintain patency of the arch vessels. The proximal neck length between the left subclavian artery and entry of dissection was measured at 12.6 mm, based on the assumption of using a fenestrated endograft. Proximally, the diameter of the aorta was approximately 25 mm (ascending aorta), while distally that was 18 mm (descending aorta, true lumen) (Fig. 1).
Fig. 1.
Computed tomography image showing distal arch aortic dissecting aneurysm
Operation 1: A Najuta fenestrated endograft 28-24-174 was placed from zone 0 to zone 4 using a pull-through method with patency of the neck vessels established. We also confirmed dissipation of the bloodstream to a false cavity and brain blood flow was secured. Postoperative contrast CT findings showed no evidence of an endoleak and the patient was discharged at 1 week after the operation. At 180 days after the procedure, the patient was brought to the emergency room from his workplace for sudden and complete intermittent loss of motor and sensory functions in the bilateral lower extremities (intermittent paraparesis). Contrast CT findings showed no evidence of an endoleak, while graft stenosis in the aortic isthmus site was revealed (Fig. 2a).
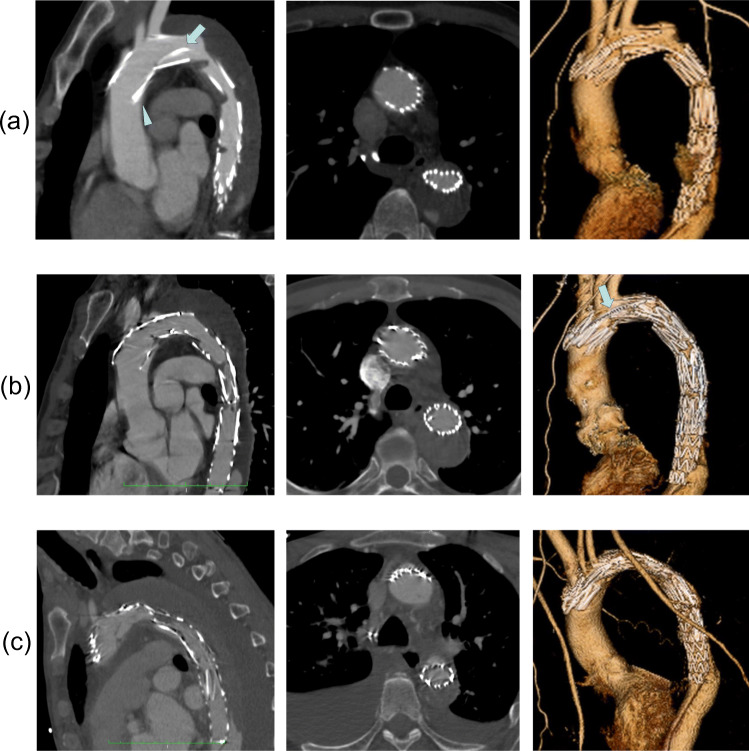
Fig. 2.
a Computed tomography images obtained after TEVAR confirming proper positioning of the device, no evidence of an endoleak, and patency of the three vessels. However, graft stenosis in the aortic isthmus site was noted. Triangle shape indicates wedge defect by bird beak phenomenon. Arrow indicates a fin used to stabilize the central side stent. b Computed tomography images showing results of additional TEVAR procedure with a Valiant stent placed in area with stenosis as well as confirmation of bloodstream improvement. However, bird-beak phenomenon was expanding. Arrow indicates fin pushing through to lesser curvature side. c Computed tomography images obtained at re-admission showing proximal endograft collapse
Operation 2: A Valiant Navion graft 22-22-94 (Medtronic Inc., Minneapolis, Minn, USA) was placed in the stenosis portion and bloodstream improvement was confirmed (Fig. 2b). Simultaneously, symptoms also improved without performing cerebrospinal fluid (CSF) drainage. The patient was readmitted due to congestive heart failure at 83 days after the second TEVAR (270 days after first TEVAR), with a rapidly increased brain natriuretic peptide (BNP) level and orthopnea was also noted. Furthermore, intermittent paraparesis, as seen previously, was again indicated. Contrast CT showed the two proximal stents with the Najuta endograft proximal edge as well as collapse of the thoracic aortic stent graft, while the Valiant Navion graft remained intact (Fig. 2c), and no evidence showing thromboembolism or abdominal organ ischemic injury was noted. Findings of acute heart failure indicated impaired circulation throughout the whole body, as shown by the sudden increase in afterload.
Operation 3: A salvage procedure, as endovascular intervention for re-expansion of the collapsed stent graft, was performed, including re-expansion ballooning with a Reliant balloon catheter (Medtronic, Minneapolis, Minnesota, USA). Expansion was readily obtained and the circulation system showed improvement, with the paraparesis symptom resolving without CSF drainage.
Operation 4: This patient had only undergone ballooning re-expansion; thus, there was concern regarding possible recurrence of collapse. The pathology of the recurrent events seemed to be potentially fatal. He remained under management in the intensive care unit for 5 days, after which a radical graft replacement operation was performed following improvement of heart failure.
A median sternotomy was performed with open removal of the stent graft and graft repair of the aortic arch using a J Graft FROZENIX open stent (Japan Lifeline Co., Ltd., Tokyo, Japan). The extracted Najuta stent graft was examined, though no damage to the frame or graft was evident. Postoperative CT findings confirmed patency of the grafts and no endoleak (Fig. 3). The patient showed a good recovery and was discharged on day 12.
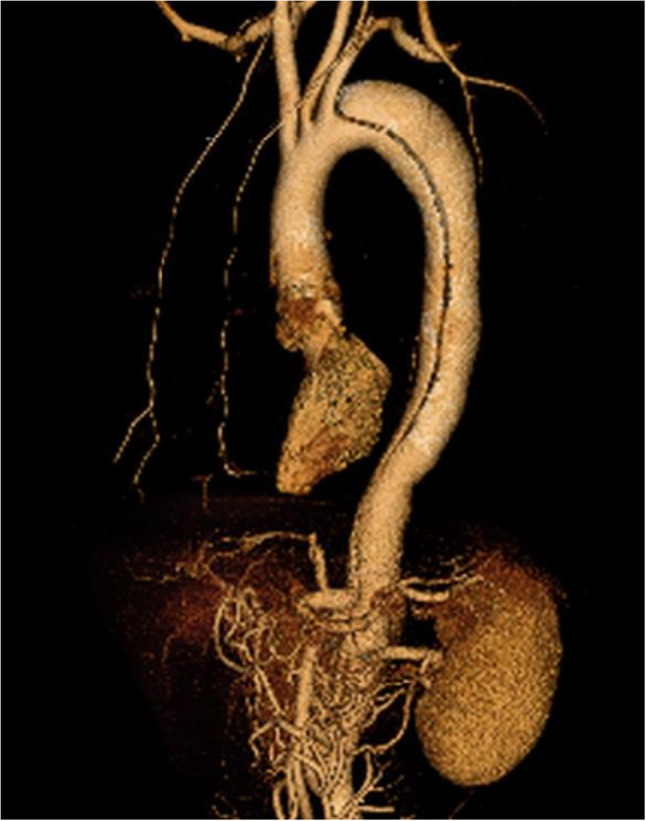
Fig. 3.

Replacement of the arch was performed 5 days after emergency re-expansion of the collapsed endograft
Discussion
A rare complication following TEVAR is occlusion of the stent graft, and rapid treatment is crucial to resolve organ and tissue malperfusion resulting from such a catastrophic event [2]. More common following a TEVAR procedure is endograft collapse, especially in patients treated for traumatic aortic dissection, with a rate of incidence difficult to estimate, though considered to range from 1.4 to 19% based on previous case series reports [2, 3]. Various factors are related to such occurrence. For example, acute aortic arch angulation and reduced aortic diameter as morphological characteristics in non-elderly trauma cases, such as the present, as well as a lack of endografts available that have been designed for such possibilities can lead to excess oversizing and also improper positioning in relation with the arch, in combination with hemodynamic forces affecting the aortic arch and predisposing conditions, resulting in endograft collapse [3–5]. Additionally, findings indicating physiologic coarctation of the aorta with distally located malperfusion syndrome may be noted in cases with partial occlusion of the aorta [6]. In rare cases, including the present, the patient may intermittently demonstrate complete acute motor and sensory loss in the lower limbs. We performed enhanced CT, though observation of a patent endograft could not be obtained because of the pathology of intermittent collapse. In consideration of the progress of the pathology, an endograft device was expected to be capable of dealing with both closed and patent conditions. Should intermittent symptoms, such as those seen in our patient, be encountered, endograft collapse phenomenon must be considered.
While the Najuta stent graft is regarded as a creative device, additional understanding of its characteristics is necessary for avoiding problems such as those encountered in our patient. The graft device is an endoskeleton and includes a structure characterized as a fin on the lesser curvature side for the purpose of stabilization of the central side stent. Furthermore, the device is custom designed and manufactured for individual patients based on a three-dimensional (3D) model of the aortic arch. The custom model is used for producing a physical plaster model. Its size is approximately 8–10% greater than the diameter of the native aorta.
In cases of chronic dissection, the false lumen appears to remain pressurized, such as seen in the present case. False lumen embolization is an important endovascular adjunct to TEVAR for promotion of reverse aortic remodeling in select patients with chronic aortic dissection and persistent retrograde false lumen perfusion [7]. Therefore, it is important to confirm that the primary entry occlusion procedure has been performed correctly with no endoleak or complications.
The Najuta stent graft enables accurate deployment and may prevent migration, while it is also possible to obtain a long proximal sealing length because of its fenestration. Moreover, the 3D skeleton of the Najuta is a pre-shaped and rigid structure, and all Z-stents are linked with two struts. Therefore, it is able to fit the greater curvature of the aortic arch and function well. On the other hand, the Najuta has no Z-stent between the first and second stents. To support sealing force in this part, we frequently perform pressure bonding of the balloon.
In the present case, during the first operation, a radiological examination detected a so-called bird-beak configuration in the stent graft at the lesser curvature of the ascending aorta, which indicated a wedge-shaped gap between the undersurface of the stent graft and aortic wall. In the second operation, the fin was observed to be pushed to the lesser curvature side because of being detained by the Valiant Navion system as the lining of the Najuta stent, which resulted in the greater curvature side pushing the central edge of the Najuta to a greater degree. Thus, it was considered that an increase in the bird-beak phenomenon on the lesser curvature side might have contributed to the collapse. When insertion of an additional stent-graft device into a Najuta device is decided, traumatic aortic dissection must be considered as a possible resulting condition, particularly in non-elderly patients.
Conclusion
In patients with intermittent paraparesis, endograft collapse phenomenon should be considered. Should stent graft collapse be revealed in subsequent workup findings, then a suitable correction method must be performed based on imaging findings.
Author contribution
Study conception: TN, YN. Data collection: TN, DY. Writing: TN. Critical review and revision: all authors. Final approval of the article: all authors. Accountability for all aspects of the work: all authors.
Funding
None.
Declarations
Ethical approval
Not applicable.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interest
The authors declare that they have no competing interests.
Statement of human and animal rights
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shukla AJ, Jeyabalan G, Cho J-S. Late collapse of a thoracic endoprosthesis. J Vasc Surg. 2011;53:798–801. doi: 10.1016/j.jvs.2010.10.058. [DOI] [PubMed] [Google Scholar]
- 2.Hinchliffe RJ, Krasznai A, Schultzekool L, et al. Observations on the failure of stent-grafts in the aortic arch. Eur J Vasc Endovasc Surg. 2007;34:451–456. doi: 10.1016/j.ejvs.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Makaroun MS, Dillavou ED, Wheatley GH, Cambria RP. Five-year results of endovascular treatment with the Gore TAG device compared with open repair of thoracic aortic aneurysms. J Vasc Surg. 2008;47:912–918. doi: 10.1016/j.jvs.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Ueda T, Fleischmann D, Dake MD, Rubin GD, Sze DY. Incomplete endograft apposition to the aortic arch: bird-beak configuration increases risk of endoleak formation after thoracic endovascular aortic repair. Radiology. 2010;255:645–652. doi: 10.1148/radiol.10091468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canaud L, Alric P, Desgranges P, Marzelle J, Marty-Ane C, Becquemin J-P. Factors favoring stent-graft collapse after thoracic endovascular aortic repair. J Thorac Cardiovasc Surg. 2010;139:1153–1157. doi: 10.1016/j.jtcvs.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Go MR, Siegenthaler MP, Rhee RY, Gupta N, Makaroun MS, Cho J-S. Physiologic coarctation of the aorta resulting from proximal protrusion of thoracic aortic stent grafts into the arch. J Vasc Surg. 2008;48:1007–1011. doi: 10.1016/j.jvs.2008.05.027. [DOI] [PubMed] [Google Scholar]
- 7.Miletic KG, Kindzelski BA, Hodges KE, et al. Impact of endovascular false lumen embolization on thoracic aortic remodeling in chronic dissection. Ann Thorac Surg. 2021;111:495–501. doi: 10.1016/j.athoracsur.2020.04.093. [DOI] [PubMed] [Google Scholar]