Abstract
Purpose: The consumption of drugs during pregnancy without medical advice constitutes a risk for the mother and the fetus. It is a public health problem. This study aimed to assess self-medication practices among pregnant women, the most used medicines, and factors associated with this practice.
Methods: A cross-sectional study was conducted using a structured questionnaire on pregnant women who were attending Settat health centers. A simple random sampling technique was used to select the study participants. Descriptive and inferential statistics were computed using the SPSS version 19.
Results: Among 364 pregnant women, 118 (32%) practiced self-medication in modern medicine. Paracetamol was the most used medication, and nausea and vomiting were the most frequent symptoms reported by self-medicated pregnant women. Multivariate logistic regression analysis showed that women over 30 years old were four-fold more likely to practice self-medication than the other groups [AOR: 4.19; 95% CI (1.80–9.77)]. Similarly, unemployed women [AOR: 3.93; 95% CI (0.80–19.23)], those in third trimester [AOR: 2.63; 95% CI (1.29–5.36)], multiparous [AOR: 6.03; 95% CI (3.12–11.65)], without chronic illness [AOR: 2.84; 95% CI (1.26–6.41)], without therapeutic treatment [AOR: 10.1; 95% CI (2.81–37.03)] and who have attended ANC at least once, were more likely to practice self-medication than the other groups.
Conclusion: The prevalence of modern drug self-medication among pregnant women in Morocco is classified as lower. Health professionals can exert positive pressure through education and information provided during ANC about OTC medications to significantly reduce the rate of self-medication.
Keywords: pregnancy, self-medication, modern drug, OTC medication, maternal and child health
Introduction
Self-medication is defined as the use of medication to treat self-diagnosed disorders or symptoms or the intermittent or continuous use of prescribed medication for chronic or recurring illnesses or symptoms (World Health Organization, 2000). This practice is widespread in the world, and its overall estimated prevalence was 32% (Mohseni et al., 2018). Several studies have shown that self-medication is very common in countries with limited resources, such as African countries. There, people use both over-the-counter and prescription drugs without supervision (Afolabi, 2008; Aziz et al., 2018; Marwa et al., 2018). What makes the difference between countries is mainly differences in health policy, access to care, and regulation of drug distribution (Branthwaite and Pechère, 1996).
Many studies have shown an association between self-medication and socio-demographic, cultural, and economic characteristics (Subashini and Udayanga, 2020; Zeid and al., 2020). Morocco is one of the developing countries where the prevalence of self-medication is 69%, of which 64.3% is represented by women in general (Oirdi et al., 2015). Very few studies have evaluated self-medication in Morocco, but none have studied self-medication among pregnant women.
Pregnant women are one of the vulnerable population groups practicing the two forms of self-medication (90%), either over-the-counter (OTC) or prescribed medications. Furthermore, studies have shown that up to 10% of birth defects (low birth weight, premature birth, feeding problems, respiratory problems, malformations, and developmental fetal toxicity) are directly linked to maternal drug exposure (Stanley et al., 2019).
In fact, as far as the drugs are concerned, some of them have been documented as safe for use during pregnancy. However, research cannot describe all the drugs used by pregnant women in self-medication for ethical concerns. Thus, in 2015, the United State Food and Drug Administration (US-FDA) implemented the Pregnancy Lactation Labeling Rule (PLLR), which requires reformulation of the content and format of drug packaging. This reformulation included a descriptive summary of the risks associated with the use of medications during pregnancy and lactation. The US-FDA authorizes a drug product based on clinical trial data using controlled groups, random assignment of participants to groups, techniques to minimize bias, and defined criteria to measure outcomes. For pregnant women, the safety of a drug means that the drug is not known to be embryonical, teratogenic, or fetotoxic, and indicates that the drug is safe for the woman herself (Food and Drug Administration, 2014; United States Food and Drug Administration, 2015).
To overcome all kinds of disorders caused by self-medication during pregnancy, health professionals involved in prenatal surveillance (general practitioners, gynecologists–obstetricians, and midwives) must have a role in preventing these risks through monitoring and raising awareness. Thus, the information provided by health professionals is a decisive lever in the prevention of risks due to self-medication (Haute Autorité de Santé, 2007).
Material and methods
General context of the study
The reduction of maternal and neonatal morbidity and mortality is among the goals of the international community. In Morocco, the maternal mortality ratio has decreased from 227 deaths per 100,000 live births in 2004 to 72.6 per 100,000 births in 2018. It is twice as high in rural areas (111 per 100,000 births) than in urban areas (45 per 100,000). This progress is explained, in part, by improved prenatal care. The latter makes it possible to assess and anticipate possible risks to future pregnancy, such as exposure to occupational and lifestyle risks, including nutrition and self-medication (ENPSF, 2018).
Study design and setting
A facility-based cross-sectional study was conducted to assess self-medication among pregnant women who were attending ANC at the seven Settat's health centers between January and July 2019. Settat, a Moroccan city located in the Casablanca-Settat region, is the capital of the province of Settat. In 2020, the population of Settat city reached 159,002 inhabitants. The city’s health infrastructure comprises a provincial hospital (Hassan II Hospital) and seven primary health centers (Haut Commissariat au Plan (HCP), 2018). These centers are state facilities offering free services to the city’s population. They provide primary health care and contain a maternal and child health service, where prenatal consultations are performed.
Population and inclusion and exclusion criteria
All pregnant women who had ANC follow-up in one of Settat’s health centers were the source population. Pregnant women of any gestational age who came during the study period were included in this study. Pregnant women who were unable to hear or communicate and those who had given birth and were unwilling to provide consent were excluded from the study.
Sampling procedure
Before starting the study, we contacted all seven health centers. Each center informed us of the number of pregnant women coming for ANC. A list of contact information for pregnant women attending each health center was provided. The seven lists were compiled in an Excel file. In total, there were 3,900 women.
The sample size was estimated using the following single proportion formula:
Since no study has reported on modern drug self-medication among Moroccan pregnant women, we proposed the prevalence of self-medication, p = 50%. Considering a margin error of 5% and a confidence level of 95%, the minimum number of participants to be included in this study was n = 350. Expecting a 10% non-response rate, we interviewed a total of 384 pregnant women. The final sample size was set at 364 participants. The sampling was carried out by the simple random method using the function RANDBETWEEN (1; 3,900) to select the 384 women to be interviewed. We called these women by phone to schedule appointments with them during their subsequent visits.
Data collection
Data were collected using a structured questionnaire developed in French and translated into the Moroccan local dialect (Darija). The questionnaire was administered face-to-face by a single interviewer. A pre-test was carried out on 5% of the sample at the health center Al Kheir of Settat. The reliability of the questionnaire was also checked using Cronbach’s alpha test, and a value of 0.80 was obtained. The questionnaire included socio-demographic characteristics, obstetric factors, and self-medication practice. Regarding self-medication, women in the first trimester of their pregnancy answered the questions during this period, those in the second trimester answered the questions for the second and first trimesters, and those in the third trimester answered the questions concerning the three trimesters. The participants collaborated in our study on a voluntary basis. They provided their written consent form after they were assured of the anonymity of the questionnaires, the confidentiality of their data, and their right to withdraw at any time during the interviews. Data were collected for each pregnant woman, noted on copies of the questionnaire, and then transcribed in an Excel file which served as the basis for statistical analysis.
Statistical analysis
Data analysis was performed using Software Statistical Package for the Social Science (SPSS) version 19. Qualitative variables were presented as frequency and percentage. The dependent variable was the modern drug self-medication, and the independent variables were socio-demographic characteristics of pregnant women. The comparison between categorical variables and self-medication practice was analyzed using Fisher’s exact test and a Chi-square test. Multicollinearity was checked out to test correlation among associated variables using the variance inflation factor (VIF). Bivariate logistic regression analysis was used for examining the association between self-medication and socio-demographic characteristics. Variables with a p-value less than 0.05 were re-analyzed using a multivariable binary logistic regression model to identify the factors independently associated with modern drug self-medication practice during pregnancy. The strength of associations between each exposure variable and the dependent variable was measured by odds ratios (OR) with 95% confidence intervals (CIs) and statistical significance was set at p < 0.05.
Results
Socio-demographic characteristics
A total of 364 pregnant women met the inclusion criteria. Among them, 355 (97.5%) were married, and 180 (49.5%) were in the age range 20–30 years. Moreover, 344 (94.5%) participants were unemployed, 109 (29.9%) were illiterate, and 107 (29.4%) were on the primary level. Furthermore, 295 (81%) of the pregnant women had no chronic illness and 312 (85.7%) were not on any treatment (Table 1).
TABLE 1.
Socio-demographic and obstetrical characteristics and self-medication during pregnancy of 364 women, 2019.
| Characteristic | Self-medication | p-value | |||
|---|---|---|---|---|---|
| Total, N = 364 (%) | Yes, N = 118 (%) | No, N = 246 (%) | |||
| Age | 18–20 | 59 | 11 (9.3) | 48 (19.5) | <0.0001 |
| 20–30 | 180 | 44 (37.3) | 136 (55.3) | ||
| 30–45 | 125 | 63 (53.4) | 62 (25.2) | ||
| Residence | Urban | 364 | 118 | 246 | — |
| Rural | 0 | 0 | 0 | ||
| Education | College/University | 42 | 16 (13.6) | 26 (11.1) | 0.403 |
| Secondary school | 93 | 36 (30.8) | 57 (24.4) | ||
| Primary school | 107 | 34 (29.1) | 73 (31.2) | ||
| Illiterate | 109 | 31 (26.5) | 78 (33.3) | ||
| Occupation | Employed | 20 | 2 (1.7) | 18 (7.3) | 0.028 |
| Unemployed | 344 | 116 (98.3) | 228 (92.7) | ||
| Chronic illness | Yes | 69 | 11 (9.3) | 58 (23.6) | 0.001 |
| No | 295 | 107 (90.7) | 188 (76.4) | ||
| Therapeutic treatment | Yes | 52 | 3 (2.5) | 49 (19.9) | <0.0001 |
| No | 312 | 115 (97.5) | 197 (80.1) | ||
| Parity | Primiparous | 168 | 38 (32.2) | 130 (52.8) | <0.0001 |
| Second parous | 110 | 33 (28.0) | 77 (31.3) | ||
| Multiparous | 86 | 47 (39.8) | 39 (15.9) | ||
| Gestational age | First trimester | 80 | 20 (16.9) | 60 (24.3) | 0.01 |
| Second trimester | 157 | 44 (37.2) | 113 (45.9) | ||
| Third trimester | 127 | 54 (45.7) | 73 (29.6) | ||
| Previous ANC follow up | 0 ANC | 61 | 19 (16.1) | 14 (5.69) | 0.004 |
| 1–3 ANC | 97 | 32 (27.1) | 87 (35.3) | ||
| 4 ANC | 206 | 67 (56.7) | 145 (58.9) | ||
Obstetric factors
Nearly half 157 (43.1%) of the participants were in the second trimester of their pregnancy, and 168 (46.2%) participants were primiparous. About 206 (56.5%) of participants had a full ANC follow-up in their previous pregnancy. The reasons for the lack of ANC follow-up were mainly financial and logistical resources 168 (46.1%) (Table 1).
Modern drug self-medication
Globally, this study showed that modern drug self-medication is practiced during the pregnancy period by 118 (32%) women. Among them, 51 (43.2%) self-medicated during the first trimester, 24 (20.3%) only in the second trimester, and 43 (36.4%) in the third trimester.
The most common reason for practicing self-medication was time-saving 67 (48.6%), followed by an assumption that the disease was minor 36 (26.1%) (Figure 1).
FIGURE 1.
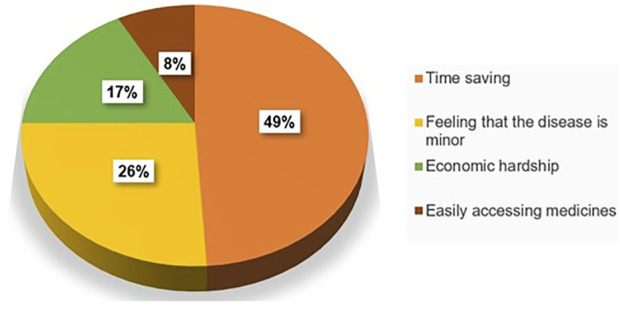
Self-medication reasons of study participants, 2019 (n = 118).
The common causes of self-medication were nausea and vomiting 83 (29.3%), headache 68 (24%), heartburn 67 (23.7%), and back and leg pain 65 (23%) (Table 2).
TABLE 2.
Characteristics of modern drug self-medication among pregnant women at Settat, 2019 (n = 118).
| Variables | Frequency (N) | Percentage (%) |
|---|---|---|
| Indication | ||
| Nausea/Vomiting | 83 | 70.3 |
| Headache | 68 | 57.6 |
| Heartburn | 67 | 56.7 |
| Back and leg pain | 65 | 55 |
| Constipation | 46 | 38.9 |
| Cough | 38 | 32.2 |
| Diarrhea | 17 | 14.4 |
| Hemorrhoids | 14 | 11.8 |
| Common drugs used for self-medication | ||
| Paracetamol | 34 | 28.8 |
| Ranitidine | 25 | 21.1 |
| Aspirin | 23 | 19.4 |
| Aluminum hydroxide/Magnesium hydroxide | 23 | 19.4 |
| Cough syrup/Pseudoephedrine hydrochloride | 22 | 18.6 |
| Sources of information | ||
| Pharmacist | 50 | 42.3 |
| Themselves | 40 | 33.8 |
| Family or friends | 28 | 23.7 |
As far as the drugs are concerned, 34 (28.8%) pregnant women self-administered paracetamol, 25 (21.1%) ranitidine, and 23 (19.4%) aspirin.
Among pregnant women who practice self-medication 118) with modern medicines during their current pregnancy, the most common sources of information were pharmacists 50 (42.3%) and by themselves 40 (33.8%) (Table 1).
Among the 364 participants, 227 (62.36%) were informed about the dangers and contraindications of self-medication during pregnancy.
Self-medication was associated with higher age (p < 0.0001), occupation (p = 0.028), chronic illness (p = 0.001), therapeutic treatment (p < 0.0001), parity (p < 0.0001), gestational age (p = 0.01), and previous ANC follow-up (p = 0.004).
Multivariate logistic regression analysis showed that women over 30 years old were four times more likely to practice self-medication than the other groups [AOR: 4, 19; 95% CI (1.80–9.77)]. Similarly, unemployed women [AOR: 3.93; 95% CI (0.80–19.23)], in third trimester [AOR: 2.63; 95% CI (1.29–5.36)], multiparous [AOR: 6.03; 95% CI (3.12–11.65)], without chronic illness [AOR: 2.84; 95% CI (1.26–6.41)], without therapeutic treatment [AOR: 10.1; 95% CI (2.81–37.03)] and who had attended ANC at least once were more likely to practice self-medication than the other groups (Table 3).
TABLE 3.
Factors associated with modern drug self-medication of study participants, 2019 (n = 364).
| Characteristic | Self-medication | COR [95% CI] | p-value | AOR [95% CI] | p-value | |
|---|---|---|---|---|---|---|
| Yes (%) | No (%) | |||||
| Age | ||||||
| < 20 | 11 (9.3) | 48 (19.5) | 1.00 | — | 1.00 | — |
| 20–30 | 44 (37.3) | 136 (55.3) | 1.41 [0.67–2.95] | 0.358 | 1.35 [0.59–3.12] | 0.47 |
| > 30 | 63 (53.4) | 62 (25.2) | 4.43 [2.11–9.32] | <0.0001 | 4.19 [1.80–9.77] | 0.001 |
| Occupation | ||||||
| Employed | 2 (1.7) | 18 (7.3) | 1.00 | — | 1.00 | — |
| Unemployed | 116 (98.3) | 228 (92.7) | 4.58 [1.05–20.07] | 0.028 | 3.93 [0.80–19.23] | 0.091 |
| Chronic illness | ||||||
| Yes | 11 (9.3) | 58 (23.6) | 1.00 | — | 1.00 | — |
| No | 107 (90.7) | 188 (76.4) | 3.00 [1.51–5.96] | 0.001 | 2.84 [1.26–6.41] | 0.011 |
| Therapeutic treatment | ||||||
| Yes | 3 (2.5) | 49 (19.9) | 1.00 | — | 1.00 | — |
| No | 115 (97.5) | 197 (80.1) | 9.53 [2.91–31.28] | <0.0001 | 10.1 [2.81–37.03] | <0.0001 |
| Parity | ||||||
| 1 | 38 (32.2) | 130 (52.8) | 1.00 | — | 1.00 | — |
| 2 | 33 (28.0) | 77 (31.3) | 1.46 [0.85–2.53] | 0.168 | 1.73 [0.92–3.23] | 0.124 |
| ≥ 3 | 47 (39.8) | 39 (15.9) | 4.12 [2.36–7.20] | <0.0001 | 6.03 [3.12–11.65] | <0.0001 |
| Gestational age | ||||||
| 1st trimester | 20 (16.9) | 60 (24.3) | 1.00 | 1.00 | — | |
| 2nd trimester | 44 (37.2) | 113 (45.9) | 1.17 [0.63–2.16] | 0.620 | 1.22 [0.61–2.48] | 0.571 |
| 3rd trimester | 54 (45.7) | 73 (29.6) | 2.22 [1.20–4.11] | 0.011 | 2.63 [1.29–5.36] | 0.008 |
| Previous ANC follow up | ||||||
| 0 ANC | 19 (16.1) | 14 (5.69) | 1.00 | 1.00 | — | |
| 1–3 ANC | 32 (27.1) | 87 (35.3) | 0.27 [0.12–0.60] | 0.001 | 0.22 [0.09–0.57] | 0.002 |
| 4 ANC | 67 (56.7) | 145 (58.9) | 0.34 [0.16–0.72] | 0.005 | 0.32 [0.13–0.77] | 0.011 |
COR: crude odds ratio; AAR: adjusted odds ratio; CI: confidence interval. Significant p values (p < 0.05) are in bold.
Discussion
This study was conducted to assess the practice of conventional medicine self-medication and associated factors regarding pregnant women attending ANC at Moroccan health centers. As a matter of fact, more than half participants had a full ANC follow-up in their previous pregnancy. The main constraints for avoiding ANC follow-up for the total group were lack of financial and logistical resources. However, women who had at least one ANC were more likely to self-medicate than others. This result could be due to lack of awareness among women about the danger of drugs during pregnancy. ANC plays a crucial role in raising women’s awareness of the different reactions of their new and changing body to drugs and to the transplacental passage of certain molecules (Biblot, 2013).
The present study showed that the prevalence of conventional medicine self-medication during pregnancy was 32%. This finding was in line with the studies carried out in Jordan (33.1%) (Alsous et al., 2021), Serbia (34.7%) (Odalovic et al., 2012), and Pakistan (37.9%) (Bohio et al., 2016). The prevalence was higher than in Indonesia (11.7%) (Atmadani et al., 2020), Netherlands (12.5%) (De Waard et al., 2019), and Egypt (16.6%) (Tawfik et al., 2021) but lower than in Ethiopia (42.2%) (Niriayo et al., 2021), Tanzania (46.2%) (Marwa et al., 2018), and Nigeria (62.9%) (Joseph et al., 2017). This was due to poor awareness in pregnant women regarding medicines (83%) (Alani et al., 2020), poor knowledge about medication use during pregnancy (Alani et al., 2020), and availability of over-the-counter drugs in pharmacies. As in most African countries, health care providers may not adequately educate pregnant women about the potential health risks of self-medication for women and their fetuses due to high workloads.
The principal reason for practicing modern drug self-medication was time-saving. This finding was in line with the study conducted in Ethiopia (73.6%) (Zewdie et al., 2018), where,as in northern Jordan, self-medication was related to previous experience with the disease (47.7%) (Alsous et al., 2021). Moreover, in southern Italy and Egypt, it was related to an assumption that the disease was minor (47%) (Navaro et al., 2018) and (47.8%) (Khalaf et al., 2018). However, in Iran, the main reason was a lack of knowledge about the disease (Baghianimoghadam et al., 2013). Access to medicines without a medical prescription facilitates self-medication.
Modern drug self-medication is practiced mainly in the first quarter, up to 68.6%. This result was different from the studies carried out in Tanzania (Marwa et al., 2018) and France (Cabut, 2017), where self-medication was more frequent in the second and third trimesters, respectively. Self-medication is a consequence of the apparition of physiological symptoms experienced by pregnant women in the first trimester, namely, nausea, vomiting, and headaches. These symptoms diminish during the second trimester and resume in the third trimester. They are combined with other symptoms such as ligament and muscle pain and gastro-esophageal reflux (Elaine et al., 2021). This highlights an alarming threat because exposure to drugs during this period is likely to cause congenital malformations (Bérard et al., 2007; Gidai et al., 2008).
In this study, pregnant women used drugs without any medical advice to treat mainly nausea and vomiting (70.3%), whereas headaches were the main ailment treated in North East Ethiopia (30%) (Tuha et al., 2020), Jordan (85.5%) (Alsous et al., 2021), Europe, North America and South America, and Australia (Lupattelli et al., 2014). Pregnancy is a normal physiological state that leads to pathological changes that must be managed properly, and pregnant women should only take medication by prescription.
Paracetamol was mostly self-used in pregnancy. This result was comparable to the study conducted in Harar town (Jambo et al., 2018). According to the FDA, acetaminophen may be linked to attention deficit hyperactivity disorder (ADHD) in children born to women who take the drug at any time during pregnancy (FDA, 2019). Other studies have shown that it can be associated with neuropsychiatric risks, neurodevelopmental delays (Brandlistuen et al., 2013), autism spectrum disorders (Liew et al., 2016), and even attention-deficit/hyperactivity disorder (Hoover et al., 2015). Therefore, the use of paracetamol during pregnancy should be carefully considered, and pregnant women should always consult their doctors before use.
The use of aspirin during pregnancy is alarming, even though it is a drug that was once classified as probably safe (category D) (Black and Hill, 2003). A study conducted among Swedish pregnant women showed that aspirin users had a higher incidence of intrapartum bleeding [AOR = 1.63; 95% CI (1.30–2.05)], postpartum hemorrhage [AOR = 1.23; 95% CI (1.08–1.39)], and postpartum hematoma [AOR = 2.21; 95% CI (1.13–4.34)], and the risk of a neonatal intracranial hemorrhage was also increased [AOR = 9.66; 95% CI (1.88–49.48)] (Hastie et al., 2021).
These data show that it is mandatory to reinforce the awareness among pregnant women on the risks related to the use of paracetamol and aspirin, especially since they are sold over the counter (Bremer et al., 2017).
The first source of information for conventional medicine self-medication was pharmacist. A similar source of information was reported in several studies conducted in Ethiopia (Sema et al., 2020; Tuha et al., 2020; Niriayo et al., 2021). The pharmacist is often in direct contact with the women when they purchase medicines and should take this opportunity to counsel them about medication use and safety (Michael et al., 2019).
This study highlights age, parity, gestational age, previous ANC follow-up, chronic illness, and drug treatment as the main factors associated with self-medication. More than half of women over 30 years old were more likely to self-medicate than others. This finding is comparable to the study conducted by Atmadani et al. in 2020, which indicated that women over 28 years of age were significantly more likely to self-medicate [AOR = 2.14, 95% CI (1.01–4.50)] (Atmadani et al., 2020). Similarly, multiparity was positively associated with self-medication. This finding agrees with a study conducted in Brazil in 2015 [AOR = 1.25, 95% CI (1.03–1.5)] (Bertoldi et al., 2014). This finding could be due to the experience acquired by these women through drug use, age, and number of pregnancies (Lutz et al., 2020).
Pregnant women with chronic illness and those who were following therapeutic treatments were less likely to administer self-medication compared to their counterparts. This was similar to a finding study conducted in China (Lei et al., 2018).
Although the level of education and occupation of pregnant women were not associated with self-medication, several studies have shown that a low level of knowledge increases the practice of self-medication (Ebrahimi et al., 2017).
This study addressed a knowledge gap regarding self-medication during pregnancy in the Settat region. The results of this study call for spreading more awareness among pregnant women by health care providers and the implementation of adequate strategies to control the marketing, distribution, and use of conventional drugs.
Study limitations
This study had some limitations, such as the sample size. The sample size needs to be increased in order to reach all social segments of the population. Also, the study can be influenced by social desirability bias and recall bias, which can lead to an underestimation of drug use among women and confusion about the names of drugs. Another limitation was that the survey did not reach pregnant women in the rural area since it was conducted at Settat health centers. This did not allow drawing a conclusion on the behavior of pregnant women toward self-medication.
Conclusion
Self-medication is a threat to the safety of the developing fetus and the pregnant woman. The prevalence of modern drug self-medication among pregnant women in Morocco is classified as lower than in several African countries such as Egypt and Ghana (Zeid et al., 2020; Gbagbo and Nikrumah., 2020). The associated factors of modern drug self-medication were age, parity, chronic illness, and therapeutic treatment.
The risk of adverse effects or intoxication related to excessive or inappropriate self-medication is well-documented. In view of these data, in the context of the modalities of delivery of medicines in Morocco, it is imperative that information concerning medicines be delivered to pregnant women by the different health professionals involved in the monitoring of pregnant women.
Acknowledgments
We sincerely thank the pregnant women who participated in the study, all health professionals at Settat city for their valuable support with records retrieving and logistic issues, Hassan First University, and the health delegation of the Casablanca-Settat region for granting us permission to conduct the study.
Data availability atatement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Hassan First University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SC is the principal investigator and a major contributor to all aspects of this study and manuscript; she was involved in study design, study execution, data analysis, critical discussion, and drafting of the manuscript. OC helped in study design and critical discussion. AM and SE contributed greatly to data analysis. IY and AH majorly contributed to critical discussion and revision of the manuscript and helped in study design. All authors read and approved the final version of the manuscript.
Funding
This study was funded by University Hassan First’s own fund [grant number FP/01/2018]. The funding body had no involvement in the design of the study, data collection, analyses and interpretation, or manuscript preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Afolabi A. O. (2008). Factors influencing the pattern of self-medication in an adult Nigerian population. Ann. Afr. Med. 7, 120–127. 10.4103/1596-3519.55666 [DOI] [PubMed] [Google Scholar]
- Alani A. H. H. D. A., Hassan B. A. R., Suhaimi A. M., Mohammed A. H. (2020). Use, awareness, knowledge and beliefs of medication during pregnancy in Malaysia. Osong Public Health Res. Perspect. 11, 373–379. 10.24171/j.phrp.2020.11.6.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsous M. M., Al‐Azzam I., Nusair M. B., Alnahar S. A., Obeidat N. A. (2021). Self‐medication among pregnant women attending outpatients’ clinics in northern Jordan‐a cross‐sectional study. Pharmacol. Res. Perspect. 9, e00735. 10.1002/prp2.735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atmadani R. N., Nkoka O., Yunita S. L., Chen Y.-H. (2020). Self-medication and knowledge among pregnant women attending primary healthcare services in malang, Indonesia: A cross-sectional study. BMC Pregnancy Childbirth 20, 42. 10.1186/s12884-020-2736-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haut Commissariat au Plan (HCP) (2018). Monograph of the province of Settat. Available at: https://www.hcp.ma/regch-aouia/docs/Publications/Monographie_prov%20SETTAT_2018_Finale.pdf .
- Aziz M. M., Masood I., Yousaf M., Saleem H., Ye D., Fang Y., et al. (2018). Pattern of medication selling and self-medication practices: A study from Punjab, Pakistan. PLoS One 13, e0194240. 10.1371/journal.pone.0194240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baghianimoghadam M. H., Mojahed S., Baghianimoghadam M., Yousefi N., Zolghadr R. (2013). Attitude and practice of pregnant women regarding self-medication in Yazd, Iran. Arch. Iran. Med. 16, 580–583. [PubMed] [Google Scholar]
- Bennadi D. (2013). Self-medication: A current challenge. J. Basic Clin. Pharm. 5, 19–23. 10.4103/0976-0105.128253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bérard A., Ramos E., Rey E., Blais L., St-André M., Oraichi D., et al. (2007). First trimester exposure to paroxetine and risk of cardiac malformations in infants: The importance of dosage. Birth Defects Res. B Dev. Reprod. Toxicol. 80, 18–27. 10.1002/bdrb.20099 [DOI] [PubMed] [Google Scholar]
- Bertoldi A. D., Camargo A. L., Silveira M. P. T., Menezes A. M. B., Assunção M. C. F., Gonçalves H., et al. (2014). Self-medication among adolescents aged 18 Years: The 1993 pelotas (Brazil) birth cohort study. J. Adolesc. Health 55, 175–181. 10.1016/j.jadohealth.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biblot P. (2013). L’automédication chez la femme enceinte : la précarité comme facteur de risque?. Médecine humaine et pathologie ffhal-01868062f. [Google Scholar]
- Black R. A., Hill D. A. (2003). Over-the-Counter medications in pregnancy. Am. Fam. Physician 67, 2517–2524. [PubMed] [Google Scholar]
- Bohio R., Brohi Z. P., Bohio F. (2016). Utilization of over the counter medication among pregnant women; a cross-sectional study conducted at Isra University Hospital, Hyderabad. J. Pak. Med. Assoc. 66, 68–71. [PubMed] [Google Scholar]
- Brandlistuen R. E., Ystrom E., Nulman I., Koren G., Nordeng H. (2013). Prenatal paracetamol exposure and child neurodevelopment: A sibling-controlled cohort study. Int. J. Epidemiol. 42, 1702–1713. 10.1093/ije/dyt183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branthwaite A., Pechère J. C. (1996). Pan-European survey of patients’ attitudes to antibiotics and antibiotic use. J. Int. Med. Res. 24, 229–238. 10.1177/030006059602400301 [DOI] [PubMed] [Google Scholar]
- Bremer L., Goletzke J., Wiessner C., Pagenkemper M., Gehbauer C., Becher H., et al. (2017). Paracetamol medication during pregnancy: Insights on intake frequencies, dosages and effects on hematopoietic stem cell populations in cord blood from a longitudinal prospective pregnancy cohort. EBioMedicine 26, 146–151. 10.1016/j.ebiom.2017.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabut S., Marie C., Vendittelli F., Sauvant-Rochat M.-P. (2017). Intended and actual use of self-medication and alternative products during pregnancy by French women. J. Gynecol. Obstet. Hum. Reprod. 46 (2), 167–173. 10.1016/j.jogoh.2016.10.005 [DOI] [PubMed] [Google Scholar]
- De Waard M., Blomjous B. S., Hol M. L. F., Sie S. D., Corpeleijn W. E., van Goudoever J., et al. (2019). Medication use during pregnancy and lactation in a Dutch population. J. Hum. Lact. 35, 154–164. 10.1177/0890334418775630 [DOI] [PubMed] [Google Scholar]
- Ebrahimi H., Atashsokhan G., Amanpour F., Hamidzadeh A. (2017). Self-medication and its risk factors among women before and during pregnancy. Pan Afr. Med. J. 27, 183. 10.11604/pamj.2017.27.183.10030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elaine N. M., Hoehn K., Nancy L. (2021). Anatomie et physiologie humaines (9e édition) - renouveau Pedagogique - grand format. Available at: https://halldulivre.com/livre/9782761369329-anatomie-et-physiologie-humaines-9e-edition-elaine-n-marieb-katja-hoehn/(Accessed April 14, 2021).
- ENPSF (2018). 2ème édition.pdf. Available at: https://www.sante.gov.ma/Documents/2020/03/Rapport%20ENPSF%202018%202i%C3%A8me%20%C3%A9dition.pdf (Accessed April 7, 2021).
- FDA (2019). FDA drug safety communication: FDA has reviewed possible risks of pain medicine use during pregnancy. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-has-reviewed-possible-risks-pain-medicine-use-during-pregnancy (Accessed March 9, 2022).
- FDA (2021). Pregnancy and lactation labeling (drugs) final rule. Available at: https://www.fda.gov/drugs/labeling-information-drug-products/pregnancy-and-lactation-labeling-drugs-final-rule (Accessed August 20, 2021).
- Food and Drug Administration (2014). Content and format of labeling for human prescription drug and biological products; requirements for pregnancy and lactation labeling. Final rule. Fed. Regist. 79, 72063–72103. [PubMed] [Google Scholar]
- Gbagbo F. Y., Nkrumah J. (2020). Self-medication among pregnant women in two municipalities in the Central Region of Ghana. Health Care Women Int. 42, 547–562. 10.1080/07399332.2020.1716235 [DOI] [PubMed] [Google Scholar]
- Gidai J., Acs N., Bánhidy F., Czeizel A. E. (2008). A study of the teratogenic and fetotoxic effects of large doses of chlordiazepoxide used for self-poisoning by 35 pregnant women. Toxicol. Ind. Health 24, 41–51. 10.1177/0748233708089018 [DOI] [PubMed] [Google Scholar]
- Hastie R., Tong S., Wikström A.-K., Sandström A., Hesselman S., Bergman L., et al. (2021). Aspirin use during pregnancy and the risk of bleeding complications: A Swedish population-based cohort study. Am. J. Obstet. Gynecol. 224, 95.e1–95.e12. 10.1016/j.ajog.2020.07.023 [DOI] [PubMed] [Google Scholar]
- Hoover R. M., Hayes V. A. G., Erramouspe J. (2015). Association between prenatal acetaminophen exposure and future risk of attention deficit/hyperactivity disorder in children. Ann. Pharmacother. 49, 1357–1361. 10.1177/1060028015606469 [DOI] [PubMed] [Google Scholar]
- Jambo A., Mengistu G., Sisay M., Amare F., Edessa D. (2018). Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of harar town, Ethiopia. Front. Pharmacol. 9, 1063. 10.3389/fphar.2018.01063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph B., Ezie I., Aya B., Dapar M. (2017). Self-medication among pregnant women attending ante-natal clinics in jos-north, Nigeria. Int. J. Trop. Dis. Health 21, 1–7. 10.9734/IJTDH/2017/28248 [DOI] [Google Scholar]
- Khalaf S., Aly S., Ahmed A. (2018). Prevalence and attitude regarding non prescribed medications among pregnant women attending maternal and child health care centers in assiut city. J. Nurs. Heal. Sci. (IOSR-JNHS) 7 (5), 1–11. [Google Scholar]
- Lei X., Jiang H., Liu C., Ferrier A., Mugavin J. (2018). Self-medication practice and associated factors among residents in wuhan, China. Int. J. Environ. Res. Public Health 15, 68. 10.3390/ijerph15010068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew Z., Ritz B., Virk J., Olsen J. (2016). Maternal use of acetaminophen during pregnancy and risk of autism spectrum disorders in childhood: A Danish national birth cohort study. Autism Res. 9, 951–958. 10.1002/aur.1591 [DOI] [PubMed] [Google Scholar]
- Lupattelli A., Spigset O., Twigg M. J., Zagorodnikova K., Mårdby A. C., Moretti M. E., et al. (2014). Medication use in pregnancy: A cross-sectional, multinational web-based study. BMJ Open 4, e004365. 10.1136/bmjopen-2013-004365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz B. H., Miranda V. I. A., Silveira M. P. T., Dal Pizzol T. da S., Mengue S. S., da Silveira M. F., et al. (2020). Medication use among pregnant women from the 2015 pelotas (Brazil) birth cohort study. Int. J. Environ. Res. Public Health 17, E989. 10.3390/ijerph17030989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marwa K. J., Njalika A., Ruganuza D., Katabalo D., Kamugisha E. (2018). Self-medication among pregnant women attending antenatal clinic at makongoro health centre in mwanza, Tanzania: A challenge to health systems. BMC Pregnancy Childbirth 18, 16. 10.1186/s12884-017-1642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael C., Angela L., Hedvig N., Marina O., Michael T., Veerle F., et al. (2019). Women’s beliefs about medicines and adherence to pharmacotherapy in pregnancy: Opportunities for community pharmacists. Curr. Pharm. Des. 25, 469–482. 10.2174/1381612825666190321110420 [DOI] [PubMed] [Google Scholar]
- Mohseni M., Azami-Aghdash S., Gareh Sheyklo S., Moosavi A., Nakhaee M., Pournaghi-Azar F., et al. (2018). Prevalence and reasons of self-medication in pregnant women: A systematic review and meta-analysis. Int. J. Community Based Nurs. Midwifery 6, 272–284. [PMC free article] [PubMed] [Google Scholar]
- Navaro M., Vezzosi L., Santagati G., Angelillo I. F., Working Group Collaborative. (2018). Knowledge, attitudes, and practice regarding medication use in pregnant women in Southern Italy. PLoS ONE 13, e0198618. 10.1371/journal.pone.0198618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niriayo Y. L., Mohammed K., Asgedom S. W., Demoz G. T., Wahdey S., Gidey K., et al. (2021). Self-medication practice and contributing factors among pregnant women. PLoS ONE 16, e0251725. 10.1371/journal.pone.0251725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odalovic M., Vezmar Kovacevic S., Ilic K., Sabo A., Tasic L. (2012). Drug use before and during pregnancy in Serbia. Int. J. Clin. Pharm. 34, 719–727. 10.1007/s11096-012-9665-8 [DOI] [PubMed] [Google Scholar]
- Oirdi M., Cherrah Y., Ahid S. (2015). Profil de l’automédication chez des patients dans la région de Rabat-Salé-Zemmour-Zair, Maroc. Revue d'Epidemiologie. de Sante Publique 63, S78. 10.1016/j.respe.2015.03.092 [DOI] [Google Scholar]
- Sema F. D., Addis D. G., Melese E. A., Nassa D. D., Kifle Z. D. (2020). Prevalence and associated factors of self-medication among pregnant women on antenatal care follow-up at university of gondar comprehensive specialized hospital in gondar, northwest Ethiopia: A cross-sectional study. Int. J. Reprod. Med., 2020. 10.1155/2020/2936862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley A. Y., Durham C. O., Sterrett J. J., Wallace B. (2019). Safety of over-the-counter medications in pregnancy. Am. J. Maternal/Child Nursing. 10.1097/NMC.0000000000000537 [DOI] [PubMed] [Google Scholar]
- Subashini N., Udayanga L. (2020). Demographic, socio-economic and other associated risk factors for self-medication behaviour among University students of Sri Lanka: A cross sectional study. BMC Public Health 20, 613. 10.1186/s12889-020-08622-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haute Autorité de Santé (2007). Suivi et Orientation des femmes enceintes en fonction des situations à risque identifiées. La Rev. Sage-Femme 6, 216–218. 10.1016/S1637-4088(07)79647-5 [DOI] [Google Scholar]
- Tawfik A. G., Abdelaziz A. I., Omran M., Rabie K. A., Ahmed A.-S. F., Abou-Ali A., et al. (2021). Assessment of community pharmacy management towards self-medication requests of tetracyclines for pregnant women: A simulated client study in upper Egypt. Int. J. Clin. Pharm. 43, 969–979. 10.1007/s11096-020-01203-0 [DOI] [PubMed] [Google Scholar]
- Tuha A., Faris A. G., Mohammed S. A., Gobezie M. Y. (2020). Self-medication and associated factors among pregnant women attending antenatal care at kemisie general hospital, North East Ethiopia. Patient prefer. Adherence 14, 1969–1978. 10.2147/PPA.S277098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Food and Drug Administration (2015). Pregnancy and lac tation labeling (drugs) final rule. Available at: https://www.fda.gov/Drugs/DevelopmentApprovalProcess/ DevelopmentResources/Labeling/ucm093307.htm . [Google Scholar]
- World Health Organization (2000). Guidelines for the regulatory assessment of medicinal products for use in self-medication. Available at: https://apps.who.int/iris/handle/10665/66154 (Accessed January 31, 2022).
- Zeid W., Hamed M., Mansour N., Diab R. (2020). Prevalence and associated risk factors of self-medication among patients attending El-Mahsama family practice center, Ismailia, Egypt. Bull. Natl. Res. Cent. 44, 92. 10.1186/s42269-020-00351-7 [DOI] [Google Scholar]
- Zewdie T., Azale T., Shimeka A., Lakew A. M. (2018). Self-medication during pregnancy and associated factors among pregnant women in goba town, southeast Ethiopia: A community based cross sectional study. BMC Res. Notes 11, 713. 10.1186/s13104-018-3821-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.


