Abstract
Purpose
With an increasing number of anterior cervical discectomy and fusion (ACDF) being conducted for degenerative cervical disc disease, there is a rising interest in the related quality of management and healthcare costs. Unplanned readmission after ACDF affects both the quality of management and medical expenses. This meta-analysis was performed to evaluate the risk factors of unplanned readmission after ACDF to improve the quality of management and prevent increase in healthcare costs.
Materials and Methods
We searched the databases of PubMed, EMBASE, Web of Science, and Cochrane Library to identify eligible studies using the searching terms, “readmission” and “ACDF.” A total of 10 studies were included.
Results
Among the demographic risk factors, older age [weighted mean difference (WMD), 3.93; 95% confidence interval (CI), 2.30–5.56; p<0.001], male [odds ratio (OR), 1.23; 95% CI, 1.10–1.36; p<0.001], and private insurance (OR, 0.34; 95% CI, 0.17–0.69; p<0.001) were significantly associated with unplanned readmission. Among patient characteristics, hypertension (HTN) (OR, 2.14; 95% CI, 1.41–3.25; p<0.001), diabetes mellitus (DM) (OR, 1.59; 95% CI, 1.20–2.11; p=0.001), coronary artery disease (CAD) (OR, 2.87; 95% CI, 2.13–3.86; p<0.001), American Society of Anesthesiologists (ASA) physical status grade >2 (OR, 2.13; 95% CI, 1.68–2.72; p<0.001), and anxiety and depression (OR, 1.39; 95% CI, 1.29–1.51; p<0.001) were significantly associated with unplanned readmission. Among the perioperative factors, pulmonary complications (OR, 22.52; 95% CI, 7.21–70.41; p<0.001) was significantly associated with unplanned readmission.
Conclusion
Male, older age, HTN, DM, CAD, ASA grade >2, anxiety and depression, pulmonary complications were significantly associated with an increased occurrence of unplanned readmission after ACDF.
Keywords: Anterior cervical spine surgery, readmission, risk factor, meta-analysis
INTRODUCTION
The number of anterior cervical discectomy and fusion (ACDF) conducted to treat degenerative cervical disc disease has increased; consequently, there is a rising interest in the quality of management after ACDF.1,2,3,4 Complications related to ACDF affect the quality of management and occurrence of unplanned readmission.5 Furthermore, unplanned readmission after ACDF eventually increases healthcare costs and decreases the quality of management.6 In hospitals, a fixed amount is allocated for medical expenses related to surgical care; therefore, unplanned readmission after ACDF that increases healthcare costs is considered a financial burden.6 For instance, a study has shown that the median costs of 30- and 90-day readmission episodes were $6727 and $8507, respectively.7 Several studies have been conducted to determine the risk factors related to unplanned readmission after ACDF. Goyal, et al.7 studied the risk factors of 30- and 90-day readmissions after ACDF and determined that age, sex, primary diagnosis, length of stay at index admission, Elixhauser comorbidity index, and payer type are significant risk factors of readmission. Sheha, et al.8 found that the incidence of readmission within 90 days after discharge following ACDF was 5.3%, and the associated risk factors were age >60 years, sex, insurance status, disposition at discharge, and length of hospital stay. The purpose of this study was to determine the risk factors of unplanned readmission after ACDF for degenerative cervical disc disease through a meta-analysis to improve the quality of management of spine surgery and prevent the rising healthcare cost related to unplanned readmissions.
MATERIALS AND METHODS
Data source and search strategy
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.9 We searched PubMed, EMBASE, Web of Science, and Cochrane Library databases for eligible studies to identify the risk factors of unplanned readmission after ACDF published by December 2021. Studies in which comparisons were made between the characteristics of patients who were readmitted and those who were not after cervical spine surgery were identified by using the search terms, “readmission” and “anterior cervical discectomy and fusion.” Only articles published in English were considered. The selected studies were independently screened by three authors (YJL, SHN, SHK) based on the inclusion and exclusion criteria. Data regarding the risk factors were then collected. Furthermore, we reviewed the reference lists of these studies to identify other relevant literature.
Inclusion and exclusion criteria
The adequacy of the studies was decided based on the PRISMA guidelines.9 Unplanned readmission was defined as hospitalization for complications related to surgery within 90 days after surgery. The inclusion criteria were as follows: 1) the patients underwent ACDF for degenerative cervical disc disease, 2) the study demonstrated the total patient population and that of patients who underwent unplanned readmission after ACDF, and 3) the studies compared the risk factors or causes of unplanned readmission. The exclusion criteria were as follows: 1) the patients underwent spine surgery other than that related to the degenerative cervical disc disease, 2) details related to the population were not reported, 3) the available data were not presented, and 4) duplication of reports and review articles.
Data extraction
Data such as patient populations, their demographic and clinical profiles, and causes of readmission were extracted and reviewed from the included studies by three authors (YJL, SHN, SHK). The common factors among the studies that were considered as differences between patients who were readmitted and those who were not were identified and analyzed, based on which the risk factors of unplanned readmission after ACDF were investigated.
Quality assessment
We used the Newcastle-Ottawa Quality Assessment Scale (NOQAS) to evaluate the quality of studies that were included,10 which were assessed based on three major categories: selection, comparability, and exposure. Studies that acquired at least six stars were included to guarantee the reliability of the present analysis.
Statistical analysis
We utilized the Review Manager software, version 5.3 (Cochrane Collaboration, Oxford, UK) for this meta-analysis.
Meta Essentials (ERASMUS Research Institute, Rotterdam, Netherlands) were used to make funnel plots. The factors were compared and measured using the weighted mean differences (WMDs) and corresponding 95% confidence intervals (CIs) for continuous data. Their effects were evaluated using 95% CI and odds ratios (ORs). Heterogeneity of the studies was assessed using the I2 index and chi-squared test. If there was high heterogeneity between the studies, a random-effects model (p<0.1 or I2 >50%) was applied; otherwise, a fixed-effects model was applied. To test for publication bias, the Egger test was performed. P-values<0.05 were considered statistically significant.
RESULTS
Included studies
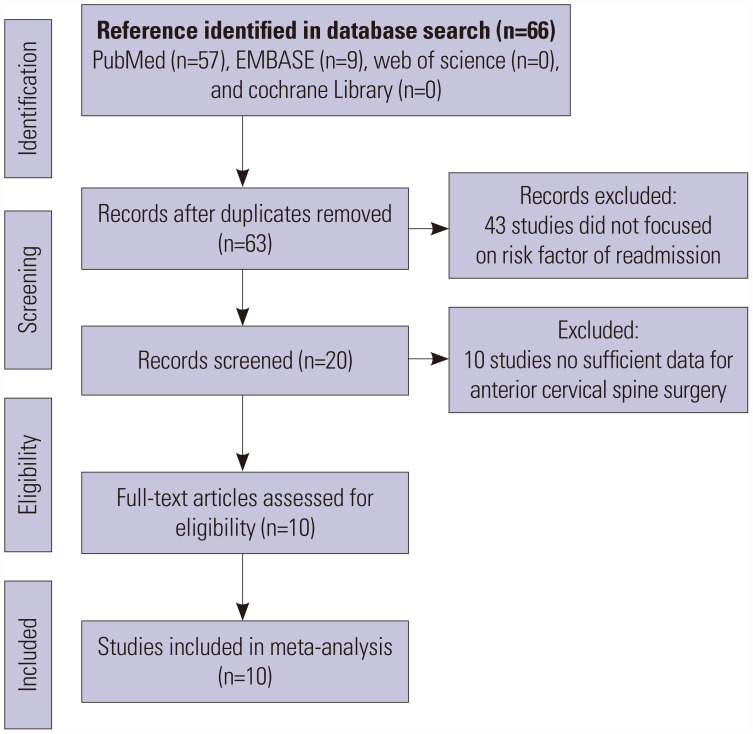
A total of 66 studies from the PubMed (57) and EMBASE (9) databases were assessed for inclusion in this study. After excluding duplicate studies, 63 remained, of which 43 were excluded after reviewing the abstracts and titles as they were not focused on unplanned readmissions after ACDF and the associated risk factors. Ten studies were eliminated due to insufficient data related to ACDF. Finally, 10 studies were selected for our meta-analysis. Fig. 1 shows the process by which we selected the studies. The characteristics of the included studies are presented in Table 1.
Fig. 1. Flow chart of study selection process.
Table 1. Characteristics of Studies Included in the Meta-Analysis.
| Study | Year | Country | Study period | Total | Unplanned readmission | Unplanned readmission rate | Mean age (yr) | Study type | Center |
|---|---|---|---|---|---|---|---|---|---|
| Bhashyam, et al.28 | 2017 | USA | 2013–2014 | 5590 | 145 | 2.6 | 52±12 | Retrospective | Multicenter |
| Zaki, et al.32 | 2019 | USA | 2013–2014 | 389 | 30 | 7.70 | 52.0±10.9 | Retrospective | Unicenter |
| Sheha, et al.8 | 2019 | USA | 2005–2012 | 41813 | 2223 | 5.32 | 50.7±11.8 | Retrospective | Multicenter |
| Goyal, et al.7 | 2020 | USA | 2012–2015 | 113418 | 6677 | 6 | 55.1 | Retrospective | Multicenter |
| Dial, et al.20 | 2020 | USA | 2013. 07–2017. 03 | 1896 | 144 | 7.60 | ND | Retrospective | Unicenter |
| Elsamadicy, et al.21 | 2020 | USA | 2013–2015 | 13093 | 856 | 6.5 | ND | Retrospective | Multicenter |
| Schafer, et al.17 | 2020 | USA | 2014. 02–2018. 07 | 3762 | 202 | 5.40 | 56.3±10.7 | Retrospective | Multicenter |
| Taylor, et al.22 | 2021 | USA | 2014. 01–2014. 09 | 50126 | 4152 | 8.3 | 55 (18–90) | Retrospective | Multicenter |
| Kamalapathy, et al.29 | 2021 | USA | 2011–2017 | 18339 | 959 | 6 | ND | Retrospective | Multicenter |
| Shah, et al.30 | 2021 | USA | 2016–2018 | 36794 | 2367 | 6.43 | ND | Retrospective | Multicenter |
ND, not described.
Quality assessment of studies
Based on the NOQAS, five studies scored seven points, and the others scored eight. Thus, the quality of each study was sufficiently high (Table 2).
Table 2. Quality Assessment of Included Studies in the Meta-Analysis according to NOQAS.
| Study | Selection | Comparability | Outcome | Total score |
|---|---|---|---|---|
| Bhashyam, et al.28 | 4 | 1 | 2 | 7 |
| Zaki, et al.32 | 4 | 1 | 2 | 8 |
| Sheha, et al.8 | 4 | 1 | 3 | 8 |
| Goyal, et al.7 | 4 | 1 | 3 | 7 |
| Dial, et al.20 | 4 | 1 | 3 | 7 |
| Elsamadicy, et al.21 | 4 | 1 | 3 | 8 |
| Schafer, et al.17 | 4 | 0 | 3 | 7 |
| Taylor, et al.22 | 4 | 1 | 2 | 7 |
| Kamalapathy, et al.29 | 4 | 1 | 3 | 8 |
| Shah, et al.30 | 4 | 1 | 3 | 8 |
NOQAS, Newcastle-Ottawa Quality Assessment Scale.
Incidence of readmission after cervical spine surgery
As reported in the studies included in this meta-analysis, 17755 patients were readmitted after ACDF. The incidence of unplanned readmission after ACDF was 6.2%.
Risk factors of unplanned readmission after cervical spine surgery
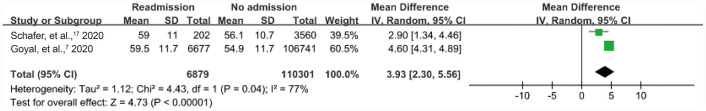
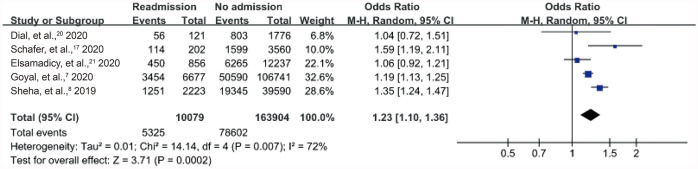
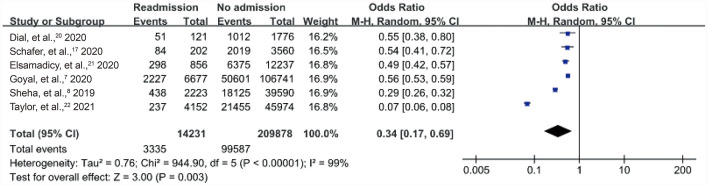
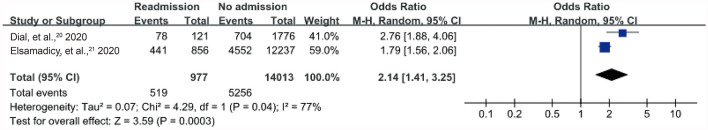
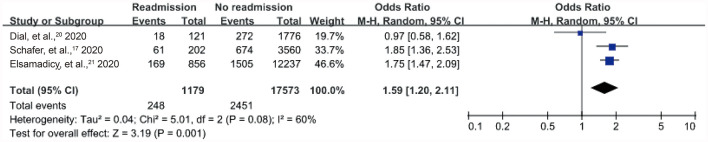
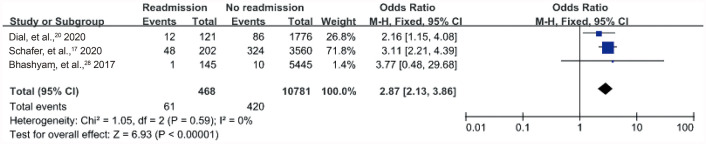
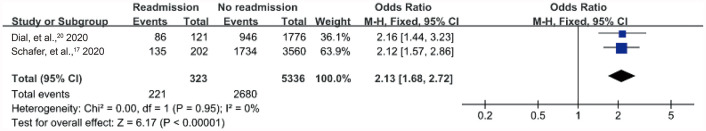
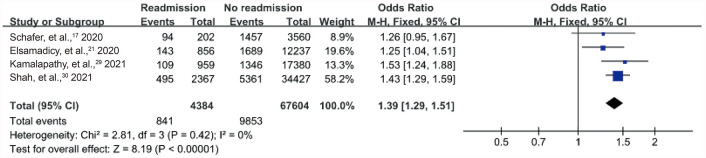
Among the demographic risk factors, advanced age (WMD, 3.93; 95% CI, 2.30–5.56; p<0.001), male sex (OR, 1.23; 95% CI, 1.10–1.36; p<0.001), and private insurance (OR, 0.34; 95% CI, 0.17–0.69; p<0.001) were significantly associated with unplanned readmission after ACDF (Figs. 2, 3, 4). Among patient characteristics, hypertension (HTN) (OR, 2.14; 95% CI, 1.41–3.25; p<0.001), diabetes mellitus (DM) (OR, 1.59; 95% CI, 1.20–2.11; p=0.001), coronary artery disease (CAD) (OR, 2.87; 95% CI, 2.13–3.86; p<0.001), American Society of Anesthesiologists (ASA) physical status grade >2 (OR, 2.13; 95% CI, 1.68–2.72; p<0.001), and anxiety and depression (OR, 1.39; 95% CI, 1.29–1.51; p<0.001) were significantly associated with unplanned readmission (Figs. 5,6, 7, 8, 9). However, current smoking (OR, 1.07; 95% CI, 0.94–1.23; p=0.300) were not significantly associated with unplanned readmission after ACDF (Table 3). Among the perioperative risk factors, pulmonary complications (OR, 22.52; 95% CI, 7.21–70.41; p<0.001) were significantly associated with unplanned readmission after ACDF (Fig. 10).
Fig. 2. Forest plot showing the relationship between age and occurrence of readmission. CI, confidence interval.
Fig. 3. Forest plot showing the relationship between male sex and occurrence of readmission. CI, confidence interval.
Fig. 4. Forest plot showing the relationship between owning private insurance and occurrence of readmission. CI, confidence interval.
Fig. 5. Forest plot showing the relationship between HTN and occurrence of readmission. CI, confidence interval; HTN, hypertension.
Fig. 6. Forest plot showing the relationship between DM and occurrence of readmission. CI, confidence interval; DM, diabetes mellitus.
Fig. 7. Forest plot showing the relationship between CAD and occurrence of readmission. CI, confidence interval; CAD, coronary artery disease.
Fig. 8. Forest plot showing the relationship between ASA class higher than 2 and occurrence of readmission. CI, confidence interval; ASA, American Society of Anesthesiologists.
Fig. 9. Forest plot showing the relationship between anxiety and depression and occurrence of readmission. CI, confidence interval.
Table 3. Summary of Risk Factors of Unplanned Readmission after Anterior Cervical Discectomy and Fusion.
| Risk factors | Number of studies | Test of differences | Test of heterogeneity | Model | ||
|---|---|---|---|---|---|---|
| WMD/OR (95% CI) | p value | I2 (%) | p value | |||
| Age | 2 | 3.93* (2.30 to 5.56) | <0.001 | 77 | 0.040 | R |
| Male | 5 | 1.23† (1.10 to 1.36) | <0.001 | 72 | 0.007 | R |
| Private insurance | 6 | 0.34† (0.17 to 0.69) | <0.001 | 99 | <0.001 | R |
| Current smoker | 3 | 1.07† (0.94 to1.23) | 0.300 | 13 | 0.320 | F |
| HTN | 2 | 2.14† (1.41 to 3.25) | <0.001 | 77 | 0.040 | R |
| DM | 3 | 1.59† (1.20 to 2.11) | 0.001 | 60 | 0.080 | R |
| CAD | 3 | 2.87† (2.13 to 3.86) | <0.001 | 0 | 0.590 | F |
| ASA class>2 | 2 | 2.13† (1.68 to 2.72) | <0.001 | 0 | 0.950 | F |
| DVT | 2 | 7.51† (0.23 to 242.24) | 0.260 | 81 | 0.020 | R |
| Anxiety/depression | 4 | 1.39† (1.29 to 1.51) | <0.001 | 0 | 0.420 | F |
| Pulmonary complication | 3 | 22.52† (7.21 to 70.41) | <0.001 | 89 | <0.001 | R |
WMD, weighted mean difference; OR, odds ratio; CI, confidence interval; HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; DVT, deep vein thrombosis; ASA, American Society of Anesthesiologists.
*Values are WMD; †Values are OR.
Fig. 10. Forest plot showing the relationship between pulmonary complication and occurrence of readmission. CI, confidence interval.
Publication bias
All the funnel plots were symmetric, and there was no significant publication bias among the studies. The Egger test results for each risk factor were as follows: age (p=0.505), male sex (p=0.864), private insurance (p=0.568), HTN (p=0.724), DM (p=0.762), CAD (p=0.642), ASA grade >2 (p=0.287), anxiety and depression (p=0.561), and pulmonary complications (p=0.378). Thus, there was no evidence of publication bias in the dataset.
DISCUSSION
With the increasing incidence of degenerative cervical spine disease, the significance of ACDF, which was introduced by Cloward in 1958 to treat this condition, has also increased.11,12 Complications related to ACDF affect the quality of management and increase the associated healthcare costs.13,14 Moreover, complications that lead to unplanned readmissions can further elevate medical expenses.5,6,15 Several articles regarding unplanned readmission after ACDF have been published, particularly since ACDF is related to specific perioperative complications owing to the relative complexity of its anatomy.16 Therefore, the purpose of this meta-analysis was to evaluate the risk factors related to unplanned readmission after ACDF.
Previous studies have shown that older age and male sex are statistically significant risk factors related to unplanned readmission after ACDF, which concur with the findings of our meta-analysis.7,17 We also found that patients who were older in age were more likely to be readmitted. Smoking history is known to be associated with postoperative complications, such as surgical site infection, which can affect the incidence of readmission secondarily.18,19 Patients are also recommended to stop smoking as it can have adverse effects on wound healing and surgical site infections. In our study, current smoking was not significantly associated with the incidence of unplanned readmission after ACDF (OR, 1.07; 95% CI, 0.94–1.23; p=0.3).
In terms of socioeconomic factors, we found that the patients who owned private insurance were less likely to be readmitted after ACDF. Many studies have shown that the payer status of patients is significantly associated with readmission.7,8,17,20,21,22 Furthermore, insurance status is associated with adverse medical events. While Dial, et al.20 reported that possessing Medicare insurance and no insurance are associated with extended length of hospital stay, Tanenbaum, et al.23 found that having Medicaid insurance is related to increased adverse events after ACDF. Therefore, the association between insurance status and incidence of unplanned readmission after ACDF may be related to the complications after ACDF that lead to readmission (OR, 0.34; 95% CI, 0.17–0.69; p<0.001).
The patient characteristics that were found to be significantly associated with unplanned readmission after ACDF in the present meta-analysis were HTN, DM, ASA grade >2, CAD, and anxiety and depression (OR, 2.14; 95% CI, 1.41–3.25; p<0.001) (OR, 1.59; 95% CI, 1.20–2.11; p=0.001) (OR, 2.13; 95% CI, 1.68–2.72; p<0.001) (OR, 2.87; 95% CI, 2.13–3.86; p<0.001) (OR, 1.39; 95% CI, 1.29–1.51; p<0.001). Diabetes has been previously associated with perioperative complications and readmission after spine surgery, and there is a significant difference in occurrence between the patients who were readmitted and those who were not.24,25 This factor also exhibited a statistically significant association with unplanned readmission after ACDF in this meta-analysis. The ASA classification is commonly used to assess the overall comorbidities in patients.26,27 Schafer, et al.17 reported that ASA grade >2 is associated with increased likelihood of readmission, while Dial, et al.20 demonstrated that the ASA score is related to 90-day readmission. Patients with ASA grade 4 tend to be readmitted more frequently than those with lower ASA grade.26 Furthermore, patients who are readmitted after ACDF are more likely to have CAD.20,28 Kamalapathy, et al.29 and Shah, et al.30 reported that patients with anxiety and depression have a higher risk of readmission after ACDF.
Among the perioperative factors, pulmonary complication was revealed to be significantly associated with unplanned readmission after ACDF. While we considered dyspnea, pulmonary edema, and pneumonia as pulmonary complications, deep vein thrombosis was examined as an independent complication. Pulmonary complications are commonly known to cause unplanned readmission after ACDF.20,31 They have been reported to result in unplanned readmission in 14% of the total number of patients.20 Similarly, another study has shown that 13.1% of the patients who were readmitted after ACDF had pulmonary complications.8 Furthermore, pulmonary complications are the second most common cause of unplanned readmission after ACDF, while the most common cause is systemic infection and sepsis.32 For another perioperative factor, wound complication was also reported to be a significant risk factor of readmission after ACDF; Zaki, et al.32 and Dial, et al.20 reported that the proportions of patients readmitted after ACDF due to wound complications were 5.7% and 5%, respectively. Another study showed that 16.7% of the patients who required readmission had wound infection, and postoperative superficial surgical site infection was revealed to be significantly associated with readmission within 30 days.24 However, in this meta-analysis, wound complication as a risk factor of readmission could not be analyzed due to the lack of data.
Finally, while postoperative dysphagia is one of the most serious complications associated with ACDF,13,16 this factor was not included in the present meta-analysis. In the absence of a uniform definition of dysphagia, its reported incidence after ACDF in the literature varies between 1% and 79%.33 In our study, we did not analyze the incidence of dysphagia after ACDF due to the lack of uniform data.
Limitations
This meta-analysis had some limitations. First, retrospective studies were analyzed, which might have affected the results. Second, some risk factors were not included in the analysis due to the lack of data. For example, although esophageal rupture is a critical but rare complication associated with ACDF,13,20,31,34,35 it was not analyzed in this study due to the limited information available. Further studies are required to analyze the risk factors that are considered clinically significant.
Conclusion
The incidence of unplanned readmission after ACDF was 6.2%. Advanced age, male sex, ASA grade >2, HTN, DM, CAD, anxiety and depression, and pulmonary complications were significantly associated with unplanned readmission after ACDF. Furthermore, having private insurance was identified as a factor that could prevent unplanned readmission after ACDF. Understanding the risk factors of readmission would help surgeons ensure the quality of management and prevent financial burden.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Data curation: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Formal analysis: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Funding acquisition: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Investigation: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Methodology: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Project administration: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Resources: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Software: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Supervision: all authors.
- Validation: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Visualization: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Writing—original draft: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Writing—review & editing: Young Ju Lee, Sang Hyun Kim, and Sung Hyun Noh.
- Approval of final manuscript: all authors.
References
- 1.Marawar S, Girardi FP, Sama AA, Ma Y, Gaber-Baylis LK, Besculides MC, et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976) 2010;35:1454–1459. doi: 10.1097/BRS.0b013e3181bef3cb. [DOI] [PubMed] [Google Scholar]
- 2.Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: a national database analysis between 2002 and 2011. Spine (Phila Pa 1976) 2014;39:476–481. doi: 10.1097/BRS.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 3.Lee JY, Park MS, Moon SH, Shin JH, Kim SW, Kim YC, et al. Loss of lordosis and clinical outcomes after anterior cervical fusion with dynamic rotational plates. Yonsei Med J. 2013;54:726–731. doi: 10.3349/ymj.2013.54.3.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JH, Park JY, Yi S, Kim KH, Kuh SU, Chin DK, et al. Anterior cervical discectomy and fusion alters whole-spine sagittal alignment. Yonsei Med J. 2015;56:1060–1070. doi: 10.3349/ymj.2015.56.4.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131:1796–1803. doi: 10.1161/CIRCULATIONAHA.114.010270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain N, Phillips FM, Khan SN. Distribution and determinants of 90-day payments for multilevel posterior lumbar fusion: a medicare analysis. Clin Spine Surg. 2018;31:E197–E203. doi: 10.1097/BSD.0000000000000612. [DOI] [PubMed] [Google Scholar]
- 7.Goyal A, Bhandarkar AR, Alvi MA, Kerezoudis P, Yolcu YU, Habermann EB, et al. Cost of readmissions following anterior cervical discectomy and fusion: insights from the nationwide readmissions database. Neurosurgery. 2020;87:679–688. doi: 10.1093/neuros/nyz443. [DOI] [PubMed] [Google Scholar]
- 8.Sheha ED, Salzmann SN, Khormaee S, Yang J, Girardi FP, Cammisa FP, et al. Patient factors affecting emergency department utilization and hospital readmission rates after primary anterior cervical discectomy and fusion: a review of 41813 cases. Spine (Phila Pa 1976) 2019;44:1078–1086. doi: 10.1097/BRS.0000000000003058. [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. Newcastle-Ottawa quality assessment scale cohort studies. Ottawa: University of Ottawa; 2014. [Google Scholar]
- 11.Machino M, Yukawa Y, Imagama S, Ito K, Katayama Y, Matsumoto T, et al. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: a comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine (Phila Pa 1976) 2016;41:476–482. doi: 10.1097/BRS.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 12.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 13.Joseph JR, Smith BW, Mummaneni PV, La Marca F, Park P. Postoperative dysphagia correlates with increased morbidity, mortality, and costs in anterior cervical fusion. J Clin Neurosci. 2016;31:172–175. doi: 10.1016/j.jocn.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Puvanesarajah V, Hassanzadeh H, Shimer AL, Shen FH, Singla A. Readmission rates, reasons, and risk factors following anterior cervical fusion for cervical spondylosis in patients above 65 years of age. Spine (Phila Pa 1976) 2017;42:78–84. doi: 10.1097/BRS.0000000000001663. [DOI] [PubMed] [Google Scholar]
- 15.Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472:188–193. doi: 10.1007/s11999-013-3034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 2002;27:2453–2458. doi: 10.1097/00007632-200211150-00007. [DOI] [PubMed] [Google Scholar]
- 17.Schafer E, Bazydlo M, Schultz L, Park P, Chang V, Easton RW, et al. Rates and risk factors associated with 90-day readmission following cervical spine fusion surgery: analysis of the Michigan Spine Surgery Improvement Collaborative (MSSIC) registry. Spine J. 2020;20:708–716. doi: 10.1016/j.spinee.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Echt M, De la Garza Ramos R, Nakhla J, Gelfand Y, Cezayirli P, Holland R, et al. The effect of cigarette smoking on wound complications after single-level posterolateral and interbody fusion for spondylolisthesis. World Neurosurg. 2018;116:e824–e829. doi: 10.1016/j.wneu.2018.05.103. [DOI] [PubMed] [Google Scholar]
- 19.Connor M, Briggs RG, Bonney PA, Lamorie-Foote K, Shkirkova K, Min E, et al. Tobacco use is associated with increased 90-day readmission among patients undergoing surgery for degenerative spine disease. Global Spine J. 2022;12:787–794. doi: 10.1177/2192568220964032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dial BL, Esposito VR, Danilkowicz R, O’Donnell J, Sugarman B, Blizzard DJ, et al. Factors associated with extended length of stay and 90-day readmission rates following ACDF. Global Spine J. 2020;10:252–260. doi: 10.1177/2192568219843111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elsamadicy AA, Koo AB, Lee M, Freedman IG, David WB, Kundishora AJ, et al. Patient risk factors associated with 30-and 90-day readmission after cervical discectomy: a nationwide readmission database study. Clin Spine Surg. 2020;33:E434–E441. doi: 10.1097/BSD.0000000000001030. [DOI] [PubMed] [Google Scholar]
- 22.Taylor BES, Hilden P, Hansen RTB, Nanda A, Gillick JL. National rates, reasons, and risk factors for 30- and 90-day readmission and reoperation among patients undergoing anterior cervical discectomy and fusion: an analysis using the nationwide readmissions database. Spine (Phila Pa 1976) 2021;46:1302–1314. doi: 10.1097/BRS.0000000000004020. [DOI] [PubMed] [Google Scholar]
- 23.Tanenbaum JE, Miller JA, Alentado VJ, Lubelski D, Rosenbaum BP, Benzel EC, et al. Insurance status and reportable quality metrics in the cervical spine fusion population. Spine J. 2017;17:62–69. doi: 10.1016/j.spinee.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeidan M, Goz V, Lakomkin N, Spina N, Brodke DS, Spiker WR. Predictors of readmission and prolonged length of stay after cervical disc arthroplasty. Spine (Phila Pa 1976) 2021;46:487–491. doi: 10.1097/BRS.0000000000003839. [DOI] [PubMed] [Google Scholar]
- 25.Zreik J, Alvi MA, Yolcu YU, Sebastian AS, Freedman BA, Bydon M. Utility of the 5-item modified frailty index for predicting adverse outcomes following elective anterior cervical discectomy and fusion. World Neurosurg. 2021;146:e670–e677. doi: 10.1016/j.wneu.2020.10.154. [DOI] [PubMed] [Google Scholar]
- 26.Phan K, Kim JS, Lee NJ, Kothari P, Cho SK. Relationship between ASA scores and 30-day readmissions in patients undergoing anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2017;42:85–91. doi: 10.1097/BRS.0000000000001680. [DOI] [PubMed] [Google Scholar]
- 27.Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77:217–222. doi: 10.1093/bja/77.2.217. [DOI] [PubMed] [Google Scholar]
- 28.Bhashyam N, De la Garza Ramos R, Nakhla J, Nasser R, Jada A, Purvis TE, et al. Thirty-day readmission and reoperation rates after single-level anterior cervical discectomy and fusion versus those after cervical disc replacement. Neurosurg Focus. 2017;42:E6. doi: 10.3171/2016.11.FOCUS16407. [DOI] [PubMed] [Google Scholar]
- 29.Kamalapathy PN, Wang KY, Puvanesarajah V, Raad M, Hassanzadeh H. Presence and severity of mental illness is associated with increased risk of postoperative emergency visits, readmission, and reoperation following outpatient ACDF: a national database analysis. Global Spine J. 2021 Jul 02; doi: 10.1177/21925682211026913. [Epub]. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah KC, Dominy C, Tang J, Geng E, Arvind V, Pasik S, et al. Significance of hospital size in outcomes of single-level elective anterior cervical discectomy and fusion: a nationwide readmissions database analysis. World Neurosurg. 2021;155:e687–e694. doi: 10.1016/j.wneu.2021.08.122. [DOI] [PubMed] [Google Scholar]
- 31.Samuel AM, Fu MC, Toy JO, Lukasiewicz AM, Webb ML, Bohl DD, et al. Most 30-day readmissions after anterior cervical discectomy and fusion are not due to surgical site-related issues: an analysis of 17,088 patients. Spine (Phila Pa 1976) 2016;41:1801–1807. doi: 10.1097/BRS.0000000000001775. [DOI] [PubMed] [Google Scholar]
- 32.Zaki O, Jain N, Yu EM, Khan SN. 30-and 90-day unplanned readmission rates, causes, and risk factors after cervical fusion: a single-institution analysis. Spine (Phila Pa 1976) 2019;44:762–769. doi: 10.1097/BRS.0000000000002937. [DOI] [PubMed] [Google Scholar]
- 33.Riley LH, 3rd, Vaccaro AR, Dettori JR, Hashimoto R. Postoperative dysphagia in anterior cervical spine surgery. Spine (Phila Pa 1976) 2010;35(9 Suppl):S76–S85. doi: 10.1097/BRS.0b013e3181d81a96. [DOI] [PubMed] [Google Scholar]
- 34.Zhong ZM, Jiang JM, Qu DB, Wang J, Li XP, Lu KW, et al. Esophageal perforation related to anterior cervical spinal surgery. J Clin Neurosci. 2013;20:1402–1405. doi: 10.1016/j.jocn.2012.11.020. [DOI] [PubMed] [Google Scholar]
- 35.Patel NP, Wolcott WP, Johnson JP, Cambron H, Lewin M, McBride D, et al. Esophageal injury associated with anterior cervical spine surgery. Surg Neurol. 2008;69:20–24. doi: 10.1016/j.surneu.2007.05.006. [DOI] [PubMed] [Google Scholar]