Abstract
Background:
Currently, there is no consensus regarding the accuracy of magnetic resonance imaging (MRI) in the detection of acetabular chondral delamination (ACD) in patients with femoroacetabular impingement (FAI), and, correspondingly, the preoperative diagnosis of ACD remains challenging.
Hypothesis:
It was hypothesized that MRI would have relatively high accuracy in detecting ACD in patients with FAI.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
We retrospectively evaluated patients who attended the sports medicine clinic of our department and underwent arthroscopic surgery for the diagnosis of FAI between January 2018 and December 2020. All patients underwent preoperative 3.0-T MRI. ACD was evaluated by 2 raters on 3.0-T MRI scans, and interrater and intrarater reliability was assessed. Sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) of MRI for diagnosis of ACD were calculated, using arthroscopic surgery as the standard.
Results:
A total of 233 patients (mean age, 37.4 years; 99 male and 134 female) were included in this study. The presence of ACD in 101 (43.3%) patients was confirmed during hip arthroscopy. The intraobserver reliability of both of the observers in detecting ACD using 3.0-T MRI scans was almost perfect (observer 1, kappa coefficient [κ] = 0.909 [95% CI, 0.854-0.964]; observer 2, κ = 0.937 [95% CI, 0.890-0.984]), and the interobserver reliability between the observers (κ = 0.801 [95% CI, 0.723-0.879]) was substantial. The overall sensitivity, specificity, PPV, and NPV of preoperative MRI to detect ACD were 83.7%, 82%, 74.2%, and 89.1%, respectively.
Conclusion:
It was found that 3.0-T MRI had a relatively high sensitivity, specificity, PPV, and NPV for diagnosis of ACD in patients with FAI and could be a reliable method of diagnosing ACD preoperatively.
Keywords: acetabular chondral delamination, femoroacetabular impingement, hip arthroscopy
Acetabular chondral delamination (ACD) occurs when the cartilage separates or debonds from the underlying subchondral bone plate and forms an unstable cartilage flap. ACD is commonly presented in patients diagnosed with femoroacetabular impingement (FAI), 2,7,16 and the reported incidence of ACD in FAI varies from 31.5% to 86.5%. 2,9,14,16,17,19,22 Accurate diagnosis of ACD is important since it has the propensity to progress into full-thickness defects and eventually results in degenerative arthritis. 4,9,13,18
Magnetic resonance arthrography (MRA) has high sensitivity in detecting labral abnormalities in patients with FAI; however, there are conflicting reports regarding the accuracy of MRA in the detection of ACD in patients with FAI. 21,23 The sensitivity of MRA for diagnosis of ACD in patients with FAI varies from 6% to 97%. 2,9,16,19,25 The results of current research are quite different, and preoperative diagnosis of ACD in FAI remains challenging and uncertain.
As far as we know, there is little research on the use of magnetic resonance imaging (MRI) in the diagnosis of ACD. Therefore, the purpose of this study was to investigate the diagnostic accuracy of MRI in ACD in patients with FAI. We hypothesized that 3.0-T MRI would have a high diagnostic accuracy in ACD in patients with FAI.
Methods
Patients
We retrospectively evaluated patients who attended the sports medicine clinic of our department and underwent arthroscopic surgery for the diagnosis of FAI between January 2018 and December 2020. The inclusion criteria were as follows: patients who (1) were diagnosed with FAI via clinical findings, plain radiography, computed tomography, and MRI; and (2) underwent hip arthroscopy for FAI. The exclusion criteria were as follows: (1) previous hip surgery, (2) avascular necrosis, (3) Legg-Calve-Perthes disease, (4) Ehlers-Danlos syndrome, (5) pigmented villonodular synovitis, (6) osteoid osteoma, (7) synovial chondromatosis, and (8) rheumatologic disease. The ethics committee of our hospital approved the protocol for this study, and all participants signed informed consent forms.
MRI Diagnosis and Follow-up
As described in a previous study, 10 hip MRI was performed using a 3.0-T magnetic resonance scanner (Magnetom Trio with TIM system; Siemens Healthcare) and a dedicated flexible surface coil around the affected hip joint. In brief, conventional MRI of the affected hip joint was performed when patients were in the supine position. A fat-suppressed turbo spin-echo (TSE) intermediate- and T2-weighted sequence was performed separately in the axial, oblique transverse, and oblique coronal planes using the following parameters: repetition time (TR), 3000 ms; time to echo (TE), 32 ms and 76 ms; field of view (FOV), 180 mm × 180 mm; slice thickness, 3.0 mm; slice gap, 0.3 mm; and matrix, 256 × 230. Imaging in the oblique transverse plane was performed parallel to the axis of the femoral neck, while that in the oblique coronal plane was performed perpendicular to the line through the anterior and posterior acetabulum edge on the axial images. TSE T1-weighted sequence was also performed routinely in the oblique coronal plane using the following parameters: TR, 820 ms; TE, 10 ms; FOV, 180 mm × 180 mm; slice thickness, 3.0 mm; slice gap, 0.3 mm; and matrix, 256 × 230. The total time taken for MRI of a single hip ranged from 30 to 35 minutes.
All MRI scans were analyzed by 2 authors who were blinded to the results of hip arthroscopy: observer 1 (G.G., a surgeon) with >5 years of experience with hip MRI and arthroscopy and observer 2 (Y.X., a surgeon) with >15 years of experience with hip MRI and arthroscopy. ACD was considered to be present when both of the following criteria were met 2,5,6 : (1) at least 2 consecutive slices in the same plane or in the same location in 2 different planes showed focal discontinuity of cartilage and fluid located between the acetabular cartilage and subchondral bone plate, and (2) the area of delaminated cartilage was not completely detached from the adjacent cartilage (Figure 1A). The preoperative alpha angle and lateral center-edge angle (LCEA) were measured as described previously. 1,3 The evaluations were performed twice by both surgeons at different times to determine the intraobserver and interobserver variability.
Figure 1.
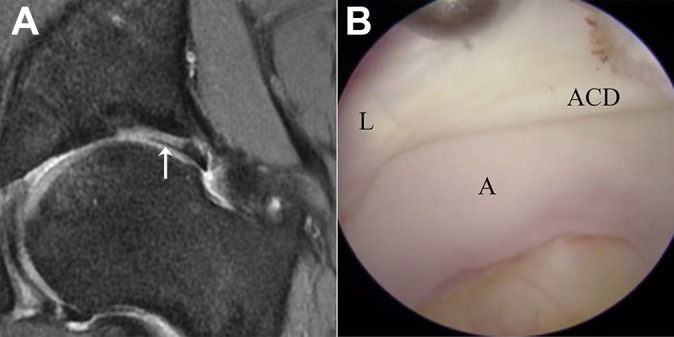
(A) Acetabular chondral delamination (arrow) shown on preoperative 3.0-T magnetic resonance imaging scan. (B) Acetabular chondral delamination identified during arthroscopy. A, acetabulum; ACD, acetabular chondral delamination; L, labrum.
Arthroscopic Surgery
Hip arthroscopy was performed by a single surgeon with >10 years of experience (Y.X.). All patients underwent standard hip arthroscopy. All surgeries were performed using a standard supine approach as described previously. 11 Arthroscopic findings of ACD for comparison with findings on MRI scans (Figure 1B) included (1) an area of degenerated cartilaginous surface at the chondrolabral junction, (2) a partial detachment of the articular cartilage from the subchondral bone without exposing it, and (3) no interruption of the articular surface. 2,18 This finding is the so-called wave sign, also known as bubble sign or carpet phenomenon. 8,13,18 Arthroscopic findings and procedures were recorded. There was no special treatment for ACD.
Statistical Analysis
Continuous variables with a normal distribution in the baseline data between patients with and without ACD were examined using the independent-samples t test, and percentages were compared using the chi-square test. Differences with P < .05 were considered statistically significant. Intra- and interobserver reliability was evaluated by calculating the kappa coefficient (κ), which was interpreted as poor (κ = 0), slight (κ = 0.01-0.200), fair (κ = 0.21-0.40), moderate (κ = 0.41-0.60), substantial (κ = 0.61-0.80), or almost perfect (κ = 0.81-1.00). 15,24 The sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) of preoperative MRI for diagnosing ACD were calculated. All statistical analyses were performed with SPSS Statistics, Version 22 (IBM).
Results
A total of 233 patients (mean age, 37.4 years; age range, 15-67 years; 99 male and 134 female) were included in this study (Table 1). A flowchart illustrating the full patient selection process can be found in Figure 2. Among these 233 patients, 215 (92.3%) were diagnosed with cam-type FAI, 102 (43.8%) were diagnosed with pincer-type FAI, and 228 (97.9%) were diagnosed with labral tear. The age of patients with ACD (mean, 39.1 years) was significantly older than that of patients without ACD (mean age, 36.4 years) (P < .05). Otherwise, there were no significant differences between patients with and without ACD. The intraoperative diagnoses and arthroscopic procedures are shown in Table 2.
Table 1.
Descriptive Data of Study Patients (N = 233) a
| Parameter | Value |
|---|---|
| Age, y, mean (range) | 37.4 (15-67) |
| Sex, n (%) | |
| Male | 99 (42.5) |
| Female | 134 (57.5) |
| Side, n (%) | |
| Left | 100 (42.9) |
| Right | 133 (57.1) |
| BMI, mean (range) | 22.8 (15.4-35.7) |
| Alpha angle, deg, mean ± SD | 57.9 ± 5.8 |
| LCEA, deg, mean ± SD | 34.4 ± 7.1 |
a BMI, body mass index; LCEA, lateral center-edge angle.
Figure 2.
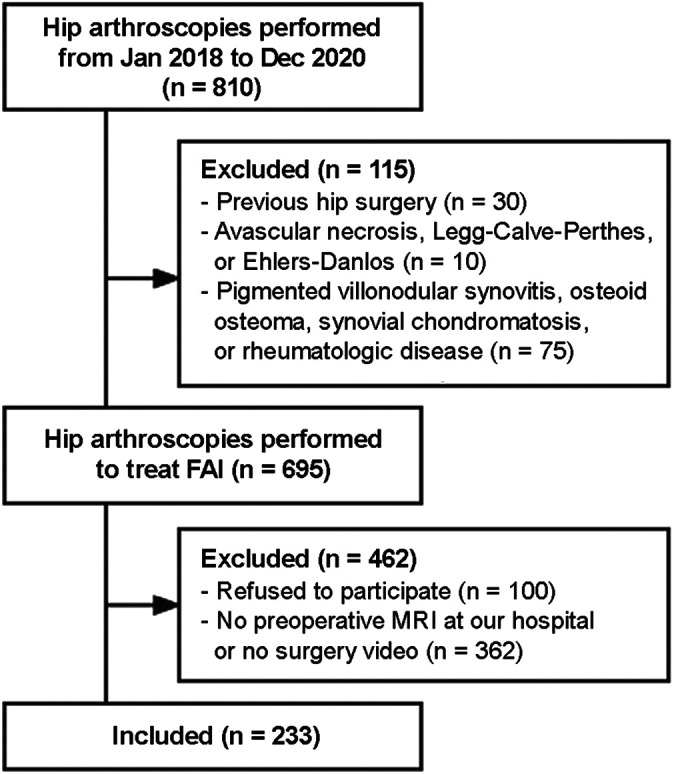
Flowchart illustrating patient selection process. FAI, femoroacetabular impingement; MRI, magnetic resonance imaging.
Table 2.
Intraoperative Diagnoses and Arthroscopic Procedures
| Diagnosis | n (%) |
|---|---|
| Labral tear | 228 (97.9) |
| Cam deformity | 215 (92.3) |
| Pincer deformity | 102 (43.8) |
| Borderline developmental dysplasia of the hip | 23 (9.9) |
| Ischiofemoral impingement | 3 (1.3) |
| Subspine impingement | 16 (6.9) |
| Arthroscopic procedure | |
| Labral repair | 218 (93.6) |
| Labral debridement | 10 (4.3) |
| Femoral osteoplasty | 215 (92.3) |
| Acetabuloplasty | 102 (43.8) |
| Capsular plication | 23 (9.9) |
| Lesser trochanter resection | 3 (1.3) |
| Focal subspinal decompression | 16 (6.9) |
The intraobserver reliability for detecting ACD using 3.0-T MRI was almost perfect for both observer 1 (κ = 0.909; 95% CI, 0.854-0.964) and observer 2 (κ = 0.937; 95% CI, 0.890-0.984). The interobserver reliability between the 2 observers was substantial (κ = 0.801; 95% CI, 0.723-0.879). The presence of ACD was confirmed in 101 (43.3%) patients during hip arthroscopy. For observer 1, of 101 patients with ACD, 73 (72.3%) were correctly diagnosed on preoperative MRI scans as shown in Table 3. Of the 132 patients without ACD, 116 (87.9%) were correctly diagnosed on preoperative MRI scans. Of the remaining patients, 16 (6.9%) had a false-positive ACD and 28 (12.0%) had false-negative ACD on MRI scans.
Table 3.
Comparison Between MRI and Arthroscopy for Diagnosis of ACD a
| Arthroscopy+ | Arthroscopy- | |
|---|---|---|
| Observer 1 | ||
| MRI+ | 73 | 28 |
| MRI- | 16 | 116 |
| Observer 2 | ||
| MRI+ | 76 | 24 |
| MRI- | 13 | 120 |
a Data are presented as No. of diagnoses. ACD, acetabular chondral delamination; MRI, magnetic resonance imaging; +, positive; −, negative.
The sensitivity, specificity, PPV, and NPV of preoperative MRI to detect ACD were 82.0%, 80.6%, 72.3%, and 87.9% for observer 1 and 85.3%, 83.3%, 76.0%, and 90.2% for observer 2, respectively. Overall, the sensitivity, specificity, PPV, and NPV of preoperative MRI were 83.7%, 82%, 74.2%, and 89.1%, respectively.
Discussion
In this study, we found that 3.0-T MRI had relatively high sensitivity, specificity, PPV, and NPV for diagnosis of ACD in patients with FAI. There was no significant difference in alpha angle, LCEA, body mass index, and sex between patients with and without ACD (P > .05). The age of patients with ACD was significantly older than that of patients without ACD (P < .05).
Previous researchers mainly used 1.5-T MRA to diagnose ACD. The reported sensitivity and specificity of MRA for diagnosis of ACD in patients with FAI varies from 6% to 97% and from 40% to 100%, respectively. 2,9,16,19,20,25 Zaragoza et al 25 evaluated 46 patients (48 hips) who underwent surgical dislocation of the hip and reported the sensitivity and specificity of 1.5-T MRA detection of ACD confirmed at surgery were 97% and 84%, respectively. This is the highest sensitivity reported to date. On the other hand, Konstantinidis et al 16 evaluated 229 patients and reported the sensitivity and specificity of 1.5-T MRA detection of ACD confirmed at surgery were 6% and 98%, respectively. It should be noted that the researchers only reviewed radiological reports of the MRA to identify ACD rather than interpreted the images. Anderson et al 2 evaluated 64 hips that had undergone a surgical dislocation procedure for the treatment of FAI and also reported a low sensitivity for ACD (22%) but a high specificity (100%) using 1.5-T MRA.
In the current study, the overall diagnostic sensitivity, specificity, PPV, and NPV of preoperative MRI were 83.7%, 82%, 74.2%, and 89.1%, respectively. In this work, we found that 3.0-T MRI had a high accuracy of diagnosis for ACD. The intra- and interobserver reliabilities of the 2 observers for detecting ACD on 3.0-T MRI scans were almost perfect and substantial. The diagnostic effect of 3.0-T MRI appears to be better than that of 1.5-T MRA, as also reported by previous studies. 2,9,16,19,25 MRA also has the disadvantages of invasive nature, high cost, and risk of allergies. In addition, we found in our daily work that MRA had poorer performance in observation of tissue edema and soft tissue compared with 3.0-T MRI. Most patients with FAI had joint effusion, which we thought could function as a contrast medium between delaminated cartilage and the underlying bone.
The diagnostic sensitivity of preoperative MRI in the current study was 83.7% rather than close to 100%, which indicates that there were factors affecting diagnosis via MRI. One such factor may be that the delaminated cartilage would sit flush on the underlying bone in patients with less joint effusion or small-scale delamination, which could be found only when the lateral border of delaminated cartilage was probed at arthroscopy. In this circumstance, there was no joint effusion between delaminated cartilage and the underlying bone to allow the delaminated cartilage to be observed clearly on MRI scans, which we thought might influence the sensitivity of MRI. Factors affecting the accuracy of diagnosis need to be further studied.
In this study, the incidence of ACD in our case series of 233 hips was 43.3%. The reported incidence of ACD in FAI varies from 31.5% to 86.5%. 2,9,14,16,17,19,22 Our findings are more in accordance with those in a publication from Anderson et al 2 (44%) in 64 hips. It has been reported that ACD is associated with increased age, male sex, increased alpha angle, and delamination cysts. 2,12 –14,16 On the contrary, there is a possible inverse correlation of ACD presence with increased LCEA in patients with symptomatic FAI. 2,16 However, we compared alpha angle, LCEA, body mass index, and sex between patients with and without ACD and found no significant difference. The age of patients with ACD (mean age, 39.1 years) was significantly older than that of patients without ACD (mean age, 36.4 years) (P < .05), which was in accordance with previous studies. 2,13 In previous studies, there were differences in risk factors of ACD other than age. 2,12 –14,16 The risk factors of ACD are still unclear, and further study is needed.
Limitations
A limitation of this study was that it was performed retrospectively. Only patients who went on to surgery were included, which created a potential for selection bias.
Conclusion
Study findings indicated that 3.0-T MRI has a relatively high sensitivity, specificity, PPV, and NPV for diagnosis of ACD in patients with FAI and is a reliable method with which to diagnose ACD preoperatively.
Footnotes
Final revision submitted May 10, 2022; accepted June 6, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Peking University Third Hospital.
References
- 1. Anderson LA, Gililland J, Pelt C, Linford S, Stoddard GJ, Peters CL. Center edge angle measurement for hip preservation surgery: technique and caveats. Orthopedics. 2011;34(2):86. [DOI] [PubMed] [Google Scholar]
- 2. Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement: risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91(2):305–313. [DOI] [PubMed] [Google Scholar]
- 3. Barton C, Salineros MJ, Rakhra KS, Beaulé PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beaulé PE, Hynes K, Parker G, Kemp KA. Can the alpha angle assessment of cam impingement predict acetabular cartilage delamination? Clin Orthop Relat Res. 2012;470(12):3361–3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beaulé PE, Zaragoza E, Copelan N. Magnetic resonance imaging with gadolinium arthrography to assess acetabular cartilage delamination. J Bone Joint Surg Am. 2004;86(10):2294–2298. [DOI] [PubMed] [Google Scholar]
- 6. Beaulé PE, Zaragoza EJ. Surgical images: musculoskeletal acetabular cartilage delamination demonstrated by magnetic resonance arthrography. Inverted “Oreo” cookie sign. Can J Surg. 2003;46(6):463–464. [PMC free article] [PubMed] [Google Scholar]
- 7. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 8. El-Radi MA, Marin-Pena OR, Said HG, Tey-Pons M. Basics in hip chondrolabral lesions and state of the art. SICOT J. 2017;3:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fontana A, Mancini D, Gironi A, Acerbi A. Hip osteochondral lesions: arthroscopic evaluation. Hip Int. 2016;26(suppl 1):17–22. [DOI] [PubMed] [Google Scholar]
- 10. Gao G, Fu Q, Cui L, Xu Y. The diagnostic value of ultrasound in anterosuperior acetabular labral tear. Arthroscopy. 2019;35(9):2591–2597. [DOI] [PubMed] [Google Scholar]
- 11. Gao G, Fu Q, Wu R, Liu R, Cui L, Xu Y. Ultrasound and ultrasound-guided hip injection have high accuracy in the diagnosis of femoroacetabular impingement with atypical symptoms. Arthroscopy. 2021;37(1):128–135. [DOI] [PubMed] [Google Scholar]
- 12. Gdalevitch M, Smith K, Tanzer M. Delamination cysts: a predictor of acetabular cartilage delamination in hips with a labral tear. Clin Orthop Relat Res. 2009;467(4):985–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jannelli E, Parafioriti A, Acerbi A, Ivone A, Fioruzzi A, Fontana A. Acetabular delamination: epidemiology, histological features, and treatment. Cartilage. 2019;10(3):314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24(6):669–675. [DOI] [PubMed] [Google Scholar]
- 15. Karanicolas PJ, Bhandari M, Kreder H, et al. Evaluating agreement: conducting a reliability study. J Bone Joint Surg Am. 2009;91(suppl 3):99–106. [DOI] [PubMed] [Google Scholar]
- 16. Konstantinidis G, Mitchell M, Boyd G, Coady C, Ghosh S, Wong I. Poor sensitivity of magnetic resonance arthrography to detect hip chondral delamination: a retrospective follow-up of 227 FAI-operated patients. Cartilage. 2021;12(2):162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mygind-Klavsen B, Gronbech Nielsen T, Maagaard N, et al. Danish Hip Arthroscopy Registry: an epidemiologic and perioperative description of the first 2000 procedures. J Hip Preserv Surg. 2016;3(2):138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Onggo JD, Onggo JR, Nambiar M, et al. The “wave sign” in hip arthroscopy: a systematic review of epidemiological factors, current diagnostic methods and treatment options. J Hip Preserv Surg. 2020;7(3):410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pfirrmann CW, Duc SR, Zanetti M, Dora C, Hodler J. MR arthrography of acetabular cartilage delamination in femoroacetabular cam impingement. Radiology. 2008;249(1):236–241. [DOI] [PubMed] [Google Scholar]
- 20. Saied AM, Redant C, El-Batouty M, et al. Accuracy of magnetic resonance studies in the detection of chondral and labral lesions in femoroacetabular impingement: systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Samaan MA, Pedoia V, Zhang AL, et al. A novel MR-based method for detection of cartilage delamination in femoroacetabular impingement patients. J Orthop Res. 2018;36(3):971–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sansone M, Ahldén M, Jonasson P, et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):774–780. [DOI] [PubMed] [Google Scholar]
- 23. Schmid MR, Nötzli HP, Zanetti M, Wyss TF, Hodler J. Cartilage lesions in the hip: diagnostic effectiveness of MR arthrography. Radiology. 2003;226(2):382–386. [DOI] [PubMed] [Google Scholar]
- 24. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85(3):257–268. [PubMed] [Google Scholar]
- 25. Zaragoza E, Lattanzio PJ, Beaulé PE. Magnetic resonance imaging with gadolinium arthrography to assess acetabular cartilage delamination. Hip Int. 2009;19(1):18–23. [DOI] [PubMed] [Google Scholar]


