Abstract
This cross-sectional study examines the percentage of deaths attributed to ischemic heart disease by age and sex of Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese decedents.
Age-standardized mortality rates for ischemic heart disease (IHD) are lower in most Asian American subgroups than among non-Hispanic Black and White adults in the US.1 Aggregating the diverse Asian American subgroups into 1 category may mask heterogeneity in health outcomes,2 and data reveal certain Asian American subgroups (eg, Asian Indian and Filipino) experience higher burden of premature IHD mortality (<65 years) and IHD risk factors (eg, diabetes).3 To characterize this burden among the Asian American population, we quantified contemporary age-specific proportional mortality from IHD among Asian American subgroups between 2018 and 2020.
Methods
The Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) was used to obtain data on deaths from all causes and IHD as the underlying cause of death (with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision diagnostic codes I20-I25) between 2018 and 2020, the years in which data with Asian American subgroup categorization were available. This study was deemed exempt from review by Northwestern University Institutional Review Board because it used deidentified publicly available data. We followed the STROBE reporting guideline.
Race and ethnicity were identified by the official signing death certificates or by the next of kin. Given the differences in IHD across race and ethnic groups, we stratified the analyses by Hispanic, non-Hispanic Asian American subgroups (Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese), non-Hispanic Black, and non-Hispanic White.1 Sex-stratified proportional mortality was calculated as the percentage of all deaths attributed to IHD in each racial and ethnic group overall and by age group (0-44, 45-64, or ≥65 years).
Z tests were used to identify differences in proportional mortality from IHD by age, sex, and race and ethnicity and compared with non-Hispanic White decedents. Two-tailed P < .05 indicated significant differences. Statistical calculations were conducted in Microsoft Excel, version 16.63.1 (Microsoft Corporation).
Results
Between 2018 and 2020, there were 8 909 996 total deaths from all causes, including 1 090 591 deaths listing IHD as the underlying cause. Overall, IHD accounted for 10.4% of deaths in non-Hispanic White women, compared with the significantly higher proportional mortality from IHD in Asian Indian and Chinese women (13.2% and 11.9%; P < .001) (Table; Figure). Similarly, IHD accounted for 14.6% of deaths in non-Hispanic White men, whereas Asian Indian (18.7%; P < .001) and Filipino (15.2%; P = .004) men experienced significantly higher proportional mortality, and Korean and Vietnamese men experienced significantly lower proportional mortality (12.4% and 12.2%; P < .001) from IHD.
Table. Age-Stratified Proportional Mortality from Ischemic Heart Disease by Race and Ethnicity in the United States, From 2018 to 2020.
| Race and ethnicitya | No. of deathsb | Mean age at death, y | Proportional mortality, %c | ||||
|---|---|---|---|---|---|---|---|
| Age group, y | Proportional mortality ratiod | ||||||
| 0-44 | 45-64 | ≥65 | All | ||||
| Women | |||||||
| Hispanic | 32 076 | 79.5 | 1.3e | 7.0e | 12.3e | 10.1e | 0.98 |
| Non-Hispanic Asian American | |||||||
| Asian Indian | 1691 | 79.9 | 1.4 | 9.1e | 15.2e | 13.2e | 1.27 |
| Chinese | 3005 | 86.2 | 0.9e | 3.9e | 13.5e | 11.9e | 1.14 |
| Filipino | 2447 | 80.4 | 2.0 | 6.9e | 11.9e | 10.7 | 1.03 |
| Japanese | 1618 | 87.3 | 2.2 | 6.3e | 10.2e | 9.9 | 0.96 |
| Korean | 1189 | 82.8 | 1.7 | 5.2e | 11.9e | 10.6 | 1.03 |
| Vietnamese | 848 | 80.5 | 1.1e | 4.6e | 10.2e | 8.8 | 0.85 |
| Non-Hispanic Black | 56 480 | 75.2 | 2.7e | 9.4e | 11.9e | 10.5 | 1.01 |
| Non-Hispanic White | 347 057 | 81.5 | 2.1 | 8.3 | 11.1 | 10.4 | 1 [Reference] |
| Men | |||||||
| Hispanic | 47 755 | 71.4 | 2.3e | 12.0e | 15.0e | 11.8e | 0.81 |
| Non-Hispanic Asian American | |||||||
| Asian Indian | 3556 | 72.2 | 6.6e | 21.2e | 20.0e | 18.7e | 1.28 |
| Chinese | 3920 | 78.8 | 5.3e | 14.4 | 15.0 | 14.4 | 0.99 |
| Filipino | 3315 | 73.4 | 5.4e | 15.9 | 16.0 | 15.2e | 1.05 |
| Japanese | 1563 | 80.3 | 4.3 | 17.1e | 15.1 | 15.2 | 1.04 |
| Korean | 1190 | 75.3 | 4.6e | 14.3 | 12.7e | 12.4e | 0.85 |
| Vietnamese | 1628 | 70.8 | 5.3e | 14.7 | 12.0e | 12.2e | 0.83 |
| Non-Hispanic Black | 71 195 | 68.5 | 3.0e | 13.4e | 13.8e | 11.9e | 0.82 |
| Non-Hispanic White | 510 058 | 75.2 | 3.2 | 15.1 | 15.4 | 14.6 | 1 [Reference] |
Race and ethnicity were identified by the official signing death certificates or by the next of kin.
Number of deaths represents the pooled number of deaths at any age between 2018 and 2020 with ischemic heart disease as the underlying cause.
Proportional mortality indicates percentage of deaths from all causes in each age group that were attributed to ischemic heart disease as the underlying cause.
Proportional mortality ratio indicates the ratio of the proportion of deaths from ischemic heart disease in a subgroup compared with non-Hispanic White individuals.
Indicates statistically significant difference (P < .05) in proportional mortality compared with non-Hispanic White decedents. Decedents in all Asian American subgroups, Black individuals, and White individuals were non-Hispanic.
Figure. Proportional Mortality From Ischemic Heart Disease by Race and Ethnicity in the US, From 2018 to 2020.
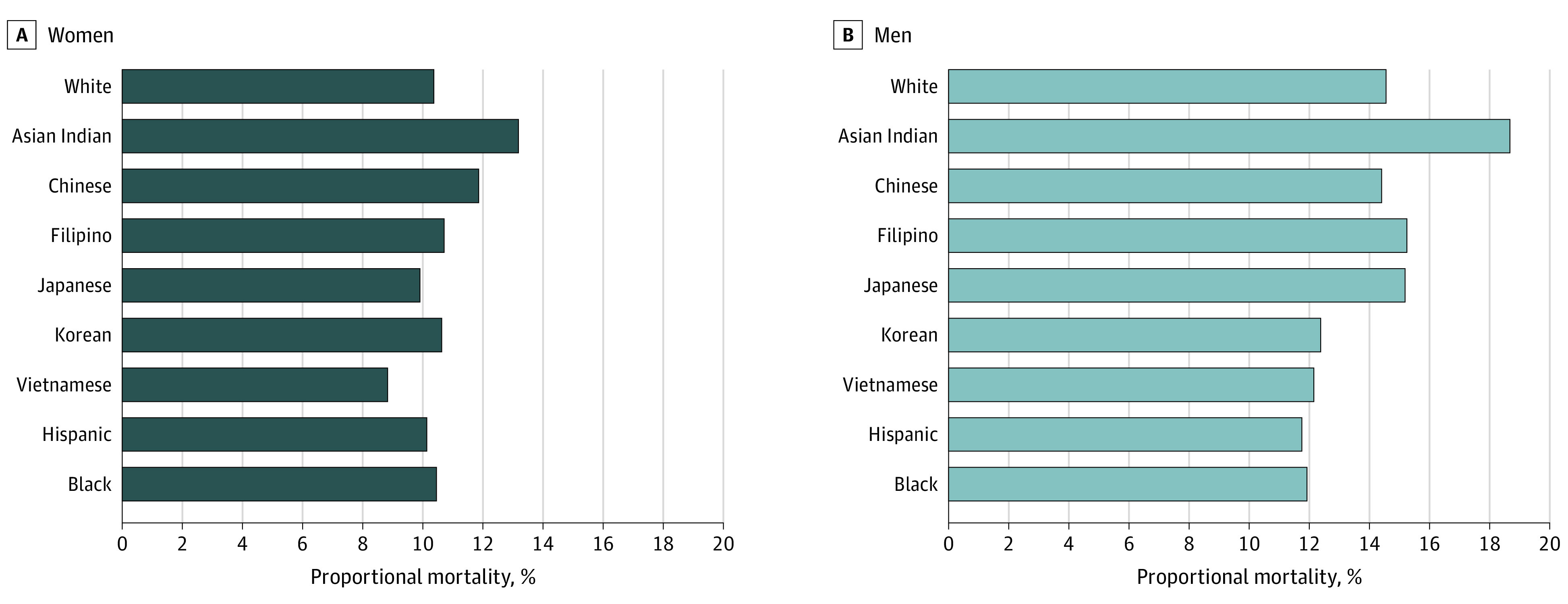
Proportional mortality indicates the percentage of deaths from all causes attributable to ischemic heart disease. Asian Indian, Chinese, and Hispanic women and Asian Indian, Filipino, Korean, Vietnamese, Hispanic, and Black men were statistically significantly different (P < .05) in proportional mortality compared with non-Hispanic White decedents.
Age-stratified proportional mortality is shown in the Table. Significant differences were observed among Asian American subgroups compared with non-Hispanic White individuals. The highest proportional mortality from IHD was observed in Asian Indian men aged 45 to 64 years, which was significantly higher than in non-Hispanic White men in the same age group (21.2% vs 15.1%; P < .001).
Discussion
Among Asian American decedents during the study period, significantly higher proportional mortality from IHD was observed particularly among Asian Indian, Chinese, and Filipino women and men. Age-specific proportional mortality revealed a substantial IHD burden among certain Asian American subgroups, particularly at younger ages, that is not recognized by age-standardized mortality rates.
Study limitations include potential miscoding of IHD on death certificates, inability to study nonfatal IHD events, and lack of population size data in the CDC WONDER to calculate contemporaneous age-standardized mortality rates. Explanations for the observed differences are likely multifactorial, including the implications of social determinants (eg, nativity or immigration and socioeconomic position) and differences in prevalent clinical risk factors (eg, diabetes).4,5
Although IHD mortality rates are generally lower in Asian American subgroups compared with other US populations,1,6 findings of this study provide evidence for the need to address cardiovascular disease risk at younger ages to reduce the burden of premature mortality from IHD among Asian American individuals. Targeted research to identify and implement culturally tailored prevention strategies may be the best first step.
References
- 1.Shah NS, Xi K, Kapphahn KI, et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes. 2022;15(5):e008651. doi: 10.1161/CIRCOUTCOMES.121.008651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diaz CL, Shah NS, Lloyd-Jones DM, Khan SS. State of the nation’s cardiovascular health and targeting health equity in the United States: a narrative review. JAMA Cardiol. 2021;6(8):963-970. doi: 10.1001/jamacardio.2021.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iyer DG, Shah NS, Hastings KG, et al. Years of potential life lost because of cardiovascular disease in Asian-American subgroups, 2003-2012. J Am Heart Assoc. 2019;8(7):e010744. doi: 10.1161/JAHA.118.010744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah NS, Luncheon C, Kandula NR, Cho P, Loustalot F, Fang J. Self-reported diabetes prevalence in Asian American subgroups: Behavioral Risk Factor Surveillance System, 2013-2019. J Gen Intern Med. 2022;37(8):1902-1909. doi: 10.1007/s11606-021-06909-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanaya AM, Hsing AW, Panapasa SV, et al. Knowledge gaps, challenges, and opportunities in health and prevention research for Asian Americans, Native Hawaiians, and Pacific Islanders: a report from the 2021 National Institutes of Health workshop. Ann Intern Med. 2022;175(4):574-589. doi: 10.7326/M21-3729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah NS, Lloyd-Jones DM, Kandula NR, et al. Adverse trends in premature cardiometabolic mortality in the United States, 1999 to 2018. J Am Heart Assoc. 2020;9(23):e018213. doi: 10.1161/JAHA.120.018213 [DOI] [PMC free article] [PubMed] [Google Scholar]


