Abstract
The current study was aimed to evaluate the performance of direct 2,3,5-triphenyl tetrazolium chloride assay and direct microscopic observation drug susceptibility assay with indirect Löwenstein-Jensen proportion method directly on Ziehl-Neelsen smear positive sputum specimens.
Methods
Direct acid fast bacilli smear positive sputum specimens (n = 264) were subjected to isoniazid and rifampicin drug susceptibility testing by direct 2,3,5-triphenyl tetrazolium chloride assay, direct microscopic observation drug susceptibility assay, and the performances were compared with indirect Löwenstein-Jensen proportion method.
Results
The direct 2,3,5-triphenyl tetrazolium chloride assay demonstrated an overall sensitivity, specificity, positive predictive value, and negative predictive value of 99.2%, 82.4%, 99.2%, and 88.5%, respectively, for the detection of isoniazid and rifampicin resistant Mycobacterium tuberculosis isolates when compared to indirect Löwenstein-Jensen proportion method. Likewise, the overall sensitivity, specificity, positive predictive value and negative predictive value of direct microscopic observation drug susceptibility assay were 98.8%, 82.4%, 99.2%, and 78.2%, respectively.
Conclusion
The direct 2,3,5-triphenyl tetrazolium chloride assay was found to be an economical alternative method for the rapid and accurate detection of isoniazid and rifampicin resistance from direct acid fast bacilli smear positive sputum specimens.
Keywords: Tuberculosis, Rapid, Evaluation, Löwenstein–Jensen
Introduction
Tuberculosis (TB) continues to be a leading public health problem across the world particularly in developing countries (Southeast Asia accounts for nearly 40% of global TB cases).1 TB is further complicated by the rising incidence of multidrug resistant (MDR) strains of tubercle bacilli and extensively drug-resistant TB, challenging TB control efforts in several low- and middle-income countries.2, 3 In India, the MDR TB is distributed among 2.9% and 15.3% of newly and previously treated TB cases, respectively, as published by Revised National Tuberculosis Control Program.4 However, the rising incidence and rate of transmission of MDR and extensive drug-resistant TB may be minimized by timely detection of the cases.5 Currently available drug susceptibility testing for mycobacterial isolates use an egg or agar based medium. These traditional culture methods detect Mycobacterium tuberculosis (MTB) growth after an average of three weeks under optimal conditions, and the drug susceptibility testing takes additional three to four weeks.6, 7 However, automated systems (broth based) considerably reduced the time to detection of drug resistance of mycobacterial isolates, but require expensive instrumentation and are technically complicated, limiting their application in low resource settings.8, 9 Furthermore, molecular methods used for the characterization of genes that confer resistance to first-line antimicrobial agents such as Isoniazid (INH) and Rifampicin (RIF) are available; however, the high cost of instruments and specialized expertise to perform these methods limit their wide spread use in developing countries.10 Furthermore, various colorimetric and non-colorimetric assays have been developed recently. However, all these methods were restricted or not evaluated under field conditions, suggesting the prerequisite of an accurate, rapid, inexpensive, and technically simple method for the detection of MDR TB in resource-limited settings.11, 12, 13, 14, 15, 16, 17, 18 In India, most of the mycobacterial clinical laboratories are experiencing intricacy in obtaining drug susceptibility information for MTB isolates due to financial or technical reasons.19 Moreover, treatment of TB unaware of susceptibility information may increase the risk of treatment failure, the spread of resistant strains, and the development of resistance to additional drugs as well.20 In view of the above issues, the current study was designed to evaluate the performance of microscopic observation drug susceptibility (MODS) assay and 2,3,5-triphenyl tetrazolium chloride (TTC) assay with indirect proportion method (using Löwenstein-Jensen (LJ) media) directly on Ziehl-Neelsen (ZN) smear positive sputum specimens. Moreover, to our knowledge, this is the first report to investigate the performance of direct TTC assay and direct MODS directly on ZN smear positive sputum specimens.
Materials and methods
Study settings
The study was conducted in the Department of Microbiology, MM Institute of Medical Sciences and Research, Mullana, Ambala, India, a tertiary care hospital (1050 bedded) that also functions as a peripheral center for the Revised National Tuberculosis Control Program.
Patient screening and recruitment
A total of 283 patients, who were positive for direct acid fast bacilli sputum smear microscopy (stained using ZN staining method) and meeting any of the following criteria were recruited: receiving anti tuberculosis treatment, suspected TB treatment failure, or suspected TB relapse cases were included. However, smear negative cases of pulmonary tuberculosis and salivary sputum samples were excluded.
For the present study, a total of two sputum specimens (spot sample at clinic and morning sample at home) from each patient were collected and all the specimens were transported immediately to the microbiology laboratory (Department of Microbiology, M.M.I.M.S.R) and refrigerated (4–8 °C) overnight. Upon receipt of the second sputum specimen, both spot and early morning sputum samples were stained using ZN staining technique and reports were issued to the patients [as all the sputum samples were collected for routine direct Acid fast bacilli (AFB) smear examination]. For this study, the spot sample at clinic and morning sample at home (both direct AFB smear positive sputum samples) were collected and then mixed irrespective of the smear grades obtained in the routine direct AFB smear examination by pouring the sample from one bottle to another containing undrilled glass beads (1–2 mm, Himedia, Mumbai, India). After mixing, the sputum specimens were homogenized (using a Pasteur pipette for one min) and vortexed for two min to assure uniform distribution of bacilli. After homogenization, the sputum specimens were divided into two aliquots. The first aliquot was subjected to direct AFB smear examination and culture on LJ media, direct MODS assay and direct TTC assay. The second aliquot was stored in a deep freezer (REMI; UDFV-185, Mumbai, India) at −80° C for three months or till the drug susceptibility test results were available. If the DST results using the first aliquot of sputum were not interpretable, then the second aliquot was used to repeat the indirect Löwenstein-Jensen proportion method (LJ PM), direct TTC assay and direct MODS assay.
Laboratory methods
Specimen processing and inoculum preparation
The first aliquot of the sputum specimen [2–3 mL in 14 mL BD Falcon™ centrifuge tube (Becton Dickinson, Franklin Lakes, NJ, USA)] was subjected to direct AFB smear examination and N-acetyl l cystiene (NALC)–sodium hydroxide (NaOH) decontamination method (final NaOH concentration 1%).6 After NALC–NaOH decontamination method, the sediment in each tube was suspended again in phosphate buffered saline to 2 mL and mixed well. This resuspended sediment was used as a common inoculum source for direct TTC assay, direct MODS assay, and indirect LJ proportion method.
Direct TTC assay
The TTC assay was carried out as described by Mohammadzadeh et al., with few modifications.17 Briefly, for each sputum specimen panels of four screw capped round bottom borosilicate glass tubes (Himedia, Mumbai) were used. Of the four screw capped tubes, two tubes were containing 1.6 mL of Middlebrook 7H9 broth, 300 μL of PANTA (PANTA; BBL MGIT PANTA Antibiotic Mixture; BD), 300 μL of solutions of INH 1 μg/mL or RIF 10 μg/mL, 300 μL of the processed specimen and 500 μL of TTC solution (30 μg/mL), giving a final volume of 3 mL per tube, and the critical concentrations of 0.1 μg/mL INH, 1 μg/mL RIF and 5 μg/mL TTC, respectively. One of the other two tubes containing Middlebrook 7H9 broth and PANTA mixture served as a sterile control tube and the other tube as a growth control tube where the inoculum of each sample was included. All the tubes were incubated at 37 °C and after 72 h of incubation these tubes were inspected for color change (growth was indicated by the formation of a red ring or the reddish discoloration of the Middlebrook 7H9 broth). In the absence of a color change, the incubation was continued and the tubes were inspected on days 3, 5, 7, 9, 11, 13, 15 and up to 21 days for a change in color. Drug susceptibility results were interpreted on the same day that the reddish discoloration or red ring appeared in growth control tube. A sample was considered susceptible if red ring or red color was produced in the growth control tube (the drug free tube) but not in the drug-containing tube. A sample was considered resistant if both the drug-free and the drug-containing tubes showed red ring or red color formation.
Direct MODS assay
The direct MODS assay was performed as described by Bwanga et al. with minor modifications21 in the reading time interval of the assay. For this assay, a 24-well tissue culture plate (Himedia, Mumbai, India) was used. To each well 700 μL of Middlebrook 7H9 broth, 100 μL mixture of polymyxin B, amphotericin B, nalidixic acid, trimethoprim, and Azlocillin (PANTA; BBL MGIT PANTA Antibiotic Mixture; BD), 100 μL of solutions of INH 1 μg/mL or RIF 10 μg/mL and 100 μL of the processed specimen was added, thus obtaining a final volume of 1 mL per well and critical concentrations of 0.1 μg/mL INH and 1 μg/mL RIF. A growth control well with Middlebrook 7 H9 broth – PANTA plus the inoculum and the sterile control well with Middlebrook 7 H9 broth-PANTA were included for each sample. All the culture plates were sealed using a cellophane tape, kept in zip lock bags and incubated at 37 °C. The drug-free control wells were observed on days 3, 5, 7, 9, 11, 13, 15, and up to 21 days using an inverted-light microscope (Zeiss, Axiovert 25, Germany) at 40× magnifications. After 15 days of incubation, the observation was restricted to once or twice and continued up to 21 days. Growth was defined as the emergence of visually detectable serpentine clusters of bacteria (cord formation). Drug susceptibility results were interpreted on the same day that distinct growth visualized in control wells. A sample was considered susceptible if growth was visible in the drug-free well but not in the drug-containing well. A sample was considered resistant if both the drug-free and the drug-containing wells showed visible growth.
Indirect LJ proportion method
The proportion method was performed according to established procedures on LJ medium with critical concentrations of 0.2 μg mL for INH and 40 μg mL for RIF. A strain was classified as susceptible to the particular drug only if the number of colonies that grew on the drug-containing medium is <1% of the number of colonies that grew on the drug free control tube and resistant if the number of colonies is >1%.4
Identification of Mycobacterium isolates
The identification of mycobacterial isolates was achieved by positive AFB smear, growth rate, colony pigmentation and morphology, nitrate test, catalase test (at 68 °C), growth on LJ media containing p-nitrobenzoic acid.22 The quality control of each new lot of LJ media and Middlebrook 7H9 broth was performed using reference strains [MTB H37Ra (ATCC 25177) and Mycobacterium kansasii (ATCC 12478)]. Further, the new lot of LJ media and Middlebrook 7H9 broth containing INH and RIF were carried out using H37Rv Mycobacterium tuberculosis strain ATCC 27294 (susceptible control), M. tuberculosis INH resistant (ATCC 35822) and RIF resistant M. tuberculosis (ATCC 35838) strains, respectively.
Time to results for the drug susceptibility assays
Time to results was calculated (in terms of days) from the dates of DST inoculation and till valid (interpretable) results were obtained. These results were interpreted as either ‘resistant’ or ‘susceptible’ whereas invalid results were referred as ‘no growth’ or ‘contaminated tube/well’ even after repeated testing.
Statistical analysis
The performance of the direct MODS assay and the direct TTC assay was compared with the indirect LJ PM and results were interpreted in terms of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). The following formulae were used for calculations; sensitivity was true positives/(true positives + false negatives) × 100; specificity was true negatives/(true negatives + false positives) × 100; PPV was true positives/(true positives + false positives) × 100; and NPV was true negatives/(true negatives + false negatives) × 100. The mean and standard deviations (SD) were calculated for age and gender as well. The differences between contamination rates of direct TTC assay and direct MODS assay were compared with indirect LJ PM and the significance was determined by Fisher's exact test using Graph pad prism online version software.
Ethic statement
Maharishi Markendeshwar University Ethical Committee offered a waiver of informed consent for this study because the specimens used were collected for use in the approved routine direct AFB smear examinations (Let. No. IEC/MMIMSR/13/47). The anti-tubercular drug susceptibility testing (using Indirect LJ proportion method, direct TTC assay and direct MODS assay) were carried out in parallel with direct AFB smear positive sputum specimens obtained from routine direct AFB smear examinations.
Results
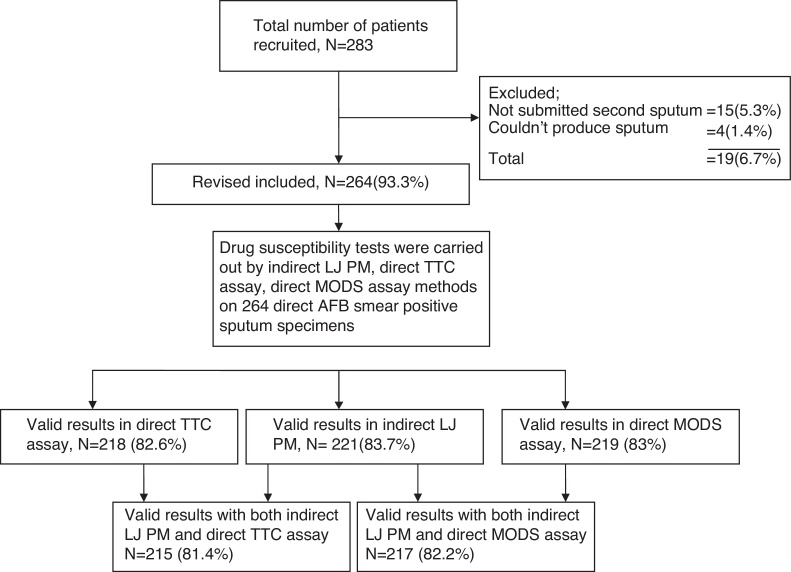
The study was carried out from March 2013 to April 2014 and the study population included both male (n = 177) and female (n = 87) patients with a mean age of 42.2 years (SD 14.4). Of the 264 sputum specimens processed, a total of 224 (84.9%) valid results were obtained in all the assays investigated. Of the total valid results (n = 224) obtained in all the assays studied, 81.4% of the direct TTC assay (valid results, n = 215) and 82.8% direct MODS assay (valid results, n = 217) were interpretable with indirect LJ proportion method (valid results, n = 221) and were considered for statistical analysis (Fig. 1). Table 1 shows valid and invalid drug susceptibility test results obtained by all the assays investigated. With direct TTC assay, 74.6% (n = 197) of the 264 results were valid at initial testing. However, repeated direct TTC assay could provide valid results in 4.6% (n = 12/264) of the contaminated cultures, 3.8% (n = 10/264) indeterminate results (lack of growth in growth control wells), respectively, accomplishing a total percentage of 82.5% (219/264). Similarly, in direct MODS assay 76.1% (n = 201) of the 264 results were valid at initial testing. However, repeated direct MODS assay added 1.5% (n = 4/264) specimens with lack of growth, 4.6% (n = 12/264) of the contaminated cultures, and 0.8% (n = 2/264) of dried wells, giving a total of 83% (219/264) valid results. Furthermore, insufficient growth of MTB, contaminated cultures and growth of non-tuberculous mycobacteria (NTM) resulted in 16.9% of invalid results in all the assays investigated (Table 1).
Fig. 1.
Flow chart showing patient enrolment and drug susceptibility assays performed.
Table 1.
Valid and invalid drug susceptibility test results (n = 264).
| Results | Indirect LJ PM (%) |
Direct TTC assay (%) |
Direct MODS assay (%) |
|---|---|---|---|
| Valid test results | |||
| Sensitive to both INH and RIF | 189 (71.6) | 184 (69.7) | 183 (69.3) |
| Resistance to INH and RIF | 21 (8) | 21 (8) | 21 (8) |
| Resistance to INH | 9 (3.4) | 10 (3.8) | 11 (4.2) |
| Resistance to RIF | 2 (0.8) | 3 (1.1) | 4 (1.5) |
| Sub total | 221 (83.7) | 218 (82.6) | 219 (83) |
| Invalid test results | |||
| No growth | 27 (10.2) | 24 (9.1) | 25 (9.5) |
| Contaminated cultures | 13 (4.9) | 19 (7.2) | 17 (6.4) |
| Non-tuberculous mycobacteria | 3 (1.1) | 3 (1.1) | 3 (1.1) |
| Sub total | 43 (16.3) | 46 (17.4) | 45 (17.1) |
INH, isoniazid; RIF, rifampicin; LJ PM, Löwenstein-Jensen proportion method; TTC assay, 2,3,5-triphenyl tetrazloium chloride assay; direct MODS assay, microscopic drug susceptibility assay.
Table 2 demonstrates turnaround times of direct TTC assay and direct MODS assays. The median time to detection of direct TTC assay was nine days (range 5–21 days). In contrast, the median time to detection of direct MODS assay and indirect LJ PM Method was seven days (range 3–21 days) and 68 days (range 42–120 days), respectively. Among the valid results obtained with the direct TTC assay (n = 215) and the direct MODS assay (n = 217), both the direct TTC assay and direct MODS assay could provide interpretable results in 94% and 93.6% of the sputum specimens within 5–15 days and 3–15 days, respectively.
Table 2.
Turnaround time of the drug susceptibility assays.
| Results (no. of days) |
Direct TTC assay n = 215 (%) |
Direct MODS assay n = 217 (%) |
|---|---|---|
| 3 | – | 1 (0.5) |
| 5 | 2 (0.9) | 53 (24.7) |
| 7 | 83 (38.6) | 77 (35.8) |
| 9 | 62 (28.8) | 35 (16.3) |
| 11 | 34 (15.8) | 19 (8.8) |
| 13 | 12 (5.6) | 2 (0.9) |
| 15 | 9 (4.2) | 16 (7.4) |
| After 15 days | 13 (6.1) | 14 (6.5) |
Direct TTC assay, 2,3,5-triphenyl tetrazloium chloride assay; direct MODS assay, microscopic drug susceptibility assay.
Table 3, Table 4 demonstrates performance of direct MODS assay and direct TTC assay with indirect LJ PM. Among the valid results obtained by direct TTC assay (n = 215), 5.6%, 1.4%, and 9.8% of the MTB isolates were resistant to INH, RIF and both INH and RIF, respectively when compared to indirect LJ PM method (in indirect LJ PM method 5.6%, 1.4%, and 9.8% isolates were resistant to INH, RIF, and both INH and RIF, respectively). Further, the overall sensitivity, specificity, PPV and NPV of direct TTC assay were 99.2%, 82.4%, 99.2, and 88.5% for the detection of INH and RIF resistant MTB isolates. Similarly, of the interpretable results obtained by direct MODS assay (n = 217), 6%, 1.8% and 9.7% of the MTB isolates were resistant to INH, RIF and both INH and RIF, respectively when compared to indirect LJ PM method (in indirect LJ PM method 5.1%, 1.8%, and 9.7% isolates were resistant to INH, RIF, and both INH and RIF, respectively). Further, the overall sensitivity, specificity, PPV and NPV of direct MODS assay were 98.8%, 82.4%, 99.2%, and 78.2%, respectively for the detection of INH and RIF resistant MTB isolates when compared to indirect LJ PM method.
Table 3.
Performance of direct TTC assay with indirect LJ PM.
| Type of assay | Indirect LJ PM |
Sensitivity (%) |
95% C.I. | Specificity | 95% C.I. | PPV | 95% C.I. | NPV | 95% C.I. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Direct TTC assay | S | R | ||||||||
| INH | ||||||||||
| S | 201 | 2 | 98.5 | 95.4–99.6 | 81.8 | 47.8–96.8 | 99 | 96.1–99.8 | 75 | 42.8–93.3 |
| R | 3 | 9 | ||||||||
| RIF | ||||||||||
| S | 211 | 1 | 100 | 97.8–100 | 75 | 21.9–98.7 | 99.5 | 97–100 | 100 | 30.1–100 |
| R | 0 | 3 | ||||||||
| INH + RIF | ||||||||||
| S | 192 | 2 | 99 | 95.9–99.8 | 90.5 | 68.2–98.3 | 99 | 95.9–99.8 | 90.5 | 68.2–98.3 |
| R | 2 | 19 | ||||||||
Table 4.
Performance of direct MODS assay with indirect LJ PM.
| Type of assay | LJ PM |
Sensitivity (%) | 95% C.I. | Specificity | 95% C.I. | PPV | 95% C.I. | NPV | 95% C.I. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Direct MODS assay | S | R | ||||||||
| INH | ||||||||||
| S | 202 | 2 | 98.1 | 94.8–99.4 | 81.9 | 47.8–97 | 99.0 | 96.1–99.8 | 69.2 | 38.9–89.6 |
| R | 4 | 9 | ||||||||
| RIF | ||||||||||
| S | 212 | 1 | 99.5 | 97–100 | 75.0 | 22–99 | 99.5 | 97–100 | 75.0 | 21.9–98.7 |
| R | 1 | 3 | ||||||||
| INH + RIF | ||||||||||
| S | 194 | 2 | 99.0 | 96–100 | 90.5 | 68.2–98.3 | 99.0 | 96–100 | 90.5 | 68.2–98.3 |
| R | 2 | 19 | ||||||||
Discussion
TB continues to be a leading cause of morbidity and mortality across the world. Globally, an estimated 480,000 people developed MDR-TB in 2013.1 However, due to scarcity of cost-effective rapid diagnostic tests, the National TB control programs are unable to routinely carry out surveillance for MDR-TB.19 Therefore, the current study was designed to evaluate the performance of direct TTC assay (a new, rapid, technically simple, cost-effective diagnostic technique) and direct MODS assay in comparison with indirect LJ PM directly on ZN smear positive sputum specimens. In the current study, the male:female ratio was 2:1 and a mean age of 42.2 years (SD 14.4). This data is in agreement with a previous study carried out by Rao et al.23 Of the 264 sputum specimens processed in this study, a total of 84.9% of valid results were obtained in all assays investigated confirming previous reports wherein 89–95% of samples subjected to direct MODS assay could provide valid results.21 However, due to the lack of published studies, the comparison of direct TTC assay was not possible. Furthermore, the relatively lower proportion of valid results in the current study (84.9% valid results obtained in all the assays investigated) may be attributed to patient recruitment criteria adopted in the study. More specifically, in the current study we have recruited patients receiving anti-tuberculosis treatment (ATT). This ATT might have killed the MTB in the sputum specimens, and the dead bacilli must have appeared in the direct sputum smear giving a false-positive AFB smear result. In addition, in this study, the valid results obtained at initial testing with direct TTC assay and direct MODS assay were 74.6% (197/264) and 76.1% (201/264), respectively. These findings indicate that these assays are easy to perform in mycobacteriology laboratories. For few sputum samples, without valid results at initial testing, the main reasons were contamination of culture media, lack of growth, and drying of the wells (in the direct MODS assay). The contamination rate of culture media was 4.9%, 7.2% and 6.4% in indirect LJ PM, direct TTC assay, and direct MODS assay, respectively (Table 1). The relatively lower contamination rate of Indirect LJ PM when compared to direct TTC assay and direct MODS assays may be attributed to the consistency of culture media. Middlebrook 7H9 broth (a liquid culture media) is more prone to develop contamination as reported earlier.24 The second major problem for failing to obtain valid results in all assays was lack of growth in the culture media (Table 1), which may be due to patient recruitment criteria adopted in this study (patients taking ATT were recruited) or may be due to the toxicity caused by NaOH, that might have killed MTB strains (NaOH in the NALC NaOH decontamination method) in the sputum specimens. The other reason for the invalid results in the assays was the growth of NTM (3.1%). This reduced rate of NTM in this study indicates either low prevalence of NTM in this geographical area or proper sterilization techniques adopted in the current study.25
In the present study, of the 264 samples processed, a total of 82.6% and 83.3% valid results were obtained by direct TTC assay and direct MODS assay, respectively. This data suggest the potential of these assays to be implemented for routine direct anti-tubercular drug susceptibility testing. Further, both direct TTC assay (valid results, n = 215) and direct MODS assay (valid results, n = 217) could render 39.5% and 60.4% valid results within the first seven days. However, by 15 days of inoculation, both direct TTC assay and direct MODS assays could provide 54.4% and 33.2% susceptibility results. Thereby, both direct TTC assay and direct MODS assay could detect equal proportion of valid results within 15 days of inoculation. It is evident from Table 2 that the median time to detection of direct TTC assay and direct MODS assay was 9 and 7 days, respectively. This data supports the WHO recommendation [that the use of validated rapid (detect resistance within 2–3 weeks) drug resistance detection methods for the detection of MDR TB if molecular methods are not available] to use direct TTC assay for the detection of drug resistant tuberculosis.26 In the current study setting, the direct TTC assay was found to be very accurate, quick (median time to detection was 9 days), and easy to perform when compared to indirect LJ PM (median time to detection was 68 days) and might represent a significant advancement in detection of MDR TB from the public health and individual patient perspectives.
Various colorimetric assays have been proposed. Among these, direct TTC assay uses the ability of mitochondrial dehydrogenase enzyme of living cells to reduce 2,3,5-TTC (an yellow colored dye) to an insoluble red colored formazan crystals. This insoluble TTC formazan crystal appears as a red ring at the bottom of the tube or reddish discoloration of the culture tube.17 In the current study, when compared to indirect LJ PM, direct TTC assay could provide an excellent sensitivity (98.5%) and specificity (81.8%) for INH, 100% and 75% for RIF, respectively, and 99% and 90.5% for both INH and RIF, respectively. The overall sensitivity and specificity of direct TTC assay was 99.2% and 82.4%, respectively for the detection of drug resistant MTB isolates. These findings are in accordance with Mohammadzadeh et al. (carried out the study directly on MTB isolates) where in a sensitivity and specificity of 100% and 92%, for both INH and RIF, respectively were obtained.17 However, no previous reports were available in literature to compare the performance of direct TTC assay with the current study. The direct TTC assay may be recommended in resource poor settings for the rapid diagnosis of MDR-TB due to its excellent sensitivity, specificity, and ease of implementation. Furthermore, the relatively higher contamination rates in the direct TTC assay (7.2%) when compared to Indirect LJ PM (4.9%) was also not statistically significant (p = 0.36, Fisher's exact test) recommending its use in the routine drug susceptibility testing. The other advantages of direct TTC assay are (a) decreased median time to detection (median detection time 9 days). This median detection time was relatively high when compared to direct MODS assay (median detection time 7 days). However, due to the ease of implementation, higher sensitivity and specificity of direct TTC assay, the median time of 9 days appears to be reasonable for the detection of drug resistant TB; (b) in direct TTC assay, 94% of valid results were obtained within 15 days after inoculation; (c) the direct TTC assay is technically easy to perform as once the required amount of Middlebrook media and drug concentrations are prepared in screw capped test tubes it can be stored at 4–8 °C for future use, minimizing the work load in the laboratory; (d) easy to read the results [as the growth of MTB is indicated with formation of red ring at the bottom (Fig. 2)] or a reddish discoloration of the culture media; (e) reduced aerosol production due to the use of screw capped test tubes; and (f) economical (single direct TTC assay costs ∼20 Indian rupees, excluding the bottle charge, instrument cost, electricity charge, labor charges – data not shown). Considering these advantages, this highly sensitive test should be used to rapidly detect MDR TB from retreatment and follow up patients to confidently eliminate MDR disease. Although, the direct TTC assay has few limitations as well; any type of bacterial (particularly, non-tuberculous mycobacteria) or fungal growth, may give color change of the culture media, giving false-positive results. However, false-positive results due to the growth of non-tuberculous mycobacteria may be resolved if PNB is incorporated in an additional culture tube (PNB, a reagent that inhibits the growth of MTB but not atypical mycobacteria) and the further confirmation of culture can be achieved by direct acid fast staining and biochemical reactions or using molecular techniques.21
Fig. 2.
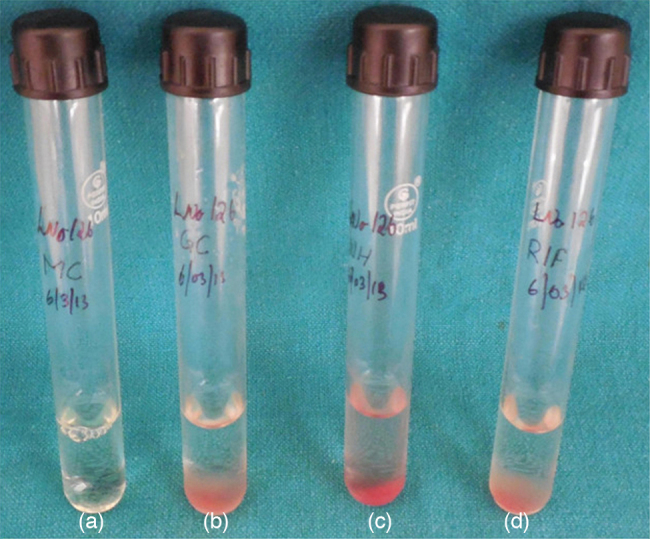
Photograph showing red ring formation in the direct TTC assay [from left to right (a) media control tube, (b) growth control tube, (c) isoniazid resistant and (d) rifampicin resistant].
Direct MODS assay utilizes the principle of direct microscopic observation of MTB cords (serpentine arrangement of MTB), which could be seen in relatively few hours or days before the production of formazan crystals, producing much faster results than the direct TTC assay.13 In this study, direct MODS assay could provide a sensitivity of 98% and specificity of 87.8% (when compared to indirect LJ PM) for INH, 99.5% and 75% for RIF, respectively, and 99% and 90.5% for both INH and RIF, respectively. The overall sensitivity and specificity of direct MODS assay was 98.8% and 84.4% for the detection of drug resistant MTB isolates, in line with previous reports wherein the sensitivity and specificity ranged between 85% and 100%.20 Further, contamination of direct MODS assay (6.4%) was moderately higher when compared to Indirect LJ PM (4.9%), not statistically significant (p = 0.57, Fisher's exact test), underscores the role of MODS assay in routine drug susceptibility testing.13, 27 Furthermore, it is evident from Table 3, Table 4, the lower overall performance of direct MODS assay compared to direct TTC assay due to the detection of fewer false-positive resistant cases. These false-positive results may happen if artifacts are interpreted as cords or may be due to the growth of NTM.27 However, false-positive results produced by the growth of NTM may be overcome by the addition of a well with a PNB, a reagent that inhibits the growth of MTB but not atypical mycobacteria.28 The other advantages of MODS assay are reduced incubator space (single 24-well tissue culture plate is adequate for four sputum specimens) and decreased median time to detection (median time to detection was seven days). However, the use of MODS assay may be limited when compared to direct TTC assay due to its lower technical performance, comparatively expensive (∼39 RS, excluding instrument cost, electricity charge, labor charges – data not shown) than direct TTC assay and indirect LJ proportion method (∼16 Indian rupees excluding bottle charge, electricity, and labor charges), require use of inverted microscope to interpret the results, and continuous monitoring of the culture plates for the formation of mycobacterial cords.
In conclusion, direct TTC and direct MODS assays may be used for effective and accurate detection of isoniazid and rifampicin resistance directly from ZN smear positive sputum samples. These alternative methods seem to have the potential to provide rapid detection of resistance to isoniazid and rifampicin when compared to indirect LJ PM (technically exacting, cumbersome, and time devouring) and could be implemented in laboratories with limited resources. However, MODS assay is relatively costly and require use of inverted microscope. On the other hand, the direct TTC assay was found to be an economical alternative method (easy to perform, do not require any special instrumentation, easy to interpret the results) for the rapid and accurate detection of INH and RIF resistance (with higher sensitivity and specificity) from direct AFB smear positive sputum specimens when compared to direct MODS assay and Indirect LJ PM.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
We appreciate Mr. Gulabh Singh, laboratory technician, for his excellent technical support, and the non-technical Staff for assisting in sputum collection and transportation.
References
- 1.World Health Organization (WHO) 2014. Global tuberculosis report. Available from: http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf. [Google Scholar]
- 2.Center of Disease Control and Prevention . 2006. Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs-worldwide, 2000–2004. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5511a2.htm. [PubMed] [Google Scholar]
- 3.Shah N.S., Wright A., Bai G.H.<ET-Al>. Worldwide emergence of extensively drug-resistant tuberculosis. Emerg Infect Dis. 2007;3:380–387. doi: 10.3201/eid1303.061400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Revised National Tuberculosis Control Programme . Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare; New Delhi, India: 2009. Manual for laboratory technicians [Online] Available from: http://www.tbcindia.nic.in/documents.html. [Google Scholar]
- 5.Stop TB Partnership The Global Plan to Stop TB, 2006–2015. Actions for life: towards a world free of tuberculosis. Int J Tuberc Lung Dis. 2006;3:240–241. [PubMed] [Google Scholar]
- 6.Kent P.T., Kubica G.P. Department of Health and Human Services/Centers for Disease Control and Prevention; Atlanta: 1985. Public health mycobacteriology – a guide for the level III laboratory. [Google Scholar]
- 7.Gazi M.A., Islam M.R., Kibria M.G., Mahmud Z. General and advanced diagnostic tools to detect Mycobacterium tuberculosis and their drug susceptibility: a review. Eur J Clin Microbiol Infect Dis. 2015;5:851–861. doi: 10.1007/s10096-014-2306-5. [DOI] [PubMed] [Google Scholar]
- 8.Libonati J.P., Stager C.E., Davis J.R., Siddiqi S.H. Direct antimicrobial drug susceptibility testing of Mycobacterium tuberculosis by the radiometric method. Diagn Microbiol Infect Dis. 1988;1:41–48. doi: 10.1016/0732-8893(88)90125-3. [DOI] [PubMed] [Google Scholar]
- 9.Goloubeva V., Lecocq M., Lassowsky P., Matthys F., Portaels F., Bastian I. Evaluation of mycobacteria growth indicator tube for direct and indirect drug susceptibility testing of Mycobacterium tuberculosis from respiratory specimens in a Siberian prison hospital. J Clin Microbiol. 2001;4:1501–1505. doi: 10.1128/JCM.39.4.1501-1505.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mokrousov I., Otten T., Vyshnevskiy B., Narvskaya O. Allele-specific rpoB PCR assays for detection of rifampin-resistant Mycobacterium tuberculosis in sputum smears. Antimicrob Agents Chemother. 2003;7:2231–2235. doi: 10.1128/AAC.47.7.2231-2235.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chauca J.A., Palomino J.C., Guerra H. Evaluation of the accuracy of the microplate Alamar Blue assay for rapid detection of MDR-TB in Peru. Int J Tuberc Lung Dis. 2007;7:820–822. [PubMed] [Google Scholar]
- 12.Raut U., Rantai S., Narang P., et al. Comparison of the 3-(4,5-dimethylthiazole-2-yl)-2,5-diphenyltetrazolium bromide tube method with the conventional method and real-time polymerase chain reaction for the detection of rifampicin resistance in Mycobacterium tuberculosis. Indian J Med Microbiol. 2012;1:81–84. doi: 10.4103/0255-0857.93047. [DOI] [PubMed] [Google Scholar]
- 13.Caviedes L., Lee T.S., Gilman R.H., et al. Rapid efficient detection and drug susceptibility testing of Mycobacterium tuberculosis in sputum by microscopic observation of broth cultures. The Tuberculosis Working Group in Peru. J Clin Microbiol. 2000;38:1203–1208. doi: 10.1128/jcm.38.3.1203-1208.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angeby K.A., Klintz L., Hoffner S.E. Rapid and inexpensive drug susceptibility testing of Mycobacterium tuberculosis with a nitrate reductase assay. J Clin Microbiol. 2002;40:553–555. doi: 10.1128/JCM.40.2.553-555.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin A., Camacho M., Portaels F., Palomino J.C. Resazurin microtiter assay plate testing of Mycobacterium tuberculosis susceptibilities to second-line drugs: rapid, simple, and inexpensive method. Antimicrob Agents Chemother. 2003;47:3616–3619. doi: 10.1128/AAC.47.11.3616-3619.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banfi E., Scialino G., Monti-Bragadin C. Development of a microdilution method to evaluate Mycobacterium tuberculosis drug susceptibility. J Antimicrob Chemother. 2003;52:796–800. doi: 10.1093/jac/dkg439. [DOI] [PubMed] [Google Scholar]
- 17.Mohammadzadeh A., Farnia P., Ghazvini K., Behdani M., Rashed T., Ghanaat J. Rapid and low-cost colorimetric method using 2,3,5-triphenyltetrazolium chloride for detection of multidrug-resistant Mycobacterium tuberculosis. J Med Microbiol. 2006;55:1657–1659. doi: 10.1099/jmm.0.46442-0. [DOI] [PubMed] [Google Scholar]
- 18.Farnia P., Masjedi M.R., Mohammadi F., et al. Colorimetric detection of multidrug-resistant or extensively drug-resistant tuberculosis by use of malachite green indicator dye. J Clin Microbiol. 2008;46:796–799. doi: 10.1128/JCM.01435-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katoch V.M. Newer diagnostic techniques for tuberculosis. Indian J Med Res. 2004;4:418–428. [PubMed] [Google Scholar]
- 20.Bwanga F., Hoffner S., Haile M., Joloba M.L. Direct susceptibility testing for multidrug resistant tuberculosis: a meta-analysis. BMC Infect Dis. 2009;1:67. doi: 10.1186/1471-2334-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bwanga F., Haile M., Joloba M.L., Ochom E., Hoffner S. Direct nitrate reductase assay versus microscopic observation drug susceptibility test for rapid detection of MDR-TB in Uganda. PLoS ONE. 2011;6:e19565. doi: 10.1371/journal.pone.0019565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO) Global Tuberculosis Programme; Geneva, Switzerland: 1998. Laboratory services in tuberculosis control. Part III. Culture. Available from: http://wwwn.cdc.gov/dls/ila/documents/lstc3.pdf. [Google Scholar]
- 23.Rao S. Tuberculosis and patient gender: an analysis and its implications in tuberculosis control. Lung India. 2009;2:46–47. doi: 10.4103/0970-2113.48897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shinu P., Nair A., Singh V., Kumar S., Bareja R. Evaluation of rapid techniques for the detection of mycobacteria in sputum with scanty bacilli or clinically evident, smear negative cases of pulmonary and extra-pulmonary tuberculosis. Mem Inst Oswaldo Cruz. 2011;5:620–624. doi: 10.1590/s0074-02762011000500016. [DOI] [PubMed] [Google Scholar]
- 25.Shinu P., Singh V., Nair A., Mehrishi P., Mehta S., Joshi E. Application of cetylpyridinium chloride and sodium chloride decontamination method for recovery of Mycobacterium tuberculosis from clinically suspected cases of pulmonary tuberculosis. Diagn Microbiol Infect Dis. 2013;77:150–157. doi: 10.1016/j.diagmicrobio.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization (WHO) 2008. Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. Available from: http://whqlibdoc.who.int/publications/2008/9789241547581_eng.pdf. [PubMed] [Google Scholar]
- 27.Mello F.C., Arias M.S., Rosales S., et al. Clinical evaluation of the microscopic observation drug susceptibility assay for detection of Mycobacterium tuberculosis resistance to isoniazid or rifampin. J Clin Microbiol. 2007;10:3387–3389. doi: 10.1128/JCM.00580-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma B., Pal N., Malhotra B., Vyas L. Evaluation of a rapid differentiation test for Mycobacterium tuberculosis from other mycobacteria by selective inhibition with p-nitrobenzoic acid using MGIT 960. J Lab Physicians. 2007;2:89–92. doi: 10.4103/0974-2727.72157. [DOI] [PMC free article] [PubMed] [Google Scholar]