Abstract
Antiretroviral therapy has increased the survival of patients with HIV/AIDS, thus necessitating health promotion practice with immunization. Vaccines are critical components for protecting people living with HIV/AIDS (PLWHA). The purpose of study was to analyze the vaccination status of PLWHA in outpatient care in Fortaleza, Ceará, Brazil. Cross-sectional study performed from June 2014 to June 2015. The screening was done with patients in antiretroviral therapy, 420 patients underwent screening, but only 99 met the inclusion criteria. Data were collected for interviews using forms to characterize sociodemographic, clinical and vaccination situations. Only 14 patients had complete vaccination schedules. The most used vaccines were hepatitis B, influenza vaccine and 23-valent pneumococcal. There was no difference between men and women regarding the proportion of PLWHA with full vaccination schedule or between sex, skin color, marital status, sexual orientation, religion or occupational status. There was no difference between having or not having a complete vaccination schedule and age, years of education, family income or number of hospitalizations. CD4+ T-cells count of patients with incomplete immunization was lower than patients with complete immunization. Health education strategies can be done individually or in groups to explain the importance of vaccination and to remind about doses to be administered. Most patients did not have proper adherence to vaccination schedules, especially due to lack of guidance. Results implied that education in health is important for vaccination adhesion, knowledge of adverse events and continuation of schemes.
Keywords: Acquired immunodeficiency syndrome, HIV, Health promotion, Immunization, Immunization schedule
Introduction
More than three decades after the recognition of acquired immunodeficiency syndrome (AIDS), the pandemic of human immunodeficiency virus (HIV) infection has had changes in its characteristics.1, 2 There was a reduction in the number of new infections and deaths by HIV/AIDS at the global level, due to the significant progress in preventing the spread of infection and an increase in the number of people who have access to antiretroviral therapy (ART).3
ART has increased the survival of people living with HIV/AIDS (PLWHA) leading to a chronic disease characteristic, and it is considered that health promotion practices have become of great importance for these patients who require specialized care to maintain their quality of life. A health promotion practice that may be considered is immunization. PLWHA should weigh the benefits and risks of vaccines, by analyzing the viral load and CD4+ T-cells count, because vaccines have an important role as they can protect against opportunistic diseases.4
Vaccines are critical components for protecting HIV-infected adults from an increasing number of preventable diseases. However, missed opportunities for vaccination among PLWHA persist, likely due to concerns regarding the safety and efficacy of vaccines, as well as the changing nature of vaccine guidelines.5
The National Immunization Program (NIP) of the Ministry of Health of Brazil provides free vaccines to children, adolescents, adults and seniors. PLWHA use the same standardized vaccination schedule for adults, with adjustment according to the type of vaccine. Regarding vaccines produced from non-living microorganisms, the Ministry of Health of Brazil recommends the following vaccines: diphtheria and tetanus (adult double), hepatitis A, hepatitis B, influenza, pneumococcal 23-valent and anti-rabies. For yellow fever vaccine, individualize the risk/benefit as the patient's immune status and the epidemiological situation in the region and, in the event of exposure, vaccinate when CD4+ T-cells count >200 cells/mm3. The rabies vaccine is only administered in possible cases of exposure to the virus, when there is injury by animals. In addition, before hepatitis B vaccination the result of the anti-HBS exam must be observed.6
Several considerations justify conducting a study involving immunization of people with HIV/AIDS. The first is that prevention of infectious diseases is important when there is impaired immunity because infection causes high morbidity and mortality in these individuals. Although ART has provided an increased survival rate of people with HIV, virus infection is still a serious public health problem. This is a challenge in many ways, but above all the absence of an effective treatment that leads to healing, beyond social and economic barriers that interfere with adherence to treatment regimen.
Thus, the purpose of this study was to analyze the vaccination status of PLWHA in outpatient care, monitoring the vaccination status, identifying the vaccination card of administered biopharmaceuticals to patients and the delay in doses, the reasons why patients do not adhere to the prescribed vaccination schedules and to indicate educational strategies that can be used in health promotion practices in the context of PLWHA immunization. The results that may be obtained will guide health promotion practices related to immunization of people with HIV, and this may identify factors that prevent vaccination, as well as to create a routine check of vaccination cards, to observe the doses of immunobiologicals already administered and indicate the pending doses.
Methods
A cross-sectional descriptive study with quantitative approach, developed in Brazil with PLWHA assisted in outpatient care from June 2014 to June 2015 with screening of all PLWHA on ART who attended the service.
Inclusion criteria were patients of both sexes; age greater than or equal to 18; ART for at least three months; taking any vaccine after knowledge of positive HIV serology; having a vaccination card to verify immunobiological administration and signature of informed consent. Exclusion criteria consisted of the presence of mental disease or any other condition that would interfere with the individual's participation in the research. Other exclusion criteria were: expression of desire to no longer participate in the study and follow-up loss.
Patients were invited to participate in the study when they came to routine appointments at the clinic, which happens on average of every three months. Those who agreed to participate formalized acceptance by signing the consent form and underwent an interview lasting an average of half an hour in a private environment. Two instruments were used in the interview: Sociodemographic and Clinical Characterization Form for People with HIV/AIDS and the Vaccination Situation of People with HIV/AIDS Form. The researchers involved in the project advised patients during the study to bring their vaccination card to the clinic.
The Sociodemographic Characterization Form included the variables: identification, contact telephone number, address, date of birth, sex, skin color, schooling (in years), marital status, exposure category, sexual orientation, if they were living with their partner, current partner's HIV serology, number of children, religion, occupational status, number of people living in the same household, monthly income of the family, HIV infection diagnosis time, previous/opportunistic diseases, ART characteristics (usage time, antiretroviral drugs, dosage, number of pills), number of hospitalizations by complications of HIV infection, CD4+ T-cells count and viral load. This form has already been validated and used in other studies involving PLWHA.7, 8, 9
The Vaccination Situation of People with HIV/AIDS Form was developed and validated specifically for this study. Before being applied to the sample of the survey, a pilot test was conducted with 20 PLWHA who did not compose the sample. It is a purely descriptive tool, aiming only to collect data from patients’ vaccination card, since the vaccination card is a document that must remain with the patient. It contains the names of all vaccines recommended for PLWHA with a checklist of the administered doses. From this, the vaccination schedule was classified as complete or incomplete. In addition, there is space to put the reasons why a patient has not taken the vaccine.
Quantitative variables (continuous and discrete) were initially analyzed by the Kolmogorov–Smirnov test to verify the normality of distribution. For descriptive statistics, they calculated the mean and standard deviation (SD) (parametric data) or the median, interquartile range and minimum and maximum values (nonparametric data). Comparisons between the strata related to participants with complete and incomplete immunization were made by using the t-test for unpaired variables (parametric data) or Mann–Whitney test (non-parametric variables).
For the nominal qualitative variables, descriptive statistics involved the calculation of absolute and relative frequency. The association between the independent variables (gender, skin color, marital status, sexual orientation, religion, employment status) and the situation of the vaccine program was tested by chi-square test or Fisher's exact test (binary variables). A significance level of 0.05 (5%) was established in all analyzes, and considered statistically significant when p value was less than 0.05. The SPSS software version 19.0 for Windows (Statistical Package for Social Sciences, SPSS Inc., Chicago, Illinois, USA, 2010) was used to perform the statistical procedures. The graphics were prepared using the GraphPad PRISM® software version 5.00 for Windows (GraphPad Software, San Diego, CA, USA, 2007).
The project was submitted to the Ethics Committee of Federal University of Ceará and approved on 02.27.2014 under protocol No. 543745. All participants signed the informed consent. The secrecy of the participant's identification was maintained and the research data was used only for scientific purposes.
Results
All PLWHA in ART that are attended at the clinic passed the initial screening, which recorded 420 patients. Only 99 had their vaccination card with their administered immunobiological registered, as it was the hardest inclusion criteria to meet. When considering the 99 patients with vaccination cards, only 14 had a complete vaccination course record. Table 1 shows the total number of vaccine doses administered to PLWHA. Considering the vaccine against diphtheria and tetanus, 52 people (52.6%) had not taken at least one dose. As for a vaccine against hepatitis B, only 22 individuals (22.2%) did not have doses on record. Most of the PLWHA (71.8%) had taken the annual dose of influenza vaccine. For the 23-valent pneumococcal vaccine, only 35 patients had taken the first dose. Most individuals had not taken the double viral (measles and rubella) (98.9%), measles, mumps, or rubella (MMR) (83.8%), and only seven PLWHA had record of a yellow fever vaccine (Table 1).
Table 1.
Total vaccine doses for people living with HIV/AIDS in outpatient care (N = 99).
| Vaccines | Total doses, N (%) |
|---|---|
| Non-living microorganism vaccine Diphtheria and tetanus | |
| No doses registered | 52 (52.6) |
| 1st dose | 16 (16.1) |
| 1st and 2nd dose | 5 (5.1) |
| 1st, 2nd and 3rd dose | 18 (18.1) |
| 1st, 2nd and 3rd dose and reinforcement | 8 (8.1) |
| Hepatitis B | |
| No doses registered | 22 (22.2) |
| 1st dose | 7 (7.1) |
| 1st and 2nd dose | 10 (10.1) |
| 1st, 2nd and 3rd dose | 60 (60.6) |
| Influenza | |
| No doses registered | 28 (28.2) |
| Single dose | 71 (71.8) |
| 23-valent pneumococcal | |
| No doses registration | 64 (64.7) |
| 1st dose | 35 (35.3) |
| Live and attenuated vaccines Measles and rubella | |
| No doses registration | 98 (98.9) |
| 1st dose | 1 (1.1) |
| Measles, mumps, and rubella (MMR) | |
| No doses registered | 83 (83.8) |
| 1st dose | 16 (16.2) |
| Yellow fever | |
| No doses registered | 92 (92.9) |
| 1st dose | 7 (7.1) |
The high rates of vaccination against hepatitis B and influenza occur because these two vaccines in Brazil are highly recommended for vulnerable populations such as the PLWHA. These two vaccines are offered free of charge to the population such as other vaccines recommended by the immunization schedule in the country, but also annual campaigns against influenza still occur.
Table 2 shows the associations between sociodemographic variables and the situation of complete and incomplete immunization. No statistically significant differences were found between men and women regarding the proportion of patients with complete vaccination schedule and between sex (p = 0.220), skin color (p = 0.434), marital status (p = 0.573), sexual orientation (p = 0.139), religion (p = 0.942) or occupational status (p = 0.638), showing that for this sample, these variables do not interfere with PLWHA following up at an outpatient clinic to complete their immunization schedule (Table 2).
Table 2.
Association between the situation of complete or incomplete immunization and sociodemographic variables.
| Sociodemographic variables | Situation of vaccination schedule |
p valuea | |
|---|---|---|---|
| Complete, N (%) | Incomplete, N (%) | ||
| Sex | |||
| Male | 7 (10.6%) | 59 (89.4%) | 0.220a |
| Female | 7 (21.2%) | 26 (78.8%) | |
| Skin color | |||
| White | 2 (6.9%) | 27 (93.1%) | 0.434b |
| Brown | 8 (17.4%) | 38 (82.6%) | |
| Black | 3 (23.1%) | 10 (76.9%) | |
| Another | 1 (9.1) | 10 (90.9%) | |
| Marital status | |||
| Single | 4 (11.1%) | 32 (88.9%) | 0.573b |
| Married | 9 (18.4%) | 40 (81.6%) | |
| Separate | 1 (12.5%) | 7 (87.5%) | |
| Widower | 0 (0.0%) | 6 (100.0%) | |
| Sexual orientation | |||
| Heterosexual | 12 (19.0%) | 51 (81.0%) | 0.139b |
| Homosexual | 2 (8.7%) | 21 (91.3%) | |
| Bisexual | 0 (0.0%) | 13 (100.0%) | |
| Religion | |||
| Catholic | 9 (13.0%) | 60 (87.0%) | 0.942b |
| Protestant | 3 (16.7%) | 15 (83.3%) | |
| Spiritualist | 0 (0.0%) | 1 (100.0%) | |
| Other | 0 (0.0%) | 1 (100.0%) | |
| Without religion | 2 (20.0%) | 8 (80.0%) | |
| Occupational status | |||
| Employee | 7 (12.5%) | 49 (87.5%) | 0.638b |
| Unemployed | 3 (11.5%) | 23 (88.5%) | |
| Retired | 3 (30.0%) | 7 (70.0%) | |
| Removed | 1 (16.7%) | 6 (83.3%) | |
Fisher's exact test.
Chi-square test.
The comparative analysis of participants age was stratified according to the situation of the full vaccination schedule (N = 14) and incomplete (N = 85). No statistically significant difference (p = 0.253) was found between the age of patients with complete (mean ± SD: 42.8 ± 13.6 years) and incomplete (mean ± SD: 39.4 ± 9.8 years) vaccination schedule. The t-test for unpaired data was used to compare the two strata. Regarding the number of years of study, there was also no statistically significant difference (p = 0.109) between the complete (mean ± SD: 11.8 ± 5.2 years) and incomplete (mean ± SD: 14.2 ± 5.2 years) vaccination schedule.
The Mann–Whitney test was used for comparative analysis of family income of stratified participants according to the situation of the vaccination schedule. There was no statistically significant difference (p = 0.376) between the family income of the patients with complete immunization schedule (minimum, 25th percentile, median, 75th percentile, maximum: US$ 40.00; 241.00; 466.00; 750.00; 8.333.00) and incomplete (US$ 0.00; 320.00; 583.00; 833.00; 6.666.00).
The Mann–Whitney test was also applied for the number of admissions of patients stratified according to the situation of the vaccination schedule, and no statistically significant difference (p = 0.462) was found for the complete vaccination schedule (minimum, 25th percentile, median, percentile 75, maximum: 0.0; 0.0; 0.0; 2.0; 3.0) and incomplete (0.0; 0.0; 0.0; 1.0; 4.0).
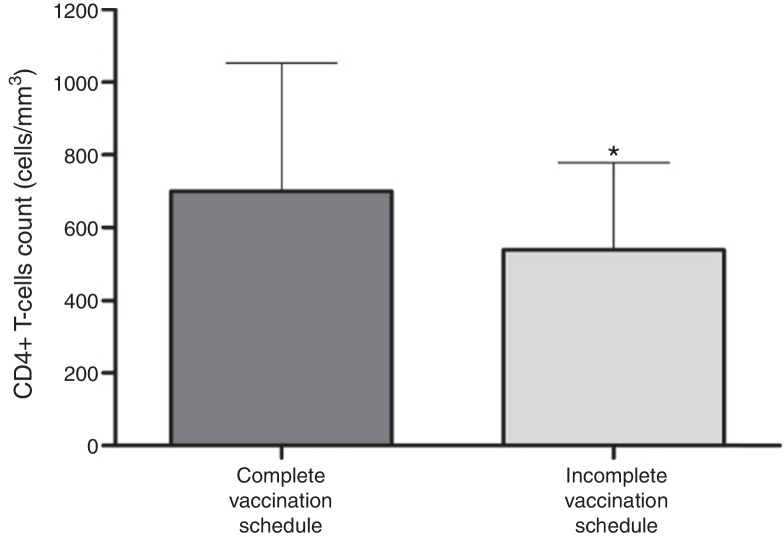
However, in the comparative analysis of the stratified CD4+ T-cells count of participants in according to the situation of vaccination card using the t-test for unpaired data, it was observed that the number of CD4+ T-cells count observed in the patients with incomplete immunization (538.0 ± 240.9 cells/mm3) was significantly lower (p = 0.034) that the observed in subjects with complete immunization schedules (699.0 ± 354.6 cells/mm3) (Fig. 1).
Fig. 1.
CD4+ T-cells count of participants stratified according to the situation of vaccination schedule. T-test for unpaired data was used to compare the two strata. CD4+ T-cells count of patients with incomplete immunization (538.0 ± 240.9 cells/mm3) was lower (*p = 0.034) than subjects with complete vaccination schedule (699.0 ± 354.6 cells/mm3).
The reasons for the 85 PLWHA not adhering to the prescribed vaccination schedules were surveyed. Reasons for not adhering to the prescribed vaccination schedule were: They were not instructed as to the number of doses of vaccines and schema (63.5%), do not know the benefits of the vaccine (16.5%), do not tolerate invasive procedures (injections) (8.2%), have no time to seek health service that administers vaccines (7.1%), and have no financial resources to attend the health service (4.7%).
It should be emphasized the importance of the participation of all members of the multidisciplinary team in health education process, which includes doctors, nurses, pharmacists, dietitians, physical therapists and other professionals who care holistically the patient. The standardization of conduits during patient care is essential to a quality health care, especially considering patients with low education and insufficient income, which may hamper the access of individuals to health services in general.
Discussion
Vaccination is important to improve immunity against opportunistic infections.10 For PLWHA, a vaccination schedule involves vaccines produced from non-living microorganisms: diphtheria and tetanus (three doses and booster every 10 years), hepatitis B (four doses, 0, 1, 2, 6 or 12 months), influenza (annual), 23-valent pneumococcal (single and booster dose after five years); and vaccines for live attenuated microorganisms, which require analysis of CD4+ T-cells count and viral load due to immunosuppression: measles, mumps and rubella (one dose and may be monovalent, double or MMR) and yellow fever.4, 10
For vaccines made from live microorganisms, the indication is based on CD4+ T-cells count (cells/mm3), and a number greater than 350 (≥20%) indicates vaccines; for between 200 and 350 (15-19%), it is necessary to evaluate clinical and epidemiological risks for decision-making; less than 200 (<15%), it is recommended that they do not vaccinate. Vaccination in symptomatic patients or with severe immunodeficiency should be delayed until satisfactory degree of immune reconstruction with ART in order to improve the vaccine response and reduce the risk of post-vaccination complications. Vaccines produced from live microorganisms that are recommended: measles, mumps and rubella – they are not indicated for patients with severe immune deficiency; yellow fever vaccine – has not been established as safe or effective in people with HIV, also CD4+ T-cells count (cells/mm3) and epidemiological risk situation should be observed; BCG – a second dose of vaccine has been contraindicated since 2006, but is indicated for leprosy contacts after health assessment. Symptomatic or asymptomatic PLWHA with CD4+ T cells count less than 200/mm3 must not be vaccinated.6
Studies about immunization of PLWHA are important, however, there is little Brazilian research on it. Research shows a low prevalence of seroprotection against diphtheria, poliomyelitis, tetanus and hepatitis B in migrants with HIV/AIDS that live in France and travel to their native countries, as they need to have their vaccine schedule completed.11 Furthemore, fear of contamination and stigmatized social attitude are main impediments to dealing with patients and providing services to them. It seems that creating effective knowledge about transmission and correcting the socio-cultural beliefs of health providers are key strategies to tackle this problem.12
There was a great number of PLWHA without a vaccination card. This was demonstrated by the number of patients who went through the screening, but were not included in the study. These patients had no vaccination card, so in addition to not remembering exactly which vaccinations and doses have been taken, they still did not have a record. The unavailability of the vaccination card is a common finding, showing that people do not have the habit of keeping their vaccination cards as a document.
The hepatitis B vaccine was administered to more PLWHA. Research has shown that this vaccine is important for individuals with HIV/AIDS, for the prevention of liver diseases due to infection from the hepatitis B virus, and may also have prognostic value in predicting the progression of HIV infection, given that it stimulates immune response.13, 14 From 1999 to 2011, there were 120,343 reported cases of hepatitis B in Brazil, and the rate increased from 0.3% in 1999 to 6.9% in 2010. Sexual contact is the predominant mean of transmission (52.7%). PLWHA are considered highly vulnerable to hepatitis B, and for this reason, the vaccination is highly recommended for this population. However, further studies are needed to estimate the co-infection rate of HIV/hepatitis B in the Brazilian population.15
For all people, including those living with HIV/AIDS, diphtheria and tetanus after the full course of three doses may be repeated every 10 years, as reinforcement.4 However, despite this vaccine being available for free, few PLWHA had it recorded on their card.
Regarding the influenza vaccine, most people had taken the single annual dose. In July, 2009, cases of sustained transmission of influenza A (H1N1) were confirmed in all regions of Brazil. Many patients presented pulmonary complications, especially children, pregnant women, obese people and those with comorbidities, such as diabetes, hypertension, cardiovascular disease, immunodeficiencies and malignancies. Thus, the Brazilian Ministry of Health annually conducts influenza vaccination campaigns in priority groups, including PLWHA, which explains the large number of doses administered in this population.16 Influenza vaccination is shown as one of the most effective measures for prevention of severe influenza and its complications. Currently in Brazil, vaccines contain antigens against three influenza strains: A (H1N1), A (H3N2) and B. These strains are chosen each year in order to prevent disease caused by strains that will circulate the following season.17 However, research is needed to estimate the co-infection rate of PLWHA/influenza in Brazilian population. PLWHA are more likely to have severe and prolonged infections from the influenza virus. The use of ART has decreased the rate of influenza complications in HIV-infected individuals. As a result, treatment guidelines recommend an annual influenza vaccination for all PLWHA.18, 19
On the yellow fever vaccine, another study also showed the unfamiliarity of PLWHA on vaccines. Although most participants adequately ascertain the vaccine as the main prevention strategy against yellow fever, few were not aware of the severity and lack of specific treatment for yellow fever, so that some patients have not taken the vaccine when indicated.20 To assure maximum effectiveness yellow fever vaccine should be given to HIV-infected patients after HIV replication has been suppressed.21
The administration of live attenuated vaccines in patients with immune deficiency should be subject to individual risk-benefit analysis and not be performed in cases of severe immunosuppression.4 Perhaps this explains the fact that very few patients had records of these biopharmaceuticals on their vaccination cards. For the comparative analysis of CD4+ T-cells count of the participants, it was observed that the number of CD4+ T-cells count of the PLWHA with incomplete immunization was significantly lower than that observed in subjects with a complete vaccination schedule. No articles were found in the literature to observe this relationship. However, some inferences can be made. The first is that to have a complete immunization schedule can demonstrate interest on the part of PLWHA in maintaining good health practices, especially so that this individual may have a greater concern with self-care. The second inference is that because it seems closer to health care, it is possible that these PLWHA with a full vaccination schedule must also have adequate adherence to ART, which in turn causes the CD4+ T-cells count to increase, the viral load to decrease, and thus the immune system stays in proper condition to receive biopharmaceuticals. It is noteworthy that all selected patients for this study were using ART as this was one of the inclusion criteria, also being a criterion for indication of vaccines.
The use of ART protects PLWHA against diseases and improves the immune response to vaccines, so the use of ART is always observed, representing a security policy when prescribing vaccines. It is noteworthy that vaccinations can cause temporary changes in the viral load of HIV-1. Thus, routine tests should not coincide with vaccination and should be made at least 30 days after receiving the vaccines.4, 10, 19
Most patients did not take vaccines because they are not directed to do so by health professionals. Therefore, health education strategies can be done individually or in a group in order to explain the importance of vaccination for patients and remind them about the doses to be administered. Health education is an essential factor in the vaccination room for those individuals to return to complete the dosing schedules. However, health education is still something that is lacking due to overwhelming demand in the vaccine area, resulting in an overload of work for professionals who work in it.
From the findings of this research, some strategies can be recommended for health promotion in the context of the immunization of PLWHA. The first is to provide further guidance about the number of vaccine doses and the importance of completing the vaccination schedules in order to have adequate immunization, as well as to promote the benefits of the vaccine, either through individual or group educational strategies. The professional who prescribes vaccines for PLWHA should also stay tuned to their specifications, through the analysis of CD4+ T-cells count and viral load, so that all patients can be awarded the benefits of vaccination.
In this context, immunization is a strategy to promote health and disease prevention, therefore advising on its benefits, indication, number of doses and adverse events is of utmost importance for proper immunization of the entire population. With the participation of members of the health team, the immunization process of the population becomes more effective and comprehensive, so the National Immunization Program may effectively fulfill its role, being the control, elimination and eradication of immunopreventable diseases of interest in Brazilian and International Public Health.
Regarding the limitations of the study, the main difficulty was to find PLWHA that possessed the vaccination card, which interfered in the sample being completed. Despite wide dissemination of the study, many patients showed no vaccination card. They reported the card lost, forgotten or just did not have it. A strategy that can be used in future studies regarding this topic is to provide financial assistance for patients to return to the clinic to present their vaccination card, as PLWHA have financial difficulties.
Conclusion
To conclude, only a few PLWHA considered it important to have their vaccination cards. Most did not properly adhere to the prescribed vaccination schedules, primarily due to lack of guidance on the subject, requiring health education to cover these aspects. The evaluated sociodemographic variables did not interfere in the patients fulfilling their vaccination schedules. Thus, it emphasizes the importance of this work, as it has identified deficits related to the care of patients about immunization and the health service on the guidelines of vaccines. Moreover, it was observed from the data analysis that the CD4+ T-cells count was lower in patients with incomplete immunization, so the conclusion was that this could be related to a deficit in self-care or inadequate adherence to ART.
For this reason, some procedures could have been performed to confirm this inference, such as the analysis of self-care and adherence to ART through scales. As this was not done in this work, it is suggested as a subject matter for further research. Another aspect that could have helped would be the existence of a computerized system at the study site, so as to notify the vaccinated and unvaccinated PLWHA treated at the outpatient service. This suggestion will be taken to the hospital where the study was conducted, with a view of future implementation in the service.
The study results implied that education in health is important for adherence to vaccinations, knowledge of adverse events and continuation of schemes, and that health professionals have essential action in this process, because they accompany the patients. It emphasizing also the importance of educational practices in the outpatient setting, especially those that promote health, and thus guide PLWHA to be able to self-care since there is still no cure for HIV/AIDS. Public policies exist and they are very clear regarding the vaccination of PLWHA, however, health professionals need to do their role of orientation of patients, demonstrating the importance of vaccines for this population.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Alimohamadi Y., Tabatabaee H., Afsar Kazerooni P., et al. Epidemiologic characteristics of HIV-positive patients referring to behavioral diseases consultation center in Shiraz, Iran. Med J Islam Repub Iran. 2014;14:147. [PMC free article] [PubMed] [Google Scholar]
- 2.Castel A.D., Magnus M., Greenberg A.E. Update on the epidemiology and prevention of HIV/AIDS in the United States. Curr Epidemiol Rep. 2015;2:110–119. doi: 10.1007/s40471-015-0042-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmetagicn S., Porobić-Jahic H., Piljic D., et al. Clinical and epidemiological characteristics of HIV infection/AIDS in hospitalized patients. Mater Sociomed. 2015;27:27–30. doi: 10.5455/msm.2014.27.27-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatt B., Jindal H., Sk S., et al. Vaccination in HIV positive adults: need to address. Hum Vaccin Immunother. 2014;10:3011–3012. doi: 10.4161/21645515.2014.971645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crum-Cianflone N.F., Wallace M.R. Vaccination in HIV-infected adults. AIDS Patient Care STDS. 2014;28:397–410. doi: 10.1089/apc.2014.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health of Brazil . 2013. Clinical protocol and therapeutic guidelines for the management of HIV infection in adults. http://www.fmt.am.gov.br/layout2011/diversos/Protocolo%20Tto%20HIV%202013.pdf [accessed 04.05.14) [Google Scholar]
- 7.Cunha G.H., Galvão M.T.G. Nursing diagnoses in patients with human immunodeficiency virus/acquired immunodeficiency syndrome in outpatient care. Acta Paul Enferm. 2010;23:526–532. [Google Scholar]
- 8.Cunha G.H., Galvão M.T.G. Contraceptive and prevention methods of transmission/reinfection of the virus among patients with HIV/AIDS. Rev Rene. 2011;12:699–708. [Google Scholar]
- 9.Cunha G.H., Galvão M.T.G. Sociodemographic context of patients with HIV/AIDS attended in nursing consultation. REUOL. 2011;5:713–721. [Google Scholar]
- 10.Corre N.L., Autran B. Vaccination in HIV-infected individuals. Future Virol. 2012;7:85–102. [Google Scholar]
- 11.Mullaert J., Abgrall S., Lele N., et al. Diphtheria, tetanus, poliomyelitis, yellow fever and hepatitis B seroprevalence among HIV1-infected migrants. Results from the ANRS VIHVO vaccine sub-study. Vaccine. 2015;33:4938–4944. doi: 10.1016/j.vaccine.2015.07.036. [DOI] [PubMed] [Google Scholar]
- 12.Zarei N., Joulaei H., Darabi E., Fararouei M. Stigmatized attitude of healthcare providers: a barrier for delivering health services to HIV positive patients. Int J Community Based Nurs Midwifery. 2015;3:292–300. [PMC free article] [PubMed] [Google Scholar]
- 13.Okulicz J.F., Mesner O., Ganesan A., et al. Hepatitis B vaccine responsiveness and clinical outcomes in HIV controllers. PLOS ONE. 2014;9:e105591. doi: 10.1371/journal.pone.0105591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee H., Park W. Public health policy for management of hepatitis B virus infection: historical review of recommendations for immunization. Public Health Nurs. 2010;27:148–157. doi: 10.1111/j.1525-1446.2010.00842.x. [DOI] [PubMed] [Google Scholar]
- 15.Ministry of Health of Brazil . 2015. Epidemiological Bulletin – Viral Hepatitis Year IV – N.1. http://www.aids.gov.br/sites/default/files/anexos/publicacao/2015/58210/_p_boletim_hepatites_final_web_pdf_p__16377.pdf (accessed 05.11.15) [Google Scholar]
- 16.Del Bianco R.D., Santos M.S., Ribeiro M.C., et al. Clinical aspects of influenza A (H1N1) in HIV-infected individuals in São Paulo during the pandemic of 2009. Braz J Infect Dis. 2011;15:170–173. doi: 10.1016/S1413-8670(11)70166-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ministry of Health of Brazil . 2015. Technical Report. National vaccination campaign against influenza. http://www.infectologia.org.br/wp-content/uploads/2015/04/Informe_Cp_Influenza-_25-03-2015_FINAL.pdf (accessed 05.11.15) [Google Scholar]
- 18.Music T. Protecting patients, protecting healthcare workers: a review of the role of influenza vaccination. Int Nurs Rev. 2012;59:161–167. doi: 10.1111/j.1466-7657.2011.00961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramirez L.A., Daniel A., Frank I., et al. Seroprotection of HIV-infected subjects after influenza A (H1N1) vaccination is directly associated with baseline frequency of naive T cells. J Infect Dis. 2014;210:646–650. doi: 10.1093/infdis/jiu132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Avelino-Silva V.I., Francelino H.S., Kallás E.G. Yellow fever prevention strategies awareness among HIV-infected patients in São Paulo, Brazil. Rev Inst Med Trop São Paulo. 2014;56:417–420. doi: 10.1590/S0036-46652014000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barte H., Horvath T.H., Rutherford G.W. Yellow fever vaccine for patients with HIV infection. Cochrane Database Syst Rev. 2014;23:CD010929. doi: 10.1002/14651858.CD010929.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]