Abstract
Objective
Hand hygiene (HH) is a critical component for controlling hospital-acquired infection (HAI). The present study was designed to develop an intervention approach to improve compliance with HH among healthcare workers in a hospital setting.
Methods
The HH intervention study was conducted in Guizhou Provincial People's Hospital, Guiyang, China and organized by its Department of HAI Management. It was an observational, prospective, quasiexperimental (before-after intervention) study. The study was divided into two phases: the baseline phase and the intervention phase. The investigative team included clinical monitoring staff and infection control practitioners who received a series of instructions on HH compliance, monitoring skills, and measurement of the use of HH products.
Results
Based on 27,852 observations in a 17-month period, the rate of compliance with HH improved from 37.78% at baseline to 75.90% after intervention. Significant improvement in compliance and an increase in consumption of HH products was observed after intervention. The per patient-day consumption of alcohol-based hand rub products and handwash agents increased by 4.75 mL and 4.55 mL, respectively. The consumption of paper towels increased 3.41 sheets per patient-day. During the same period, the prevalence rate of HAI decreased 0.83%.
Conclusions
This study demonstrates that a significant improvement in compliance with HH can be achieved through a systemic, multidimensional intervention approach involving all categories of healthcare workers in a hospital setting, which may result in a decrease of the HAI rate.
Keywords: Hand hygiene, Compliance, Hospital-acquired infection
Introduction
Hospital-acquired infections (HAI) are associated with increased morbidity and mortality both in developed and developing countries, resulting in increased healthcare costs, length of hospitalization, use of drugs, and unnecessary laboratory investigations.1, 2 Several studies have reported that hand hygiene (HH) is the most important, easy, and economical measure to reduce HAI.3, 4 It has been demonstrated that enhancing HH compliance results in a reduction of HAI and antimicrobial resistance.5 However, adherence to HH recommendations among healthcare workers (HCWs) remains suboptimal, with compliance rates being 30–75% as reported in published studies.6, 7, 8 There have been limited reports on HAI and compliance with HH in China. In order to improve awareness of HAI, its prevention and control, and to increase HH compliance among HCWs, we initiated an intervention program, including HH training and monitoring. It was hoped that the hospital-wide intervention on HH compliance could be used in other hospitals in order to reduce HAI in China and in other countries as well.
Methods
The present study was conducted in Guizhou Provincial People's Hospital, Guiyang, China, organized by its Department of HAI Management and carried out between August 2012 and December 2013. The hospital-wide intervention program included the following elements: administrative support, education and training, improved supply of HH products, surveillance, and feedback.
Study population and hospital setting
The study was carried out in Guizhou Provincial People's Hospital. The hospital was founded in 1947 and earned a ranking of AAA in China's general hospital licensing and accreditation system. The hospital is located in the city of Guiyang, Guizhou Province, China. The hospital has 2000 beds, 52 clinical units or departments, and 3182 HCWs, covering an area of approximately 45,000 square meters. The present study was carried out in 33 wards of the hospital from August 2012 to December 2013.
Study design
It was an observational, prospective, quasi-experimental (before-after intervention) study. The study was divided into two phases: the baseline phase (from August 2012 to October 2012) and the intervention phase (from October 2012 to December 2013). The primary outcome variables were compliance with HH and consumption per patient-day of alcohol-based hand rub (ABHR) products, handwash agents, and paper towels. The other outcome variable was the rate of HAI.
Intervention procedures
The present intervention program included a series of measures to improve compliance with HH among HCWs hospital-wide.
The first intervention was aimed at improving HH facilities. After the baseline survey, the following changes in the HH facilities were accomplished: 150 hand twist taps were changed to non-hand twist taps; the number of dispensers for paper towels and ABHR products was increased; and all hand faucets were equipped with paper towels, put up HH posters on HH dispensers. In addition, education, training and monitoring measures were implemented.
The second part of the campaign was an aggressive education program related to HH. As part of the education program, the ICP attended all the staff meetings in all departments and provided education on proper HH techniques. Two education lectures about HH to HCWs were given at an auditorium; additionally, issues of HH education was presented to the department staff at the health care quality meeting. Educational issues related to HH were also discussed with the head nurses at the department of nursing two times; for the nurse attendants and the medical professionals HH education was carried on at the local workplace. This action had to be repeated in some wards, especially in ICU. HH video played in the hospital's promotional video.
The final part of this campaign was to strengthen the management of HH. Every quarter, the department of HAI management prepared and sent a final report on compliance with HH, and on the consumption of HH products to the hospital director and department chief. Such reports were to include information on HH compliance in examination of medical quality and presentation of the rate HH compliance to the hospital director's council. Feedback on the observed data of HH was written on a whiteboard at the ICU which could be seen every day.
Data collection
The investigation team included the clinical monitoring staff (physicians or nurses who had not only their regular clinical duties, but also responsibilities associated with HH surveillance and HAI prevention) and the infection control practitioners (ICP). During the baseline phase, ICP assessed HH compliance, then ICP completed the follow-up with the clinical monitoring staff during the intervention phase. The investigation team received standardized instructions, including the definition of HH compliance, and monitoring/recording recommendations. Before conducting observation sessions, the observer trained and must be validated, parallel observation the World Health Organization (WHO) training film. Results were then compared and discordant notifications discussed. This process was repeated until considered adequate. The observation period was from 08:00–18:00 on a work day, with each observation lasting no more than 20 min with no shift changes to avoid any impact on the results.
HH was monitored according to the WHO HH observation method. Based on the WHO guidelines, “My Five Moments for HH” (5MHH), the observers recorded the following data on paper questionnaires for each of their observations: department, time and date, HCW type, 5MHH, and HH type. The HH type was either a positive action by performing handrub or handwash, or a negative action by missing handrub or handwash. The subjects to be observed in the present study were divided into the following categories: physicians and interns (medical students and refresher doctors); nursing staff and nursing trainees (nursing students and refresher nurses); care workers (nursing assistants and other HCW); other staff and family members (including rehabilitative and therapeutic service staff, radiology technicians, and family members of patients). Observations for the 5MHH included the moment before touching the patient (bef-pat), moment before aseptic per clean procedure (bef-asept), moment after body fluid exposure risk (aft-b.f), moment after touching the patient (aft-pat), and moment after touching the patient surroundings (aft-p.surr). For instances in which opportunities involved more than one indication, only one was considered for the sake of simplicity of analysis by applying the following priority rule: bef-asept > aft-b.f > aft-pat > bef-pat > aft-p.surr.9
The team was instructed to collect at least 20 observations per inpatient department per month. The clinical monitoring nurse registered HH products consumption data monthly. All wards took part in this HH study and intervention program.
The definition of HAI was based on the criteria set by the Ministry of Health of the People's Republic of China in 2001. New infection was defined as an HAI diagnosed 48 h or longer after admission, provided that there was no evidence that the infection was sub-clinical or undiagnosed at the time of admission.
Statistical analysis
The observational data were entered into a Microsoft Excel database. Analysis was performed with Excel and IBM SPSS Statistics version 19. Frequency tables were tabulated with 95% confidence intervals. The χ2 test was used for comparison between groups and the differences were deemed statistically significant if p < 0.05.
Results
Hand hygiene compliance
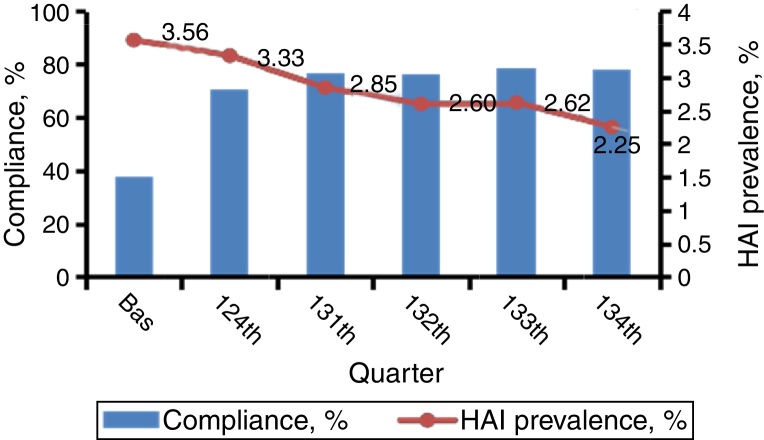
There were 27,852 unique observations over 17 months. The HH compliance rate improved from 37.78% at baseline to 75.90% after intervention (Fig. 1, Table 1). The majority of observations (33.07%) were of nursing staff, followed by physicians (27.82%), practical nurses (17.43%), interns (13.53%), and care workers (8.15%). The proportion of other staff accounted for less than 1% (0.71%) and were therefore ignored. Nursing staff was the group with the highest compliance (78.50%), and physicians (71.42%) had greater compliance than practical nurses and interns (66% and 61%, respectively). Care workers were the group with the least compliance (48.17%). HH compliance was higher aft-b.f (82.38%) than aft-pat (73.54%). Compliance was lower aft-p.surr and bef-asept (60.62% and 59.39%, respectively). The lowest compliance was seen bef-pat (58.04%). The compliance rates were statistically different before and after intervention for all categories of HCWs (p < 0.001). Regardless of the baseline survey period or intervention period, the best two moments of HH compliance were the aft-b.f moment and the aft-pat moment. Gratifyingly, the bef-pat moment improved the most after intervention.
Fig. 1.
HH compliances and prevalence rates of HAI.
Table 1.
Compliance with HH before and after intervention.
| Time | No. of HH opportunities | Compliance, % | 95% CI |
p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Bas | 1266 | 37.78 | 18.68 | 25.86 | <0.001 |
| Int | 26,586 | 75.90 | 62.64 | 66.92 | |
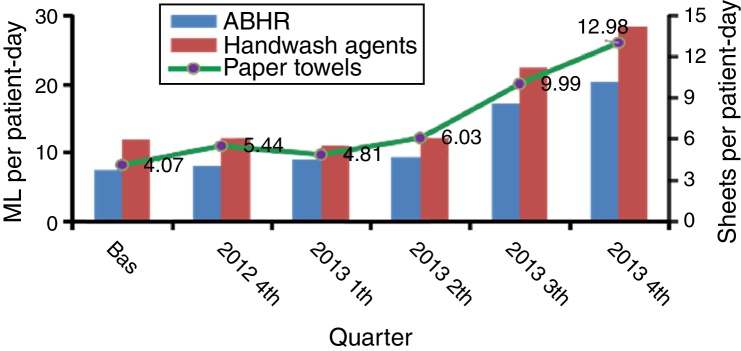
Consumption of HH products
Average ABHR consumption increased from 7.40 mL per patient-day in the baseline period to 12.15 mL per patient-day after intervention (Fig. 2, Table 2). The handwash agent consumption increased by 38.54% from 11.80 mL per patient-day at baseline to 16.35 mL per patient-day after intervention. Paper towels were used more frequently after intervention (7.48 sheets per patient-day) than at the baseline period (4.07 sheets per patient-day) (p < 0.001).
Fig. 2.
HH agent consumption before and after intervention.
Table 2.
HH agent consumption before and after intervention.
| Variable | Time | Consumption | 95% CI |
p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| ABHR (mL per patient-day) | Bas | 7.40 | 5.69 | 9.12 | 0.004 |
| Int | 12.15 | 10.95 | 13.36 | ||
| Handwashing agents (L per patient-day) | Bas | 11.80 | 9.09 | 14.52 | 0.009 |
| Int | 16.35 | 14.27 | 18.43 | ||
| Paper towels (sheets per patient-day) | Bas | 4.07 | 3.30 | 4.85 | <0.001 |
| Int | 7.48 | 6.58 | 8.39 | ||
HAI rates
There was a significant difference in HAI rates between baseline and intervention periods (3.56%; 95% CI: 2.33–4.79 vs. 2.73%, 95% CI: 2.30–3.16, respectively; p = 0.002; Fig. 1, Table 3). The fourth quarter of 2013 was the period that registered the most sharp reduction of nosocomial infections during the study period.
Table 3.
Prevalence rates of HAI before and after HH intervention.
| Time | No. of HAI cases | HAI prevalence (%) | 95% CI |
p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Bas | 613 | 3.56 | 2.33 | 4.79 | <0.001 |
| Int | 2699 | 2.73 | 2.30 | 3.16 | |
Discussion
There are increasing efforts in developing effective measures to improve hygiene and to reduce infections in hospital settings in China. China's Ministry of Health formally promulgated the “Standard for HH for HCWs in Healthcare Settings” in 2009.10 To meet the requirements of the Ministry of Health for hospital accreditation in 2011,11 the majority of hospitals in China began to pay attention to HH in 2012. In the past, HH has not received close attention and the HH facilities were essentially lacking in our hospital; some HCWs were not aware of HH requirements and regulations. To the best of our knowledge, the present study represents the first attempt in Guizhou Province to develop an interventional approach to improve compliance with HH in a hospital setting. In the present study, the mean overall HH compliance rate improved from 37.78% in the baseline phase to 75.90% in the intervention phase. The consumption of ABHR products and handwash agents increased by 64.19% and 38.56% per patient-day, respectively. The consumption of paper towels increased by 83.78% per patient-day. As a result of the intervention, the incidence of HAI decreased from 3.56% at baseline to 2.73% after intervention.
The department of HAI management developed a series of actions to improve the medical staff's HH compliance, including improvements in HH facilities, awareness of HH, training, education, assessment, and establishment of a quality evaluation system through monitoring and feedback. In order to improve the HH facilities and make easy the access to HH instruments, our hospital changed 150 hand twist taps to non-hand twist taps, increased the number of paper towel and ABHR dispensers, and equipped all hands faucets with paper towels. ABHR was made easily available, and additional dispensers were installed on the walls in patients’ rooms, on the clinical trolley in general ward areas, and at every bedside in the intensive care unit, infectious disease wards and patient wards with other invasive operations. In all wards HH posters were affixed on HH dispenser. During December 2012, mandatory HH training was held for all HCWs according to WHO recommendations.12, 13 All staff participated in training of “how to do” and “when to do” according to WHO guidelines on HH in health care hygiene practices.9 The ICP attended all staff meetings of all departments and provided education on proper hand hygiene techniques. Education sessions of HH to different professionals were conducted in different places. After some training to enhance HH consciousness of the medical staff there was a gradual perception of the importance of such practice to patient health.
The most frequently reported methods of measuring compliance with HH are direct observation of the practice, measurement of the consumption of products used for HH, and electronic counters for dispensers of ABHR.11, 12 In the present study, the first two methods were chosen. It was useful to stratify adherence by institutional sector, professional type, and moment of HH using the “5MHH”. Feedback to the clinical departments and hospital were provided quarterly. Our study showed an increase in compliance with HH and consumption of products used in HH after intervention.
Following the intervention, there has been an overall improvement of compliance with HH of all HCWs. However, it should be pointed out that the building up of HH consciousness takes time, requires repeated training, and reminding. Timely and regular feedback might be a key factor in improving and maintaining the compliance rate. Incorporating HH into the medical quality evaluation, and feedback to the department chief attracted attention. Part of the department will formulate a punitive policy to penalize HCWs who do not perform HH, thus attracting more attention from HCWs. Feedback on the observed data of HH written on a whiteboard at the ICU can be seen every day. The HH compliance rates were analyzed according to professional category and moment category. There were far more opportunities of HH for nurses in most departments than for physicians; nurses’ HH compliance rate was higher than that of physicians and other staff. Our observations were similar to previous reports.14, 15 Care workers were mostly illiterate and the majority was not aware of the benefits of HH before the intervention. Through the intervention, their compliance with HH improved significantly, but their compliance rates were still lower than that of other professionals. Although the method of direct observation of HH has several advantages, it has a major disadvantage, which is that only a very small portion of all HH opportunities are captured besides being labor-intensive and time-consuming. Additionally, the presence of an observer may produce the Hawthorne effect.16, 17 In the future, we may use trained medical students to observe the HH compliance of medical staff to decrease the observation bias or Hawthorne effect.
In the present study, the consumption of products used for HH was monitored and ought to be in accordance with the observed HH compliance. The consumption of HH products can be affected by various factors, including the patient's condition, treatment behavior of different hospitals or departments, and number and types of HCWs. Boyce et al.18 found that the amount of ABHR used increased from 3 L/1000 patient-days to 30 L/1000 patient-days when the overall HH compliance rate among HCWs increased from a baseline level of 38% to 63% after intervention. Pittet et al.19 reported that compliance was improved progressively from 48% in 1994 to 66% in 1997 and that, during the same period, the overall nosocomial infection rate decreased from 16.9% in 1994 to 9.9% in 1998. The group also found that the methicillin-resistant Staphylococcus aureus transmission rate decreased and the hospital-wide consumption of ABHR increased from 3.5 to 15.4 L per 1000 patient-days.
HAI is an important cause of morbidity and mortality among hospitalized patients worldwide. The transmission of healthcare-associated pathogens often occurs via the contaminated hands of HCWs. HH is considered the most effective and simple measure in preventing the spread of infection and multiresistant organisms. Compliance with HH increased continuously, followed by improved HCW awareness of infection control, to achieve the original goal of infection control for reducing the incidence of HAI and the spread of pathogens.20, 21
Of note, during our monitoring in the present study, the direct observation was focused on the right time to perform HH, not the correctness of the operator, the duration and steps, or appropriateness of rubbing. The quality of HH relies on the correct operation of all procedures at the right time. If not performed correctly, the removal of transient microorganism from HCWs’ hands cannot be achieved.22 In future studies, the correctness of each HH procedure should be emphasized in observation and analysis.
In conclusion, our intervention program resulted in significantly increased compliance with HH in all categories of HCWs in our hospital. HH seems to be simple, but persistence of HH is difficult23, 24 and requires long-term commitment to change from the part of hospital administration and all HCWs and patients.
Ethical approval
The study protocol was reviewed and approved by the Institutional Review Board of Guizhou Provincial People's Hospital.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
This work was supported by the Science Foundation of Guizhou Province of China (Nos. LS[2011]026 and J[2012]2242). We would like to thank other colleagues (Guizhou Provincial People's Hospital, Guizhou, China) for the contribution to data acquisition.
References
- 1.Derde L.P., Cooper B.S., Goossens H., et al. Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis. 2014;14:31–39. doi: 10.1016/S1473-3099(13)70295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allegranzi B., Gayet-Ageron A., Damani N., et al. Global implementation of WHO's multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis. 2013;13:843–851. doi: 10.1016/S1473-3099(13)70163-4. [DOI] [PubMed] [Google Scholar]
- 3.Boyce J.M., Larson E.L., Pittet D. Hand hygiene must be enabled and promoted. Am J Infect Control. 2012;40(Suppl. 1):S2. doi: 10.1016/j.ajic.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Al-Tawfiq J.A., Pittet D. Improving hand hygiene compliance in healthcare settings using behavior change theories: reflections. Teach Learn Med. 2013;25:374–382. doi: 10.1080/10401334.2013.827575. [DOI] [PubMed] [Google Scholar]
- 5.Helms B., Dorval S., Laurent P.S., Winter M. Improving hand hygiene compliance: a multidisciplinary approach. Am J Infect Control. 2010;38:572–574. doi: 10.1016/j.ajic.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Pittet D., Simon A., Hugonnet S., Pessoa-Silva C.L., Sauvan V., Perneger T.V. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. doi: 10.7326/0003-4819-141-1-200407060-00008. [DOI] [PubMed] [Google Scholar]
- 7.Allegranzi B., Sax H., Pittet D. Hand hygiene and healthcare system change within multi-modal promotion: a narrative review. J Hosp Infect. 2013;83 (Suppl. 1):S3–S10. doi: 10.1016/S0195-6701(13)60003-1. [DOI] [PubMed] [Google Scholar]
- 8.Lee A., Chalfine A., Daikos G.L., et al. Hand hygiene practices and adherence determinants in surgical wards across Europe and Israel: a multicenter observational study. Am J Infect Control. 2011;39:517–520. doi: 10.1016/j.ajic.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Sax H., Allegranzi B., Chraiti M.N., Boyce J., Larson E., Pittet D. The World Health Organization hand hygiene observation method. Am J Infect Control. 2009;37:827–834. doi: 10.1016/j.ajic.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health of China; 2009. Standard for hand hygiene for healthcare workers in healthcare setting. [Google Scholar]
- 11.Ministry of Health of China; 2011. Evaluation standard of grade 3 general hospital. [Google Scholar]
- 12.Chou D.T., Achan P., Ramachandran M. The World Health Organization ‘5 moments of hand hygiene’: the scientific foundation. J Bone Joint Surg Br. 2012;94:441–445. doi: 10.1302/0301-620X.94B4.27772. [DOI] [PubMed] [Google Scholar]
- 13.Pittet D., Allegranzi B., Boyce J. The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30:611–622. doi: 10.1086/600379. [DOI] [PubMed] [Google Scholar]
- 14.Larson E.L. APIC guideline for handwashing and hand antisepsis in health care settings. Am J Infect Control. 1995;23:251–269. doi: 10.1016/0196-6553(95)90070-5. [DOI] [PubMed] [Google Scholar]
- 15.Allegranzi B., Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73:305–315. doi: 10.1016/j.jhin.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 16.Braun B.I., Kusek L., Larson E. Measuring adherence to hand hygiene guidelines: a field survey for examples of effective practices. Am J Infect Control. 2009;37:282–288. doi: 10.1016/j.ajic.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . 2009. WHO guidelines for hand hygiene in health care. [Google Scholar]
- 18.Boyce J.M., Ligi C., Kohan C., Dumigan D., Havill N.L. Lack of association between the increased incidence of Clostridium difficile-associated disease and the increasing use of alcohol-based hand rubs. Infect Control Hosp Epidemiol. 2006;27:479–483. doi: 10.1086/504362. [DOI] [PubMed] [Google Scholar]
- 19.Pittet D., Hugonnet S., Harbarth S., et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection control programme. Lancet. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Resendez M.F., Garza-Gonzalez E., Mendoza-Olazaran S., et al. Impact of daily chlorhexidine baths and hand hygiene compliance on nosocomial infection rates in critically ill patients. Am J Infect Control. 2014 doi: 10.1016/j.ajic.2014.03.354. [DOI] [PubMed] [Google Scholar]
- 21.Ferrelli J., DiCuccio M.H. Sustainable hand hygiene efforts; a review of a successful campaign. Infect Disord Drug Targets. 2013;13:169–176. doi: 10.2174/1871526511313030004. [DOI] [PubMed] [Google Scholar]
- 22.Aldeyab M.A., Baldwin N., McElnay J.C., Scott M.G., McNally M., Kearney M.P. Strategy for improving and maintaining compliance with adequate hospital hand hygiene practices. J Hosp Infect. 2011;77:87–88. doi: 10.1016/j.jhin.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 23.Mortell M., Balkhy H.H., Tannous E.B., Jong M.T. Physician ‘defiance’ towards hand hygiene compliance: is there a theory-practice-ethics gap? J Saudi Heart Assoc. 2013;25:203–208. doi: 10.1016/j.jsha.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michaelsen K., Sanders J.L., Zimmer S.M., Bump G.M. Overcoming patient barriers to discussing physician hand hygiene: do patients prefer electronic reminders to other methods? Infect Control Hosp Epidemiol. 2013;34:929–934. doi: 10.1086/671727. [DOI] [PubMed] [Google Scholar]