Abstract
The introduction of highly active antiretroviral therapy marked a major gain in efficacy of HIV/AIDS treatment and a reduction in morbidity and mortality of the infected patients. However, high levels of adherence are required to obtain virologic suppression. In Brazil, the policy of free and universal access to antiretroviral therapy has been in place since 1996, although there are reports of poor adherence.
Objective
To define the clinical, demographic and psychological characteristics, and quality of life of patients with HIV/AIDS who present poor adherence to highly active antiretroviral therapy.
Methods
This was a cross-sectional study. To be included in the study patients had to be 18 through 65 years old, diagnosed with HIV/AIDS, having the two previous viral loads above 500 copies, a surrogate for poor adherence to antiretrovirals. The following instruments were applied to all eligible patients: the sociodemographic questionnaire “Adherence Follow-up Questionnaire”, the Beck Depression Inventory (BDI-II), the Beck Anxiety Inventory (BAI), and the 36-Item Short Form Survey.
Results
47 patients were evaluated, 70.2% were female, mean age of 41.9 years (±10.5), 46.8% were single, 51.1% self-reported adherence ≥95%, 46.8% mentioned depression as the main reason for not taking the medication, 59.5% presented symptoms of moderate to severe depression, and 44.7% presented symptoms of moderate to severe anxiety. Finally, regarding health-related quality of life these patients obtained low scores in all dimensions, physical component summary of 43.96 (±9.64) and mental component summary of 33.19 (±13.35).
Conclusion
The psychological component is considered to be fundamental in the management of HIV/AIDS patients. Psychoeducation should be conducted at the initial evaluation to reduce negative beliefs regarding antiretroviral therapy Assessment of anxiety and depression symptoms should be done throughout therapy as both psycological conditions are associated with patient adherence, success of treatment, and ultimately with patients’ quality of life.
Keywords: Highly active antiretroviral therapy, HIV/AIDS, Adherence, Nonadherence, Anxiety, Depression, Quality of life
Introduction
The introduction of highly active antiretroviral therapy (HAART) in the 1990s marked a major gain in HIV/AIDS treatment efficacy, and a reduction in morbidity, mortality, and quality of life of these patients. In Brazil, the policy of free and universal access to antiretroviral therapy1 has been in place since 1996. Currently, the recommendation is for early onset of HAART, due to the benefits for people living with HIV/AIDS as well as for viremia control.2, 3
However, in order for HAART to be successful, adherence is crucial and is strictly associated with virologic suppression.4, 5 Therefore, the efficacy of HAART depends on maintaining high rates of treatment adherence, considered in most of the scientific literature as adherence equal to or greater than 95% of the prescribed dosages.6 Although the more potent drug regimens currently used allow for moderate adherence levels, no regimen allows for a partial adherence.7
Low levels of adherence increase disease progression as well as viral resistance, and limit the therapeutic options. In Brazil, between 1999 and 2008, there were reports of poor adherence to HAART, varying between 23.3% and 36.9%.8, 9, 10
Adherence is a complex dynamic and multifactorial process that encompasses physical, psychological, social, cultural, and behavioral aspects.2 Therefore, there are diverse challenges faced by people living with HIV/AIDS associated with the difficulties in maintaining high and prolonged levels of therapeutic adherence. In previous studies on the factors associated with poor adherence, the following were emphasized: depression, anxiety, low social support, complexity of therapeutic regimen, relationship with medical personnel, low level of schooling, side effects, negative beliefs about the treatment, stigma, and alcohol/substance abuse.2, 11
In short, the predictive factors of nonadherence may be grouped as follows: patient characteristics, the prescribed treatment regimen, the characteristics of the disease, doctor-patient relationship, and the location of medical care delivery.12, 13 Thus, the initial challenge for the managers of national policies and health care services specialized in HIV/AIDS is to understand how all these factors influence patient adherence, in order to establish effective actions, adjusted to the population characteristics. Furthermore, there are few studies in Brazil that evaluate the factors associated with low adherence and the quality of life of patients undergoing HAART.14, 15 Therefore, the main objective of this study was to define the clinical-demographic and psychological characteristics as well as quality of life and beliefs about HAART of the patients who present poor adherence to HAART, and evaluate the relation of some of these characteristics to adherence and quality of life.
Materials and methods
Study setting
This study was conducted at the Prof. Edgard Santos University Hospital (HUPES), Salvador, Bahia, Brazil, a reference center that provides health care services at the outpatient clinic or by hospitalization, for patients with HIV/AIDS diagnosis.
Study design and population
This study was a cross-sectional study carried out between February and May of 2016. Patients with HIV, on antiretroviral therapy for at least one year, aged between 18 and 65 years, receiving care at the AIDS outpatient clinics, having the last two viral loads above 500 copies, and who could read and write were invited to participate. Patients who presented neurocognitive impairment or psychotic disturbances that could compromise their understanding of the study were excluded.
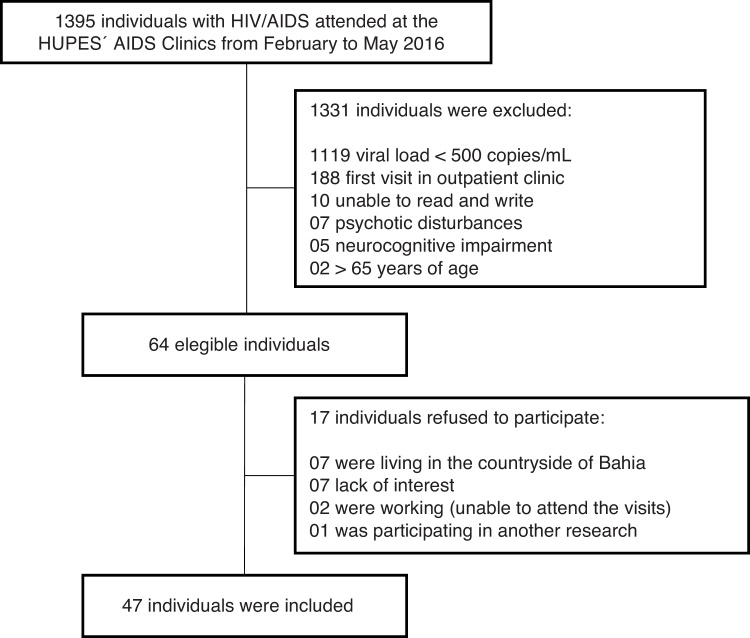
During the study period, 1395 patients with an HIV/AIDS diagnosis looked for care at the HUPES outpatient clinic; of these, 898 were male and 497 were female, and had their medical records were checked for the eligibility criteria considered. A total of 1331 patients did not meet the inclusion criteria thus leaving 64 patients to be studied. However, 17 (26%) patients refused to participate remaining 47 (73.4%) to be evaluated (Fig. 1).
Fig. 1.
Summary of the selection process of HIV-AIDS patients presenting poor adherence to HIV therapy in Salvador-Brazil.
Assessments
Sociodemographic characteristics
A structured questionnaire was developed for the study aimed at obtaining the participants’ sociodemographic information: gender, age, ethnicity, marital status, sexual orientation, education, occupation, and types of support. Furthermore, they were asked questions related to their habits and health conditions, such as year of diagnosis and when they began HAART, other chronic illnesses, alcohol consumption, use of psychoactive drugs, and medical assistance. Their medical records were reviewed to obtain information on the most recent viral load and the CD4+ lymphocyte count.
Adherence
Two questionnaires were used to measure adherence: (1) “Adherence Follow-up Questionnaire” from the Aids Clinical Trial Groups (ACTG),16 translated to Portuguese17 to assess self-reported adherence in the previous four days, use of pills by dosage and reasons for not taking the drugs; and (2) a questionnaire on knowledge and beliefs related to AIDS and to HAART, developed by the same group and translated to Portuguese by a previous study.18
Adherence was calculated as the number of doses that were effectively taken divided by the number of prescribed doses in the previous four days. Participants with adherence greater or equal to 95% were considered as being adherent.
Depression
The Beck Depression Inventory II (BDI-II) in the Portuguese version19, 20 was used to measure depression symptoms. The BDI-II is a self-reported scale with 21 items, each one with four choices of answer that imply increasing levels of depression severity. The total score is the sum of the individual scores of the items and provides the classification of the intensity of depression as minimal, mild, moderate, or severe.
Anxiety
The Beck Anxiety Inventory (BAI), Portuguese version,20 comprising 21 items or anxiety symptom affirmations that are evaluated by the subject on a scale of four points related to the levels of increasing severity of each symptom, was used to assess the anxiety symptoms of the patients. The total score is the sum of the individual scores of the items and provides the classification of the intensity level of anxiety as minimal, mild, moderate, or severe.
Quality of life
To estimate quality of life, the 36-item Short Form Health Survey (SF-36), Portuguese version21 was chosen. This questionnaire has 36 questions that measure quality of life related to health in eight dimensions: Physical Functioning, Physical Role, Bodily Pain, General Health, Vitality, Social Functioning, Emotional Role, and Mental Health. Furthermore, the questionnaire allows for evaluations of the physical component summary as well as the mental component summary.
Statistical analysis
The descriptive analyses of the qualitative variables were presented in absolute and relative frequencies. Continuous variables with normal distribution (age) were presented as mean and standard deviation. Continuous variables without normal distribution (years since diagnosis, years of treatment, number of pills, viral load, and CD4+ lymphocyte count) were expressed as median, minimum and maximum. Scores of quality of life were compared between genders and between those who had or had not used antiretroviral drugs in the last month by the Mann–Whitney nonparametric test.
Furthermore, the depression and anxiety variables were categorized in dichotomous variables (minimal and mild, and moderate and severe), with moderate and severe being considered as the presence of clinically significant symptomatology.19, 22 Comparisons among dimensions of quality of life were carried out using the Mann–Whitney nonparametric test. In the same way, Pearson's chi-squared test was used to evaluate whether the intensity of anxiety and depression symptoms were associated with the participants’ gender, and also whether the most relevant reason reported by the participants for stopping HAART was associated with the intensity of depression symptoms. A p-value less than 0.05 was considered statistically significant. The Statistical Package for the Social Sciences (SPSS) version 20.0 for Windows was used.
Ethical considerations
The present study was approved by the Research Ethics Committee of the School of Medicine of the Federal University of Bahia, in August of 2015 (case number 1.154.393). All participants signed a written consent form.
Results
The sociodemographic characteristics of the participants are presented in Table 1. Of the 47 participants, 70.2% were female, mean age 41.9 years (±10.5), and 46.8% self-reported as being of black ethnicity. Regarding marital status, 46.8% were single and 40.4% married; the majority (89.4%) was heterosexual. Only 53.2% had an individual income, and of these 23.4% reported the income originated from disability/retirement insurance payment related to illness. In the realm of social support, 91.6% of the participants reported that the family was aware of the HIV diagnosis, and 83% reported having family support. Alcohol consumption in the last three months were admitted by 51.1%, with 21.3% having consumed at least once a week, and 14.9% had heavy alcohol consumption, defined as five or more doses more than once a week. Only 6.4% (all males) reported use of other psychoactive substances in addition to heavy alcohol consumption.
Table 1.
Sociodemographic characteristics of the participants with HIV/AIDS who present poor adherence to HAART, in Salvador, Bahia, 2016.
| Variables | Total n = 47 (%) |
|---|---|
| Female sex | 33 (70.2) |
| Age (years) (mean, Ds) | 41.9 (±10.5) |
| Ethnicity | |
| Black | 22 (46.8) |
| Racially mixed | 13 (27.7) |
| White | 10 (21.3) |
| Indigenous | 2 (4.3) |
| Education | |
| Elementary school, complete/incomplete | 22 (46.8) |
| High school, complete/incomplete | 25 (53.2) |
| Marital status | |
| Single | 22 (46.8) |
| Married/living with partner | 19 (40.4) |
| Divorced/widowed | 6 (12.7) |
| Sexual orientation | |
| Heterosexual | 42 (89.4) |
| Homosexual | 4 (8.5) |
| Bisexual | 1 (2.1) |
| Individual income | |
| Has individual income | 25 (53.2) |
| Has no individual income | 22 (46.8) |
| Early retirement due to illness | 11 (23.4) |
| Family support | |
| Support | 39 (83) |
| Reject | 4 (8.6) |
| No one knows the diagnosis | 4 (8.6) |
| Type of supporta | |
| Spiritual | 23 (48.9) |
| Emotional | 7 (14.8) |
| Therapeutic | 5 (10.6) |
| Financial | 12 (25.5) |
| No type of support | 8 (17) |
| Alcohol | |
| Consumed alcohol in the last three months | 24 (51.1) |
| Frequent alcohol consumption (at least once a week) | 10 (21.3) |
| Heavy alcohol consumption | 7 (14.9) |
| Psychoactive substance consumption | 3 (6.4) |
| Missed doctor's appointment in the last 6 months | 25 (53.2) |
Including family support.
The clinical and psychological characteristics are listed in Table 2. The mean number of years since diagnosis was 13.5 (minimum 2 and maximum 28), and the average number of years on treatment was 13 (minimum 1 and maximum 20); at the time of evaluation the mean TCD4+ lymphocytes was 366 cells/μL (minimum 1 and maximum 970), and 80% of the participants presented a viral load between 400 and 100,000 copies. Moreover, among the participants who had other chronic diseases requiring medication, depression was the most common, with 31.2%. It is relevant because 59.5% of all patients presented moderate to severe symptoms of depression, and 44.7% presented anxiety symptoms. That means that only a minority were on treatment for such problems. An association was also found between stopping HAART due to feeling depressed and moderate and severe intensity of depression symptoms (p = 0.02). When evaluating the association of gender with anxiety and depression, an association was observed between the female sex and moderate and severe anxiety symptoms (p = 0.006) but there was no association between gender and symptoms of depression (p = 0.13).
Table 2.
Clinical and psychological characteristics of participants with HIV/AIDS who present poor adherence to HAART, treated in Salvador, Bahia, 2016.
| Variables | Total n = 47 (%) |
|---|---|
| Years since diagnosis (n = 45) (Md; min-max) | 13.5 (2–28) |
| Years of HAART (n = 40) (Md; min-max) | 13 (1–20) |
| Number of pills per day (Md; min-max) | 3 (1–9) |
| Self-reported Adherence ≥ 95% | 24 (51.1) |
| CD4+ (Md; min-max) | 366 (1–970) |
| Viral load (n = 45) | |
| 400–100,000 | 36 (80) |
| 100,000 | 9 (20) |
| Other chronic diseases with medication | 16 (34.0) |
| Depression with medication | 5 (10.6) |
| Depressiona | |
| Minimal | 9 (19.1) |
| Mild | 10 (21.3) |
| Moderate | 19 (40.4) |
| Severe | 9 (19.1) |
| Anxietyb | |
| Minimal | 11 (23.4) |
| Mild | 15 (31.9) |
| Moderate | 13 (27.7) |
| Severe | 8 (17.0) |
Beck Depression Inventory – BDI, Portuguese version. Minimal 0–11, Mild 12–19, Moderate 20–35 and Severe 36–63.
Beck Anxiety Inventory – BAI, Portuguese version. Minimal 0–10, Mild 11–19, Moderate 20–30 and Severe 31–63.
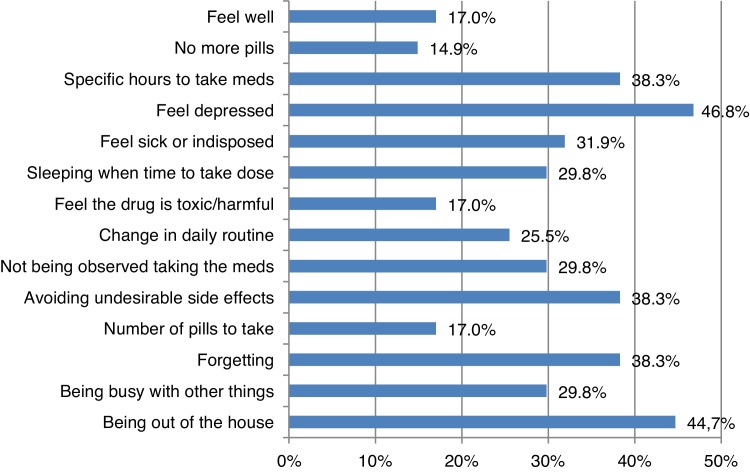
Regarding adherence, although 51.1% of the participants presented adherence equal to or greater than 95% in the previous four days, 57.4% did not take some of the medication in the previous week, and 74.5% in the month prior. The most relevant reason for not taking HAART (Fig. 2) was being depressed, with 46.8%, and other reasons were being away from home 44.7%; forgetfulness; avoiding undesired side effects, and taking the pills at specific times, with 38.3% each. On the other hand, even though 89.4% of the participants acknowledged that taking HAART helps one remain healthy for a longer time, they also showed some negative beliefs related to the treatment: 89.4% believed that the side effects were intense, 74.4% thought that taking HAART meant you had AIDS, and 72.3% had the belief that HAART was toxic (Table 3).
Fig. 2.
Reasons for stopping therapy among HIV/AIDS patients who present poor adherence to HAART, in Salvador, Brazil.
Table 3.
Beliefs about HAART of participants with HIV/AIDS, treated in Salvador, Bahia, 2016, who present poor adherence to antiretroviral therapy.
| Variables | Total n = 47 (%) |
|---|---|
| Undergoing HAART is a good idea even if you don’t have symptoms | 37 (78.7) |
| HAART has demonstrated its efficacy | 32 (68.0) |
| By undergoing HAART a person will be healthy for longer | 42 (89.4) |
| Side effects are intense for most people | 42 (89.4) |
| Undergoing HAART means you have AIDS | 35 (74.4) |
| HAART is toxic for most people | 34 (72.3) |
When evaluating quality of life related to health from a multidimensional approach, it was observed that the participants presented lower than expected (by scale's reference values) mean scores in all the dimensions (Table 4), with the dimensions of the mental component having the lowest score. Moreover, when comparing gender, women had lower scores in the dimensions of vitality (males: 47.9, females: 37.2; p = 0.03), mental health (males: 40.2, females: 32.3; p = 0.008) and mental component summary (males: 39.5, females: 31.7; p = 0.014). Furthermore, the patients who missed doses of antiretrovirals in the previous month had lower scores in the dimensions of general health (yes 39.2, not 50.9; p = 0.01) and bodily pain (yes 41.8, not 50.8; p = 0.01). When comparing intensity of anxiety and depression symptoms (Table 4), the patients who had moderate and severe symptoms of depression or anxiety also had lower scores in all dimensions except depression with bodily pain (p = 0.12) and anxiety with physical functioning (p = 0.63), general health (p = 0.35) and physical component summary (p = 0.42).
Table 4.
Quality of life scores, compared by levels of depression and anxiety of participants with HIV/AIDS, treated in Salvador, Bahia, 2016, who present poor adherence to HAART.
| Dimensions | Total n = 43 Mean (SD)a | Median | Depression, median |
Anxiety, median |
||||
|---|---|---|---|---|---|---|---|---|
| Minimal and mild | Moderate and severe | p-Value | Minimal and mild | Moderate and severe | p-Value | |||
| Physical functioning | 40.65 (10.49) | 42.4 | 44.6 | 39.1 | 0.008b | 40.4 | 44.6 | 0.63 |
| Physical Role | 38.47 (10.62) | 35.0 | 42.1 | 27.9 | 0.002b | 42.1 | 27.9 | 0.03b |
| Bodily Pain | 41.62 (10.73) | 42.1 | 46 | 37.9 | 0.12 | 46 | 37.9 | 0.008b |
| General Health | 41.23 (11.13) | 41.5 | 46.2 | 37.5 | 0.04b | 43.9 | 39.2 | 0.35 |
| Vitality | 41.29 (10.58) | 39.6 | 49 | 36 | 0.001c | 45.5 | 34.8 | 0.03b |
| Social Functioning | 36.05 (12.43) | 35.4 | 40.8 | 30 | 0.003b | 40.8 | 24.6 | 0.008b |
| Emotional Role | 32.06 (12.70) | 23.7 | 34.3 | 23.7 | 0.01b | 29 | 23.7 | 0.02b |
| Mental Health | 34.06 (13.97) | 36.8 | 39 | 27.7 | 0.003b | 39.1 | 23.2 | 0.002b |
| Physical component summary | 43.96 (9.64) | 42.9 | 49.3 | 39.8 | 0.04b | 46.1 | 41.8 | 0.42 |
| Mental component summary | 33.19 (13.35) | 32.9 | 36.1 | 26.1 | 0.002b | 36.2 | 25.8 | 0.002b |
Reference scores normalized by Short Form-36 mean 50 SD 10.
p < 0.05 for Mann–Whitney U test.
p < 0.01 for Mann–Whitney U test.
Discussion
The aim of this study was to identify the relevant characteristics that might have been associated with non-adherence to treatment, in a group of patients who presented poor adherence to HAART. During the time period of the study, 898 (64.4%) men and 497 (35.6%) women were treated at the HUPES outpatient clinic. It is noteworthy that more women (33 subjects, 70% of sample) showed poor adherence to HAART. This result is consistent with a study developed in Belo Horizonte, MG, that confirmed poorer adherence among women.23 Likewise, another multicentric study developed by the AIDS Clinical Trials Group in the United States, Puerto Rico and Italy24 reported women as having a greater risk of virologic failure due to poor adherence. Nevertheless, there are other recent studies that did not find a relationship between gender and levels of adherence.25, 26 Moreover, a systematic review on differences of adherence according to gender found a marginally significant difference of lower adherence in women.27
This study also investigated the participants’ beliefs about HAART and the reasons for not using the treatment. Although they admitted that HAART was effective and helped one to remain healthy for a longer time, negative ideas related to side effects, toxicity, and the concept that undergoing HAART meant one had AIDS were also presented. A review article on adherence and HAART demonstrated that the patient's belief system about the nature of the illness, its treatment, and the fears regarding side effects may be important obstacles to adherence.6 It is noteworthy that avoiding undesirable side effects was also one of the relevant reasons reported by 38.3% of the participants for stopping HAART, a finding that is near the 33.3% found in another Brazilian study.28
High prevalence of depression and symptoms of depression have been widely demonstrated in the literature in patients with HIV/AIDS. Prevalence studies reported a 28.1% in France,29 25.6% in the United States,30 and 32% in Brazil.31 Several studies mention depression as one of the most important barriers to adhering to HAART.6, 32 In this study, we found that the reason for stopping HAART because of feeling depressed was associated with moderate and severe levels of depression symptoms. This finding is even more relevant when considering that feeling depressed was the greatest reason reported by the participants for stopping HAART and that most (59.5%) of them presented clinically significant symptoms of depression.19, 22
The percentage of participants who presented depressive symptoms between moderate and severe (59.5%) was significantly higher than those from other Brazilian studies (18% and 21.5%),31, 33 that evaluated patients with HIV who did not necessarily have adherence issues as in this present study. In addition, only 10.6% had prescriptions of antidepressive drugs. Other studies mention that between 50% and 60% of the patients with depression are undiagnosed.31
The rates of moderate and severe symptoms of anxiety were higher in this study (44.7%) than in another previous study in Brazil (35.8%), that detected symptoms of severe anxiety (12.6%) as an important predictor for non-adherence to HAART.33 Since our work was focused on a non-adherent population, our results were expected, and reinforces the importance of anxiety in the adherence process. A relationship with the intensity of anxiety symptoms and female gender was also observed, which is consistent with a study published in 2016.34 This also reinforces the importance of finding a high proportion of women in our study.
Differences by gender were also observed in some dimensions of quality of life: women had lower scores in the dimensions vitality, mental health, and mental component summary, which might be related to the fact that they had more symptoms of moderate and severe anxiety than did men. In a previously published Brazilian work it was found that women living with HIV and patients with anxiety had worse quality of life scores.35
One of the purposes of HAART is to improve the quality of life of patients, which is confirmed by several studies that have shown an improvement in quality of life after patients started therapy.36, 37 In this study, however, it was demonstrated that the quality of life of patients who showed poor adherence was lower in all the dimensions, and mental health was the most affected. Furthermore, when compared to another study conducted in Brazil in 2009, with HIV/AIDS patients, regardless of the adherence level, these results retain lower scores in all components, including mental component summary.38 On the other hand, a multicentric study that evaluated the changes during one year in quality of life of patients on HAART concluded that patients with less than 80% adherence to HAART had lower quality of life, and patients with continuous adherence to HAART had improvements in quality of life,36 which could explain in part the results of the present study.
Similarly, several studies established the association of lower quality of life with depression and anxiety,39, 40 some of which were developed in Brazil.37, 41 In this study, presenting clinically significant anxiety and depression symptomatology was associated with lower scores in some dimensions of physical health and mental health.
In addition, our study showed a significantly higher proportion of women among non-adherent patients, and a strong association between the presence of moderate or severe levels of anxiety, depression symptoms, and low scores in quality of life. Similar characteristics were found in a study published in 2016, carried out in Thailand in patients with HIV/AIDS, which found associations between anxiety in female patients with poor adherence to HAART and associations between anxiety and depression with low quality of life.34 Therefore, there is a need for further studies to clarify and understand how gender, anxiety, depression, and quality of life might be associated with adherence to HAART.
The role of the psychological component is considered to be fundamental in the management of HIV/AIDS patients. Psychoeducation should be used to reduce negative beliefs regarding antiretroviral therapy, beyond the initial evaluation and subsequent assessments of anxiety and depression symptoms. These points warrant greater attention because they are associated with adherence, the success of the treatment and ultimately, with the patients’ quality of life. Furthermore, it is pertinent to develop studies related to women's adherence to HAART, to gather the necessary information that would allow the implementation of differentiated interventions tailored to women.
Finally, the limitations of this cross-sectional study include difficulties in establishing causal relationships to poor adherence, the use of self-report to assess adherence that could foster under- or overestimating the rates of participants’ adherence, and the small sample size. However, self-reported adherence is a validated method to evaluate the proper use of antiretroviral drugs, despite some clear limitations.16 The use of a biological marker (viral load) reduces the effect of inaccurate self-reported adherence levels. In addition, our results clearly pointed out to the importance of a better evaluation of psychological aspects of women failing antiretroviral therapy due to non-adherence. Strategies to overcome these barriers are urgently needed.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.BRASIL. Congresso Nacional. Lei n° 9.313, 13 de novembro de 1996. Dispõe sobre a distribuição gratuita de medicamentos aos portadores do HIV e doentes de AIDS. Diário Oficial [da República Federativa do Brasil], Brasília, DF. (14 de nov 1996).
- 2.Ministerio da Saúde . Departamento de DTS, Aids e Hepatites Virais; Brasilia: 2013. Secretaria de Vigilância em Saúde. Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. p. 216. [Google Scholar]
- 3.Günthard H.F., Saag M.S., Benson C.A., et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the international antiviral society–USA panel. JAMA. 2016;316:191–210. doi: 10.1001/jama.2016.8900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bangsberg D.R., Perry S., Charlebois E.D., et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 5.Thompson M.A., Aberg J.A., Hoy J.F., et al. Antiretroviral treatment of adult HIV infection: 2012 recommendations of the international antiviral society–USA panel. JAMA. 2012;308:387–402. doi: 10.1001/jama.2012.7961. [DOI] [PubMed] [Google Scholar]
- 6.Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17:169–177. doi: 10.1089/108729103321619773. [DOI] [PubMed] [Google Scholar]
- 7.Peltzer K., Ramlagan S., Jones D., Weiss S.M., Fomundam H., Chanetsa L. Efficacy of a lay health worker led group antiretroviral medication adherence training among non-adherent HIV-positive patients in KwaZulu-Natal, South Africa: results from a randomized trial. SAHARA J. 2012;9:218–226. doi: 10.1080/17290376.2012.745640. [DOI] [PubMed] [Google Scholar]
- 8.de Carvalho C.V., Merchan-Hamann E., Matsushita R. [Determinants of antiretroviral treatment adherence in Brasilia, Federal District: a case-control study] Rev Soc Bras Med Trop. 2007;40:555–565. doi: 10.1590/s0037-86822007000500013. [DOI] [PubMed] [Google Scholar]
- 9.Bonolo P.F., Machado C.J., Cesar C.C., Ceccato M., Guimarães M.D. Vulnerability and non-adherence to antiretroviral therapy among HIV patients, Minas Gerais State, Brazil. Cad Saude Publica. 2008;24:2603–2613. doi: 10.1590/s0102-311x2008001100015. [DOI] [PubMed] [Google Scholar]
- 10.Brigido L.F., Rodrigues R., Casseb J., et al. Impact of adherence to antiretroviral therapy in HIV-1-infected patients at a university public service in Brazil. AIDS Patient Care STDS. 2001;15:587–593. doi: 10.1089/108729101753287685. [DOI] [PubMed] [Google Scholar]
- 11.Remien R.H., Bastos F.I., Jnr V.T., et al. Adherence to antiretroviral therapy in a context of universal access, in Rio de Janeiro, Brazil. AIDS Care. 2007;19:740–748. doi: 10.1080/09540120600842516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ickovics J.R., Meade C.S. Adherence to HAART among patients with HIV: breakthroughs and barriers. AIDS Care. 2002;14:309–318. doi: 10.1080/09540120220123685. [DOI] [PubMed] [Google Scholar]
- 13.Fogarty L., Roter D., Larson S., Burke J., Gillespie J., Levy R. Patient adherence to HIV medication regimens: a review of published and abstract reports. Patient Educ Couns. 2002;46:93–108. doi: 10.1016/s0738-3991(01)00219-1. [DOI] [PubMed] [Google Scholar]
- 14.Silva J.A., Dourado I., Brito A.M., Silva C.A. Factors associated with non-adherence to antiretroviral therapy in adults with AIDS in the first six months of treatment in Salvador, Bahia State, Brazil. Cad Saude Publica. 2015;31:1188–1198. doi: 10.1590/0102-311X00106914. [DOI] [PubMed] [Google Scholar]
- 15.Zubaran C., Medeiros G., Foresti K., May W., Michelim L., Madi J.M. Quality of life and adherence to antiretroviral therapy in Southern Brazil. AIDS Care. 2014;26:619–625. doi: 10.1080/09540121.2013.841838. [DOI] [PubMed] [Google Scholar]
- 16.ACTG, Adherence follow up questionnaire. Available from: https://www.frontierscience.org/apps/cfmx/apps/common/QOLAdherenceForms/resources/actg/forms/english/ql0702.pdf [accessed 5.5.16].
- 17.Ricci G., Netto E.M., Luz E., Rodamilans C., Brites C. Adherence to antiretroviral therapy of Brazilian HIV-infected children and their caregivers. Braz J Infect Dis. 2016;20:429–436. doi: 10.1016/j.bjid.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sampaio-Sa M., Page-Shafer K., Bangsberg D.R., et al. 100% adherence study: educational workshops vs. video sessions to improve adherence among ART-naive patients in Salvador, Brazil. AIDS Behav. 2008;12(4 Suppl):S54–S62. doi: 10.1007/s10461-008-9414-0. [DOI] [PubMed] [Google Scholar]
- 19.Gomes-Oliveira M.H., Gorenstein C., Lotufo Neto F., Andrade L.H., Wang Y.P. Validation of the Brazilian Portuguese version of the Beck Depression Inventory-II in a community sample. Rev Bras Psiquiatr. 2012;34:389–394. doi: 10.1016/j.rbp.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Cunha J.A. Casa do Psicólogo; São Paulo: 2001. Manual da versão em português das Escalas Beck. [Google Scholar]
- 21.Ciconelli R.M., Ferraz M.B., Santos W., Meinão I., Quaresma M.R. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36) Rev Bras Reumatol. 1999;39:143–150. [Google Scholar]
- 22.Dozois D.J.A., Dobson K.S., Ahnberg J.L. A psychometric evaluation of the Beck Depression Inventory-II. Psychol Assess. 1998;10:83–89. [Google Scholar]
- 23.Bonolo P.F., Cesar C.C., Acurcio F.A., et al. Non-adherence among patients initiating antiretroviral therapy: a challenge for health professionals in Brazil. AIDS. 2005;19(Suppl 4):S5–S13. doi: 10.1097/01.aids.0000191484.84661.2b. [DOI] [PubMed] [Google Scholar]
- 24.Collier A.C., Ribaudo H., Mukherjee A.L., Feinberg J., Fischl M.A., Chesney M. A randomized study of serial telephone call support to increase adherence and there by improve virologic outcome in persons initiating antiretroviral therapy. J Infect Dis. 2005;192:1398–1406. doi: 10.1086/466526. [DOI] [PubMed] [Google Scholar]
- 25.McCoy K., Waldrop-Valverde D., Balderson B.H., Mahoney C., Catz S. Correlates of antiretroviral therapy adherence among HIV-infected older adults. J Int Assoc Provid AIDS Care. 2016;15:248–255. doi: 10.1177/2325957416642019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beer L., Mattson C.L., Bradley H., Skarbinski J. Understanding cross-sectional racial, ethnic, and gender disparities in antiretroviral use and viral suppression among HIV patients in the United States. Medicine (Baltimore) 2016;95:e3171. doi: 10.1097/MD.0000000000003171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ortego C., Huedo-Medina T.B., Santos P., et al. Sex differences in adherence to highly active antiretroviral therapy: a meta-analysis. AIDS Care. 2012;24:1519–1534. doi: 10.1080/09540121.2012.672722. [DOI] [PubMed] [Google Scholar]
- 28.Guimarães M.D., Rocha G.M., Campos L.N., et al. Difficulties reported by HIV-infected patients using antiretroviral therapy in Brazil. Clinics (Sao Paulo) 2008;63:165–172. doi: 10.1590/s1807-59322008000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feuillet P., Lert F., Tron L., Aubriere C., Spire B., Dray-Spira R. Prevalence of and factors associated with depression among people living with HIV in France. HIV Med. 2016 [Google Scholar]
- 30.Do A.N., Rosenberg E.S., Sullivan P.S., et al. Excess burden of depression among HIV-infected persons receiving medical care in the United States: data from the medical monitoring project and the behavioral risk factor surveillance system. PLoS One. 2014;9:e92842. doi: 10.1371/journal.pone.0092842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silveira M.P., Guttier M.C., Pinheiro C.A., Pereira T.V., Cruzeiro A.L., Moreira L.B. Depressive symptoms in HIV-infected patients treated with highly active antiretroviral therapy. Rev Bras Psiquiatr. 2012;34:162–167. doi: 10.1590/s1516-44462012000200008. [DOI] [PubMed] [Google Scholar]
- 32.Krumme A.A., Kaigamba F., Binagwaho A., Murray M.B., Rich M.L., Franke M.F. Depression, adherence and attrition from care in HIV-infected adults receiving antiretroviral therapy. J Epidemiol Commun Health. 2015;69:284–289. doi: 10.1136/jech-2014-204494. [DOI] [PubMed] [Google Scholar]
- 33.Campos L.N., Guimarães M.D., Remien R.H. Anxiety and depression symptoms as risk factors for non-adherence to antiretroviral therapy in Brazil. AIDS Behav. 2010;14:289–299. doi: 10.1007/s10461-008-9435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prasithsirikul W., Chongthawonsatid S., Ohata P.J., et al. Depression and anxiety were low amongst virally suppressed, long-term treated HIV-infected individuals enrolled in a public sector antiretroviral program in Thailand. AIDS Care. 2016:1–7. doi: 10.1080/09540121.2016.1201194. [DOI] [PubMed] [Google Scholar]
- 35.Passos S.M., Souza L.D. An evaluation of quality of life and its determinants among people living with HIV/AIDS from Southern Brazil. Cad Saude Publica. 2015;31:800–814. doi: 10.1590/0102-311x00000514. [DOI] [PubMed] [Google Scholar]
- 36.Mannheimer S.B., Matts J., Telzak E., et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. 2005;17:10–22. doi: 10.1080/09540120412331305098. [DOI] [PubMed] [Google Scholar]
- 37.Campos L.N., Cesar C.C., Guimarães M.D. Quality of life among HIV-infected patients in Brazil after initiation of treatment. Clinics (Sao Paulo) 2009;64:867–875. doi: 10.1590/S1807-59322009000900007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soarez P.C., Castelo A., Abrão P., Holmes W.C., Ciconelli R.M. [Brazilian-Portuguese translation and validation of the HIV/AIDS-Targeted Quality of Life Instrument] Rev Panam Salud Publica. 2009;25:69–76. doi: 10.1590/s1020-49892009000100011. [DOI] [PubMed] [Google Scholar]
- 39.Ezeamama A.E., Woolfork M.N., Guwatudde D., et al. Depressive and anxiety symptoms predict sustained quality of life deficits in HIV-positive Ugandan adults despite antiretroviral therapy: a prospective cohort study. Medicine (Baltimore) 2016;95:e2525. doi: 10.1097/MD.0000000000002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peter E., Kamath R., Andrews T., Hegde B.M. Psychosocial determinants of health-related quality of life of people living with HIV/AIDS on antiretroviral therapy at Udupi District, Southern India. Int J Prev Med. 2014;5:203–209. [PMC free article] [PubMed] [Google Scholar]
- 41.Tostes M.A., Chalub M., Botega N.J. The quality of life of HIV-infected women is associated with psychiatric morbidity. AIDS Care. 2004;16:177–186. doi: 10.1080/09540120410001641020. [DOI] [PubMed] [Google Scholar]