Abstract
By relying on data from existing patient-reported outcome measures of quality of life, the true impact of skin conditions on patients’ lives may be underestimated. This study systematically reviewed all dermatology-specific (used across skin conditions) patient-reported outcome measures and makes evidence-based recommendations for their use. The study protocol is registered on PROSPERO (CRD42018108829). PubMed, PsycInfo and CINAHL were searched from inception to 25 June 2018. The Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) criteria were used to assess the measurement properties and methodological quality of studies. A total of 12,925 abstracts were identified. Zero patient-reported outcome measures were assigned to category A (ready for use without further validation), 31 to category B (recommended for use, but only with further validation) and 5 to category C (not recommended for use). There is no gold-standard dermatology-specific patient-reported outcome measure that can be recommended or used without caution. A new measure that can comprehensively capture the impact of dermatological conditions on the patient’s life is needed.
Key words: patient-reported outcome measures, measurement properties, dermatology-specific, burden, quality of life
Dermatological conditions are reported to cause substantial pain, disfigurement, disability, and stigma and have a psychological, social and financial burden (1, 2). Our qualitative research with people with dermatological conditions resulted in the first conceptual framework of the impact of these conditions on patients’ lives (unpublished data). Impact was defined as a multifaceted construct shown across physical, psychological, social, financial and daily functioning.
The measurement of impact is particularly pertinent to dermatology, where the goal of treatment is often to improve the patient’s quality of life (QoL) rather than prolong it. The true impact of dermatological conditions on patients’ lives is probably underestimated, because most of the evidence derives from data collected using QoL patient-reported outcome measures (PROMs), which have some limitations. First, these PROMs are typically used to assess the impact of an intervention on the patient’s life, not the impact of the skin condition on the patient’s life. Secondly, individual dermatology QoL PROMs do not adequately address all of the relevant domains or aspects thereof. For example, the psychological functioning domain has focussed largely on emotions and, to a lesser extent, coping behaviour, and typically ignores the cognitive impact. Cognitions are known to predict outcomes for a range of long-term conditions (1). In dermatology, beliefs about psoriasis are better predictors of outcomes than clinician-assessed disease severity (2–4) and are closely linked with medication adherence (5). Thirdly, work on cumulative life course impairment (CLCI) and major life decisions has established that skin conditions have a cumulative impact over time (4, 5). Recall bias increases with a long recall period, so it is generally recommended that PROMs are repeatedly administered to capture impacts over time. However, dermatology QoL PROMs typically do not contain items that can be used to track CLCI over time. Finally, the measurement properties of most PROMs used in dermatology have not been evaluated according to the “gold-standard” criteria, the Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) criteria (9). This is important because PROMs must meet pre-defined criteria across a range of measurement properties (including validity, reliability and responsiveness) for the data they produce to be meaningful (6–8). Without knowledge of their measurement properties, we cannot judge the quality of a measure nor have confidence in the data it produces.
SIGNIFICANCE
This is the first study to systematically evaluate all published dermatology-specific (for use across skin conditions), patient-reported outcome measures against the gold-standard Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) criteria and make evidence-based recommendations for their use. The study found that no dermatology-specific patient-reported outcome measure can be unequivocally recommended for use. These results question the validity of the data collected using these patient-reported outcome measures, which has implications for clinical decision-making and research.
To fully understand the impact of skin conditions on patients’ lives there is a need to develop a measure specifically designed to capture this. This systematic review is the first step in the development of the Patient-Reported Impact of Dermatological Diseases (PRIDD) measure: a dermatology-specific PROM of the impact of dermatological conditions on the patient’s life for use with adults worldwide. PRIDD will have discriminative and evaluative applications for use in research and clinical practice. This review aims to: (i) identify all dermatology-specific PROMs (see Table I for information on levels of measurement) and assess their suitability for use as a measure of impact, (ii) evaluate their measurement properties according to the COSMIN criteria, and (iii) make evidence-based recommendations for their use.
Table I.
Levels of measurement
| Definition | Example | |
|---|---|---|
| Generic | Instrument can be used across therapeutic areas, e.g. dermatology, diabetes or cancer. | Short Form-36, EuroQOL 5D, Nottingham Health Profile |
| Dermatology-specific | Instrument is specific to dermatology and can be used across skin conditions. | Dermatology Life Quality Index, Skindex, Patient Benefit Index |
| Disease-specific | Instrument is to be used only with a certain skin condition. | Patient Oriented Eczema Measure, Rosacea Quality of Life Index, Comprehensive Appraisal of Life Impact of Psoriasis |
MATERIALS AND METHODS
The review protocol was registered on PROSPERO (CRD-42018108829), an international database of prospectively registered systematic reviews with a health outcome. Ethics approval was not required. A comprehensive search strategy (Table SI1) identified published evidence of the development and validation of dermatology PROMs. It comprised 3 blocks of search terms: (i) dermatological conditions; (ii) life impact; and (iii) a validated, highly sensitive search filter for measurement properties (10). Searches of PubMed, PsycInfo and CINAHL from inception to 25 June 2018 were limited to journal articles and human subjects. No limit was applied for language, and non-English papers were translated. Due to the volume of articles retrieved, the current study focused on dermatology-specific PROMs. Disease-specific PROMs will be reported in a separate manuscript.
The systematic review was conducted according to the COSMIN methodology which is the gold-standard critical appraisal tool for systematic reviews of PROMs (9). According to COSMIN, all PROMs in a review should be assessed according to both the construct of interest and target population of the review (9). The aim of this review was to identify measures of impact and to establish the quality of dermatology-specific PROMs currently in use. As such, the target population was patients with dermatological conditions (as opposed to disease-specific samples, e.g. atopic dermatitis) and the construct of interest was that of the PROM assessed. This allowed us to both identify measures of impact and establish the quality of PROMs currently used in dermatology.
Three reviewers independently screened titles and abstracts. To satisfy the inclusion criteria, the title and/or abstract had to include at least one term from each of the 3 search strategy blocks. Three reviewers independently assessed and ranked the selected articles according to adapted criteria by Kitchen et al. (11) (Table II). Only articles ranked 1a were included. Reviewers screened and rank-ordered 10% of the others’ samples to determine inter-rater reliability. The results were compared and any discrepancies were resolved through discussion.
Table II.
Ranking criteria for articles adapted from Kitchen et al. (11)
| Rank | Criteria |
|---|---|
| 1a |
|
| 1b |
|
| 2 |
|
| 3 |
|
| X |
|
PRO: patient-reported outcome.
An electronic data extraction form complied with the COSMIN guidance (12). The key data extracted were: summary data of included studies; the characteristics of included studies; the-measurement properties of the studied PROM(s); and information on the interpretability and feasibility of included PROMs.
Methodological quality of included studies
The COSMIN risk of bias checklist (9, 12) was used by 6 independent reviewers to evaluate the methodological quality of included studies.
Quality of measurement properties
Measurement properties from the COSMIN checklist were evaluated against predefined criteria by 6 independent reviewers (9). Criterion validity was not assessed, as no gold-standard exists for the constructs evaluated (e.g. QoL) (13). Interpretability and feasibility data were collected where available.
Best-evidence synthesis
For each PROM, evidence for the methodological quality of the studies and quality of measurement properties per measurement property were pooled and summarized. The summary was rated against the criteria for good measurement properties and then graded using a modified Grades of Recommendation, Assessment, Development and Evaluation (GRADE) to form a best-evidence synthesis (9, 12). The quality of the evidence was graded as high, moderate, low or very low evidence, according to the COSMIN procedures (9). All versions of a PROM were considered separately (9, 12).
The GRADE approach specifies 5 factors to determine the quality of evidence: risk of bias (quality of the studies), inconsistency (of the results of the studies), indirectness (evidence comes from different populations, interventions or outcomes than the ones of interest in the review), imprecision (wide confidence intervals), and publication bias (9). The fifth factor, publication bias, is not included in the COSMIN methodology, since there are no registries for studies on measurement properties. Thus, a modified GRADE approach specifying 4 factors was used to downgrade the evidence.
Generating recommendations for use of dermatology-specific patient-reported outcome measures
The primary outcome assessed was recommendation for use. Each PROM was assigned to 1 of 3 standardized “recommendation for use” categories according to COSMIN criteria (9) similar to a traffic-light system of green indicating good to go, amber meaning proceed with caution and red do not proceed:
-
A:
PROM can be recommended for use (has evidence for sufficient content validity [any level] and at least low-quality evidence for sufficient internal consistency).
-
B:
PROM has potential to be recommended for use, but requires further validation (cannot be categorized into A or C).
-
C:
PROM should not be recommended for use (has high-quality evidence demonstrating insufficient measurement criteria).
The secondary outcome was establishing the existence of dermatology-specific PROM capable of measuring impact, achieved by evaluating the domains measured in each PROM.
RESULTS
The search identified 12,925 abstracts. An additional 3 articles (14–16) were identified through reference lists and expert input. Fig. 1 details the full article selection process. Of the 53 dermatology-specific PROM articles identified, data were extracted from 52 articles. One article (17) was excluded, since the psychometric testing for 2 separate PROMs was combined. Two studies examined more than one PROM (18, 19). Six articles that met inclusion criteria were not included in the COSMIN analysis, but data were extracted (17, 20–25); 2 because only interpretability information was reported (22, 24); and 4 review articles did not provide sufficient information on the methodological quality of included studies, but included information on interpretability and feasibility (20, 21, 23, 25). In all, 36 PROMs (Tables SII and SIII1), reported in 46 articles (Table SIV1), were included in the COSMIN analysis.
Fig. 1.
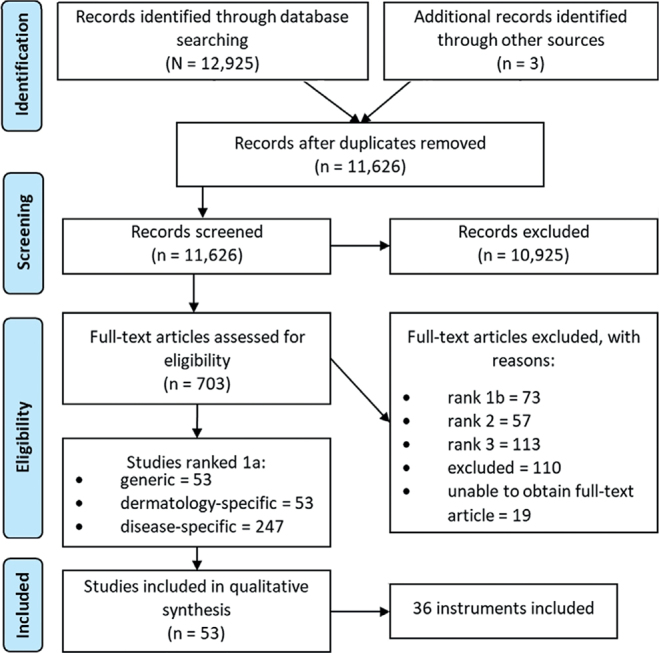
Flow diagram of the screening and selection process.
Identification of an impact measure
A comparison of each PROM at the domain level is shown in Table III. Domains were derived based on the subscales reported by the developers or through structural validity analyses (i.e. factor analysis). Many of the instruments (83%) measured QoL. The most common domains observed were symptoms, emotional/psychological functioning, physical functioning, social functioning and daily activities. None of the PROMs included other life domains, such as financial impact and life course impairment; therefore, they should not be considered a comprehensive measure of the impact of living with a skin disease.
Table III.
Comparison of patient-reported outcome measures (PROMs) at domain level
| PROM | Symptoms | Emotional/psychological functioning | Physical functioning | Social functioning | Daily activities | Treatment beliefs/impact | Work/school | Quality of care | Coping behaviours | Stigmatization | Education/support needs | Intimacy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACSD | × | × | × | × | × | × | × | × | × | × | × | |
| CDLQI | × | × | × | × | × | × | × | × | ||||
| CQI-CSD | × | |||||||||||
| DIS | × | |||||||||||
| DLQI | × | × | × | × | × | × | × | × | ||||
| DQOLs | × | × | × | × | ||||||||
| DSQL | × | × | × | × | × | |||||||
| FLQA-d | × | × | × | × | × | × | ||||||
| PBI | × | |||||||||||
| PeDeSI | × | |||||||||||
| PRISM | ||||||||||||
| SF-QES | × | × | × | × | ||||||||
| Skindex | × | × | × | × | × | × | × | |||||
| S29 | × | × | × | |||||||||
| S16 | × | × | × | |||||||||
| TQL | × | × | × | × | × | |||||||
| VQ-Dermato | × | × | × | × | × |
x: domain present; ACSD: Adjustment to Chronic Skin Diseases Questionnaire; CDLQI: Children’s Dermatology Life Quality Index; CQI-CSD: Consumer Quality Index Chronic Skin Disease; DIS: Dermatology Intimacy Scale; DLQI: Dermatology Life Quality Index; DQOLs: Dermatology Quality of Life scales; DSQL: Dermatology-specific Quality of Life; FLQA-d: Freiburg Life Quality Assessment; PBI: Patient Benefit Index; PeDeSI: Person-Centred Dermatology Self-Care Index; PRISM: Pictorial Representation of Illness & Self-Measure; SF-QES: Short-form of the Questionnaire on Experience with Skin Complaints; S29: Skindex-29; TQL: Turkish Quality of Life Instrument for skin disease.
Methodological quality of included studies and quality of measurement properties
Table IV shows the methodological quality of studies and the quality of the results for the PROM content validity studies. Evidence for content validity was based only on development and pilot-testing studies (n = 22) for most instruments, as a content validity study was conducted only for the Spanish version of Skindex-29 (S29-S). The majority (86%) of the development studies were of very low methodological quality. Only the Patient Benefit Index (PBI; low quality), Turkish Quality of Life Instrument (TQL; low quality) and Skindex 29-Spanish (high quality) were rated as having adequate methodological quality. The most common reason for the downgrading of the overall quality of evidence to very low was that a cognitive interview was not conducted or was of poor methodological quality.
Table IV.
Methodological quality and quality assessment of results per development and content validity study per patient-reported outcome measure (PROM)
| PROM | Methodological quality | Quality assessment of results | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Design | Comprehensibility | Comprehensiveness | Cognitive interview study | Total development | Content validity study | Overall relevance | Overall comprehensiveness | Overall Content comprehen-validity sibility study | Overall content validity | Quality of evidence | |
| ACSD (32) | D | × | × | I | I | × | + | + | + | + | Very low |
| CDLQI (33) | I | × | I | I | I | × | + | + | + | + | Very low |
| CDLQI-C (34) | I | D | I | I | I | × | + | + | + | + | Very low |
| CQI-CSD (74) | A | I | I | I | I | × | ± | + | + | ± | Very low |
| DIS (35) | I | D | D | D | I | × | + | + | + | + | Very low |
| DLQI (36) | I | D | D | D | I | × | + | + | + | + | Very low |
| DQOLs (48) | I | × | × | I | I | × | ? | ? | ? | ? | Very low |
| DSQL (49) | D | I | D | I | I | × | + | + | + | + | Very low |
| FLQA-d (14) | D | D | I | I | I | × | + | + | + | + | Very low |
| PBI (51) | D | D | D | D | D | ± | + | ± | ± | Low | |
| PeDeSi (52) | D | × | × | I | I | × | + | + | + | + | Very low |
| SF-QES (15) | I | I | I | I | I | × | ± | + | + | + | Very low |
| Skindex (54) | D | I | I | I | I | × | + | + | + | + | Very low |
| S29 (55) | D | I | D | I | I | × | + | + | + | + | Very low |
| S29-S (31) | D | I | I | I | I | × | – | ? | ? | ? | Very low |
| S29-Sp (26) | D | I | I | I | I | A | – | – | -- | – | High |
| S29-C (18) | D | D | I | I | I | × | – | ? | – | – | Very low |
| S16 (57) | D | I | D | I | I | × | + | + | + | + | Very low |
| S16-C (18) | D | D | I | I | I | × | – | ? | – | – | Very low |
| S16-M (61) | D | I | I | I | I | × | – | ? | ? | ? | Very low |
| TQL (62) | D | D | D | D | D | × | ± | ? | – | ± | Low |
| VQ-D (63) | D | D | D | D | I | × | + | + | + | + | Very low |
ACSD: Adjustment to Chronic Skin Diseases Questionnaire; CDLQI: Children’s Dermatology Life Quality Index; CDLQI-C: CDLQI Cantonese; CQI-CSD: Consumer Quality Index Chronic Skin Disease; DIS: Dermatology Intimacy Scale; DLQI: Dermatology Life Quality Index; DQOLs: Dermatology Quality of Life scales; DSQL: Dermatology-specific Quality of Life; FLQA-d: Freiburg Life Quality Assessment; PBI: Patient Benefit Index; PeDeSI: Person-Centred Dermatology Self-Care Index; SF-QES: Short-form of the Questionnaire on Experience with Skin Complaints; S29: Skindex-29; S16: Skindex-16; TQL: Turkish Quality of Life Instrument for skin disease; A: adequate; D: doubtful; I: inadequate; ×: study not performed; +: sufficient; –: insufficient; ±: inconsistent; ?: indeterminate.
The methodological quality of studies on measurement properties (Table V) and quality of the measurement properties (Table VI) per study are also presented. No PROM was tested for all measurement properties. The amount of measurement properties tested per PROM ranged between 1 and 6. Internal consistency was the most popular psychometric test (n = 37), measurement invariance the least (n = 2) and measurement error was not tested at all.
Table V.
Methodological quality of each study per measurement property
| PROM | Study | Structural validity | Internal consistency | Reliability | Measurement error | Construct validity | Cross-cultural validity/measurement invariance | Responsiveness |
|---|---|---|---|---|---|---|---|---|
| ACSD | (32) | V | ||||||
| CDLQI | (33) | I | D | |||||
| CDLQI-C | (34) | D | D | D | ||||
| CQI-CSD | (74) | I | I | I | ||||
| DIS | (35) | D | ||||||
| DQLI | (38) | I | I | |||||
| (24) | V | V | V | |||||
| (39) | V | V | A | |||||
| (16) | A | D | D | |||||
| (76) | I | I | I | |||||
| (75) | D | |||||||
| (36) | D | D | V | |||||
| DLQI-B | (40) | I | A | |||||
| DLQI-C | (42) | V | D | V | I | |||
| (41) | A | I | I | |||||
| (44) | V | V | V | |||||
| (43) | A | A | ||||||
| DLQI-D | (27) | I | D | |||||
| DLQI-I | (45) | V | V | V | ||||
| DLQI-N | (46) | A | A | A | ||||
| DLQI-S | (30) | V | D | D | ||||
| DLQI-T | (47) | A | D | |||||
| DLQI-U | (19) | I | ||||||
| DQOLs | (48) | A | I | D | D | |||
| DSQL | (50) | V | D | V | V | |||
| (49) | V | V | I | A | ||||
| FLQA-d | (14) | V | V | I | V | |||
| PBI | (51) | D | D | A | ||||
| PeDeSI | (52) | A | A | |||||
| PRISM | (53) | V | D | |||||
| SF-QES | (29) | V | V | D | ||||
| Skindex | (54) | V | I | I | D | I | ||
| S29 | (77) | V | ||||||
| (55) | V | V | I | D | I | |||
| S29-C | (18) | A | I | V | ||||
| S29-G | (56) | V | V | V | I | |||
| S29-S | (31) | V | D | V | ||||
| S29-Sp | (28) | V | I | A | D | |||
| (26) | V | V | ||||||
| S16 | (57) | A | A | I | D | D | ||
| S16-BP | (59) | V | A | V | ||||
| S16-A | (58) | V | A | |||||
| S16-C | (18) | V | I | V | ||||
| S16-J | (60) | V | V | |||||
| S16-M | (61) | V | D | V | ||||
| S16-U | (19) | V | ||||||
| TQL | (62) | A | A | D | A | |||
| VQ-Dermato | (63) | A | A | D | V | A |
PROM: patient-reported outcome measures; ACSD: Adjustment to Chronic Skin Diseases Questionnaire; CDLQI: Children’s Dermatology Life Quality Index; CDLQI-C: CDLQI Cantonese; CQI-CSD: Consumer Quality Index Chronic Skin Disease; DIS: Dermatology Intimacy Scale; DLQI: Dermatology Life Quality Index; DLQI-B: DLQI-Portuguese; DLQI-C: DLQI Chinese; DLQI-D: DLQI Danish; DLQI-I: DLQI Italian; DLQI-N: DLQI Norwegian; DLQI-S: DLQI Sinhala; DLQI-T: DLQI Turkish; DLQI-U: DLQI Ukrainian; DQOLs: Dermatology Quality of Life scales; DSQL: Dermatology-specific Quality of Life; FLQA-d: Freiburg Life Quality Assessment; PBI: Patient Benefit Index; PeDeSI: Person-Centred Dermatology Self-Care Index; PRISM: Pictorial Representation of Illness & Self-Measure; SF-QES: Short-form of the Questionnaire on Experience with Skin Complaints; S29: Skindex-29; S29-C: S29-Chinese; S29-G: S29-German; S29-S: S29-Serbian; S29-Sp: S29-Spanish; S16: Skindex16; S16-BP: S16-Brazilian-Portuguese; S16-A: S16-Arabic; S16-C: 16-Chinese; S16-J: S16-Japanese; S16-M: S16-Moroccan-Arabic; S16-U: S16-Ukrainian; TQL: Turkish Quality of Life Instrument for skin disease; V: very good; A: adequate; D: doubtful; I: inadequate.
Table VI.
Quality assessment of measurement properties per study according to predefined criteria proposed by Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) (12)
| PROM | Study | Structural validity | Internal consistency | Reliability | Measurement error | Construct validity | Cross-cultural validity/measurement invariance | Responsiveness |
|---|---|---|---|---|---|---|---|---|
| ACSD | (32) | ? | ||||||
| CDLQI | (33) | ? | + | |||||
| CDLQI-C | (34) | + | ? | ? | ||||
| CQI-CSD | (74) | ? | + | ? | ||||
| DIS | (35) | ? | ||||||
| DLQI | (38) | ? | ? | |||||
| (37) | + | ? | + | |||||
| (39) | ? | + | ? | |||||
| (16) | – | ? | – | |||||
| (76) | ? | ? | ± | |||||
| (75) | + | |||||||
| (36) | ? | ? | ? | |||||
| DLQI-B | (40) | + | ? | |||||
| DLQI-C | (42) | – | ? | ? | ||||
| (41) | ? | ? | ? | |||||
| (44) | + | + | ? | |||||
| (43) | + | + | ||||||
| DLQI-D | (27) | + | ? | ? | ||||
| DLQI-I | (45) | + | + | + | ||||
| DLQI-N | (46) | ? | + | ? | ||||
| DLQI-S | (30) | – | + | + | ||||
| DLQI-T | (47) | ? | + | |||||
| DLQI-U | (19) | + | ||||||
| DQOLs | (48) | ? | + | + | ± | |||
| DSQL | (50) | + | + | – | ||||
| (49) | ? | + | ? | ± | ||||
| FLQA-d | (14) | – | ? | ? | ? | |||
| PBI | (51) | + | ? | |||||
| PeDeSI | (52) | ? | + | |||||
| PRISM | (53) | + | + | |||||
| SF-QES | (29) | + | + | + | ||||
| Skindex | (54) | ? | ? | ? | + | ? | ||
| S29 | (77) | + | ||||||
| (55) | ? | + | ? | + | + | |||
| S29-C | (18) | – | ? | + | ||||
| S29-G | (56) | ? | + | ? | ? | |||
| S29-S | (31) | + | – | ± | ||||
| S29-Sp | (28) | + | + | + | + | |||
| (26) | + | + | ||||||
| S16 | (57) | + | + | + | ? | |||
| S16-A | (58) | + | + | |||||
| S16-BP | (59) | + | + | + | ||||
| S16-C | (18) | + | ? | + | ||||
| S16-J | (60) | + | + | |||||
| S16-M | (61) | + | + | + | ||||
| S16-U | (19) | + | ||||||
| TQL | (62) | ? | + | – | ? | |||
| VQ-Dermato | (63) | ? | – | ? | + | + |
PROM: patient-reported outcome measures; ACSD: Adjustment to Chronic Skin Diseases Questionnaire; CDLQI: Children’s Dermatology Life Quality Index; CDLQI-C: Children’s Dermatology Life Quality Index Cantonese; CQI-CSD: Consumer Quality Index Chronic Skin Disease; DIS: Dermatology Intimacy Scale; DLQI: Dermatology Life Quality Index; DLQI-B: DLQI Brazilian-Portuguese; DLQI-C: DLQI Chinese; DLQI-D: DLQI Danish; DLQI-I: DLQI Italian; DLQI-N: DLQI Norwegian; DLQI-S: DLQI Sinhala; DLQI-T: DLQI Turkish; DLQI-U: DLQI Ukrainian; DQOLs: Dermatology Quality of Life scales; DSQL: Dermatology-specific Quality of Life; FLQA-d: Freiburg Life Quality Assessment; PBI: Patient Benefit Index; PeDeSI: Person-Centred Dermatology Self-Care Index; PRISM: Pictorial Representation of Illness & Self-Measure; SF-QES: Short-form of the Questionnaire on Experience with Skin Complaints; S29: Skindex 29; S29-C: S29-Chinese; S29-G: S29-German; S29-S: S29-Serbian; S29-Sp: S29-Spanish; S16: Skindex-16; S16-A: S16-Arabic; S16-BP: S16-Brazilian-Portuguese; S16-C: S16-Chinese; S16-J: S16-Japanese; S16-M: S16-Moroccan-Arabic; S16-U: S16-Ukrainian; TQL: Turkish Quality of Life Instrument for skin disease; +: sufficient; –: insufficient; ±: inconsistent; ?: indeterminate.
Quality of PROMs: best-evidence synthesis and recommendations
The results of the best-evidence synthesis per PROM (Table VII) are shown below according to the category of recommendation (A–C). The results presented are an overview; a more detailed account is shown in Table SV1. The best-evidence synthesis shows the overall evidence for each measurement property per PROM expressed as 1 result, combining both the level of evidence (high, moderate, low, very low) and the quality of the measurement property (sufficient, insufficient, indeterminate, inconsistent).
Table VII.
Best-evidence synthesis and recommendations
| PROM | Content validity | Structural validity | Internal consistency | Reliability | Measurement error | Construct validity | Measurement invariance | Responsiveness | Recommendation |
|---|---|---|---|---|---|---|---|---|---|
| ACSDQ | W | ??? | B | ||||||
| CDLQI | W | W | + | B | |||||
| CDLQI-C | W | ? | W | W | B | ||||
| CQI-CSD | W | W | W | W | B | ||||
| DIS | W | ? | B | ||||||
| DLQI | W | ??? | +++ | ? | +++ | +++ | B | ||
| DLQI-B | W | ++ | B | ||||||
| DLQI-C | +++ | +++ | +++ | W | B | ||||
| DLQI-D | W | W | ??? | B | |||||
| DLQI-I | +++ | +++ | +++ | B | |||||
| DLQI-N | ?? | ++ | ++ | B | |||||
| DLQI-S | --- | W | + | C | |||||
| DLQI-T | ? | W | B | ||||||
| DLQI-U | W | B | |||||||
| DQOLs | W | ?? | W | + | – | B | |||
| DSQL | W | ??? | +++ | + | +++ | +++ | B | ||
| FLQA-d | W | +++ | ? | +++ | +++ | B | |||
| PBI | ± | ? | ? | ++ | B | ||||
| PeDeSI | W | ?? | ++ | B | |||||
| PRISM | +++ | + | B | ||||||
| SF-QES | W | --- | ++ | C | |||||
| Skindex | W | ??? | W | W | – | W | B | ||
| S29 | W | ??? | +++ | W | +++ | W | B | ||
| S29-C | W | -- | W | +++ | B | ||||
| S29-G | ??? | +++ | +++ | W | B | ||||
| S29-S | W | +++ | – | --- | C | ||||
| S29-Sp | --- | +++ | W | +++ | W | C | |||
| S16 | W | ++ | ++ | + | W | B | |||
| S16-A | +++ | ++ | B | ||||||
| S16-BP | +++ | W | +++ | B | |||||
| S16-C | W | --- | W | +++ | C | ||||
| S16-J | +++ | +++ | B | ||||||
| S16-M | W | +++ | + | +++ | B | ||||
| S16-U | ++ | B | |||||||
| TQL | ± | ?? | ++ | W | ++ | B | |||
| VQ-Dermato | W | ?? | -- | ? | +++ | ++ | B |
PROM: patient-reported outcome measures; ACSD: Adjustment to Chronic Skin Diseases Questionnaire; CDLQI: Children’s Dermatology Life Quality Index; CDLQI-C: CDLQI Cantonese; CQI-CSD: Consumer Quality Index Chronic Skin Disease; DIS: Dermatology Intimacy Scale; DLQI: Dermatology Life Quality Index; DLQI-B: DLQI Brazilian-Portuguese; DLQI-C: DLQI Chinese; DLQI-D: DLQI Danish; DLQI-I: DLQI Italian; DLQI-N: DLQI Norwegian; DLQI-S: DLQI Sinhala; DLQI-T: DLQI Turkish; DLQI-U: DLQI Ukrainian; DQOLs: Dermatology Quality of Life scales; DSQL: Dermatology-specific Quality of Life; FLQA-d: Freiburg Life Quality Assessment; PBI: Patient Benefit Index; PeDeSI: Person-Centred Dermatology Self-Care Index; PRISM: Pictorial Representation of Illness & Self-Measure; SF-QES: Short-form of the Questionnaire on Experience with Skin Complaints; S29: Skindex 29; S29-C: S29-Chinese; S29-G: S29-German; S29-S: S29-Serbian; S29-Sp: S29-Spanish; S16: Skindex-16; S16-A: S16-Arabic; S16-BP: S16-Brazilian-Portuguese; S16-C: S16-Chinese; S16-J: S16-Japanese; S16-M: S16-Moroccan-Arabic; S16-U: S16-Ukrainian; TQL: Turkish Quality of Life Instrument for skin disease; +++: High-quality evidence for a sufficient measurement property. ---: High-quality evidence for an insufficient measurement property. ???: High-quality evidence for an indeterminate measurement property. ++: Moderate evidence for a sufficient measurement property. --: Moderate evidence for an insufficient measurement property. ??: Moderate evidence for an indeterminate measurement property. +: Low-quality evidence for a sufficient measurement property. –: Low-quality evidence for an insufficient measurement property. ?: Low-quality evidence for an indeterminate measurement property. W: Very low evidence for a measurement property. ±: Conflicting evidence for a measurement property.
Category A (green traffic light). No PROMs met the requirements for use as an ideal dermatology-specific PROM.
Category C (red traffic light). Five PROMs (18, 26–31) had high-quality evidence for insufficient measurement properties and are not recommended for use: the Sinhala version of the Dermatology Life Quality Index (DLQI-S), the Short-form of the Questionnaire on Experience with Skin Complaints (SF-QES), the Serbian and Spanish versions of Skindex-29 and the Chinese version of Skindex-16.
Category B (amber traffic light). A total of 31 PROMs can be recommended for use pending further validation. Where no PROMs categorized as A are found (as here), COSMIN recommends that the PROM with the best evidence for content validity in category B could be provisionally recommended for use until further evidence is provided (9). Based on the evidence for content validity across instruments in the best-evidence synthesis, the Patient Benefit Index (PBI) and Turkish Quality of Life (TQL) instrument are provisionally recommended for use as measures of patient needs and treatment benefits, and QoL, respectively. However, it is worth noting that, although both of these have content validity studies of acceptable methodological quality, their results were inconsistent. Here, we report only on the PROMs that require further context or to provide additional information that is not shown in Tables IV–VII.
Dermatology Life Quality Index and translations
Dermatology Life Quality Index (DLQI) (36) is a QoL PROM for patients with skin disease. Minimally important difference (MID) thresh olds range between 2.34 and 5.7 (24, 37). One study found a ceiling effect with 11% of patients (22).
A number of studies assessed the structural validity of the DLQI, although most were of low methodological quality (38) or did not report statistics corresponding to the COSMIN criteria (16). One good methodological study (defined as a very good or adequate rating on the COSMIN Risk of Bias checklist) suggests that the DLQI is unidimensional (39), although relevant statistics were not reported. Sufficient internal consistency, construct validity and responsiveness were supported by high-quality evidence. There was some evidence of indeterminate reliability in the DLQI.
The measurement properties of the DLQI-Chinese have been evaluated using Rasch analysis (41, 42) and classical test theory (CTT) (43, 44). The results of the Rasch analyses do not directly correspond to the criteria for good structural validity, internal consistency and measurement invariance and, therefore, were not included in the bestevidence synthesis. There is high-quality evidence of a unidimensional structure and internal consistency. One study of adequate methodological quality found 2 factors (43), though these violated criteria for good measurement properties (Comparative Fit Index [CFI] 0.935). Another study of very good methodological quality found evidence of unidimensionality that met the criteria for good measurement properties (44). There was sufficient construct validity.
Dermatology-specific Quality of Life
Dermatology-specific Quality of Life (DSQL) (49) is a QoL PROM for patients with skin disease. Two studies found floor effects for the daily activities (25.2%), social functioning (27.6%), and work/school (41.2% and 53.8%) subscales (49, 50). High-quality evidence for sufficient internal consistency, construct validity and indeterminate structural validity was found, but low-quality evidence of sufficient reliability.
Freiburg Life Quality Assessment
The Freiburg Life Quality Assessment (FLQA) is a set of core, generic items and additional disease-specific items used to assess QoL in dermatology patients. The FLQA-d (14) is a variant of the FLQA for use with patients with long-term skin conditions. High-quality evidence for insufficient internal consistency, sufficient construct validity and responsiveness was found, but so was low-quality evidence of indeterminate reliability.
Patient Benefit Index
The Patient Benefit Index (PBI) (51) is a measure of patient needs and treatment benefits for dermatology patients. The developers found a “major floor effect”. Although the PBI showed low-quality evidence of inconsistent content validity; the overall development study was methodologically adequate and the criteria for good content validity and reviewers’ rating were sufficient overall. There was moderate evidence of sufficient responsiveness, and low-quality evidence of indeterminate internal consistency and reliability.
Skindex
Skindex (54) is a QoL PROM for patients with skin disease. High-quality evidence for indeterminate structural validity was found. Internal consistency was indeterminate because it was tested using hypothesized subscales, rather than those identified by the factor analysis. Low-quality evidence for insufficient construct validity was found.
Skindex-29 and translations
Skindex-29 (55) is a revised version of Skindex. There was high-quality evidence for sufficient internal consistency and construct validity, but also indeterminate structural validity.
Skindex-29-Chinese (18) had highquality evidence for sufficient construct validity. Moderate evidence suggested insufficient structural validity. No floor or ceiling effects were observed.
Skindex-16 and translations
Skindex-16 (57) is a revised version of Skindex-29. There was moderate evidence for sufficient structural validity and internal consistency and low-quality evidence for sufficient construct validity.
Turkish Quality of Life instrument for skin disease
Turkish Quality of Life (TQL) instrument (62) is a Turkish language QoL PROM for patients with skin disease. TQL has low-quality evidence for inconsistent content validity. The cognitive interview (n = 40) was methodologically adequate, although the results were inconsistent. Moderate evidence was found for sufficient internal consistency and construct validity, and indeterminate structural validity.
DISCUSSION
To our knowledge, this is the first study to systematically evaluate published dermatology-specific PROMs in accordance with the COSMIN guidelines. A total of 36 dermatology-specific PROMs were identified and the majority measured QoL. Examination of the instruments at the domain level revealed that no single PROM could comprehensively assess the impact of living with a skin condition according to our conceptual framework, indicating that the development of a new PRIDD measure is warranted.
Based on their reported measurement properties, no PROM met the COSMIN requirements to be recommended for unqualified use, 30 showed potential to be recommended for use, but require further validation, and 6 are not recommended for use. Of those with the potential to be recommended for use, in accordance with the COSMIN guidance, only the PBI and TQL can be provisionally recommended for use, as they have the best evidence for content validity (9).
The use of PROMs of poor or unknown quality is wasteful and unethical, in part, because measures that are not valid or reliable can produce misleading results (64). Although, in some situations, an imperfect PROM (beyond accepted levels of measurement error) may be better than no PROM; it is useful to recognize the limitations of the measure so that conclusions drawn can be tempered accordingly (7). This is pertinent in dermatology, where PROMs are used in research, including clinical trials, and in clinical practice to make individual treatment decisions. This review highlighted the paucity of high-quality evidence for dermatology-specific PROMs. These findings concur with another recent COSMIN systematic review of dermatology-specific QoL instruments used in the context of eczema (65). Of the 135 measurement properties evaluated, only 26 had evidence of both adequate methodological quality and sufficient psychometric properties. No PROM performed well across all measurement properties; evidence for measurement invariance and interpretability was lacking and measurement error was absent. Content validity is considered to be the most important measurement property (12). Because PROMs aim to capture information directly from patients, adequate patient input is necessary to establish content validity. However, all original PROM development studies identified were of low or very low methodological quality and only 1 PROM, the Spanish version of Skindex-29, underwent an additional content validity study. Together, this indicates a lack of adequate patient input to the initial development of these PROMs. Future PROM validation and development work should focus on improving the methodological quality of studies, establishing content validity and addressing gaps in known measurement properties.
Four of the 5 PROMs not recommended for use were translated versions of other PROMs, potentially indicating an issue with current practise in cross-cultural translation. Our findings cannot generalize to all translated PROMs in dermatology, as we did not find published development and validation studies for some known translations. It does seem, however, that there are issues in the translation of PROMs in this area. There was a lack of measurement invariance (or cross-cultural validity) testing for translated PROMs in any recommendation category. Measurement invariance is core to the process of validation as it provides evidence of “construct equivalence”, the assumption that items in the translated version measure the same construct in the same way as in the original version (65–68). Evidence of construct equivalence, therefore, is required to synthesize and compare data across the language versions with obvious implications for research. We believe there is a need to standardize cross-cultural translation studies of PROMs in terms of methods (e.g. back- and forward-translation procedures) and measurement properties tested.
Strengths and weakness
Given that no PROMs could be unreservedly recommended for use, it could be argued the COSMIN criteria are too strict. The COSMIN criteria were developed with a range of experts including PROM developers, psychometricians, statisticians, qualitative researchers and clinicians (69, 70). In their systematic review of dermatology-specific QoL instruments, Gabes et al. concluded that the COSMIN guidance was “less strict and slightly more sympathetic to candidate PROMs” (p. 72) (64) than the previously recommended OMERACT approach (71, 72). Use of COSMIN is a strength of this review as it: (i) reduces bias in the evaluation of measurement properties; (ii) allows comparisons between PROMs; (iii) enables standardized recommendations; and (iv) highlights issues in the field, including poor methodological quality and reporting. However, COSMIN conflates inadequate reporting of studies with poor inherent methodological quality, which reduces the validity of the best-evidence synthesis. In addition, COSMIN tools do not adequately evaluate the methodological quality of studies conducted with Rasch analysis, which is considered superior to the CTT framework, since they make limited reference to Rasch relevant statistics. Inadequate evaluation of item response theory/Rasch studies also reduces the validity of the best-evidence synthesis.
A further strength of this review is that the search strategy was developed by a multidisciplinary team with expertise in dermatology, psychology and measurement instrument development and included a COSMIN-validated search filter. Three databases recommended by a subject librarian were searched. However, reference lists of included studies were not searched, which may explain why some translated PROMs were not found. Finally, at least 3 independent reviewers were involved in screening, data extraction and analysis; 2 of whom were involved at every step to ensure consistency.
Conclusion
This study found that no dermatology-specific PROMs could be unreservedly recommended for use according to the COSMIN standards. The single most common reason for poor quality assessment was the lack of patient input to the initial development of the measure. No measure of impact across skin conditions exists in dermatology and, therefore, we argue that the new measure PRIDD, developed with substantial patient input, is warranted.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the input of those serving on the GRIDD project’s Scientific Advisory Board: Prof. Andrew Finlay (Cardiff University, UK), Professor Arnon D. Cohen (Clalit Health Services, Israel), Professor Ncoza Dlova (Nelson R Mandela School of Medicine, South Africa), Dr Toshiya Ebata (The Jikei University School of Medicine, Japan), Dr Cristina Echeverría (ECHO Psoriasis, Argentina), Dr Alice Gottlieb (Icahn School of Medicine at Mt Sinai, USA), Dr Luigi Naldi (Ospedale San Bortolo di Vincenza, Italy), Dr Lone Skov (University of Copenhagen, Denmark) and Marc Yale (International Pemphigus Pemphigoid Foundation, USA).
The authors thank the Scientific Communication Team of the IVDP, in particular Merle Twesten and Mario Gehoff, for copy editing.
The project was funded by the International Alliance of Dermatology Patient Organizations (IADPO) as part of its Global Research on the Impact of Dermatological Diseases (GRIDD) research project. The views expressed in this article are those of the authors and not necessarily those of IADPO. The funders had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation and approval of the manuscript.
Conflicts of interest. CB, MA, RP and NTS received grants from IADPO during the conduct of this study. MA created 2 measures (Patient Benefit Index and Freiburg Life Quality Assessment) that are included in this review but was not involved in the COSMIN analysis of any measure. The remaining authors have no conflicts of interest to declare.
REFERENCES
- 1.Koo J, Lebwohl A. Psycho dermatology: the mind and skin connection. Am Fam Physician 2001; 64: 1873–1878. [PubMed] [Google Scholar]
- 2.Ahmed A, Leon A, Butler DC, Reichenberg J. Quality-of-life effects of common dermatological diseases. Semin Cutan Med Surg 2013; 32: 101–109. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Constitution of the World Health Organization. Geneva: World Health Organization; 1948. [Google Scholar]
- 4.Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB, Augustin M. Psoriasis: is the impairment to a patient’s life cumulative? J Eur Acad Dermatol Venereol 2010; 24: 989–1004. [DOI] [PubMed] [Google Scholar]
- 5.Bhatti ZU, Salek MS, Finlay AY. Major life changing decisions and cumulative life course impairment. J Eur Acad Dermatol Venereol 2011; 25: 245–246; author reply 246. [DOI] [PubMed] [Google Scholar]
- 6.Terwee CB, Bot SDM, Boer MR de, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60: 34–42. [DOI] [PubMed] [Google Scholar]
- 7.DeVellis RF. Scale development: theory and applications. Fourth edition. Los Angeles: SAGE; 2017. [Google Scholar]
- 8.Souza ACd, Alexandre NMC, Guirardello EdB. Propriedades psicométricas na avaliação de instrumentos: avaliação da confiabilidade e da validade. Epidemiol Serv Saude 2017; 26: 649–659. [DOI] [PubMed] [Google Scholar]
- 9.Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, Vet HCW de, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res 2018; 27: 1147–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terwee CB, Jansma EP, Riphagen II, Vet HCW de. Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res 2009; 18: 1115–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kitchen H, Cordingley L, Young H, Griffiths CEM, Bundy C. Patient-reported outcome measures in psoriasis: the good, the bad and the missing! Br J Dermatol 2015; 172: 1210–1221. [DOI] [PubMed] [Google Scholar]
- 12.Mokkink LB, Vet HCW de, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, et al. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual Life Res 2018; 27: 1171–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feeny DH, Eckstrom E, Whitlock EP, Perdue LA. A primer for systematic reviewers on the measurement of functional status and health-related quality of life in older adults. Agency for Healthcare Research and Quality (US), Rockville, MD, USA; 2013. [PubMed] [Google Scholar]
- 14.Augustin M, Zschocke I, Seidenglanz K, Lange S, Schiffler A, Amon U. Validation and clinical results of the FLQA-d, a quality of life questionnaire for patients with chronic skin disease. Dermatol Psychosom 2000; 1: 12–17. [Google Scholar]
- 15.Schmid-Ott G, Burchard R, Niederauer HH, Lamprecht F, Künsebeck H-W. Stigmatisierungsgefühl und Lebensqualität bei Patienten mit Psoriasis und Neurodermitis. Hautarzt 2003; 54: 852–857. [DOI] [PubMed] [Google Scholar]
- 16.Ofenloch RF, Diepgen TL, Weisshaar E, Elsner P, Apfelbacher CJ. Assessing health-related quality of life in hand eczema patients: how to overcome psychometric faults when using the dermatology life quality index. Acta Derm Venereol 2014; 94: 658–662. [DOI] [PubMed] [Google Scholar]
- 17.Jobanputra R, Bachmann M. The effect of skin diseases on quality of life in patients from different social and ethnic groups in Cape Town, South Africa. Int J Dermatol 2000; 39: 826–831. [DOI] [PubMed] [Google Scholar]
- 18.He Z, Lu C, Chren M-M, Zhang Z, Li Y, Ni X, et al. Development and psychometric validation of the Chinese version of Skindex-29 and Skindex-16. Health Qual Life Outcomes 2014; 12: 190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chernyshov PV. Health-related quality of life in adult atopic dermatitis and psoriatic patients matched by disease severity. G Ital Dermatol Venereol 2016; 151: 37–43. [PubMed] [Google Scholar]
- 20.Tiedra AG de, Mercadal J, Badía X, Mascaró JM, Lozano R. A method to select an instrument for measurement of HR-QOL for cross-cultural adaptation applied to dermatology. Pharmacoeconomics 1998; 14: 405–422. [DOI] [PubMed] [Google Scholar]
- 21.Augustin M, Zschocke I, Lange S, Seidenglanz K, Amon U. Lebensqualität bei Hauterkrankungen: Vergleich verschiedener Lebensqualitäts-Fragebögen bei Psoriasis und atopischer Dermatitis. Hautarzt 1999; 50: 715–722. [DOI] [PubMed] [Google Scholar]
- 22.Hahn HB, Melfi CA, Chuang TY, Lewis CW, Gonin R, Hanna MP, et al. Use of the Dermatology Life Quality Index (DLQI) in a midwestern US urban clinic. J Am Acad Dermatol 2001; 45: 44–48. [DOI] [PubMed] [Google Scholar]
- 23.Korte J de, Mombers FMC, Sprangers MAG, Bos JD. The suitability of quality-of-life questionnaires for psoriasis research: a systematic literature review. Arch Dermatol 2002; 138: 1221–1227. [DOI] [PubMed] [Google Scholar]
- 24.Shikiar R, Harding G, Leahy M, Lennox RD. Minimal important difference (MID) of the Dermatology Life Quality Index (DLQI): results from patients with chronic idiopathic urticaria. Health Qual Life Outcomes 2005; 3: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bronsard V, Paul C, Prey S, Puzenat E, Gourraud P-A, Aractingi S, et al. What are the best outcome measures for assessing quality of life in plaque type psoriasis? A systematic review of the literature. J Eur Acad Dermatol Venereol 2010; 24: 17–22. [DOI] [PubMed] [Google Scholar]
- 26.Jones-Caballero M, Peñas PF, García-Díez A, Badía X, Chren MM. The Spanish version of Skindex-29. Int J Dermatol 2000; 39: 907–912. [DOI] [PubMed] [Google Scholar]
- 27.Zachariae R, Zachariae C, Ibsen H, Mortensen JT, Wulf HC. Dermatology life Quality Index: data from Danish inpatients and outpatients. Acta Derm Venereol 2000; 80: 272–276. [DOI] [PubMed] [Google Scholar]
- 28.Jones-Caballero M, Peñas PF, García-Díez A, Chren MM, Badía X. [The Spanish version of Skindex-29. An instrument for measuring quality of life in patients with cutaneous diseases] Med Clin (Barc) 2002; 118: 5–9 (in Spanish). [DOI] [PubMed] [Google Scholar]
- 29.Müller H, Brockow T, Franke A, Resch K-L, Calliess IT, Schmid-Ott G. Construct validity of the questionnaire on experience with skin complaints (Short Form). European Journal of Psychological Assessment 2007; 23: 176–184. [Google Scholar]
- 30.Madarasingha NP, Silva P de, Satgurunathan K. Validation study of Sinhala version of the dermatology life quality index (DLQI). Ceylon Med J 2011; 56: 18–22. [DOI] [PubMed] [Google Scholar]
- 31.Milutinović JD, Krstić N, Janković SM. Translation and validation of the Serbian version of the Skindex-29 instrument for measuring impact of skin disease on quality of life. Acta Dermatovenerol Croat 2017; 25: 120–127. [PubMed] [Google Scholar]
- 32.Stangier U, Ehlers A, Gieler U. Measuring adjustment to chronic skin disorders: validation of a self-report measure. Psychol Assess 2003; 15: 532–549. [DOI] [PubMed] [Google Scholar]
- 33.Lewis-Jones MS, Finlay AY. The Children’s Dermatology Life Quality Index (CDLQI): initial validation and practical use. Br J Dermatol 1995; 132: 942–949. [DOI] [PubMed] [Google Scholar]
- 34.Chuh AAT. Validation of a Cantonese version of the Children’s Dermatology Life Quality Index. Pediatr Dermatol 2003; 20: 479–481. [DOI] [PubMed] [Google Scholar]
- 35.Malakouti M, Brown GE, Leon A, Wang E, Naegeli AN, Edson-Heredia E, et al. The dermatologic intimacy scale: quantitatively measuring the impact of skin disease on intimacy. J Dermatolog Treat 2017; 28: 347–352. [DOI] [PubMed] [Google Scholar]
- 36.Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) – a simple practical measure for routine clinical use. Clin Exp Dermatol 1994; 19: 210–216. [DOI] [PubMed] [Google Scholar]
- 37.Shikiar R, Willian MK, Okun MM, Thompson CS, Revicki DA. The validity and responsiveness of three quality of life measures in the assessment of psoriasis patients: results of a phase II study. Health Qual Life Outcomes 2006; 4: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Twiss J, Meads DM, Preston EP, Crawford SR, McKenna SP. Can we rely on the Dermatology Life Quality Index as a measure of the impact of psoriasis or atopic dermatitis? J Invest Dermatol 2012; 132: 76–84. [DOI] [PubMed] [Google Scholar]
- 39.Lennox RD, Leahy MJ. Validation of the Dermatology Life Quality Index as an outcome measure for urticaria-related quality of life. Ann Allergy Asthma Immunol 2004; 93: 142–146. [DOI] [PubMed] [Google Scholar]
- 40.Ferraz LB, Almeida FA, Vasconcellos MR, Faccina AS, Ciconelli RM, Ferraz MB. The impact of lupus erythematosus cutaneous on the quality of life: the Brazilian-Portuguese version of DLQI. Qual Life Res 2006; 15: 565–570. [DOI] [PubMed] [Google Scholar]
- 41.Liu Y, Li T, An J, Zeng W, Xiao S. Rasch analysis holds no brief for the use of the Dermatology Life Quality Index (DLQI) in Chinese neurodermatitis patients. Health Qual Life Outcomes 2016; 14: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He Z, Lo Martire R, Lu C, Liu H, Ma L, Huang Y, et al. Rasch analysis of the dermatology life quality index reveals limited application to Chinese patients with skin disease. Acta Derm Venereol 2018; 98: 59–64. [DOI] [PubMed] [Google Scholar]
- 43.Liu J-B, Yao M-Z, Si A-L, Xiong L-K, Zhou H. Life quality of Chinese patients with chronic urticaria as assessed by the Dermatology Life Quality Index. J Eur Acad Dermatol Venereol 2012; 26: 1252–1257. [DOI] [PubMed] [Google Scholar]
- 44.He Z, Lu C, Basra MKA, Ou A, Yan Y, Li L. Psychometric properties of the Chinese version of Dermatology Life Quality Index (DLQI) in 851 Chinese patients with psoriasis. J Eur Acad Dermatol Venereol 2013; 27: 109–115. [DOI] [PubMed] [Google Scholar]
- 45.Mazzotti E, Barbaranelli C, Picardi A, Abeni D, Pasquini P. Psychometric properties of the Dermatology Life Quality Index (DLQI) in 900 Italian patients with psoriasis. Acta Derm Venereol 2005; 85: 409–413. [DOI] [PubMed] [Google Scholar]
- 46.Mørk C, Wahl A, Moum T. The Norwegian version of the dermatology life quality index: a study of validity and reliability in psoriatics. Acta Derm Venereol 2002; 82: 347–351. [DOI] [PubMed] [Google Scholar]
- 47.Balci DD, Inandi T. [Dermatology life quality index scores in lichen planus: comparison of psoriasis and healthy controls]. Arch Turkish Dermatol Venerol 2008; 42: 127 (in Turkish). [Google Scholar]
- 48.Morgan M, McCreedy R, Simpson J, Hay RJ. Dermatology quality of life scales – a measure of the impact of skin diseases. Br J Dermatol 1997; 136: 202–206. [PubMed] [Google Scholar]
- 49.Anderson RT, Rajagopalan R. Development and validation of a quality of life instrument for cutaneous diseases. J Am Acad Dermatol 1997; 37: 41–50. [DOI] [PubMed] [Google Scholar]
- 50.Anderson R, Rajagopalan R. Responsiveness of the Dermatology-specific Quality of Life (DSQL) instrument to treatment for acne vulgaris in a placebo-controlled clinical trial. Qual Life Res 1998; 7: 723–734. [DOI] [PubMed] [Google Scholar]
- 51.Augustin M, Radtke MA, Zschocke I, Blome C, Behechtnejad J, Schäfer I, et al. The patient benefit index: a novel approach in patient-defined outcomes measurement for skin diseases. Arch Dermatol Res 2009; 301: 561–571. [DOI] [PubMed] [Google Scholar]
- 52.Cowdell F, Ersser SJ, Gradwell C, Thomas PW. The Person-Centered Dermatology Self-Care Index: a tool to measure education and support needs of patients with long-term skin conditions. Arch Dermatol 2012; 148: 1251–1255. [DOI] [PubMed] [Google Scholar]
- 53.Mühleisen B, Büchi S, Schmidhauser S, Jenewein J, French LE, Hofbauer GFL. Pictorial Representation of Illness and Self Measure (PRISM): a novel visual instrument to measure quality of life in dermatological inpatients. Arch Dermatol 2009; 145: 774–780. [DOI] [PubMed] [Google Scholar]
- 54.Chren MM, Lasek RJ, Quinn LM, Mostow EN, Zyzanski SJ. Skindex, a quality-of-life measure for patients with skin disease: reliability, validity, and responsiveness. J Invest Dermatol 1996; 107: 707–713. [DOI] [PubMed] [Google Scholar]
- 55.Chren MM, Lasek RJ, Flocke SA, Zyzanski SJ. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch Dermatol 1997; 133: 1433–1440. [PubMed] [Google Scholar]
- 56.Augustin M, Wenninger K, Amon U, Schroth MJ, Küster W, Chren M, et al. German adaptation of the Skindex-29 questionnaire on quality of life in dermatology: validation and clinical results. Dermatology 2004; 209: 14–20. [DOI] [PubMed] [Google Scholar]
- 57.Chren MM, Lasek RJ, Sahay AP, Sands LP. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutan Med Surg 2001; 5: 105–110. [DOI] [PubMed] [Google Scholar]
- 58.AlGhamdi KM, AlShammari SA. Arabic version of Skindex-16: translation and cultural adaptation, with assessment of reliability and validity. Int J Dermatol 2007; 46: 247–252. [DOI] [PubMed] [Google Scholar]
- 59.Cárcano CBM, Oliveira CZ de, Paiva BSR, Paiva CE. The Brazilian version of Skindex-16 is a valid and reliable instrument to assess the health-related quality of life of patients with skin diseases. PLoS One 2018; 13: e0194492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Higaki Y, Kawamoto K, Kamo T, Horikawa N, Kawashima M, Chren M-M. The Japanese version of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Dermatol 2002; 29: 693–698. [DOI] [PubMed] [Google Scholar]
- 61.El Fakir S, Baybay H, Bendahhou K, Obtel M, Benchat L, Mernissi FZ, et al. Validation of the Skindex-16 questionnaire in patients with skin diseases in Morocco. J Dermatolog Treat 2014; 25: 106–109. [DOI] [PubMed] [Google Scholar]
- 62.Gurel MS, Yanik M, Simsek Z, Kati M, Karaman A. Quality of life instrument for Turkish people with skin diseases. Int J Dermatol 2005; 44: 933–938. [DOI] [PubMed] [Google Scholar]
- 63.Grob JJ, Auquier P, Martin S, Lançon C, Bonerandi JJ. Development and validation of a quality of life measurement for chronic skin disorders in french: VQ-Dermato. The RéseaudEpidémiolo gie en Dermatologie. Dermatology 1999; 199: 213–222. [DOI] [PubMed] [Google Scholar]
- 64.Ioannidis JPA, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet 2014; 383: 166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gabes M, Tischer C, Apfelbacher C, Ebisawa M. Measurement properties of quality-of-life outcome measures for children and adults with eczema: an updated systematic review. Pediatr Allergy Immunol 2020; 31: 66–77. [DOI] [PubMed] [Google Scholar]
- 66.Byrne BM, Campbell TL. Cross-cultural comparisons and the presumption of equivalent measurement and theoretical structure: a look beneath the surface. J Cross-Cultural Psychol 1999; 30: 555–574. [Google Scholar]
- 67.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Philadelphia, Pa 1976) 2000; 25: 3186–3191. [DOI] [PubMed] [Google Scholar]
- 68.Hawkins M, Cheng C, Elsworth GR, Osborne RH. Translation method is validity evidence for construct equivalence: analysis of secondary data routinely collected during translations of the Health Literacy Questionnaire (HLQ). BMC Med Res Methodol 2020; 20: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 2010; 63: 737–745. [DOI] [PubMed] [Google Scholar]
- 70.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 2010; 19: 539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schmitt J, Spuls P, Boers M, Thomas K, Chalmers J, Roekevisch E, et al. Towards global consensus on outcome measures for atopic eczema research: results of the HOME II meeting. Allergy (Copenhagen) 2012; 67: 1111–1117. [DOI] [PubMed] [Google Scholar]
- 72.Apfelbacher CJ, Heinl D, Prinsen CAC, Deckert S, Chalmers J, Ofenloch R, et al. Measurement properties of adult quality-of-life measurement instruments for eczema: Protocol for a systematic review. Systemat Rev 2015; 4: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Waters A, Sandhu D, Beattie P, Ezughah F, Lewis-Jones S. Severity stratification of Children’s Dermatology Life Quality Index (CDLQI) scores. Br J Dermatol 2010; 163: 121.20346023 [Google Scholar]
- 74.van Cranenburgh OD, Krol MW, Hendriks MCP, Rie MA de, Smets EMA, Korte J de, et al. Consumer Quality Index Chronic Skin Disease (CQI-CSD): a new instrument to measure quality of care from the patient’s perspective. Br J Dermatol 2015; 173: 1032–1040. [DOI] [PubMed] [Google Scholar]
- 75.Herd RM, Tidman MJ, Ruta DA, Hunter JA. Measurement of quality of life in atopic dermatitis: correlation and validation of two different methods. Br J Dermatol 1997; 136: 502–507. [PubMed] [Google Scholar]
- 76.Reilly MC, Lavin PT, Kahler KH, Pariser DM. Validation of the Dermatology Life Quality Index and the Work Productivity and Activity Impairment-Chronic Hand Dermatitis questionnaire in chronic hand dermatitis. J Am Acad Dermatol 2003; 48: 128–130. [DOI] [PubMed] [Google Scholar]
- 77.Nijsten T, Sampogna F, Abeni D. Categorization of Skindex-29 scores using mixture analysis. Dermatology 2009; 218: 151–154. [DOI] [PubMed] [Google Scholar]


