Abstract
Objectives
This study includes a systematic review of cost-effectiveness analyses (CEAs) and cost–benefit analyses (CBAs) of mindfulness-based interventions (MBIs).
Methods
A literature search was conducted using PubMed, Web of Science, JSTOR, and CINAHL for studies published between January 1985 and September 2021, including an original cost-related evaluation of an MBI. A qualitative assessment of bias was performed using the Drummond checklist.
Results
Twenty-eight mindfulness-based intervention studies (18 CEAs and 10 CBAs) were included in this review. Mindfulness-based stress reduction (MBSR) was less costly and more effective when compared with the usual care of cognitive behavioral therapy among patients with chronic lower back pain, fibromyalgia, and breast cancer. MBSR among patients with various physical/mental conditions was associated with reductions in healthcare costs. Mindfulness-based cognitive therapy (MBCT) was also less costly and more effective than the comparison group among patients with depression, medically unexplained symptoms, and multiple sclerosis. MBCT’s cost-effectiveness advantage was also identified among breast cancer patients with persistent pain, non-depressed adults with a history of major depressive disorder episodes, adults diagnosed with ADHD, and all cancer patients. From a societal perspective, the cost-saving property of mindfulness training was evident when used as the treatment of aggressive behaviors among persons with intellectual/developmental disabilities in mental health facilities.
Conclusions
Based on this review, more standardized MBI protocols such as MBSR and MBCT compare favorably with usual care in terms of health outcomes and cost-effectiveness. Other MBIs may result in cost savings from both healthcare and societal perspectives among high-risk patient populations.
Keywords: Cost-effectiveness analysis, Meditation, Mindfulness, Complementary and alternative medicine
Mindfulness-based interventions (MBIs) aim to develop a nonjudgmental awareness and experiential acceptance of present experiences (Ludwig & Kabat-Zinn, 2008). MBIs have developed over the last 30 years as a lifestyle approach to manage chronic health conditions and avert the negative psychological impacts from a range of medical and psychological disorders (Duarte et al., 2019). Mindfulness-based stress reduction (MBSR; Irving et al., 2009; Kabat-Zinn, 2009) and mindfulness-based cognitive therapy (MBCT; Teasdale et al., 2000) are commonly used MBIs found to significantly improve outcomes such as depressive symptoms, anxiety, stress, and physical functioning for patients with cancer, chronic pain, cardiovascular disease, somatic diseases, and depression (Duarte et al., 2019). There are other variations of MBIs that have also shown a positive impact on health, such as mindfulness-based positive behavior support training (MBPBS; Singh et al., 2015), meditation on the soles of the feet (a component of MBPBS; Felver & Singh, 2020; Singh et al., 2003), and mindfulness-based art therapy (MBAT; Prioli et al., 2017). With respect to the mental health challenges resulting from the COVID-19 global pandemic (Yao et al., 2020), meditation can serve as a protective factor against psychological distress (Conversano et al., 2020) and has been associated with more engagement in COVID-19 preventive health behavior (Haliwa et al., 2020). In response to social distancing and shelter-in-place pandemic protocols, MBIs have been successfully adapted to a telehealth delivery model (Chadi et al., 2020; Niles et al., 2012).
Most, if not all, health behavior interventions result in costs that must be considered when planning and allocating resources. Therefore, economic evaluations should be performed to understand the cost-effectiveness of alternative therapies such as MBIs (Reeves et al., 2019) to inform health policy, programming, and budget decisions. Such evaluations would help to objectively assess the costs and consequences of an MBI relative to an alternative course of action (Drummond et al., 2015; Duarte et al., 2019). Though several systematic reviews and meta-analyses have demonstrated the overall effectiveness of mindfulness-based training programs (Burton et al., 2017; Li et al., 2017; Xunlin et al., 2020) in improving health-related outcomes, there is a need for a systematic review to summarize and evaluate the evidence on the cost-effectiveness and cost-saving properties for MBIs. Such evidence is important for ensuring that scarce resources are allocated to health interventions that return value for money (Duarte et al., 2019). The aim of this study was to synthesize the existing evidence on the economic evaluations of MBIs by providing a systematic review of cost-effectiveness analyses (CEAs) and cost–benefit analyses (CBAs) of MBIs. The results from this study can help insurers, administrators, providers, employers, and patients to make more strategic and informed decisions related to using or enrolling in any specific types of MBIs with respect to patient conditions and needs, as well as assisting providers in anticipating and planning for costs for training and certification of MBIs.
Methods
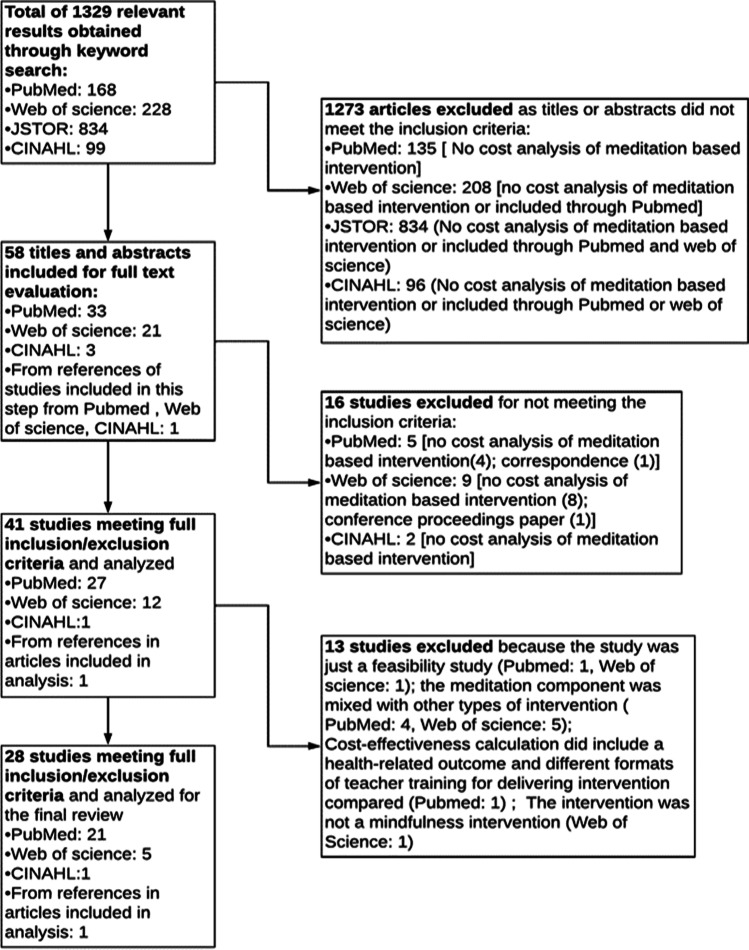
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2010). Four databases (PubMed, Web of Science, JSTOR, and CINAHL) were systematically searched for studies between January 1985 and September 2021 that matched English search terms in both cost analysis (i.e., cost-effectiveness, cost–benefit, cost-reduction, cost-utility, economic evaluation) and MBIs (i.e., meditation, mindfulness). A manual search of the references of the reviewed studies was also conducted.
Studies with standard economic evaluation designs were searched for, including CEA and CBA (Atusingwize et al., 2015). The included studies were conducted from a variety of perspectives, such as societal (Jönsson, 2009), healthcare (Kunz et al., 2016), payer (Sorensen et al., 2011), provider (Navas et al., 2007), government (Einarson et al., 1994), and employer (Grimani et al., 2018) perspectives. In the review, CEA refers to the evaluation of the effectiveness of two or more interventions relative to their cost, where benefits are measured in non-monetary units (e.g., life years gained) to obtain an incremental cost-effectiveness ratios (ICERs: defined as the ratio of the additional costs per unit of incremental benefit of an intervention; York Health Economics Consortium, 2016). A CEA enables comparison between interventions by estimating the cost for achieving a unit gain of a health outcome, for example, a life year gained (Centers for Disease Control & Prevention, 2021). When quality-adjusted life years (QALYs) are used as a CEA outcome measure, a cost per QALY is calculated (Raisch, 2000). CBA refers to the studies about the cost outcome for the healthcare system and/or the society (through reducing productivity loss, employee turnover, etc.) following the “human capital” approach of defining cost–benefit analyses (Colombo et al., 2006; Robinson, 1993).
Studies were included in this review if they (1) reported original cost-related analysis, and (2) included an evaluation of an MBI. Conference proceedings, letters to the editor, commentaries, other review studies, studies where the meditation component was mixed with other types of interventions, cost analysis studies without outcomes, and studies where the effectiveness outcome was not health related were excluded.
Data extraction, quality assessment, and evaluation of indirectness (Schünemann et al., 2020) in outcome measures were performed by the lead reviewer and validated by a second reviewer. Any disagreement was resolved through a discussion between the two reviewers to achieve a consensus or by consulting a third reviewer. Data extraction included the following characteristics of each study: study population, type of intervention, comparator, effectiveness data (CEA studies), measure of benefit (CBA studies), cost data, discounting, time horizon, study perspective, sensitivity analyses, and results. All monetary values reported were converted to 2020 US dollars to allow the comparison of results across studies. Quality assessment was conducted using the Drummond 10-point checklist (Drummond et al., 2015), a concise tool for assessing the quality and possible biases of empirical studies (Atusingwize et al., 2015). The studies were evaluated to check whether they used proxy or surrogate measures when reporting their intervention outcomes (Schünemann et al., 2020). This systematic review was not prospectively registered.
Results
The database search yielded 1329 relevant articles. One additional study was identified through manual search of the references of the included studies. After screening titles and abstracts, 1273 articles were excluded, leaving 58 articles for full-text reviews. Sixteen articles were excluded after the initial full-text review, including one conference proceeding, one correspondence article, and 14 articles without cost analyses of MBIs. Two articles (van Ravesteijn, 2016; van Ravesteijn et al., 2013) were considered a duplication since they were based on the same study. Thus, there were 41 studies included at this stage. At the final level of review for inclusion, 13 additional studies were excluded because the meditation component was mixed with other types of interventions (D’Amico et al., 2020; Doyle et al., 2019; Gaupp et al., 2020; Ljótsson et al., 2011, 2014; Mercer et al., 2016; Orme-Johnson & Herron, 1997; Stahl et al., 2015; Sun et al., 2021), they were feasibility studies with only intervention costs (Hennelly et al., 2020; Tulloh et al., 2018), the effectiveness outcome included for cost-effectiveness calculation was not a health-related outcome (e.g., teaching competency as the effectiveness outcome; Crane et al., 2020), or the meditation intervention was not an MBI (Herron, 2011), leaving 28 studies meeting the criteria to be included in this study (Fig. 1).
Fig. 1.
Search and selection process of studies
About the specific types of MBIs included in the study, MBSR (Irving et al., 2009; Kabat-Zinn, 2009), MBCT (Teasdale et al., 2000), MBPBS (Singh et al., 2015), meditation on the soles of the feet (Singh et al., 2003), MBAT (Prioli et al., 2017), and non-standarded formats of MBIs (Müller et al., 2019; Saha et al., 2020; van Dongen et al., 2016) were presented in the analyses.
Characteristics of the Studies
Tables 1 and 3 report the key characteristics of the included studies. The 28 articles were divided into two categories: (1) CEAs (n = 18) that addressed both cost (direct costs and/or indirect costs) and treatment effectiveness outcomes (Table 1); and (2) CBAs (n = 10) that focused on cost outcomes (direct costs and/or indirect costs) (Table 3). The studies included were based in nine countries: USA (n = 11), Netherlands (n = 5), UK (n = 4), Canada (n = 2), Denmark (n = 2), Sweden (n = 1), Spain (n = 1), Australia (n = 1), and Germany (n = 1). The types of interventions in the reviewed studies included MBCT (n = 10), MBSR (n = 5), MBPBS (n = 4), meditation on the soles of the feet (n = 1), MBAT (n = 1), and other MBIs (n = 7). The study design included randomized controlled trials (RCTs) (n = 17), quasi-experimental studies (n = 4), multiple baseline design studies (n = 2), observational studies (n = 2), and simulation studies (n = 3).
Table 1.
Cost-effectiveness analyses
| Author, year, country | Study population | Study design/blinding procedures | Intervention | Comparator | Effectiveness data | Measures of benefit | Perspective/time | Cost data included in the perspective | Cost currency/year | Sensitivity analyses (SA) | Results (USD in 2020) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Shawyer et al., 2016, Australia | Non-depressed adults with a history of three or more major depressive episodes | RCT/assessor blinding | MBCT—8 sessions, 2 h each, 1 session/week, w/ optional session at 3-month intervals and relapse monitoring | Depressive relapse active monitoring | Effect of treatment was measured from an RCT using the WHO CIDI question | DALYs | Societal and health care system/2 years | Health care costs (physician, hospitalization, pharmacy), costs from productivity losses due to illness | The 2009 Australian dollars/discount rate: 3% | SAs were conducted using bootstrapping methods | In 2 perspectives, MBCT was cost saving compared to UC (lower costs, higher health gains). Incremental gain per DALY for MBCT was AUD83,744 (USD91,080) net benefit, with annual cost saving of AUD143,511 (USD156,083) for people in specialist care |
| Johannsen et al., 2017, Denmark | Women with primary breast cancer and persistent pain | RCT/no blinding | MBCT—8 sessions, 2 h each, 1 session/week | No intervention (“wait-list”) | Pain intensity [minimum clinically important difference (MCID)] | Number of patients who achieved MCID in pain intensity | Health care system/8 months | Health care service utilization, medication costs, intervention delivery costs (materials and salaries of personnel) | The 2015 Euro/no discounting | SAs assessed effects of higher program cost and imputed values | MBCT group had a 729€ (USD945) lower cost per participant and 2.71 higher odds of achieving MCID in pain intensity, than control group |
| Bogosian et al., 2015, UK | Patients with multiple sclerosis (MS) | RCT/assessor blinding | eMBCT, sessions, 1 h each, 1 session/week, via skype video conference | No intervention (“wait-list”) | General health, hospital anxiety and depression scale, EQ-5D | Distress/pain/fatigue/anxiety/depression/MS impact/QALY | Societal:20 weeks from baseline | Service use and costs (including hospital, community, social care, and informal caregiver services), intervention costs (including materials, time spent by therapists) | The 2012–2013 GBP/no discounting | SAs were done to assess the impact of imputation on missing baseline variables | MBCT group cost less, had better outcomes (e.g., lower distress), is cost saving with an 87% probability of being cost-effective at threshold of 20,000 GBP (USD37,964) |
| Herman et al., 2017, USA | Patients with chronic lower back pain | RCT/clinical outcomes assessors blinded | MBSR—8 sessions, 2 h each, 1 session/week | UC, Cognitive behavioral therapy (CBT) | Effect was measured using SF-6D scores | QALYs | Societal and health plan (payer)/1 year |
Intervention cost, health plan reimbursed costs for healthcare Participants copayments for healthcare, absenteeism and presenteeism at work due to lower back pain |
The 2013 US $/no discounting | Healthcare costs for those w/ less than 1-year enrollment; types of productivity loss | MBSR had less cost (− $724 [− USD878] for societal, − $982 [− USD1191] for payer) and gains in QALYs (.034) than UC. MBSR has a 90% chance of less than $50,000/QALY (USD60,654/QALY), was cost-effective, could save costs |
| Pahlevan et al., 2020, Canada | Adults (18–65 years) with a history of 2 or more past episodes of MDD, in remission | Simulation study —meta-analysis/not applicable | MBCT, 8 weeks | m-ADM | EQ-5D scores from other studies used to calculate QALY scores | Improved QALYs over 24 month period | Healthcare and societal perspective/24 months | Cost of the intervention, maintenance antidepressant medication, healthcare cost related to relapse, productivity costs | Canadian dollar (2018) | (1) Probabilistic sensitivity analysis; (2) univariate sensitivity analysis; (3) scenarios: health care perspective and assuming 60% adherence probability for both groups | MBCT less costly (–$2224.67 (USD1826) per patient) and more effective (0.08 QALY). MBCT was cost-effective using a threshold of $50,000/QALY (USD41,048/QALY) |
| Lengacher et al., 2015, USA | Women with breast cancer | RCT/no blinding | MBSR—6 sessions, 2 h each, 1 session/week | UC | Effect was measured from an RCT using the SF-12v1 | QALYs | Societal /12 weeks | Intervention costs to the provider: personnel time, materials, environment. Intervention costs to the patient: training and travel time, transportation costs, childcare meals, lodging, lost wages due to time spent in the intervention | Not specified/discounting rate: 3% (for SAs) | SAs were done by varying efficacy and cost | ICER for MBSR was $19,733–$22,200 (USD23,058–USD25,941) per QALY gained at the 12-week time point. ICER is smaller at longer follow-up |
| van Ravesteijn et al., 2013 and van Ravesteijn 2016, Netherlands | Patients w/ medically unexplained symptoms | RCT/no blinding | MBCT—8 sessions, 2.5 h each | EUC | Effect of treatment was measured by a RCT using SF-36 | QALYs | Societal/1 year | Employment participation, health care use (including intervention cost) | The 2010 Euro/no discounting | SAs tested impact of the societal vs. healthcare perspective | Compared w/ EUC, MBCT was more costly and more effective, with an ICER of 56,637 Euro (USD99,818) per QALY gained (robust to SA) |
| Kuyken et al., 2008, UK | Patients with recurrent depression | RCT/Assessor blinding | MBCT—8 sessions w/ support to taper or stop antidepressant medication | m-ADM | Primary outcome: time to relapse or recurrence of depression | 1. Number of depression relapse/recurrences averted; 2. depression-free days (DFD) | Societal and health care system/15 months | Costs of the intervention, productivity losses (individual’s salary* days off work due to illness), hospital, community health and social services used | The 2006 US $/no discounting | Probabilistic sensitivity analyses were conducted using bootstrapping methods | ICER of MBCT over m-ADM was $962 (USD1476) per relapse prevented and $50 (USD77) per DFD (societal). ICER of MBCT over m-ADM was $439 (USD673) per relapse averted and $23/DFD (USD35/DFD) (healthcare) |
| Saha et al., 2020, Sweden | Adult patients with depression, anxiety or stress and adjustment disorder | RCT/no blinding | Based on MBSR + MBCT, 8 sessions, 2 h each, 1 session/week | UC (pharmacological treatment often accompanied by psychotherapy or counseling) | Quality of life measured using the EQ-5D-5L questionnaire | Improved QALYs at 8 weeks post-intervention follow-up as compared to baseline | Healthcare and societal perspective/8 weeks | Intervention cost, medication, healthcare visits for usual care and productivity costs |
EUR (2012) (converted from Swedish Kroner SEK 2012) No discounting |
(1) Multiple imputation for missing QALY or cost data; (2) excluding outliers; (3) accounting for attendance | The intervention had €115 (USD184) less healthcare cost and €112 (USD179) less societal costs than UC. No notable difference in QALY. At threshold of €24,691/QALY (USD39,457/QALY), MGT’s probability to be cost-effective is 67% (societal) and 70% (healthcare) |
| Kuyken et al., 2015, UK | Patients with recurrent major depression disorder | RCT/Participants blinded | MBCT: 8 sessions, 2.5 h each, 1 session/week, w/ 4 refresher sessions for 1 year + tapering support | m-ADM | Primary: time to relapse. Secondary: outcomes: depression-free days, quality-of-life, etc | Number of depression relapse/recurrence averted, number of depression-free days, and QALYs | Societal and health care system/2 years | Costs of the intervention, productivity losses, medications, other healthcare, and social services used | The 2011–2012 GBP/discounting rate: 3.5% | Probabilistic sensitivity analyses were conducted using bootstrapping methods | From either societal or healthcare system perspective, there was no evidence that MBCT is more cost-effective than m-ADM, in terms of either relapse or recurrence or QALYs |
| Prioli et al., 2017, USA | Women with breast cancer | Secondary data analysis, Quasi-experimental/not applicable | MBAT—8 2.5-h sessions, 1 session/week | Breast cancer support group (BCSG) | SF-36 | QALYs | Health care system/9 weeks | Direct costs related to intervention delivery (including travel costs for patients and providers), costs of other medical services and/or medications used by the participants | The 2011 US dollars/no discounting | SAs were conducted by varying the cost of intervention components | MBAT was $429.78 (USD554) more costly than BCSG. Both achieved similar changes in health-related utility. SAs show MBAT can be cost saving compared to BCSG |
| van Dongen et al., 2016, Netherlands | Employees of two Dutch government research institutes | RCT/no blinding | Worksite mindfulness intervention—8 sessions, 1 session/week w/ information about other health promotion activities | Information about other health promotion activities in their workplace | Work engagement, general vitality, job satisfaction, and work ability | Work engagement and vitality (societal); work engagement, job satisfaction, work ability (employer’s perspective) | Societal and Employer/12 months | Intervention development, implementation and operation costs, health care utilization, sickness absence, sports membership, presenteeism, market price payed by the employers for program implementation | The 2011 Euro/no discounting | SAs were conducted by varying cost and study population |
No significant between-group differences on job satisfaction, general vitality, and work ability. The maximum probability of cost-effectiveness was very low for all outcome, irrespective of the willingness-to-pay (0.25). Control group had more work satisfaction |
| Compen et al., 2020, Netherlands | All types of cancer patients | RCT/no blinding | (1) MBCT; (2) eMBCT. 8 sessions, 2.5 h each session, 1 session/week | UC | EQ‐5D‐3L utility scores | Improved QALYs | Societal perspective/3 months | Healthcare costs including prescriptions, formal and informal productivity costs, intervention costs | EUR (2016) | None | Effect is insignificant in both interventions (compared to controls). Lower costs for MBCT and eMBCT (compared to controls). Incremental monetary benefit over control group = €1916 (USD2358) (eMBCT) and €2365 (USD2911) (MBCT). 99% chance to be cost-effective |
| Müller et al., 2019, Germany | Adult covered under German Insurance fund AOK Baden-Wuerttemberg | Observational study with propensity score matching/not applicable | “Life Balance”, an MBI. 6 weekly sessions, one session per week, 1.5 h each and 1 additional session a month after completion of the 6 weeks sessions | UC | Hospital Anxiety and Depression Scale (HADS) score | Improvement in mental health as measured by the HADS | Healthcare and Societal perspective/12 months | Healthcare costs covered by the insurance agency and lost work days, intervention costs | EUR (2014–2015, no adjustment for time difference) | SAs controlled for the HADS psychopathological symptoms severity at baseline | From societal perspective, intervention has lower costs (€-57) (USD74) and higher effectiveness (1.97 HADS units), was cost-effective (ICER = €-29 (USD38)/ per HADS unit). From healthcare perspective, intervention has higher costs (€181) (USD235) and had ICER = €91 (USD118)/per HADS unit |
| Janssen et al., 2019, Netherlands | Adults diagnosed with ADHD | RCT/clinical outcomes assessor blinded | MBCT + UC. MBCT was 8-week intervention, 2.5 h each session, and a 6-h silent day | UC | (1) QALYs measured using SF-12; (2) ADHD symptoms measure using DSM-IV criteria | Improvement in QALYs and higher percentage of treatment responders based on ADHD symptoms score | Societal and healthcare perspective/9 months | Healthcare costs (including intervention costs), productivity loss costs | EUR (2016) | (1) Imputating missing data with last observation carried forward + multiple imputation; (2) exclude cost outliers; (3) intention to treat and per protocol analysis | Societal: higher QALYs, more treatment responders and higher costs (€183) (USD225) for intervention. ICER = €21,963 (USD27,031)/QALY gained and €389 (USD479)/responder. Intervention had 51% chance of being cost-effective at €30,000 (USD36,922) threshold. Directions of differences from healthcare perspective same as societal |
| Pérez-Aranda et al., 2019, Spain | Adults with a diagnosis of fibromyalgia | Quasi-experimental/not applicable | MBSR—8 sessions, 2 h each, one session/week; and a 6 h silent retreat between week 6 and 7 | (1) FibroQoL program (similar to MBSR but without mindfulness component); (2) UC (no active treatment with usual medications if any) | EQ-5D-5L | Improvement in QALYs and visual analogue scale (EQ VAS) score | Government and healthcare perspective/12 months | Government perspective: direct healthcare costs covered by the Catalan government and indirect costs related to productivity losses by the Spanish government. Healthcare perspective: direct health care costs, including intervention costs | EUR (2016) | Intention to treat analysis using multiple imputation for missing data and per protocol analysis | After 12 months, significant differences among 3 groups: MBSR had lowest total costs (€1557.5) ($1917) followed by FibroQol (€2015.2) ($2480) and TAU (€2528.7) ($3112). Also, the QALY was highest in the MBSR grop (0.54) followed by FibroQol (0.50) and TAU (0.48). ICERs: MBSR was dominant when compared to TAU in all analyses |
| Herman et al., 2020, USA | Adults (young and middle aged) with chronic lower back pain | Markov simulation to secondary effectiveness data /not applicable | MBSR (8 sessions, 2 h each, 1 session/week; and an optional 6 h retreat) | UC | QALYs calculated by the Markov model using secondary effectiveness data | Improvement in QALYs | Societal and payer perspective/1 year | Healthcare and productivity costs | US$ (2015) | Varying the assumption of chronic back pain severity | Compared with UC, MBSR had lower costs from societal (− $180) (− USD 210) and payer (− $52) (− USD 61) perspectives, and higher QALYs (0.007). MBSR was cost-effective (below $50,000 (USD 58,426)/QALY threshold). QALY gains and cost saving for MBSR were higher when all patients were assumed to have high-impact chronic pain |
| Bogosian et al., 2021, UK | Parkinson’s disease patients | RCT/Assessor blinding | Online MBCT modified for Parkinson’s disease (8 weekly 1-h sessions) | Wait-list control group receiving treatment-as-usual | QALY | EQ-5D-3 L | Healthcare/20 weeks | Healthcare costs | £/2016 | (1) Analyzed without imputing missing data; (2) univariate, probabilistic SA for ICER | 0.0089 QALY gain in intervention group. ICER = £27,107 (USD 40,872) |
Abbreviations: DALY, disability-adjusted life years; UC, usual care; EUC, enhanced usual care; ICER, incremental cost-effectiveness ratio; m-ADM, maintenance antidepressant medication; MBCT, mindfulness-based cognitive behavior therapy; eMBCT, MBCT delivered via an internet platform; MBSR, mindfulness-based stress reduction; MGT, mindfulness group therapy; MBAT, mindfulness-based ART therapy; QALY, quality-adjusted life years; RCT, randomized controlled trial; SA, sensitivity analysis
If there are multiple perspectives including the societal perspective, cost components of only the societal perspective are provided in the table. Monetary values with a specific year were converted to 2020 US dollars and put as USD
Table 3.
Cost–benefit analyses
| Author, year, country | Study population | Study design/blinding procedures | Intervention | Comparator | Perspective/time horizon | Cost data included in the perspective | Currency/year/discount | Results |
|---|---|---|---|---|---|---|---|---|
| Singh et al., 2016b, USA | Formal caregivers for those w/ IDD | RCT/no blinding | MBPBS | Training as usual (TAU) | Societal/40 weeks | Costs borne by the agency and workers’ compensation due to lost workdays due to injury, 1:1 patient-staff ratio, treatment for staff injuries, staff resigning, hiring temporary staff, staff required for training for the interventions | Not specified/no discounting | Compared to TAU, MBPBS was cost saving (through a reduction of aggressive events): net saving of $457,920 for 38 caregivers receiving MBPBS (− $12,051 per person in 40 weeks) |
| Singh et al., 2008, USA | Offenders with mild IDD in a forensic mental health facility | Multiple baseline design/not applicable | Meditation on soles of feet (30-min 1-on-1, 2/day, 5 d/wk, 27mon) | None | Societal/costs during 12 months prior and 12 months post intervention were analyzed | Medical care for injury of staff providing care to inmates, absenteeism, salary/worker compensation. Costs of training staff for intervention were not included | Not specified | The costs during a 12-month period following intervention decreased by 95.7% compared to the 12 months prior to intervention, a net saving of $50,346 ($8391 per participant) |
| Singh et al., 2015, USA | Formal caregivers of group homes for adults w/ IDD | Multiple baseline design/not applicable | MBPBS | None | Societal/from pre-MBPBS 40 weeks vs. 40 weeks after MBPBS begins | Cost of staff medical care due to injury, lost staff work days and staff turnover related to injury, new employee training and MBPBS training cost (costs for usual standard of care not included) | Not specified | The costs in 40 weeks during MBPBS decreased cost by 87.25% compared to the 40 weeks prior to intervention, a net reduction of $133,380.00 ($14,820/trainee) |
| Singh et al., 2016a, USA | Formal caregivers from group homes giving service to adults w/ IDD | Quasi-experimental (1 group pretest–posttest)/not applicable | MBPBS | None | Societal/40 weeks | Cost of staff medical care due to injury, lost staff work days and staff turnover related to injury, new employee training and MBPBS training cost (costs incurred by both, the service provider or by the State Worker’s Compensation were included | Not specified | Cost in 40 weeks during MBPBS decreased by 89.27% compared to the 40 weeks prior to intervention (a net saving of $447,372.00 for the provider, $13,555/trainee) |
| Fjorback et al., 2013, Denmark | Patients w/ somatization disorder and functional somatic syndromes (bodily distress syndrome) | RCT/no blinding | Mindfulness therapy (8 sessions, 3.5 h each, 1 session/week, 1 follow-up session) | EUC | Societal/15 months; healthcare/1 year | Costs included direct healthcare costs (e.g., costs of mindfulness therapy or EUC, hospitalization, etc.) and indirect costs (e.g., disability pension) | The 2007 US$ | Fewer in the therapy group (25%) got disability pension vs. ETAU (45%) at the 15-month follow-up. Care utilization was reduced in both groups from the year before |
| Knight et al., 2015, Canada | Patients with various physical /mental health conditions | Observational (prospective)/not applicable | MBSR (10-week, 9 3-h sessions, and one 7-h session) | No intervention control group | Healthcare perspective/from 1- and 2-year periods prior to MBSR to 1- and 2-yr periods after | Costs included physician-provided services, emergency department and inpatient costs | Not specified | MBSR reduced cost at 1-year pre/post intervention period ($250/person). The gap disappeared at the 2-year pre/post interval w/ the exception of laboratory utilization |
| Rakel et al., 2013, USA | Adults 50 + reporting ≥ 1 acute respiratory infection episode/year | RCT/Assessor blinding | Mindfulness meditation: 8 2.5-h classes, 1 session/week | Moderate intensity exercise group and waitlist control group | Societal/costs in the 14 weeks following the intervention were analyzed | Costs included costs related to healthcare visits and medications for acute respiratory infection, and cost from lost work time | Not specified | Total cost/person for the control group: $214, exercise group: $136, meditation group: $65. Cost saving was through reducing missed work days and was offset by the intervention ($450 per person) |
| Klatt et al., 2016, USA | Employees of a large university | Quasi-experimental with matched controls/not applicable | MBI—8 sessions, 1 h each, 1 session/week) | Matched controls from non-participants | Healthcare/5 years pre/post intervention period | Healthcare costs included all inpatient, outpatient, laboratory and pharmacy costs | Not specified | MBI group had lower healthcare cost than controls (without statistical significance). MBI group had more prescription drug cost and less primary care visits |
| Singh et al., 2020, USA | Formal caregivers for institutionalized individuals with intellectual and developmental disabilities | RCT/no blinding | MBPBS | PBS | Provider perspective/40 weeks | Costs related to absenteeism, additional temporary or permanent staffing, healthcare for worksite injuries, intervention costs | US$, year not identified/no discounting reported | The costs incurred for MBPBS ($21,000) were higher than PBS ($7000). However, total additional cost was $119,122 for MBPBS and $631,540 for PBS resulting in an overall cost saving of $512,418 for MBPBS as compared to PBS |
| Steegers-Theunissen et al., 2020, Netherlands | Couples with fertility issues and obese women undergoing reproductive technology treatment (in the context of the Netherlands) | Simulation modeling/not applicable | Mindfulness intervention | App-based coach (1) nutrition/lifestyle; (2) Outpatient support; (3) “1” and “2” combined; (4) tobacco cessation for men | Healthcare/annual costs per couple | Direct medical costs related to the intervention, fertility treatment, medication, and pregnancy (up to 6 weeks post partum) | €/2016 | Mindfulness interventions resulted in reduction in number of in vitro fertilization (IVF) treatments by 11.8%, and intracytoplasmic sperm injection (ICSI) by 0.9%. The cost saving for mindfulness intervention was €36 (USD44) per couple per year |
Abbreviations: EUC, enhanced usual care; MBCT, mindfulness-based cognitive behavior therapy; MBSR, mindfulness-based stress reduction; MBPBS, mindfulness-based positive behavior support; PBS, positive behavior support; QALY, quality-adjusted life years; RCT, randomized controlled trial; SA, sensitivity analysis; UC, usual care
Monetary values with a specific year were converted to 2020 US dollars and put as USD
If there are multiple perspectives including the societal perspective, cost components of only the societal perspective are provided in the table
Cost-effectiveness Analyses (CEAs)
Table 1 reports the findings on interventions that were both clinically effective and cost saving. To summarize, MBCT for the following types of patients had the cost-saving property in addition to effectiveness: (1) individuals with a history of major depressive disorder episodes (Pahlevan et al., 2020; Shawyer et al., 2016); (2) women with breast cancer and persistent pain (Johannsen et al., 2017); (3) multiple sclerosis patients (Bogosian et al., 2015); and (4) Parkinson’s disease patients (Bogosian et al., 2021). In addition, for patients with chronic lower back pain, the standardized protocol of MBSR also had the property of cost saving plus its effectiveness advantage as compared with the usual care of cognitive behavioral therapy (Herman et al., 2017).
Cost-effectiveness thresholds vary among countries and other entities, as these variations reflect the highest financial amount that a payer entity is willing to pay for an additional QALY. MBSR among women with breast cancer versus usual care was an illustration of interventions that improved effectiveness, but increased cost, which resulted in the cost per QALY gained of $19,733 (equivalent to $23,058 in 2020) for patients and $22,200 (equivalent to $25,941 in 2020) for providers at the 12-week time point (Lengacher et al., 2015). These values fall well below the cost-effectiveness threshold of $100 K/QALY gained (Neumann et al., 2014). For patients with medically unexplained symptoms, MBCT’s ICER as compared with enhanced usual care was 56,637 Euro, equivalent to $99,818 in 2020 per QALY gained (van Ravesteijn, 2016; van Ravesteijn et al., 2013) which fell just slightly below the threshold (Neumann et al., 2014), and £27,107 (equivalent to $40,872 in 2020) as compared to usual care (Bogosian et al., 2021).
No effectiveness advantage was documented for mindfulness group therapy using a non-standardized protocol (Bogosian et al., 2015). Saha et al. (2020) showed that mindfulness group therapy had a considerable probability of being cost-effective (67% from the societal perspective and 70% from the healthcare perspective) among adult patients with depression, anxiety or stress, and adjustment disorder as compared with usual care. Economic evaluations of less common mindfulness intervention protocols did not find the programs to be more effective or cost-effective than controls, for example, MBAT among breast cancer patients (Prioli et al., 2017) and worksite MBIs among government employees (van Dongen et al., 2016).
When costs are measured from a healthcare perspective in terms of adverse episodes averted among patients with recurrent depression, MBCT with support to taper off/stop antidepressant medication (MBCT-TS) saved $439 (equivalent to $673 in 2020) per relapse averted and $23 (equivalent to $35 in 2020) per disease-free day gained, as compared with maintenance-antidepressant medication treatment (m-ADM; Kuyken et al., 2008). This result compared favorably with the ICER of popular adjunctive therapies such as cognitive therapy (Scott et al., 2003) in depression care. However, when Kuyken et al. (2015) further tested the effectiveness and cost-effectiveness of MBCT-TS among patients with three or more major depressive disorder episodes and on prescribed medication, they found that MBCT-TS was neither more effective nor more cost-effective compared with m-ADM, though both MBCT-TS and m-ADM had enduring effectiveness.
The CEA studies included a broad variety of interventions and used different measures of costs and effectiveness. Therefore, it was not possible to statistically compare the results across studies. Instead, to categorically assess the studies, a matrix was created where individual studies were classified based on their findings as follows: (1) cost-effective, results under the threshold of $100 K/QALY or with a higher probability of increased willingness to pay (n = 9); (2) cost saving, i.e., an intervention with less costs than the comparison group with greater or equal effectiveness (n = 6); and (3) neither, interventions that reported non-statistically significant results or results with higher cost and lower benefit (n = 3). The reviewed studies are classified accordingly in Table 2.
Table 2.
Matrix of cost-effectiveness analyses’ findings (results were not limited by the threshold of 100 K per QALY but with other denominators): intervention vs. comparator
| Cost-effective | Cost saving | Neither | |
|---|---|---|---|
| MBSR |
Lengacher et al., 2015 Pérez-Aranda et al., 2019 Herman et al., 2020 |
Herman et al., 2017 | |
| MBCT |
Kuyken et al., 2008 van Ravesteijn et al., 2013 & van Ravesteijn, 2016 Janssen et al., 2019 Pahlevan et al., 2020 Bogosian et al., 2021 |
Bogosian et al., 2015 Johannsen et al., 2017 Shawyer et al., 2016 Compen et al., 2020 |
Kuyken et al., 2015 |
| Other MBIs | Müller et al., 2019 | Saha et al., 2020 |
Prioli et al., 2017 van Dongen et al., 2016 |
Cost–Benefit Analyses (CBAs)
The reviewed cost analyses included studies on caregivers (n = 4), patients (n = 3), professional caregivers of adult patients with mild intellectual disabilities (n = 1), high-cost insurance enrollees (n = 1), and employees of a large university (n = 1) (Table 3). The cost-saving property of mindfulness training was most salient when applied to societal outcomes. In particular, MBIs for aggressive behavior among individuals with intellectual/developmental disabilities in mental healthcare facilities resulted in reduced caregiver stress, injuries, and turnover (Singh et al., 2015, 2016a, b). Net savings between $12,051 and $14,820 per caregiver were achieved (Singh et al., 2015, 2016a, b). In considering additional cost benefits from the societal perspective, MBIs have demonstrated reductions in disability pensions in a Danish sample (Fjorback et al., 2013) and reduction in missed days of work in a sample of older adults with multiple respiratory infections (Rakel et al., 2013). From the healthcare perspective, findings were mixed. A Canadian study showed that MBSR among patients with multiple physical and/or mental health conditions (Knight et al., 2015) led to reductions in healthcare costs when compared to no intervention. In contrast, a study of US university employees found no relative cost differences between MBI participants and matched controls, a result attributed to fewer primary care visits but higher prescription drug costs (Klatt et al., 2016).
Quality Assessment and Evaluation of Indirectness of Outcome Measures
Results of the quality assessment of studies are presented in Table 4. Studies were rated as follows: having defined their research questions appropriately (n = 24); having clear and comprehensive description of competing alternatives (n = 22); and having identified important and relevant costs and (for CEA studies only) consequences for each alternative (n = 23). While most of the reviewed studies provided either the societal or healthcare viewpoint and all had operating costs, few included capital and operating costs (n = 2) (Kuyken et al., 2008; van Dongen et al., 2016). Most studies included appropriate and accurate measurements for outcomes (n = 21) and credible valuation of costs (for CEA studies only) and consequences (n = 21), as well as covered issues of concern to user satisfaction in their presentation and discussion of results (n = 19).
Table 4.
Quality assessment
| Author, year | Drummond’s checklist items # | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| CEA | Saha et al., 2020 | ✓ | X | ✓ | ✓ | 0 | ✓ | NA | ✓ | ✓ | ✓ |
| Bogosian et al., 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | X | |
| van Dongen et al., 2016 | ✓ | ✓ | 0 | ✓ | 0 | ✓ | NA | ✓ | ✓ | ✓ | |
| Herman et al., 2017 | ✓ | ✓ | 0 | ✓ | ✓ | 0 | NA | ✓ | 0 | X | |
| Johannsen et al., 2017 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | X | |
| Kuyken et al., 2008 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | X | ✓ | 0 | ✓ | |
| Kuyken et al., 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Lengacher et al., 2015 | ✓ | ✓ | ✓ | X | ✓ | ✓ | ✓ | ✓ | ✓ | X | |
| Prioli et al., 2017 | ✓ | X | ✓ | ✓ | 0 | ✓ | NA | ✓ | 0 | ✓ | |
| Shawyer et al., 2016 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 0 | ✓ | ✓ | ✓ | |
| van Ravesteijn et al., 2013, van Ravesteijn, 2016 | ✓ | ✓ | ✓ | ✓ | 0 | 0 | NA | ✓ | 0 | ✓ | |
| Pahlevan et al., 2020 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Compen et al., 2020 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | ✓ | |
| Müller et al., 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | ✓ | |
| Janssen et al., 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | ✓ | |
| Pérez-Aranda et al., 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | NA | ✓ | ✓ | NA | |
| Herman et al., 2020 | ✓ | ✓ | ✓ | ✓ | ✓ | 0 | NA | X | ✓ | ✓ | |
| Bogosian et al., 2021 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 0 | ✓ | ✓ | ✓ | |
| CBA | Fjorback et al., 2013 | ✓ | ✓ | NA | ✓ | 0 | ✓ | 0 | NA | ✓ | ✓ |
| Klatt et al., 2016 | ✓ | ✓ | NA | X | ✓ | ✓ | X | NA | ✓ | X | |
| Knight et al., 2015 | ✓ | X | NA | X | ✓ | ✓ | X | NA | ✓ | ✓ | |
| Rakel et al., 2013 | ✓ | ✓ | NA | X | ✓ | ✓ | NA | NA | ✓ | ✓ | |
| Singh et al., 2008 | X | X | NA | X | X | X | X | NA | X | X | |
| Singh et al., 2015 | X | X | NA | ✓ | ✓ | X | NA | NA | ✓ | X | |
| Singh et al., 2016a | X | X | NA | ✓ | ✓ | X | NA | NA | ✓ | X | |
| Singh et al., 2016b | 0 | ✓ | NA | ✓ | ✓ | X | NA | NA | ✓ | ✓ | |
| Singh et al., 2020 | ✓ | ✓ | NA | ✓ | ✓ | ✓ | NA | X | ✓ | ✓ | |
| Steegers-Theunissen et al., 2020 | ✓ | ✓ | NA | ✓ | NA | ✓ | NA | X | ✓ | ✓ | |
✓ = criteria satisfied; X = criteria not satisfied; NA = not applicable; 0 = unclear
This table is computed based upon the 10-item Drummond’s checklist: 1. Was a well-defined question posed in answerable form? 2. Was a comprehensive description of the competing alternatives given (i.e., can you tell who did what to whom, where and how often)? 3. Was the effectiveness of the programme or services established? 4. Were all the important and relevant costs and consequences for each alternative identified? 5. Were costs and consequences measured accurately in appropriate physical units (e.g., hours of nursing time, number of physician visits, lost work-days, gained life years)? 6. Were the cost and consequences valued credibly? 7. Were costs and consequences adjusted for differential timing? 8. Was an incremental analysis of costs and consequences of alternatives performed? 9. Was allowance made for uncertainty in the estimates of costs and consequences? 10. Did the presentation and discussion of study results include all issues of concern to users?
Among studies with a time horizon of at least 1 year for costs, three adjusted for differential timing and provided information on, and justification for, the discount rate used. The quality assessment of the CEA studies indicated that most studies established effectiveness of MBI at improving health outcomes (n = 16), calculated ICERs taking into account both costs and consequences to compare between the alternative treatments (n = 17), and adequately characterized uncertainty in the estimates of costs (for CEA studies only) and consequences (n = 23).
Discussion
This systematic review summarized the cost-effectiveness and cost-saving properties of 28 economic evaluations of MBIs, with a notable variety in study populations, types of MBIs, and measures and outcomes reported. Study participants included adult caregivers, specific insurance enrollees, and those with a broad range of physical, behavioral, or mental health conditions. The time horizon of MBIs varied from 8 weeks to 2 years. With few exceptions, the results of this review showed that MBIs were generally cost-effective and/or cost saving in comparison with other treatments (usual care or other non-MBI treatments), at least in the short term (< 5 years). The standardized protocols of MBSR and MBCT indicated robust empirical evidence for their cost-effective properties—a pattern consistent across different patient groups and countries. The most favorable outcomes, i.e., interventions that achieved both cost-effectiveness and cost savings, were noted for the following: (1) MBSR, for women with breast cancer (Lengacher et al., 2015), patients with chronic lower back pain (Herman et al., 2017, 2020), and patients with fibromyalgia (Pérez-Aranda et al., 2019); (2) MBCT, for patients with depression (Kuyken et al., 2008), patients with medically unexplained symptoms (van Ravesteijn, 2016; van Ravesteijn et al., 2013), patients with multiple sclerosis (Bogosian et al., 2015), women with primary breast cancer and persistent pain (Johannsen et al., 2017), non-depressed adults with a history of major depressive episodes (Pahlevan et al., 2020; Shawyer et al., 2016), adults diagnosed with ADHD (Janssen et al., 2019), and all types of cancer patients (Compen et al., 2020); and (3) other MBIs, for adults with national insurance (Müller et al., 2019).
Additionally, the cost-effectiveness advantages of MBIs were found to be most salient among participants with mental health challenges (Janssen et al., 2019; Kuyken et al., 2008; Pahlevan et al., 2020; Saha et al., 2020; Shawyer et al., 2016), breast cancer (Johannsen et al., 2017; Lengacher et al., 2015), lower back pain (Herman et al., 2017, 2020), fibromyalgia (Pérez-Aranda et al., 2019), and multiple sclerosis (Bogosian et al., 2015) with the comorbidity of pain. Among the CBAs reviewed, MBPBS for professional caregivers of persons with intellectual and developmental disabilities (Singh et al., 2008, 2015, 2016a, b, 2020) was found to have a net economic benefit, from both the healthcare and societal perspectives. When delivered to people with various physical/mental health conditions (Knight et al., 2015) or somatization disorder and functional somatic syndromes (Fjorback et al., 2013), MBIs were found to achieve cost savings from the healthcare perspective. For adults with acute infection episodes (Rakel et al., 2013) and non-clinical employees (Klatt et al., 2016), findings were inconclusive related to the cost/cost-effectiveness of MBIs reported. It is important to note that MBIs’ observed cost-effectiveness among patients with pain due to certain chronic diseases may not be generalizable for MBIs’ cost-effectiveness among all patients with chronic diseases since pain reduction is a specific outcome where MBIs have more evidential support compared with MBIs’ impact on chronic disease management in general (Hilton et al., 2017).
It is also worth noting the extent to which cost-effectiveness may vary depending on the “usual care” comparator programs’ cost volume. For example, in one study (Lengacher et al., 2015), the cost of the MBSR program to improve the QALY among breast cancer survivors comprised less than 1% of direct medical costs, whereas in another study (Fjorback et al., 2013), the MBI delivered to patients with somatization disorder and functional somatic syndromes was 5–6 times more expensive than the cost of usual care for these patients.
Although the heterogeneity in MBIs’ delivery formats, as implemented to meet the needs of vastly different populations, presented a challenge for conducting a meta-analysis of these included studies, it highlighted the utility of MBIs as being adaptable, effective, and accessible to a variety of populations. Furthermore, the findings of this study underscored the potential positive impact of MBIs on population health, especially in systems with limited resources. This review confirmed prior findings that mindfulness training is a well-established, low-cost, and scalable intervention, and can serve as an effective therapeutic treatment with relatively few adverse effects reported (Greenlee et al., 2017).
Limitations and Future Research
More research is needed to understand the long-term effectiveness of MBIs (i.e., more than 5 years). More cost-effectiveness and cost–benefit analyses for other standardized MBIs, such as mindfulness-oriented recovery enhancement (MORE; Garland et al., 2014) and mindfulness-based relapse prevention (MBRP; Witkiewitz et al., 2013), are also needed.
The absence of studies from Asia, Africa, and Latin America may have been impacted by the search strategy used in this study (database searches only conducted with English keywords), or the fact that MBIs (and the resulting academic reporting) may not be widely implemented and/or evaluated yet in these regions. The studies that met the inclusion criteria in this study were conducted in middle- and high-income countries with generally higher per capita incomes. Given the cost-effectiveness and cost-saving properties of MBIs in the findings of this study, more interventions and research are needed to document the extent to which MBIs could be successfully implemented in communities or regions with lower economic resources. Indeed, given the encouraging findings related to the cost-effectiveness and cost savings of the studies reviewed, low-resource settings might need these MBIs more than high-resource countries. In addition to health and cost-effectiveness benefits, concerns regarding participant recruitment, retention, and adoption, all of which are impacted by social determinants that may result in disparity, should also be assessed when considering implementation, sustainability, and feasibility.
Due to the variations in the types of MBIs, populations included, health outcomes targeted, differences in study designs, and time frames for assessing outcomes, it was not possible to conduct a quantitative meta-analysis of the cost saving or cost-effectiveness of MBIs. Efforts to report data that could be more easily statistically compared would assist such efforts in the future. More studies could also be done to understand better the overall cost savings of MBIs from the societal perspective, as most of the articles reviewed in this study still were limited to the healthcare perspective of cost savings.
MBSR has been shown effective in reducing symptoms of anxiety and depression, perceived stress, blood pressure, and body mass index among patients with coronary heart disease (Parswani et al., 2013). Strong and consistent evidence indicates that MBIs can lower blood pressure (Parswani et al., 2013; Shi et al., 2017), and MBSR generally shows promise in addressing symptoms for people with hypertension (Conversano et al., 2021). MBIs have growing support as a promising treatment for obesity-related eating behaviors as well (O’Reilly et al., 2014). Cost-effectiveness or cost analyses on MBIs for people with cardiovascular conditions would be informative. In addition, arthritis ranks among the top five chronic diseases which contribute the most to national healthcare expenditures (Lee et al., 2017). Economic evaluations of MBIs with demonstrated effects among arthritis patients could also be worthwhile.
Similarly, with the ongoing and growing healthcare impacts resulting from opioid addiction and other substance misuse disorders (Haight et al., 2018), MBIs for those in recovery for substance misuse disorders, such as MBRP, have been developed and standardized to become a notable option to control addictive behaviors (Garland, 2016; Grant et al., 2017; Li et al., 2017). However, economic evaluations of MBIs targeting substance misuse/relapse prevention have not been conducted. Given the substantial healthcare burden of drug and alcohol misuse disorders (Barrio et al., 2017; Inocencio et al., 2013) and MBIs’ emerging role in reducing substance abuse, future research needs to address these research gaps with rigorous study designs.
Additional research could also be done to further the understanding of the potential role of MBIs beyond the individual level. MBIs have been associated with increased labor productivity (Bhargava et al., 2001), reduced tax burden (Bhargava et al., 2001), and reductions in care facility employee turnover and disability insurance (Singh et al., 2008, 2015, 2016a, b, 2020), which provide evidence that MBIs could create cost savings for society at large. More research regarding MBIs and productivity can in turn inform discussions on issues such as private sector human resources development (Dewa & McDaid, 2011) as well as public sector investment in the future labor force.
In summary, while MBIs are not yet commonly covered by health insurance, this review study synthesized evidence for decision-making about whether MBIs should be covered by health insurance. More economic evaluations of MBIs in areas such as physical health and substance use will broaden the understanding about their cost-effectiveness and cost-saving properties for both healthcare and society.
Author Contribution
LZ contributed to the conceptualization of the study and led the methodology development. SL contributed to the methodology. LZ and SL conducted the literature search and analysis of articles, and collaborated on the writing of the manuscript and revisions. TL contributed to the methodology of the study. KOJ contributed to the article coding and manuscript writing. TL, KOJ, LC, MJ, and HZ reviewed and edited the manuscript. LS conceptualized the study and collaborated on the development of the methodology, writing of the manuscript, review, and revisions. Lingling Zhang and Snehal Lopes are the co-first authors.
Funding
This study was funded through the Greenville Health Authority (GHA) Healthy Greenville 2018 Grant Award Initiative. LS is the Principal Investigator.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
References marked with an * are included in the review
- Atusingwize E, Lewis S, Langley T. Economic evaluations of tobacco control mass media campaigns: A systematic review. Tobacco Control. 2015;24(4):320–327. doi: 10.1136/tobaccocontrol-2014-051579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrio P, Reynolds J, García-Altés A, Gual A, Anderson P. Social costs of illegal drugs, alcohol, and tobacco in the European Union: A systematic review. Drug and Alcohol Review. 2017;36(5):578–588. doi: 10.1111/dar.12504. [DOI] [PubMed] [Google Scholar]
- Bhargava A, Jamison DT, Lau LJ, Murray CJ. Modeling the effects of health on economic growth. Journal of Health Economics. 2001;20(3):423–440. doi: 10.1016/S0167-6296(01)00073-X. [DOI] [PubMed] [Google Scholar]
- Bogosian A, Chadwick P, Windgassen S, Norton S, McCrone P, Mosweu I, Silber E, Moss-Morris R. Distress improves after mindfulness training for progressive MS: A pilot randomised trial. Multiple Sclerosis Journal. 2015;21(9):1184–1194. doi: 10.1177/1352458515576261. [DOI] [PubMed] [Google Scholar]
- Bogosian A, Hurt CS, Hindle JV, McCracken LM, Vasconcelos e Sa DA, Axell S, Tapper K, Stevens J, Hirani PS, Salhab M. Acceptability and feasibility of a mindfulness intervention delivered via videoconferencing for people with Parkinson’s. Journal of Geriatric Psychiatry and Neurology. 2021;35(1):155–167. doi: 10.1177/0891988720988901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton A, Burgess C, Dean S, Koutsopoulou GZ, Hugh-Jones S. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress and Health. 2017;33(1):3–13. doi: 10.1002/smi.2673. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021). Cost-Effectiveness Analysis.https://www.cdc.gov/policy/polaris/economics/cost-effectiveness/index.html. Accessed 19 Mar 2022
- Chadi N, Weisbaum E, Vo DX, Ahola Kohut S. Mindfulness-based interventions for adolescents: Time to consider telehealth. The Journal of Alternative and Complementary Medicine. 2020;26(3):172–175. doi: 10.1089/acm.2019.0302. [DOI] [PubMed] [Google Scholar]
- Colombo GL, Ferro A, Vinci M, Zordan M, Serra G. Cost-benefit analysis of influenza vaccination in a public healthcare unit. Therapeutics and Clinical Risk Management. 2006;2(2):219–226. doi: 10.2147/tcrm.2006.2.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compen F, Adang E, Bisseling E, van der Lee M, Speckens A. Cost-utility of individual internet-based and face-to-face mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in cancer patients. Psycho-Oncology. 2020;29(2):294–303. doi: 10.1002/pon.5246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conversano C, Di Giuseppe M, Miccoli M, Ciacchini R, Gemignani A, Orrù G. Mindfulness, age and gender as protective factors against psychological distress during Covid-19 pandemic. Frontiers in Psychology. 2020;11:1900. doi: 10.3389/fpsyg.2020.01900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A. Is mindfulness-based stress reduction effective for people with hypertension? A systematic review and meta-analysis of 30 Years of evidence. International Journal of Environmental Research and Public Health. 2021;18(6):2882. doi: 10.3390/ijerph18062882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane, C., Ganguli, P., Ball, S., Taylor, L., Blakemore, S.J., Byford, S., Dalgleish, T., Ford, T., Greenberg, M., Kuyken, W., Lord Ma, L., Montero-Marin, J., Sonley, A., Ukoumunne, O. C., & Williams, J. (2020). Training school teachers to deliver a mindfulness program: Exploring scalability, acceptability, effectiveness, and cost-effectiveness. Global Advances in Health and Medicine,9, 1–15. 10.1177/2164956120964738 [DOI] [PMC free article] [PubMed]
- D’Amico F, Feliu-Soler A, Montero-Marín J, Peñarrubía-María MT, Navarro-Gil M, Van Gordon W, García-Campayo J, Luciano JV. Cost-utility of attachment-based compassion therapy (ABCT) for fibromyalgia compared to relaxation: A pilot randomized controlled trial. Journal of Clinical Medicine. 2020;9(3):726. doi: 10.3390/jcm9030726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewa, C. S., & McDaid, D. (2011). Investing in the mental health of the labor force: Epidemiological and economic impact of mental health disabilities in the workplace. In I. Z. Schultz & E. S. Rogers (Eds.), Work accommodation and retention in mental health (pp. 33–51). Springer. 10.1007/978-1-4419-0428-7_2
- Doyle SL, Brown JL, Rasheed D, Jones DE, Jennings PA. Cost analysis of ingredients for successful implementation of a mindfulness-based professional development program for teachers. Mindfulness. 2019;10(1):122–130. doi: 10.1007/s12671-018-0958-4. [DOI] [Google Scholar]
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford University Press; 2015. [Google Scholar]
- Duarte R, Lloyd A, Kotas E, Andronis L, White R. Are acceptance and mindfulness-based interventions ‘value for money’? Evidence from a systematic literature review. British Journal of Clinical Psychology. 2019;58(2):187–210. doi: 10.1111/bjc.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einarson TR, Arikian SR, Shear NH. Cost-effectiveness analysis for onychomycosis therapy in Canada from a government perspective. British Journal of Dermatology. 1994;130:32–34. doi: 10.1111/j.1365-2133.1994.tb06092.x. [DOI] [PubMed] [Google Scholar]
- Felver JC, Singh NN. Mindfulness in the classroom: An evidence-based program to reduce disruptive behavior and increase academic engagement. New Harbinger Publications; 2020. [Google Scholar]
- Fjorback LO, Carstensen T, Arendt M, Ornbøl E, Walach H, Rehfeld E, Fink P. Mindfulness therapy for somatization disorder and functional somatic syndromes: Analysis of economic consequences alongside a randomized trial. Journal of Psychosomatic Research. 2013;74(1):41–48. doi: 10.1016/j.jpsychores.2012.09.010. [DOI] [PubMed] [Google Scholar]
- Garland E. Restructuring reward processing with mindfulness-oriented recovery enhancement: Novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Annals of the New York Academy of Sciences. 2016;1373(1):25–37. doi: 10.1111/nyas.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82(3):448–459. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaupp R, Walter M, Bader K, Benoy C, Lang UE. A two-day acceptance and commitment therapy (ACT) workshop increases presence and work functioning in healthcare workers. Frontiers in Psychiatry. 2020;11:861. doi: 10.3389/fpsyt.2020.00861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant S, Colaiaco B, Motala A, Shanman R, Booth M, Sorbero M, Hempel S. Mindfulness-based relapse prevention for substance use disorders: A systematic review and meta-analysis. Journal of Addiction Medicine. 2017;11(5):386–396. doi: 10.1097/ADM.0000000000000338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenlee H, DuPont-Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, Johnson JA, Mumber M, Seely D, Zick SM. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: A Cancer Journal for Clinicians. 2017;67(3):194–232. doi: 10.3322/caac.21397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimani A, Bergström G, Casallas MIR, Aboagye E, Jensen I, Lohela-Karlsson M. Economic evaluation of occupational safety and health interventions from the employer perspective: A systematic review. Journal of Occupational and Environmental Medicine. 2018;60(2):147–166. doi: 10.1097/JOM.0000000000001224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization—United States, 1999–2014. Morbidity and Mortality Weekly Report. 2018;67(31):845–849. doi: 10.15585/mmwr.mm6731a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haliwa I, Lee J, Wilson J, Shook NJ. Mindfulness and engagement in COVID-19 preventive behavior. Preventive Medicine Reports. 2020;20:101246. doi: 10.1016/j.pmedr.2020.101246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennelly SE, Perman-Howe P, Foxcroft DR, Smith LA. The feasibility of ‘Mind the Bump’: A mindfulness based maternal behaviour change intervention. Complementary Therapies in Clinical Practice. 2020;40:101178. doi: 10.1016/j.ctcp.2020.101178. [DOI] [PubMed] [Google Scholar]
- Herman PM, Anderson ML, Sherman KJ, Balderson BH, Turner JA, Cherkin DC. Cost-effectiveness of mindfulness-based stress reduction versus cognitive behavioral therapy or usual care among adults with chronic low back pain. Spine. 2017;42(20):1511–1520. doi: 10.1097/BRS.0000000000002344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman PM, McBain RK, Broten N, Coulter ID. Update of Markov Model on the cost-effectiveness of nonpharmacologic interventions for chronic low back pain compared to usual care. Spine. 2020;45(19):1383–1385. doi: 10.1097/BRS.0000000000003539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herron RE. Changes in physician costs among high-cost transcendental meditation practitioners compared with high-cost nonpractitioners over 5 years. American Journal of Health Promotion. 2011;26(1):56–60. doi: 10.4278/ajhp.100729-ARB-258. [DOI] [PubMed] [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inocencio TJ, Carroll NV, Read EJ, Holdford DA. The economic burden of opioid-related poisoning in the United States. Pain Medicine. 2013;14(10):1534–1547. doi: 10.1111/pme.12183. [DOI] [PubMed] [Google Scholar]
- Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR) Complementary Therapies in Clinical Practice. 2009;15(2):61–66. doi: 10.1016/j.ctcp.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Janssen L, Grutters JP, Schellekens MP, Kan CC, Carpentier PJ, Sizoo B, Hepark S, Buitelaar JK, Speckens AE. Mindfulness-based cognitive therapy versus treatment as usual in adults with ADHD: A trial-based economic evaluation. Mindfulness. 2019;10(9):1803–1814. doi: 10.1007/s12671-019-01133-7. [DOI] [Google Scholar]
- Johannsen M, Sørensen J, O’Connor M, Jensen AB, Zachariae R. Mindfulness-based cognitive therapy (MBCT) is cost-effective compared to a wait-list control for persistent pain in women treated for primary breast cancer—Results from a randomized controlled trial. Psycho-Oncology. 2017;26(12):2208–2214. doi: 10.1002/pon.4450. [DOI] [PubMed] [Google Scholar]
- Jönsson B. Ten arguments for a societal perspective in the economic evaluation of medical innovations. The European Journal of Health Economics. 2009;10(4):357–359. doi: 10.1007/s10198-009-0173-2. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta; 2009. [Google Scholar]
- Klatt MD, Sieck C, Gascon G, Malarkey W, Huerta T. A healthcare utilization cost comparison between employees receiving a worksite mindfulness or a diet/exercise lifestyle intervention to matched controls 5 years post intervention. Complementary Therapies in Medicine. 2016;27:139–144. doi: 10.1016/j.ctim.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Knight RW, Bean J, Wilton AS, Lin E. Cost-Effectiveness of the Mindfulness-Based Stress Reduction Methodology. Mindfulness. 2015;6(6):1379–1386. doi: 10.1007/s12671-015-0408-5. [DOI] [Google Scholar]
- Kunz WG, Hunink MM, Sommer WH, Beyer SE, Meinel FG, Dorn F, Wirth S, Reiser MF, Ertl-Wagner B, Thierfelder KM. Cost-effectiveness of endovascular stroke therapy: A patient subgroup analysis from a US healthcare perspective. Stroke. 2016;47(11):2797–2804. doi: 10.1161/STROKEAHA.116.014147. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): A randomised controlled trial. The Lancet. 2015;386(9988):63–73. doi: 10.1016/S0140-6736(14)62222-4. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, Barrett B, Byng R, Evans A, Mullan E, Teasdale JD. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology. 2008;76(6):966–978. doi: 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- Lee AC, Harvey WF, Price LL, Morgan LP, Morgan NL, Wang C. Mindfulness is associated with psychological health and moderates pain in knee osteoarthritis. Osteoarthritis and Cartilage. 2017;25(6):824–831. doi: 10.1016/j.joca.2016.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengacher CA, Kip KE, Reich RR, Craig BM, Mogos M, Ramesar S, Paterson CL, Farias JR, Pracht E. A cost-effective mindfulness stress reduction program: A randomized control trial for breast cancer survivors. Nursing Economics. 2015;33(4):210–232. [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, Lazar M. Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2017;75:62–96. doi: 10.1016/j.jsat.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Ljótsson B, Andersson G, Andersson E, Hedman E, Lindfors P, Andréewitch S, Rück C, Lindefors N. Acceptability, effectiveness, and cost-effectiveness of internet-based exposure treatment for irritable bowel syndrome in a clinical sample: A randomized controlled trial. BMC Gastroenterology. 2011;11(1):1–13. doi: 10.1186/1471-230X-11-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljótsson B, Atterlöf E, Lagerlöf M, Andersson E, Jernelöv S, Hedman E, Kemani M, Wicksell RK. Internet-delivered acceptance and values-based exposure treatment for fibromyalgia: A pilot study. Cognitive Behaviour Therapy. 2014;43(2):93–104. doi: 10.1080/16506073.2013.846401. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- Mercer SW, Fitzpatrick B, Guthrie B, Fenwick E, Grieve E, Lawson K, Boyer N, McConnachie A, Lloyd SM, O’Brien R. The CARE Plus study–a whole-system intervention to improve quality of life of primary care patients with multimorbidity in areas of high socioeconomic deprivation: Exploratory cluster randomised controlled trial and cost-utility analysis. BMC Medicine. 2016;14(1):88. doi: 10.1186/s12916-016-0634-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group, P Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Müller G, Pfinder M, Schmahl C, Bohus M, Lyssenko L. Cost-effectiveness of a mindfulness-based mental health promotion program: Economic evaluation of a nonrandomized controlled trial with propensity score matching. BMC Public Health. 2019;19(1):1309. doi: 10.1186/s12889-019-7585-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navas E, Salleras L, Domínguez A, Ibanez D, Prat A, Sentís J, Garrido P. Cost-effectiveness analysis of inactivated virosomal subunit influenza vaccination in children aged 3–14 years from the provider and societal perspectives. Vaccine. 2007;25(16):3233–3239. doi: 10.1016/j.vaccine.2007.01.038. [DOI] [PubMed] [Google Scholar]
- Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. The New England Journal of Medicine. 2014;371(9):796–797. doi: 10.1056/NEJMp1405158. [DOI] [PubMed] [Google Scholar]
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(5):538. doi: 10.1037/a0026161. [DOI] [Google Scholar]
- O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: A literature review. Obesity Reviews. 2014;15(6):453–461. doi: 10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orme-Johnson DW, Herron RE. An innovative approach to reducing medical care utilization and expenditures. The American Journal of Managed Care. 1997;3(1):135–144. [PubMed] [Google Scholar]
- Pahlevan T, Ung C, Segal Z. Cost–utility analysis of mindfulness-based cognitive therapy versus antidepressant pharmacotherapy for prevention of depressive relapse in a Canadian context. The Canadian Journal of Psychiatry. 2020;65(8):568–576. doi: 10.1177/0706743720904613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parswani MJ, Sharma MP, Iyengar SS. Mindfulness-based stress reduction program in coronary heart disease: A randomized control trial. International Journal of Yoga. 2013;6(2):111–117. doi: 10.4103/0973-6131.113405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Aranda A, D’Amico F, Feliu-Soler A, McCracken LM, Peñarrubia-María MT, Andrés-Rodríguez L, Angarita-Osorio N, Knapp M, García-Campayo J, Luciano JV. Cost–utility of mindfulness-based stress reduction for fibromyalgia versus a multicomponent intervention and usual care: A 12-month randomized controlled trial (EUDAIMON Study) Journal of Clinical Medicine. 2019;8(7):1068. doi: 10.3390/jcm8071068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prioli KM, Pizzi LT, Kash KM, Newberg AB, Morlino AM, Matthews MJ, Monti DA. Costs and effectiveness of mindfulness-based art therapy versus standard breast cancer support group for women with cancer. American Health and Drug Benefits. 2017;10(6):288–295. [PMC free article] [PubMed] [Google Scholar]
- Raisch DW. Understanding quality-adjusted life years and their application to pharmacoeconomic research. Annals of Pharmacotherapy. 2000;34(7–8):906–914. doi: 10.1345/aph.19314. [DOI] [PubMed] [Google Scholar]
- Rakel D, Mundt M, Ewers T, Fortney L, Zgierska A, Gassman M, Barrett B. Value associated with mindfulness meditation and moderate exercise intervention in acute respiratory infection: The MEPARI Study. Family Practice. 2013;30(4):390–397. doi: 10.1093/fampra/cmt008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves P, Edmunds K, Searles A, Wiggers J. Economic evaluations of public health implementation-interventions: A systematic review and guideline for practice. Public Health. 2019;169:101–113. doi: 10.1016/j.puhe.2019.01.012. [DOI] [PubMed] [Google Scholar]
- Robinson R. Cost-benefit analysis. British Medical Journal. 1993;307(6909):924–926. doi: 10.1136/bmj.307.6909.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Jarl J, Gerdtham U, Sundquist K, Sundquist J. Economic evaluation of mindfulness group therapy for patients with depression, anxiety, stress and adjustment disorders compared with treatment as usual. British Journal of Psychiatry. 2020;216(4):197–203. doi: 10.1192/bjp.2018.247. [DOI] [PubMed] [Google Scholar]
- Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, Bossuyt P, Glasziou P, Jaeschke R, Lange S. GRADE guidelines: 21 part 1. Study design, risk of bias, and indirectness in rating the certainty across a body of evidence for test accuracy. Journal of Clinical Epidemiology. 2020;122:129–141. doi: 10.1016/j.jclinepi.2019.12.020. [DOI] [PubMed] [Google Scholar]
- Scott J, Palmer S, Paykel E, Teasdale J, Hayhurst H. Use of cognitive therapy for relapse prevention in chronic depression: Cost-effectiveness study. The British Journal of Psychiatry. 2003;182(3):221–227. doi: 10.1192/bjp.182.3.221. [DOI] [PubMed] [Google Scholar]
- Shawyer F, Enticott JC, Özmen M, Inder B, Meadows GN. Mindfulness-based cognitive therapy for recurrent major depression: A ‘best buy’ for health care? Australian & New Zealand Journal of Psychiatry. 2016;50(10):1001–1013. doi: 10.1177/0004867416642847. [DOI] [PubMed] [Google Scholar]
- Shi L, Zhang D, Wang L, Zhuang J, Cook R, Chen L. Meditation and blood pressure: A meta-analysis of randomized clinical trials. Journal of Hypertension. 2017;35(4):696–706. doi: 10.1097/HJH.0000000000001217. [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Karazsia BT, Myers RE. Caregiver training in mindfulness-based positive behavior supports (MBPBS): Effects on caregivers and adults with intellectual and developmental disabilities. Frontiers in Psychology. 2016;7:98. doi: 10.3389/fpsyg.2016.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Karazsia BT, Chan J, Winton ASW. Effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) vs. training-as-usual (TAU): A randomized controlled trial. Frontiers in Psychology. 2016;7:1549. doi: 10.3389/fpsyg.2016.01549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Winton ASW, Singh AN, Adkins AD, Singh J. Clinical and benefit—cost outcomes of teaching a mindfulness-based procedure to adult offenders with intellectual disabilities. Behavior Modification. 2008;32(5):622–637. doi: 10.1177/0145445508315854. [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Medvedev ON, Myers RE, Chan J, McPherson CL, Jackman MM, Kim E. Comparative effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) and positive behavior support (PBS) in a randomized controlled trial. Mindfulness. 2020;11(1):99–111. doi: 10.1007/s12671-018-0895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Karazsia BT, Myers RE, Winton AS, Latham LL, Nugent K. Effects of training staff in MBPBS on the use of physical restraints, staff stress and turnover, staff and peer injuries, and cost effectiveness in developmental disabilities. Mindfulness. 2015;6(4):926–937. doi: 10.1007/s12671-014-0369-0. [DOI] [Google Scholar]
- Singh NN, Wahler RG, Adkins AD, Myers RE, Mindfulness Research Group Soles of the feet: A mindfulness-based self-control intervention for aggression by an individual with mild mental retardation and mental illness. Research in Developmental Disabilities. 2003;24(3):158–169. doi: 10.1016/S0891-4222(03)00026-X. [DOI] [PubMed] [Google Scholar]
- Sorensen SV, Kansal AR, Connolly S, Peng S, Linnehan J, Bradley-Kennedy C, Plumb JM. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: A Canadian payer perspective. Thrombosis and Haemostasis. 2011;105(05):908–919. doi: 10.1160/TH11-02-0089. [DOI] [PubMed] [Google Scholar]
- Stahl JE, Dossett ML, LaJoie AS, Denninger JW, Mehta DH, Goldman R, Fricchione GL, Benson H. Relaxation response and resiliency training and its effect on healthcare resource utilization. PLoS One. 2015;10(10):e0140212. doi: 10.1371/journal.pone.0140212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steegers-Theunissen R, Hoek A, Groen H, Bos A, van den Dool G, Schoonenberg M, Smeenk J, Creutzberg E, Vecht L, Starmans L. Pre-conception interventions for subfertile couples undergoing assisted reproductive technology treatment: Modeling analysis. JMIR mHealth and uHealth. 2020;8(11):e19570. doi: 10.2196/19570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Wong SY, Zhang D, Chen CH, Yip BH. Behavioral activation with mindfulness in treating subthreshold depression in primary care: A cost-utility and cost-effectiveness analysis alongside a randomized controlled trial. Journal of Psychiatric Research. 2021;132:111–115. doi: 10.1016/j.jpsychires.2020.10.006. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68(4):615–623. doi: 10.1037//0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- Tulloh R, Garratt V, Tagney J, Turner-Cobb J, Marques E, Greenwood R, Howard L, Gin-Sing W, Barton A, Ewings P. A pilot randomised controlled trial investigating a mindfulness-based stress reduction (MBSR) intervention in individuals with pulmonary arterial hypertension (PAH): The PATHWAYS study. Pilot and Feasibility Studies. 2018;4(1):78. doi: 10.1186/s40814-018-0270-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dongen JM, van Berkel J, Boot C, Bosmans JE, Proper KI, Bongers PM, van der Beek AJ, van Tulder MW, van Wier MF. Long-term cost-effectiveness and return-on-investment of a mindfulness-based worksite intervention: Results of a randomized controlled trial. Journal of Occupational and Environmental Medicine. 2016;58(6):550–560. doi: 10.1097/JOM.0000000000000736. [DOI] [PubMed] [Google Scholar]
- van Ravesteijn H. Mindfulness-based cognitieve therapie voor patiënten met somatoforme stoornissen. Tijdschrift Voor Psychiatrie. 2016;58(3):198–206. [PubMed] [Google Scholar]
- van Ravesteijn H, Grutters J, Olde Hartman T, Lucassen P, Bor H, van Weel C, van der Wilt GJ, Speckens A. Mindfulness-based cognitive therapy for patients with medically unexplained symptoms: A cost-effectiveness study. Journal of Psychosomatic Research. 2013;74(3):197–205. doi: 10.1016/j.jpsychores.2013.01.001. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addictive Behaviors. 2013;38(2):1563–1571. doi: 10.1016/j.addbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xunlin NG, Lau Y, Klainin-Yobas P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: A systematic review and meta-analysis. Supportive Care in Cancer. 2020;28(4):1563–1578. doi: 10.1007/s00520-019-05219-9. [DOI] [PubMed] [Google Scholar]
- Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Health Economics Consortium. (2016). Cost-effectiveness analysis [online]. https://yhec.co.uk/glossary/cost-effectiveness-analysis/. Accessed 19 Mar 2022