Abstract
Purpose of Review
The COVID-19 pandemic has placed unprecedented challenges on breast cancer patients and health care providers. The impact of the pandemic on preexisting breast cancer disparities remains unknown but is projected to have adverse outcomes.
Recent Findings
Early work has demonstrated that pandemic-related temporary suspensions in breast cancer screening, interruption of clinical trials, and treatment delays have an adverse impact on breast cancer patient outcomes and may worsen disparities.
Summary
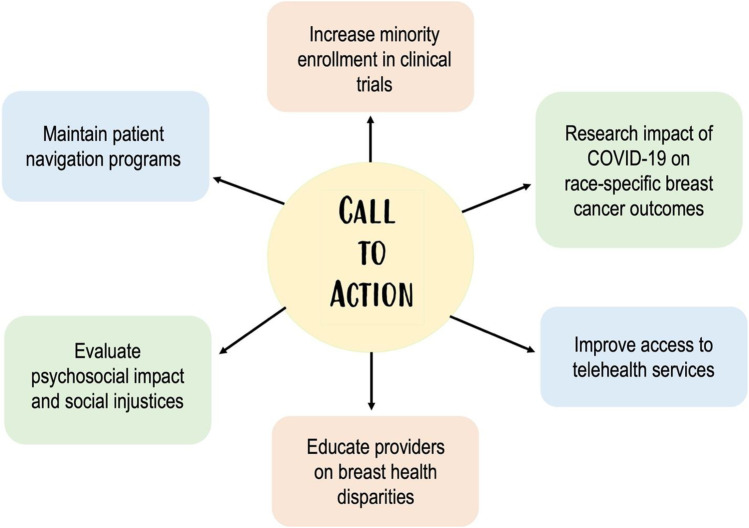
In this review, we highlight existing knowledge regarding breast cancer disparities and the impact of the COVID-19 pandemic. Strategies for mitigating disparities moving forward include targeted research evaluating race-specific outcomes, targeted education for providers regarding breast health disparities, improved access to telehealth, maintenance of patient navigation programs, and patient education regarding the safety and necessity of enrollment in clinical trials.
Keywords: Breast cancer, Health disparities, COVID-19 pandemic, Breast cancer disparities, Social determinants of health
Introduction
Breast cancer is the most common cancer diagnosed among women in the USA after skin cancer and is the second leading cause of cancer death after lung cancer. While White women have the highest breast cancer incidence rate (130.8 per 100,000), Black women have the highest mortality rate (28.4 per 100,000) which is 40% higher than that of White women (20.3 per 100,000). These disparities are in part driven by differences in presentation, biology, and phenotype of breast cancer among Black women. Population-based estimates show that 8% of Black women with breast cancer are diagnosed with metastatic disease, compared to only 5–6% of women from other racial/ethnic groups. Additionally, Black women are most likely to be diagnosed with tumors that are ≥ 5 cm and are the only group for which high-grade tumors are more common than low- or intermediate-grade lesions. Tumors lacking the estrogen, progesterone, and HER2/neu receptor (triple negative tumors) are also diagnosed more frequently among black women (19% Black vs. 9% White) [1].
Reasons for these striking differences are complex and involve not only biological factors, but also social determinants of health, access to care, genetics/genomics, and disproportionate representation in clinical trials. For example, 2020 Census data reveal that the poverty rate for non-Hispanic Whites is 8.2% compared to 19.5% for Blacks and 17% for Hispanics [2]. Additionally, the percentage of Blacks and Hispanics without health insurance coverage was 9.6% compared to 5.2% for Whites in 2020 [3]. This impacts the ability to undergo timely cancer screening. The most recent American Cancer Society data estimates that only 39% of uninsured women had a mammogram within the last 2 years compared to 75% of those with health insurance [4]. Furthermore, a recent systematic review and meta-analysis showed that Black and Hispanic populations had lower odds of utilizing screening mammography compared to White patients (OR 0.81, 95% confidence interval 0.72–0.91) [5]. Compounding these socioeconomic factors, recent work has indicated a genetic basis for these differences, particularly among breast cancer patients. Increased frequency of pathogenic variants of the BRCA1 and BRCA2 genes has been reported among Black and Hispanic patients, which confers an increased lifetime risk of developing breast cancer [6]. Importantly, reduced participation in clinical trials by racial and ethnic minorities has hindered scientific progress to design more targeted therapies to account for biological differences in disease [7, 8].
The COVID-19 Pandemic Exacerbates Cancer Disparities
The COVID-19 pandemic has placed an unprecedented strain on the US healthcare system and has illuminated preexisting healthcare disparities. Trends in morbidity and mortality from COVID-19 infection have mirrored disparities in other diseases including breast cancer. Like cancer, risk for COVID-19 infection is influenced by both a patient’s genetic makeup such as cellular expression of angiotensin-converting enzyme 2 receptors as well as socioeconomic factors including lifestyle factors and access to medical care. These similarities in risk among African American populations are evidenced by the higher risk of acquiring and dying from the disease [9••]. The disproportionate impact of COVID-19 on racial and ethnic minorities has been well-documented over the last 2 years. Like breast cancer, age-adjusted mortality and hospitalization rates for COVID-19 demonstrate that Black patients are more than three times as likely to be hospitalized and more than twice as likely to die from COVID-19 compared to their White counterparts [10]. This disparity has multiple driving factors, including differences in comorbidities, types of jobs held by minorities and the inability to work remotely, living conditions with multiple generations living in one household, and reduced access to healthcare [11]. The COVID-19 pandemic has been projected to result in 10,000 additional cancer deaths because of decreased access to screening [12]. Simultaneously, the pandemic is projected to worsen disparities by amplifying pre-existing issues that normally limit access to healthcare, such as financial insecurity, loss of employment leading to loss of employer-sponsored health coverage, and difficulty obtaining childcare [13, 14].
The COVID-19 Adverse Impact on Breast Cancer Screening
Population-based modeling suggests that a substantial increase in avoidable cancer deaths may occur due to diagnostic delays resulting from the COVID-19 pandemic [15]. Temporary suspension of elective healthcare has led to a reduction in the availability of breast cancer screening. This may lead to more advanced disease presentation, especially among patient subsets that are already more likely to present with later stage tumors and have difficulties accessing healthcare. Few studies have sought to evaluate how the reduction in breast cancer screening may have disproportionately impacted women of racial and ethnic minorities.
For example, Amram and colleagues investigated the impact of COVID-19 on breast cancer screening among different socioeconomic groups utilizing 55,678 screening mammograms within a large statewide nonprofit community healthcare system. From 2019 to 2020, a 49% decrease in screenings was observed with significant differences in the demographics of patients within each year. Greater reductions in screening were observed among Hispanic, American Indian/Alaska Native, mixed race, Native Hawaiian or Pacific Islander, and Black women compared to White. Additionally, when stratified by insurance status, patients who self-paid or were insured by Medicaid experienced the largest reduction in screening [16].
Another cross-sectional analysis evaluating trends in breast cancer screening at a US safety-net hospital stratified patients into groups based on pandemic phase (e.g., pre-COVID, first stay-at-home order, reopening, second stay-at-home order). Compared to pre-COVID, significant reductions in the volume of completed mammograms was observed during the second stay-at-home order with the largest reduction seen among Black/African American and LatinX women (− 10% for White, − 15% for Asian, − 20% for LatinX, and − 21% for Black/African American) [17].
Regional differences in the magnitude of the reduction in screening have also occurred, due to differences in timing and severity of the incidence of COVID-19 infections. Screening within the Northeast appears to have been affected most substantially. For example, data from the National Breast and Cervical Cancer Early Detection Program showed that screening for breast and cervical cancer declined most in New York, up to 96% for breast cancer [18]. Other work has also found regional differences in the magnitude of reduction in screening with the Northeast demonstrating the sharpest decline compared to other regions in the USA [19••].
Aside from race, other factors associated with obtaining delayed breast imaging during the pandemic have included younger age, higher total household residents, personal history of COVID-19 infection, and the need to quarantine [20]. Furthermore, a lower likelihood of returning to breast cancer screening after COVID-19-related closures has been independently associated with residence in a higher poverty area, lack of health insurance, need for an interpreter, longer travel time, and higher utilization of mobile mammography services [21].
Reduced Access to Clinical Trials During the COVID-19 Pandemic
Clinical trials serve as a powerful mechanism to improve the standard of care for breast cancer patients. Most trials aim to replicate the existing racial and ethnic distribution seen within the general population. However, a significant flaw within oncology research is that racial and ethnic minorities are underrepresented [22]. Furthermore, minority groups, particularly African American women, are overrepresented among more advanced stages of disease that may seek to benefit from results of these clinical trials. A recent review of the clinical trial registry found that between 2009 and 2019, Black and Hispanic patients represented only 2.47% and 2.30%, respectively, of enrollees in clinical trials for oral chemotherapy agents [8]. Reasons for this are multifactorial but include longstanding mistrust and fear of the healthcare system [23].
The COVID-19 pandemic has placed unprecedented challenges on the healthcare system and has also negatively impacted patients’ access to clinical trials. Shortages of medical staff, inadequate monitoring, interruptions of supply chains, shortages of personal protective equipment, and social distancing restrictions have led to a reduction in the ability for clinical trials to continue. Asaad and colleagues recently estimated that between March 1 and April 26, 2020, a total of 1052 clinical trials were suspended, with at least 905 reporting the COVID-19 pandemic as the primary reason [24]. While the resumption of clinical trials is inevitable, the impact that the pandemic’s interruption of clinical trials will have on pre-existing disparities in enrollment remains unknown.
Unintended Consequences of Treatment Delays
The COVID-19 pandemic presented extraordinary challenges for breast cancer patients and providers alike. To both conserve hospital resources such as personal protective equipment and ventilators and promote social distancing, non-emergency surgery was postponed in many regions, especially in the Northeast. Recommendations for the management of breast cancer patients were provided by the Society of Surgical Oncology and the American Society of Breast Surgeons [25, 26]. These measures included treating patients with estrogen receptor–positive ductal carcinoma in situ (DCIS) or stage I–III tumors with neoadjuvant endocrine therapy with monthly monitoring for progression, prioritization of surgery for patients with small triple-negative breast cancer (TNBC) or HER2 + tumors, and urgent surgery for malignant phyllodes tumors, angiosarcoma, and for patients with progression of disease on systemic therapy. These recommendations were made with the caveat that each case be discussed by the institutional multidisciplinary tumor board and must account for whether surgery was even deemed safe by the healthcare system at the time [25]. The American College of Surgeons also echoed these guidelines and suggested that breast surgery cases should only be performed if survivorship would be compromised if surgery was delayed [27].
Prior to COVID-19, several studies have documented disparities in time to treatment for breast cancer. Analyses of large national datasets have consistently found that Black women receive treatment later than their White counterparts, including surgery [28–33]. While a pause in the surgical management of breast cancer was necessary given the challenges faced by the healthcare system, these guidelines may inadvertently worsen disparities in time to surgery for black breast cancer patients [34•]. Data are sparce regarding the impact that surgical delays have had on breast cancer patients, particularly regarding disparities. An early study of breast medical oncology patients treated at a New York City academic medical center found that patients who self-identified as Black or African American, Asian, or other races were more likely to experience a delay and/or change in their treatment compared to White patients. Additionally, multivariate analysis demonstrated that Medicaid compared to commercial insurance was associated with increased odds of a delay [35•].
While expert guidelines were put in place to standardize the treatment of breast cancer patients diagnosed during the COVID-19 pandemic, providers were cautioned to factor in their own healthcare system’s trends in infection rates and capacity for non-emergent cases. This created unintended consequences because even among New York City, drastic differences were seen within each of the five boroughs in the ability to divert resources. For example, consider two New York City public hospitals: Bellevue Hospital in Manhattan and Elmhurst Hospital in Queens. While both hospitals treat a large proportion of medically underserved and vulnerable patients, they had drastically different surge capacities which impacted the ability to offer breast cancer surgery. As a result, while Bellevue was able to continue to provide essential breast surgery, the breast service at Elmhurst was completely shut down due to the overwhelming impact of COVID-19 in the community [36•].
While these studies provide a glimpse of the potential impact that the COVID-19 pandemic has had, more research is warranted. Future work should aim to characterize the diagnosis and treatment of breast cancer patients during this time and analyze treatment intervals, including dates of abnormal imaging, biopsy, and first treatment and the association with race, insurance status, and other social determinants of health. It is essential to collect data regarding patient and institutional reasons for treatment delays. We must learn from this experience so that when faced with another healthcare crisis, targeted interventions can be designed for patient subsets that may be most at risk.
Call to Action
The COVID-19 pandemic has illuminated the urgency to address health care disparities within our nation. We propose several mechanisms for achieving this goal within breast oncology (Fig. 1). First, more research is needed to fully evaluate the toll that the COVID-19 pandemic has had on breast health disparities. While this is likely to involve longitudinal studies spanning the next decade, there is a paucity of data that examines race-specific outcomes and delays as well as preventable morbidity and mortality. Additionally, while some studies have begun to evaluate the psychosocial impact that the pandemic has had on breast cancer patients, more work is needed to examine how social injustices relate to breast disparities [37].
Fig. 1.
Strategies to mitigate breast cancer disparities in the COVID-19 era
Increased support for community outreach initiatives and novel approaches to engagement are needed to provide education for both patients and providers alike. For patients, it is essential that we educate on the importance and safety of resuming cancer screening and other routine preventative care. For providers, more opportunities to learn about breast health disparities can be provided through free continuing medical education (CME) courses. For example, at our institution, we converged a group of breast disparities experts from across the country to educate both patients and healthcare providers in a series of lectures delivered virtually to improve access, safety, and convenience. Topics included genetic mechanisms for breast cancer disparities, current breast cancer epidemiology, recent innovations in breast cancer research, mammography screening in minority populations, mechanisms for community engagement, and case studies for discussion. Additionally, barriers to screening mammography should be considered for patient populations and strategies implemented. For example, consider expanding mammography screening hours to evening and weekends to improve access for patients that may work during the day and/or have other responsibilities. Depending on current COVID-19 pandemic waves and local ease on restrictions, mammography screening vans may also be a useful tool. Finally, education and collaboration with respected community organizations, churches, and minority social networks are additional strategies that can be implemented to improve screening.
Since the start of the pandemic through multiple waves, there continues to be unprecedented strain on the healthcare system. Despite this, patient access and navigation programs need to be maintained and supported within health systems. Patient navigation programs are often the first to be lost among hospitals faced with financial instability, especially at safety-net hospitals. However, the importance of these staff members cannot be overstated, and they are likely more important to patient care now than ever. It is essential that these navigation programs are maintained and utilized appropriately, particularly in the face of a changing work force. In addition to access to navigation, digital services such as telemedicine and personal electronic medical record should also be available to patients. With the introduction of the electronic medical record, patients are given the opportunity to have more of a hands-on role in their care, thus empowering them. Additionally, many of the electronic health platforms facilitate the delivery of telemedicine and messaging services. However, access to broadband internet for Black and Hispanic patients lags behind their White counterparts [38]. Therefore, more work is needed to develop policies that specifically address these barriers and to determine best practices for delivering equitable telehealth services and communication with patients.
Lastly, there is an urgent need to continue to enroll racial and ethnic minorities in clinical trials. This cannot be done without providing robust patient education and trust-building within communities. This may be accomplished through consistent community outreach initiatives and activities, or even through social media that emphasize the safety and necessity of clinical trial enrollment. For example, at our institution, in addition to having physicians go out into the community to engage with patients and give educational seminars, we also have created a virtual channel containing short cartoon videos highlighting key breast health messages.
Conclusions
In summary, the COVID-19 pandemic has had a significant impact on every element of the delivery of comprehensive breast cancer care and has highlighted pre-existing disparities and the need for more robust mitigation strategies. While the true toll of the pandemic continues to evolve, we must learn from the unprecedented strain placed on the healthcare system during the last 2 years as we continue to pave the road to breast health equity.
Acknowledgements
We acknowledge the expertise and support of the librarians of the Weill Cornell Medicine Samuel J. Wood Library.
Declarations
Conflict of Interest
Vivian J. Bea declares grants from the American Cancer Society and Pfizer outside the submitted work. Genevieve A. Fasano and Solange Bayard declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Breast Cancer Disparities.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 2.United States Census Bureau. Income and poverty in the United States: 2020. https://www.census.gov/library/publications/2021/demo/p60-273.html; Accessed Jan 31, 2022.
- 3.United States Census Bureau. Health Insurance Coverage in the United States: 2019. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p60-271.pdf; Accessed Jan 31, 2022.
- 4.American Cancer Society. Breast cancer facts & figures 2019–2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf; Accessed Jan 31, 2022.
- 5.Ahmed AT, Welch BT, Brinjikji W, Farah WH, Henrichsen TL, Murad MH, et al. Racial disparities in screening mammography in the United States: a systematic review and meta-analysis. J Am Coll Radiol. 2017;14:157–165.e9. doi: 10.1016/j.jacr.2016.07.034. [DOI] [PubMed] [Google Scholar]
- 6.Churpek JE, Walsh T, Zheng Y, Moton Z, Thornton AM, Lee MK, et al. Inherited predisposition to breast cancer among African American women. Breast Cancer Res Treat. 2015;149:31–39. doi: 10.1007/s10549-014-3195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Behrendt CE, Hurria A, Tumyan L, Niland JC, Mortimer JE. Socioeconomic and clinical factors are key to uncovering disparity in accrual onto therapeutic trials for breast cancer. J Natl Compr Canc Netw. 2014;12:1579–1585. doi: 10.6004/jnccn.2014.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ajewole VB, Akindele O, Abajue U, Ndulue O, Marshall JJ, Mossi YT. Cancer disparities and Black American representation in clinical trials leading to the approval of oral chemotherapy drugs in the United States between 2009 and 2019. JCO Oncol Pract. 2021;17:e623–e628. doi: 10.1200/OP.20.01108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.•• Newman LA, Winn RA, Carethers JM. Similarities in risk for COVID-19 and cancer disparities. Clin Cancer Res 2021;27:24–7. 10.1158/1078-0432.CCR-20-3421. Newman and colleagues provide a thorough overview of the similarities in risk for both COVID-19 and cancer that has led to a disproportionate impact on racial and ethnic minorities. Driven by not only genetic predisposition but also socioeconomic factors, racial and ethnic minority populations face an increased burden of acquiring and dying from both diseases. Additionally, in both scenarios, these populations are underrepresented in clinical trials which may lead to long-term disparities. This paper provides suggestions for collaborative strategies for addressing the root cause of these disparities. [DOI] [PMC free article] [PubMed]
- 10.Kaiser Family Foundation. COVID-19 cases and deaths by race/ethnicity: current data and changes over time. https://www.kff.org/racial-equity-and-health-policy/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/; Accessed Jan 31, 2022.
- 11.Newman L, Fejerman L, Pal T, Mema E, McGinty G, Cheng A, et al. Breast cancer through the lens of the COVID-19 pandemic. Curr Breast Cancer Rep. 2021;6:1–3. doi: 10.1007/s12609-021-00419-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavallo, J. How delays in screening and early cancer diagnosis amid the COVID-19 pandemic may result in increased cancer mortality. https://ascopost.com/issues/september-10-2020/how-delays-in-screening-and-early-cancer-diagnosis-amid-the-covid-19-pandemic-may-result-in-increased-cancer-mortality/; Accessed Feb 23, 2022.
- 13.Balogun OD, Bea VJ, Phillips E. Disparities in cancer outcomes due to COVID-19-a tale of 2 cities. JAMA Oncol. 2020;6:1531–1532. doi: 10.1001/jamaoncol.2020.3327. [DOI] [PubMed] [Google Scholar]
- 14.Carethers JM, Sengupta R, Blakey R, Ribas A, D'Souza G. Disparities in cancer prevention in the COVID-19 era. Cancer Prev Res (Phila) 2020;13:893–896. doi: 10.1158/1940-6207.CAPR-20-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amram O, Robison J, Amiri S, Pflugeisen B, Roll J, Monsivais P. Socioeconomic and racial inequities in breast cancer screening during the COVID-19 pandemic in Washington state. JAMA Netw Open. 2021;4:e2110946. doi: 10.1001/jamanetworkopen.2021.10946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Velazquez AI, Hayward JH, Gregory B, Dixit N. Trends in breast cancer screening in a safety-net hospital during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2119929. doi: 10.1001/jamanetworkopen.2021.19929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeGroff A, Miller J, Sharma K, Sun J, Helsel W, Kammerer W, et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January-June 2020, in the United States. Prev Med. 2021;151:106559. doi: 10.1016/j.ypmed.2021.106559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.•• Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021:7:878–884. 10.1001/jamaoncol.2021.0884. This large retrospective study quantifies the decrease in screening rates that occurred for breast, colorectal, and prostate cancer due to the COVID-19 pandemic in different geographic regions within the USA. While screening for breast, colorectal, and prostate cancers declined from March through May of 2020, the sharpest decline was observed for breast during April 2020 where the screening rate decreased by 90.8%. Additionally, geographic variation was observed such that the Northeast experienced the largest decline in screening. Importantly, when stratified by socioeconomic status, the largest screening decline was seen for patients within the largest socioeconomic index quartile suggesting that not all patient populations were affected equally. [DOI] [PMC free article] [PubMed]
- 20.Li S, O'Brien S, Murphy C, Nabil C. Identifying patients at risk of delayed breast imaging due to the COVID-19 pandemic. Cureus. 2021;13:e17235. doi: 10.7759/cureus.17235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller MM, Meneveau MO, Rochman CM, Schroen AT, Lattimore CM, Gaspard PA, et al. Impact of the COVID-19 pandemic on breast cancer screening volumes and patient screening behaviors. Breast Cancer Res Treat. 2021;189:237–246. doi: 10.1007/s10549-021-06252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newman LA, Roff NK, Weinberg AD. Cancer clinical trials accrual: missed opportunities to address disparities and missed opportunities to improve outcomes for all. Ann Surg Oncol. 2008;15:1818–1819. doi: 10.1245/s10434-008-9869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheppard VB, Hurtado-de-Mendoza A, Talley CH, Zhang Y, Cabling ML, Makambi KH. Reducing racial disparities in breast cancer survivors’ ratings of quality cancer care: the enduring impact of trust. J Healthc Qual. 2016;38:143–163. doi: 10.1097/JHQ’.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 24.Asaad M, Habibullah NK, Butler CE. The impact of COVID-19 on clinical trials. Ann Surg. 2020;272:e222–e223. doi: 10.1097/SLA.0000000000004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bartlett DL, Howe JR, Chang G, Crago A, Hogg M, Karakousis G, et al. Management of cancer surgery cases during the COVID-19 pandemic: considerations. Ann Surg Oncol. 2020;27:1717–1720. doi: 10.1245/s10434-020-08461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The American Society of Breast Surgeons. ASBrS resource guide to endocrine therapy in the COVID-19 pandemic. https://www.breastsurgeons.org/docs/statements/ASBrS-Resource-Guide-on-Endocrine-Therapy-in-the-COVID-19-Pandemic.pdf?v1; Accessed Jan 31, 2022.
- 27.American College of Surgeons. COVID-19: elective case triage guidelines for surgical care. https://www.facs.org/covid-19/clinical-guidance/elective-case; Accessed Jan 31, 2022.
- 28.Bachand J, Soulos PR, Herrin J, Pollack CE, Xu X, Ma X, et al. Physician peer group characteristics and timeliness of breast cancer surgery. Breast Cancer Res Treat. 2018;170:657–665. doi: 10.1007/s10549-018-4789-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benefield HC, Reeder-Hayes KE, Nichols HB, Calhoun BC, Love MI, Kirk EL, et al. Outcomes of hormone-receptor positive, HER2-negative breast cancers by race and tumor biological features. JNCI Cancer Spectr. 2020:5:pkaa072. 10.1093/jncics/pkaa072. [DOI] [PMC free article] [PubMed]
- 30.Doe S, Petersen S, Buekers T, Swain M. Does a multidisciplinary approach to invasive breast cancer care improve time to treatment and patient compliance? J Natl Med Assoc. 2020;112:268–274. doi: 10.1016/j.jnma.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emerson MA, Golightly YM, Aiello AE, Reeder-Hayes KE, Tan X, Maduekwe U, et al. Breast cancer treatment delays by socioeconomic and health care access latent classes in Black and White women. Cancer. 2020;126:4957–4966. doi: 10.1002/cncr.33121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoppe EJ, Hussain LR, Grannan KJ, Dunki-Jacobs EM, Lee DY, Wexelman BA. Racial disparities in breast cancer persist despite early detection: analysis of treatment of stage 1 breast cancer and effect of insurance status on disparities. Breast Cancer Res Treat. 2019;173:597–602. doi: 10.1007/s10549-018-5036-z. [DOI] [PubMed] [Google Scholar]
- 33.Jackson DK, Li Y, Eskander MF, Tsung A, Oppong BA, Bhattacharyya O, et al. Racial disparities in low-value surgical care and time to surgery in high-volume hospitals. J Surg Oncol. 2021;123:676–686. doi: 10.1002/jso.26320. [DOI] [PubMed] [Google Scholar]
- 34.• Obeng-Gyasi S, Oppong B, Paskett ED, Lustberg M. Purposeful surgical delay and the coronavirus pandemic: how will black breast cancer patients fare? Breast Cancer Res Treat. 2020:182:527–530. 10.1007/s10549-020-05740-0. An important editorial that examines the possible implications of the pandemic-related surgical delays on black breast cancer patients and directions for future study to further elucidate the impact. [DOI] [PMC free article] [PubMed]
- 35.• Satish T, Raghunathan R, Prigoff JG, Wright JD, Hillyer GA, et al. Care delivery impact of the COVID-19 pandemic on breast cancer care. JCO Oncol Pract. 2021:17:e1215-e1224. 10.1200/OP.20.01062. As one of the first studies to examine how breast cancer care in the USA was affected by the COVID-19 pandemic, this study found that among breast oncology patients, patients who identified as Black/African American, Asian, or other races were more likely to experience a delay or change in their treatment compared to Whites; additionally, they found that Medicaid compared with commercial insurance was associated with increased odds of a delay and/or change. [DOI] [PubMed]
- 36.• Escobar N, Crown A, Pocock B, Joseph K. The devastating impact of the COVID-19 pandemic on breast cancer care among medically underserved populations at two New York City public hospitals. Annals of Surgery 2020:2:1–6. 10.1097/AS9.0000000000000018. An important real-world account of the impact that the COVID-19 pandemic has had on two New York City hospitals that resulted in vastly different experiences among similar patient populations. This paper highlights how the breast services at Bellevue Hospital and Elmhurst Hospital reallocated hospital resources to care for medically underserved breast cancer patients. The experience of these two hospitals shows how COVID-19 has contributed to the widening of health care disparities.
- 37.Rentscher KE, Zhou X, Small BJ, Cohen HJ, Dilawari AA, Patel SK, et al. Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer. 2021;127:3671–3679. doi: 10.1002/cncr.33687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pew Research Center. Internet/Broadband Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/internet-broadband/?menuItem=3109350c-8dba-4b7f-ad52-a3e976ab8c8f; Accessed Feb 23, 2022.