Abstract
Objective
To understand the impact of the coronavirus disease 2019 (COVID-19) pandemic on adolescents and young adults (AYAs), we adapted the COVID-19 Exposure and Family Impact Scales (CEFIS; Kazak et al., 2021) for AYAs. Here, we report on the development, structure, and psychometric properties of the CEFIS-AYA.
Methods
The CEFIS-AYA was developed by a multidisciplinary, multi-institutional team using a rapid iterative process. Data from 3,912 AYAs from 21 programs at 16 institutions across the United States were collected from May 2020 to April 2021. We examined the underlying structure of the CEFIS-AYA using principal component analysis (PCA), calculated internal consistencies, and explored differences in scores by gender and age.
Results
Participants reported exposure to a range of COVID-19-related events (M = 9.08 events, of 28). On the bidirectional 4-point Impact scale, mean item scores were mostly above the midpoint, indicating a slightly negative impact. Kuder–Richardson 20/Cronbach’s Alpha was good for Exposure (α = .76) and excellent for Impact (α = .93). PCA identified seven factors for Exposure (Severe COVID-19, Loss of Income, Limited Access to Essentials, COVID-19 Exposure, Disruptions to Activities, Disruptions to Living Conditions, and Designation as an Essential Worker) and five for Impact (Self and Family Relationships, Physical Well-Being, Emotional Well-Being, Social Well-Being, and Distress). Gender and age differences in CEFIS-AYA scores were identified.
Discussion
Initial reliability data are strong and support use of the CEFIS-AYA for measuring the effect of the COVID-19 pandemic on AYAs in research and clinical care.
Keywords: adolescents, COVID-19, families, pediatric, trauma, young adults
Introduction
Since March 2020, coronavirus disease 2019 (COVID-19) has been pervasive, with a sustained and often dramatic impact on health and wellbeing (Pater, 2021). Despite availability of vaccines in the United States, challenges in implementing wide-spread mitigation strategies, such as vaccine hesitancy, and numerous mutations in the virus contribute to the persistent and widespread threat of COVID-19 (Pater, 2021; Walensky et al., 2021). Mitigation strategies to combat the virus (e.g., lockdown, quarantine for infected or exposed individuals, mask mandates), and the experience of having COVID-19 for some, have significantly altered daily life and resulted in lasting physical and emotional effects.
Growing evidence documents the broad and profound impact of COVID-19 on adolescents and young adults (AYAs; Branje & Morris, 2021; Listernick & Badawy, 2021; Samji et al., 2021). Developmental tasks (e.g., developing autonomy, socializing away from home, forming close relationships, engaging in school, work, and sports) have been impeded by COVID-19, and mental health and lifestyle behaviors have been disrupted (Chaffee et al., 2021; Chaturvedi et al., 2021; Kujawa et al., 2020; Socarras et al., 2021; Wilson et al., 2021). Evidence also highlights the importance of examining pre-existing health conditions as a factor in COVID-19 adjustment (Alonzi et al., 2020). The pandemic has exposed and exacerbated health disparities (Gupta & Jawanda, 2020), with identified impacts based on age (Listernick & Badawy, 2021) and gender (Kamal et al., 2021).
A traumatic stress framework is well supported and helpful clinically in understanding the reactions of patients of all ages, and their family members, to potentially traumatic illnesses and injuries (Price et al., 2016). The COVID-19 pandemic has many potentially traumatic aspects, including its unpredictability, persistence, and the potential losses associated with social isolation, economic constraints, and acute and chronic illness and death. While global in its scope, the extent of exposure to COVID-19-related events may vary across individuals.
Having a validated measure to capture the extent to which AYAs presenting to health care systems impacted by the pandemic is critical to providing optimal clinical care. A brief assessment of AYA’s experiences in the pandemic, based on a medical traumatic stress model (Price et al., 2016), may provide valuable information in terms of addressing strengths and vulnerabilities and considering the impact, over time, of their pandemic experiences on their health and healthcare. Additionally, the internal validity of research studies may be threatened if we cannot quantify the impact of COVID-19 on participants, changes in research procedures (e.g., data collection, delivery of interventions), and outcomes of ongoing studies (Mara & Peugh, 2020; Stiles-Shields et al., 2020).
To address these needs, we adapted the COVID-19 Exposure and Family Impact Scales (CEFIS; Kazak et al., 2021), a measure for caregivers of youth in pediatric healthcare settings, to assess exposure to and impact of COVID-19 for AYAs, via self-report. Based on a national sample of 1,805 U.S. families using the initial caregiver-report version of the CEFIS, three CEFIS scales (Exposure, Impact, Distress) were established (Kazak et al., 2021). In a subsequent study of 2,531 families scheduled for an outpatient visit at a children’s health system, confirmatory factor analysis validated the original factor structure (Enlow et al., 2022). Higher scores on CEFIS scales, indicating greater exposure, more negative impact, and more distress, were related to more mental health concerns, poorer family functioning, and clinically significant posttraumatic stress symptoms (Enlow et al., 2022).
This paper describes the development of the CEFIS-AYA, evaluates the structure of the scales and their psychometric properties, and explores differences in scores as a function of gender and age to provide a basis for the use of this measure in research and clinical care.
Methods
The CEFIS-AYA was adapted from the CEFIS, a caregiver-report measure developed by a multidisciplinary, multi-institutional team in March 2020, at the start of the pandemic (Kazak et al., 2021). Development of the CEFIS-AYA was completed in May 2020 and its availability was announced on listservs of relevant divisions of the American Psychological Association, specifically Division 54 (Society of Pediatric Psychology) and Division 38 (Society of Health Psychology) on May 18, 2020 and registered with the National Institutes of Health Disaster Information Management Research Center: https://tools.niehs.nih.gov/dr2/index.cfm/resource/22041
Sample
Data analyzed in this paper are from 3,912 AYAs, ages 15 through 29 years, who completed the CEFIS-AYA in English. Data were collected by 21 registered CEFIS-AYA users at 16 sites in 10 states across the nation representing the east (NY, PA, MA) and west (CA, WA) coasts, the mid-West (IL, MO, OH), and the south (GA, OK). Most users administered the CEFIS-AYA for research. One site used it clinically and one used it both clinically and in research. Three users reported data from multisite studies.
Most participants completing the CEFIS-AYA were female (N = 2,787, 71.2%); 1,061 (27.1%) were male, and 61 reported their gender as other (1.6%).1 The average age was 20.69 years (SD = 2.68) with 5.9% under 18 years, and 70.8% between 18 and 22 years. The medical diagnoses of participants were varied like the original CEFIS sample (Kazak et al., 2021) and included patients: (a) with oncological or hematological diagnoses or undergoing stem cell transplantation; (b) experiencing chronic pain; (c) experiencing other chronic pediatric conditions; and (d) seeking care in primary care settings (see Table I).
Table I.
Patient Populations Included in CEFIS-AYA Validation
| Patient group | Number of sites | Number of participants |
|---|---|---|
| Hematology/oncology/stem cell transplant | 4 | 260 |
| Community | 3 | 1,687 |
| Pain | 3 | 550 |
| Primary care | 2 | 491 |
| Diabetes | 2 | 41 |
| Irritable bowel syndrome | 2 | 11 |
| Students with chronic conditions | 1 | 492 |
| Spina bifida | 1 | 308 |
| Eating disorders | 1 | 57 |
| Genomic medicine | 1 | 13 |
| HIV | 1 | 2 |
Measure
The first author (L. A. S.) led the adaptation of the CEFIS-AYA with the original team that created the CEFIS along with two additional psychologists (A. M. P. and L. C.) and one exercise scientist (S. K.-D.) with expertise in pediatric populations. Our intent was to develop a parallel measure to the CEFIS, while expanding to include assessment of AYA-specific concerns. Like the CEFIS, the CEFIS-AYA includes domains consistent with a medical traumatic stress framework. The exposure domain captures AYAs’ experiences with a range of pandemic-related events. The impact domain assesses the perceived effect of pandemic-related events on functioning and distress.
The process of developing the CEFIS-AYA was iterative and began with a review of each of item on the caregiver-report CEFIS. Proposed modifications or removals of items and new items were discussed via email and teleconferences. Changes in the CEFIS-AYA (from the CEFIS) include items worded in the third person (e.g., we, our) were changed to first person (e.g., I, mine) and “not applicable” was added as a response option for certain items (e.g., related to attending school or having child/ren).
The CEFIS-AYA opens with a general introduction, similar to the CEFIS but with a broader definition of “family”—Please tell us about your family’s experiences during the novel Coronavirus (COVID-19) pandemic. In answering these questions, please think about what has happened from March 2020 to the present, due to COVID-19. By family we mean people who live in your household, family members who live outside your home, and close friends who you consider “like family.” Following the introduction, the CEFIS-AYA has three sections.
Part 1 (Exposure) consists of 28 items (Yes/No responses) that measure the participants’ “exposure” to COVID-19 and related events (e.g., stay at home orders, changes in housing, difficulty meeting family needs, missing family events, etc.). A cascading set of items asked about someone in the family: (a) being exposed to someone with COVID-19; (b) having symptoms/diagnosis of COVID-19; (c) trying but being unable to get tested for COVID-19; (d) being hospitalized; (e) being admitted to an intensive care unit; and (f) dying from COVID-19. Examples of new items include difficulty getting a COVID test, missing important milestones (e.g., proms, graduations, weddings), cutting back hours at work, and losing health insurance/benefits. Higher scores indicate greater exposure to COVID-19-related events.
Part 2 (Impact) consists of 16 items that measure the impact of COVID-19 on family, emotional, and physical wellbeing. Fifteen items use a 4-point Likert scale rating (1 = Made it a lot better; 2 = Made it a little better; 3 = Made it a little worse; 4 = Made it a lot worse) and a Not Applicable option. A single distress item, scored separately from the other Impact items, uses a 1–10-point Likert-type scale. New items assess COVID-19’s impact on AYA ability to be independent, sedentary behavior, substance use, loneliness, relationship with friends, and romantic relationships. Higher scores denote more negative impact/more distress.
Part 3 is an open-ended question, Please tell us about other effects of COVID-19 on you and your family, both negative and/or positive.2
Procedure
Data collection was from May 2020 to April 2021. The study protocol was reviewed by the Nemours Institutional Review Board and was determined not to meet the criteria for human subjects research (#161342). The CEFIS-AYA was distributed through the Center for Pediatric Traumatic Stress and is available free of charge in English and Spanish3 as a REDCap survey; registration is required. When they registered, users agreed to share de-identified data monthly, facilitated by a REDCap data dictionary, to allow for assessing the psychometric properties of the measure. Users specified a priori what patient groups would complete the CEFIS-AYA. Sites using the measure in research also confirmed they had IRB-approved protocols. Age and gender (male, female, other) were the only demographic data provided to us by users.4
Data Analysis
Data analysis followed the same procedures as that of the CEFIS validation (Kazak et al., 2021). The distribution of responses and missing data for each CEFIS-AYA item was first examined using descriptive statistics and graphs. Principal component analysis (PCA) with varimax rotation with Kaiser Normalization was conducted to determine the underlying structure and characterize the content of the CEFIS-AYA scales. Because the CEFIS-AYA was developed with two distinct theoretical domains (Exposure, Impact), and to be consistent with the medical traumatic stress model and the caregiver CEFIS, PCA was conducted for each domain separately. For the Exposure PCA, NA responses were coded as No. For the Impact PCA, responses on the single distress scale item were converted from a 10 to a 4-point scale (1–2 = 1; 3–5 = 2; 6–8 = 3; 9–10 = 4) for consistency across items. NA responses were considered missing. In each PCA, to determine the number of Principal Components (PCs) to extract, a PCA was first conducted without rotation. The resulting scree plot was examined to determine the number of PCs to test in subsequent solutions using varimax rotation. Rotation was necessary as many of the unrotated PCs had intermediate coefficient values that made their interpretation difficult. Rotation facilitated interpretation as it drove the component coefficients to high or low values. The PCs and the total variance explained were the same before and after rotation. The interpretability of PCs and percentage of variance explained by the solution were considered in deciding upon the final components retained (Tabachnick & Fidell, 2019).
The internal consistency of the Exposure and Impact scales was calculated using Cronbach’s Alpha/Kuder–Richardson Formula 20 and item-total correlations were examined. Analysis of Variances (ANOVAs) were used to explore differences across health conditions, for those conditions in which the sample size exceeded 100 and data were contributed from two or more sites (Table I). ANOVAs were also conducted to explore gender (male, female, other) and age differences (15–17, 18–22, 23–29) in CEFIS-AYA scores. Finally, Pearson Product Moment Correlations were calculated to establish the associations among Exposure, Impact, and Distress scores. SPSS v27 was used for all analyses.
Results
Item Distributions
Exposure
The percentage responding “Yes” to each Exposure item is presented in Figure 1. Of those for whom it was applicable, 89.7% reported that their education was disrupted. Over half reported disruptions in their lives such as missing important family events (56.1%) or someone having to cut back work hours (56.3%). A substantial proportion of AYAs reported direct experience with COVID-19 within their families: exposure to someone with COVID-19 (41.0%) or symptoms/diagnosis (28.0%), with far fewer reporting hospitalization (7.4%), ICU admission (4.9%), or death (5.0%). Overall, missing data were minimal for the Exposure items (<1%). The questions regarding employment and school did not apply for 7.7% and 13.4%, respectively.
Figure 1.
Endorsement of CEFIS-AYA exposure items.
Note. Reported percentages were calculated based on those responding yes or no.
Impact
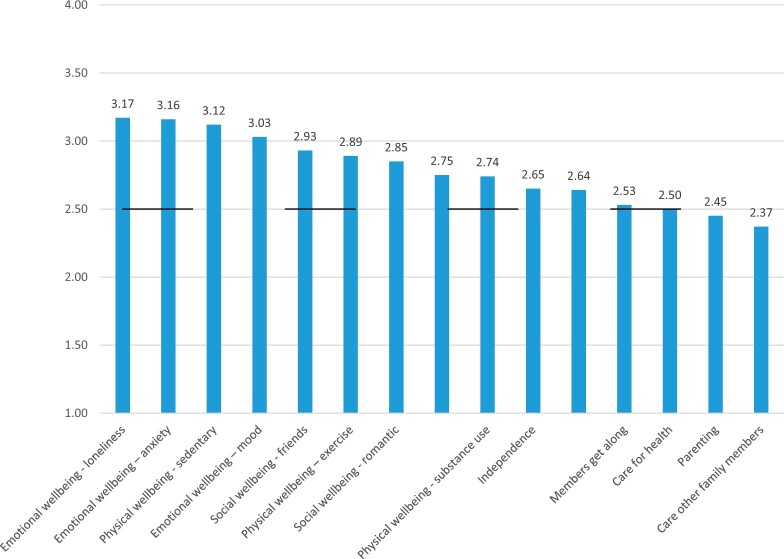
Responses to the Impact items utilized the full range of the 4-point scale (Figure 2). The rate of NA responses or missing data was generally within acceptable ranges (6.7–18.5%). However, four items had more missing or NA data: “Parenting your children” (80.7% missing/NA); “substance use” (52.9%), “ability to care for others in your family” (27.6%), and “romantic relationships” (26.0%). The means for most items on the Impact scale were slightly above the midpoint, indicating a mildly negative impact of the pandemic. The impact was rated highest (most negative) on loneliness (M = 3.17, SD = 0.86), anxiety (M = 3.16, SD = 0.86), and sedentary behavior (M = 3.12, SD = 0.92). The sample mean for COVID-19’s impact on caring for other family members tipped slightly positive (M = 2.37, SD = 0.87).
Figure 2.
Endorsement (mean values) of CEFIS-AYA impact items.
Note. Participants responded on a 4-point scale: 1 = Made it a lot better; 2 = Made it a little better; 3 = Made it a little worse; 4 = Made it a lot worse. Higher scores indicate more negative impact. The range for all items is 1–4. The midpoint of the scale (marked above) is 2.5.
Internal Reliability and Structure of the CEFIS-AYA
Exposure
Cronbach’s Alpha/KR20 for the Exposure scale with all items was very good (α = .76) and was not improved by dropping items. The final component structure for the Exposure items converged in seven rotations (Table II). Seven factors were identified among the 28 items, accounting for 50.3% of the variance. Two items had low coefficients (< 0.4) across all factors: losing benefits and unable to get tested for COVID-19. The resulting factors were: (a) Severe COVID-19 (3 items, α = .80); direct experiences with COVID-19—hospitalization, ICU admission, and death—in any family member; (b) Loss in income (4 items; α = .67); a decrease in income, cutting back work hours, furlough, or job loss in either the respondent or a family member; (c) Limited access to essentials (4 items; α = .58); difficulty in obtaining food, medicine, healthcare, or other essentials; (d) COVID-19 exposure (4 items; α = .59); exposure to the virus, experiencing symptoms or being diagnosed, quarantine due to exposure or travel, and being unable to visit family or friends; (e) Disruptions to activities (5 items; α = .56); stay at home order, school closure, education disruption, and missing a milestone or important family event; (f) Disruptions to living conditions (4 items; α = .46); living separately, someone moving in or out of the home, and caring for a family member; and (g) Designation as an essential worker (2 items; α = .43); having a family member who kept working outside the home or was a healthcare provider or first responder providing direct patient care.
Table II.
CEFIS-AYA Exposure Items and Rotated Component Structure
| Exposure items (scale α = .76) | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| I had a “stay at home” order | –0.015 | 0.092 | –0.015 | 0.174 | 0.408 | 0.105 | –0.115 |
| My school physically closed | 0.034 | 0.043 | –0.103 | –0.172 | 0.748 | 0.146 | –0.033 |
| My education was disrupted | –0.002 | 0.069 | –0.128 | 0.027 | 0.767 | 0.015 | 0.060 |
| I missed an important milestone event that was canceled or postponed | 0.056 | –0.015 | 0.181 | 0.203 | 0.502 | –0.049 | 0.132 |
| I missed an important family event, or it was canceled | 0.009 | 0.053 | 0.226 | 0.354 | 0.416 | –0.115 | 0.094 |
| I had to start caring for a family member | 0.136 | 0.058 | 0.175 | –0.040 | 0.072 | 0.544 | 0.095 |
| People in our family lived separately for health, safety, or job demands | –0.014 | 0.054 | 0.100 | 0.207 | 0.032 | 0.580 | 0.042 |
| Someone moved into our home | 0.110 | 0.016 | 0.122 | 0.014 | 0.005 | 0.585 | 0.053 |
| I had to move | –0.037 | 0.124 | 0.016 | 0.132 | 0.063 | 0.522 | –0.045 |
| Someone in family kept working outside the home (essential personnel) | –0.024 | 0.110 | –0.003 | 0.148 | 0.016 | –0.069 | 0.768 |
| Someone in family/household is a healthcare provider/first responder | 0.085 | –0.010 | –0.011 | 0.019 | 0.038 | 0.225 | 0.765 |
| I/we had difficulty getting food | 0.112 | 0.118 | 0.682 | –0.055 | –0.084 | 0.206 | –0.009 |
| I/we had difficulty getting medicine | 0.097 | 0.061 | 0.722 | –0.033 | –0.010 | 0.197 | –0.016 |
| I/we had difficulty getting health care when we needed it | 0.059 | 0.100 | 0.678 | –0.009 | 0.018 | 0.205 | 0.020 |
| I/we had difficulty getting other essentials | –0.080 | 0.092 | 0.481 | 0.272 | 0.082 | –0.196 | –0.014 |
| My/our income decreased | –0.023 | 0.687 | 0.178 | 0.065 | 0.093 | 0.014 | 0.001 |
| I/family member had to cut back hours at work | 0.013 | 0.769 | 0.078 | 0.089 | 0.123 | 0.025 | 0.077 |
| I/family member was required to stop working (expect to be called back) | 0.074 | 0.761 | –0.015 | 0.047 | 0.093 | 0.067 | 0.034 |
| I/family member lost my job permanently | 0.128 | 0.509 | 0.113 | –0.013 | –0.118 | 0.245 | –0.002 |
| I was unable to visit or care for a family member | –0.042 | 0.045 | 0.186 | 0.433 | 0.296 | 0.138 | 0.028 |
| I/we self-quarantined due to travel or possible exposure | –0.021 | 0.083 | –0.040 | 0.567 | 0.116 | 0.278 | –0.083 |
| Someone in the family was exposed to someone with COVID-19 | 0.183 | 0.042 | –0.025 | 0.738 | 0.033 | 0.041 | 0.178 |
| Someone in the family had symptoms or was diagnosed with COVID-19 | 0.335 | 0.041 | –0.047 | 0.675 | –0.015 | 0.068 | 0.092 |
| Someone in the family was hospitalized for COVID-19 | 0.842 | 0.060 | 0.048 | 0.136 | 0.007 | 0.117 | 0.029 |
| Someone in the family was in the Intensive Care Unit (ICU) for COVID-19 | 0.867 | 0.054 | 0.056 | 0.095 | 0.018 | 0.060 | 0.008 |
| Someone in the family died from COVID-19 | 0.756 | 0.049 | 0.091 | 0.069 | 0.030 | 0.021 | 0.024 |
| Eigenvalue | 3.83 | 2.08 | 2.01 | 1.47 | 1.36 | 1.24 | 1.1 |
| Percent variance accounted for | 14.73 | 8.01 | 7.74 | 5.64 | 5.23 | 4.75 | 4.24 |
| Mean | 0.06 | 0.39 | 0.19 | 0.43 | 0.64 | 0.18 | 0.41 |
| Standard deviation | 0.20 | 0.33 | 0.25 | 0.32 | 0.28 | 0.23 | 0.36 |
Note. Factor 1: Severe COVID-19 (α = .80); Factor 2: Loss of income (α = .67); Factor 3: Access to essentials (α = .58); Factor 4: Exposure to COVID-19 exposure (α = .59); Factor 5: Disruption to activities (α = .56); Factor 6: Disruptions to living conditions (α = .46); Factor 7: Designation as an essential worker (α = .43). COVID-19 = coronavirus disease 2019. Items with loadings greater than or equal to .40 are bolded.
Impact
Cronbach’s Alpha for the Impact scale with all items was excellent (α = .93) and was not improved by dropping items. The final component structure converged after six rotations (Table III) and accounted for 71.8% of the variance. The factors are: (a) Family and self-care (4 items; α = .78); the impact of COVID-19 on the family/household’s ability to get along, the AYA’s ability to care for their health, be independent, and care for others in their family/household; (b) Physical wellbeing (4 items; α = .80); sedentary behavior, exercise, eating, and sleeping; (c) Emotional wellbeing (3 items; α = .85); anxiety, mood, and loneliness; (d) Social wellbeing (2 items; α = .60); friend and romantic relationships; and (e) Distress (1 item); the AYA’s distress level. Items regarding parenting and substance use did not contribute to any of these five factors (coefficients < 0.40). Two items cross-loaded: sedentary behavior had a secondary loading with emotional wellbeing, and loneliness with social wellbeing.
Table III.
CEFIS-AYA Impact Items and Rotated Component Structure
| Impact items (scale α = .93) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| How family/household members get along | 0.705 | 0.120 | 0.206 | 0.115 | 0.087 |
| Ability to care for your health | 0.748 | 0.282 | 0.140 | 0.116 | 0.065 |
| Ability to be independent | 0.683 | 0.205 | 0.202 | 0.212 | −0.070 |
| Ability to care for others in your family | 0.806 | 0.151 | 0.061 | 0.046 | 0.142 |
| Your physical wellbeing—sedentary behavior | 0.260 | 0.608 | 0.446 | 0.116 | −0.136 |
| Your physical wellbeing—exercise/physical activity | 0.250 | 0.741 | 0.251 | 0.117 | −0.021 |
| Your physical wellbeing—eating | 0.244 | 0.801 | 0.170 | 0.166 | 0.091 |
| Your physical wellbeing—sleeping | 0.134 | 0.705 | 0.144 | 0.134 | 0.301 |
| Your emotional wellbeing—anxiety/worry | 0.188 | 0.273 | 0.816 | 0.137 | 0.168 |
| Your emotional wellbeing—mood | 0.222 | 0.285 | 0.784 | 0.187 | 0.177 |
| Your emotional wellbeing—loneliness | 0.189 | 0.190 | 0.691 | 0.418 | 0.104 |
| Your social well-being—relationships with friends | 0.195 | 0.143 | 0.335 | 0.699 | 0.112 |
| Your social well-being—romantic relationships or dating | 0.140 | 0.179 | 0.135 | 0.859 | 0.035 |
| Distress thermometer (4-point scale) | 0.135 | 0.126 | 0.230 | 0.103 | 0.891 |
| Eigenvalue | 6.09 | 1.34 | 1.05 | 0.88 | 0.70 |
| Percent variance accounted for | 43.47 | 9.57 | 7.51 | 6.27 | 5.03 |
| Mean | 2.54 | 2.84 | 3.10 | 2.88 | 5.95 |
| Standard deviation | 0.71 | 0.76 | 0.76 | 0.81 | 2.19 |
Note. Factor 1: Family/self-care (α = .78); Factor 2: Physical wellbeing (α = .80); Factor 3: Emotional wellbeing (α = .85); Factor 4: Social wellbeing (α = .60); Factor 5: Distress (α = n/a). Items with loadings greater than or equal to .40 are bolded.
Inter-Correlations among Exposure, Impact, and Distress5
The association between Exposure and Impact was of low magnitude although statistically significant (r = 0.20, p < .0001). The single distress item was significantly correlated with both Exposure (r = 0.36, p < .0001) and Impact (r = 0.39, p < .0001).
Scoring the CEFIS-AYA
The total Exposure Score was calculated as a count of Yes responses. Scores range from 0 to 28 with higher scores indicating greater exposure.6 The mean Exposure Score in our sample calculated across all items was 9.08 (SD = 4.22, median = 9.00, range = 0–28). Use of the mean for the Impact items (without the Distress item) allows for quick interpretation of the value by examining scores in relation to the midpoint of the scale (positive valence if < 2.5; negative valence if > 2.5). The mean Impact Score with 15 items was 2.82 (SD = 0.60, median = 2.90). Based upon the component structure and response scale differences between the Impact items and the Distress item, a separate Distress Score should be used. The mean for AYA self-reported distress in our sample was 5.95 (SD = 2.19, median = 6, range = 1–10).
Differences Based on Health Condition
Scores on each of the CEFIS-AYA scales were compared across the four largest groups in the sample—a community sample, primary care, pain, and hematology/oncology/transplantation. ANOVAs revealed statistically significant differences among the samples for Exposure, F (3, 2,973) = 78.66, p < .001, Impact F (3, 2,421) = 7.09, p < .001, and Distress, F (3, 2,756) = 43.42, p < .001. As summarized in Table IV, the community sample consistently made the highest scores (most exposure and impact), and the hematology/oncology/transplant group was consistently among the lowest.
Table IV.
CEFIS-AYA Scores and Effect Sizes (ηp2) by Condition
| Community M | Primary care | Pain | Hem/Onc | ηp2 | ||
|---|---|---|---|---|---|---|
| (SD) | M (SD) | M (SD) | M (SD) | F | (95% CI) | |
| Exposure, M (SD) | 10.09 (4.30)a | 8.82 (3.59)b | 7.43 (4.05)c | 7.50 (3.10)c | 78.66*** | 0.074 |
| N = 1,685 | N = 482 | N = 550 | N = 260 | (0.056–0.091) | ||
| Impact, M (SD) | 2.92 (0.55)a | 2.57 (0.60)a | 2.81 (0.62)b | 2.57 (0.60)c | 21.79*** | 0.026 |
| N = 1,461 | N = 381 | N = 397 | N = 186 | (0.014–0.039) | ||
| Distress, M (SD) | 6.24 (1.98)a | 6.01 (2.28)a,b | 6.17 (2.32)b | 4.64 (2.41)c | 43.42*** | 0.045 |
| N = 1,674 | N = 480 | N = 347 | N = 259 | (0.031–0.060) |
p < .001.
Note. Within rows, groups with different superscripts were significantly different in post-hoc analyses using Least Significant Difference (LSD) tests.
Gender and Age Differences
There were significant gender differences for CEFIS-AYA Exposure, Impact, and Distress scores (Table V). In general, males reported significantly less COVID-19 Exposure, Impact, and Distress than both those that identified as female or other. Those that identified as female or other only differed in Impact (female < other). Regarding age differences, 18–22-year-olds reported greater Exposure and Impact than the younger and older AYA groups who scored similarly. Distress had a different pattern with younger AYAs reporting less distress than the two older groups (Table IV).
Table V.
CEFIS-AYA Scores and Effect Sizes (ηp2) by Gender and Age Groups
| Gender (M, SD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (N = 1,060) | Female (N = 2,786) | Other (N = 61) | F | ηp2 (95% CI) | |||||
| CEFIS AYA scale | |||||||||
| Exposure, M (SD) | 8.40 (4.46)a | 9.32 (4.09)b | 9.97 (4.58)b | 19.81*** | 0.010 (0.005–0.017) | ||||
| Impact, M (SD) | 2.69 (0.60)a | 2.86 (0.58)b | 3.27 (0.41)c | 39.63*** | 0.024 (0.014–0.035) | ||||
| Distress, M (SD) | 5.32 (2.38)a | 6.19 (2.06)b | 6.45 (2.21)b | 61.94*** | 0.033 (0.022–0.044) | ||||
| Age groups in years (M, SD) | |||||||||
| 15–17 (N = 233) | 18–22 (N = 2,766) | 23–29 (N = 911) | F | ηp2 (95% CI) | |||||
| CEFIS AYA Scale | |||||||||
| Exposure, M (SD) | 7.49 (3.11)a | 9.38 (3.88)b | 8.57 (5.23)a | 30.31*** | 0.015 (0.008–0.023) | ||||
| Impact, M (SD) | 2.62 (0.56)a | 2.86 (0.59)b | 2.77 (0.61)a | 17.06*** | 0.011 (0.004–0.018) | ||||
| Distress, M (SD) | 4.90 (2.44)a | 6.01 (2.13)b | 6.08 (2.21)b | 29.68*** | 0.016 (0.009–0.024) | ||||
p < .001.
Note. Within rows, groups with different superscripts were significantly different in post-hoc analyses using Least Significant Difference (LSD) tests.
Discussion
Understanding the exposure of AYAs to COVID-19-related events and how they appraise the impact of those events is critical for understanding short and long-term effects of COVID-19, providing supportive and sensitive healthcare, and addressing possible confounders and threats to internal validity in studies. The impact of COVID-19 in studies where outcomes include psychosocial or behavioral factors is likely significant. Consistent with a medical traumatic stress model (Price et al., 2016), we modified the caregiver-report CEFIS to create the CEFIS-AYA in response to a need to quickly understand the impact of COVID on AYAs in healthcare settings and research. The CEFIS-AYA can be integrated into clinical care and research studies, as evidenced by already published studies using it (Feldman et al., 2021; Stiles-Shields et al., 2021).
The strengths of the CEFIS-AYA include the incorporation of both exposure and impact of COVID-19 as well as an appreciation of AYAs being embedded in the context of their families and broader social contexts. The CEFIS-AYA was adapted quickly from the Caregiver CEFIS and made available within 2 months of the March 2020 onset of the pandemic. We were able to amass a large sample and establish strong internal consistency of the scales. The national sample supports its generalizability in that it allowed for inclusion of participants from many states and regions that experienced different, and changing, mitigation directives.
Correlations among Exposure, Impact, and Distress scores demonstrate the importance of examining all three in clinical care. Distress was associated with both Exposure and Impact, supporting a trauma model. Females and individuals who identify as other reported greater exposure, impact, and distress than males, consistent with other young adult findings (Kamal et al., 2021; Stroud & Gutman, 2021). Those aged 18–22 years reported greater exposure and impact than younger or older AYAs. This is consistent with significant increases in depression and anxiety and lower levels of well-being and physical activity for this age range during the pandemic (Tasso et al., 2021; Wilson et al., 2021), and may also reflect the many transitions typically occurring during these years (e.g., employment, education, social relationships).
PCA supports the Exposure scale as a means of measuring the extent to which AYA have experienced potentially traumatic events related to COVID-19. Scores reflect a range of exposures, from those that are common (e.g., stay at home orders, schools closed) to those that impacted at least half the sample (e.g., decreased family income, missed events) and some that are less common (e.g., hospitalization, death). Of course, some of the uncommon exposures such as deaths are most likely to be traumatic. We used PCA to help characterize the content of the scales; we do not intend the components to be used as subscales.
The Impact scale assesses perceived COVID-19 influences on family relationships and AYA social, physical, and emotional well-being. This scale, including the newly added items for AYAs, was supported by a high internal consistency. In fact, the new items assessing loneliness, anxiety, and sedentary behavior were the most endorsed impact items, a finding consistent with other studies of the pandemic (Branje & Morris, 2021; Wilson et al., 2021). AYAs have continued to struggle with anxiety and deleterious impact of prolonged isolation and distance from peers and usual activities (Branje & Morris, 2021; Pagoto & Conroy, 2021). Given the chronicity and uncertain course of the pandemic, anticipating and appreciating its long-term effects on AYA mental health and development will continue to be important (Christakis, 2020; Hussong et al., 2021).
Although the means for most of the Impact items indicated negative consequences, the full range of response options was used for all items, and most were only slightly above the mid-point, a finding that may point toward adaptive coping with the effects of the pandemic. For example, there is evidence that sleep duration and quality has increased for some AYAs during the pandemic (Becker et al., 2021). Among the items rated most positively on the CEFIS-AYA were those related to caring for others in the family, although this had a low number of endorsements.
It will be important to validate the CEFIS-AYA, especially as the incidence and impact of COVID-19 changes. Convergent and criterion related validity will help establish its association with other measures and relevant outcomes, including those with clinical utility. A significant limitation of the CEFIS-AYA data in this report is the absence of demographic and disease-related characteristics of participants. In the context of the very early months of the pandemic when we were developing the CEFIS-AYA, we prioritized the rapid development and deployment of the measure. Collecting identifiable data would have resulted in delays, as sites would have needed to take additional time-consuming steps to transmit these data to the central site. It is also a limitation that the sample was 71% female. It is critical that subsequent papers using the CEFIS-AYA report on and examine the role of participant characteristics and demographics. This will allow for understanding the differential impact of COVID-19 based on race and ethnicity, age, sex, gender, geographic location, and education, and will help identify health disparities related to COVID-19 exposures and impact in this age group, as well as highlight areas of resilience.
In conclusion, the CEFIS-AYA has promising psychometrics (internal reliability and validation of its underlying structure) supporting its continued use and evaluation. Future research should examine the convergent and criterion validity of the CEFIS-AYA. In the meantime, there is substantial evidence to justify the use of the CEFIS-AYA for research and clinical care. It facilitates a brief measure of exposures and impact of COVID-19 that may impact physical and psychological well-being and access to care for AYA, and that may be addressed with help from multidisciplinary team members in healthcare settings.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Acknowledgments
We thank Glynnis A. McDonnell, PhD and Janet Deatrick, PhD for their feedback during the development process. We appreciate the helpful feedback provided by Darlene Barkman and Kerry Doyle-Shannon and thank the sites that contributed de-identified data for this project.
Funding
This research is supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (U54GM104941) and the State of Delaware to Anne Kazak, PhD. Additional support is provided by the Center for Pediatric Traumatic Stress (U79SM080048) and the Nemours Center for Healthcare Delivery Science.
Conflicts of interest: None declared.
Supplementary Material
Footnotes
Given the reporting of gender as male, female, or other, we cannot presume that those who marked “other” identify as nonbinary. We refer to the label as “other” throughout the paper to be consistent with the wording of the question.
These data are not reported in this paper.
CEFIS-AYA was translated into Spanish by a native Spanish-speaking member of the research team (GV) and certified as an accurate translation by an independent certified medical interpreter. Due to a lack of data at this point, the Spanish version is not reported in this paper.
The CEFIS-AYA was developed and distributed early in the COVID-19 pandemic. In order to collect data quickly and be responsive to the rapidly changing and uncertain global environment, we were not able to collect data on race, ethnicity, and other sociodemographic characteristics. To do so would have required protocols to allow transmittal of identifying information, approvals of IRBs at and implementation of data use agreements. The time necessitated by these steps would have prohibited developing and testing the scale quickly.
We examined changes in CEFIS-AYA scores over time (Supplemental Figure 1). There were no differences in Distress scores over the period of data collection; Exposure and Impact scores were significantly higher over the second 6 months of data collection but the increase in scores was small (Exposure: 1.2 points; Impact: 0.13 points).
Four items (cut back work hours, temporary or permanent job loss, and loss of benefits) were asked separately for the individual AYA and their family. Data were combined across self and family for scoring.
Contributor Information
Lisa A Schwartz, Children’s Hospital of Philadelphia, USA; Perelman School of Medicine, University of Pennsylvania, USA.
Amanda M Lewis, Nemours Children’s Health, USA.
Melissa A Alderfer, Nemours Children’s Health, USA; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Gabriela Vega, Nemours Children’s Health, USA.
Lamia P Barakat, Children ’s Hospital of Philadelphia, USA; Perelman School of Medicine, University of Pennsylvania, USA.
Sara King-Dowling, Children’s Hospital of Philadelphia, USA.
Alexandra M Psihogios, Children’s Hospital of Philadelphia , USA; Perelman School of Medicine, University of Pennsylvania, USA.
Kimberly S Canter, Nemours Children’s Health, USA; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Lori Crosby, Cincinnati Children’s Hospital Medical Center, USA.
Kamyar Arasteh, Nemours Children’s Health , USA.
Paul Enlow, Nemours Children’s Heal th, USA; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Aimee K Hildenbrand, Nemour s Children’s Health, USA; Sidney Kimmel Medical College , Thomas Jefferson University, USA.
Nancy Kassam-Adams, Children’s Hospital of Philadelphia, USA ; Perelman School of Medicine, University of Pennsylvania, USA.
Ahna Pai, Cincinnati Children’s Hospital Medical Center, USA.
Thao-Ly Phan, Nemours Children’s Health, USA; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Julia Price, Nemours Children’s Health, USA ; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Corinna L Schultz, Nemours Children’s Health, USA ; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Erica Sood, Nemour s Children’s Health, USA; Sidney Kimmel Medical College, Thomas Jefferson University, USA.
Jordan Wood, Children’s Hospital of Philadelphia, USA.
Anne Kazak, Nemours Ch ildren’s Health, USA; Sidney Kimmel Medical College, Thomas Jefferson University , USA.
References
- Alonzi S., La Torre A., Silverstein M. (2020). The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S236–S238. [DOI] [PubMed] [Google Scholar]
- Becker S. P., Dvorsky M. R., Breaux R., Cusick C. N., Taylor K. P., Langberg J. M. (2021). Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep, 44(8), zsab054. 10.1093/sleep/zsab054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branje S., Morris A. S. (2021). The impact of COVID-19 pandemic on adolescent emotional, social, and academic adjustment. Journal of Research on Adolescence, 31(3), 486–499. 10.1111/jora.12668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffee B. W., Cheng J., Couch E. T., Hoeft K. S., Halpern-Felsher B. (2021). Adolescents’ substance use and physical activity before and during the COVID-19 pandemic. JAMA Pediatrics, 175(7), 715. 10.1001/jamapediatrics.2021.0541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaturvedi K., Vishwakarma D. K., Singh N. (2021). COVID-19 and its impact on education, social life and mental health of students: A survey. Children and Youth Services Review, 121, 105866. 10.1016/j.childyouth.2020.105866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis D. (2020). Pediatrics and COVID-19. JAMA, 324(12), 1147–1148. [DOI] [PubMed] [Google Scholar]
- Enlow P., Phan T. L., Lewis A., Hildenbrand A., Sood E., Canter K., Vega G., Alderfer M., Kazak A. (2022). Validation of the COVID-19 Exposure and Family Impact Scales (CEFIS). Journal of Pediatric Psychology, 47(3), 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman C. H., Balistreri K. A., Lampert S., Durkin L. K., Bugno L. T., Davies W. H., Greenley R. N. (2021). Emerging adults’ adherence to preventative health guidelines in response to COVID-19. Journal of Pediatric Psychology, 46(6), 635–644. 10.1093/jpepsy/jsab047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Jawanda M. K. (2020). The impacts of COVID-19 on children. Acta Paediatrica (Oslo, Norway: 1992), 109(11), 2181–2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong A. M., Benner A. D., Erdem G., Lansford J. E., Makila L. M., Petrie R. C.; The SRA COVID-19 Response Team. (2021). Adolescence amid a pandemic: Short- and long-term implications. Journal of Research on Adolescence, 31(3), 820–835. 10.1111/jora.12671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal K., Li J., Hahm H., Liu C. (2021). Psychiatric impacts of the COVID-19 global pandemic on U.S. sexual and gender minority young adults. Psychiatry Research, 299, 113855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A., Alderfer M., Enlow P., Lewis A., Vega G., Barakat L., Kassam-Adams N., Pai A., Canter K., Hildenbrand A., McDonnell G., Price J., Schultz C., Sood E., Phan L. (2021). COVID-19 Exposure and Impact Scales (CEFIS): Factor structure and initial psychometrics. Journal of Pediatric Psychology, 46(5), 504–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A., Green H., Compas B. E., Dickey L., Pegg S. (2020). Exposure to COVID‐19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depression and Anxiety, 37(12), 1280–1288. [DOI] [PubMed] [Google Scholar]
- Listernick Z., Badawy S. (2021). Mental health implications of the COVID-19 pandemic among children and adolescents: What do we know so far? Pediatric Health, Medicine and Therapeutics, 12, 543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mara C., Peugh J. (2020). Validity of data collected from randomized behavioral clinical trials during the COVID-19 pandemic. Journal of Pediatric Psychology, 45(9), 971–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagoto S. L., Conroy D. E. (2021). Revitalizing adolescent health behavior after the COVID-19 pandemic. JAMA Pediatrics, 175(7), 677–679. 10.1001/jamapediatrics.2021.0547 [DOI] [PubMed] [Google Scholar]
- Pater A. A. (2021). Emergence and evolution of a prevalent new SARS-CoV-2 variant in the United States. bioRxiv. Advance online publication. https://doi.org/10.1101/2021.01.11.426287
- Price J., Kassam-Adams N., Alderfer M., Christofferson J., Kazak A. (2016). An integrative model of pediatric medical traumatic stress: An update based on a systematic literature review. Journal of Pediatric Psychology, 41(1), 86–97. [DOI] [PubMed] [Google Scholar]
- Samji H., Wu J., Ladak A., Vossen C., Stewart E., Dove N., Long D., Snell G. (2021). Review: Mental health impacts of the COVID-19 pandemic on children and youth - a systematic review. Child and Adolescent Mental Health. Advance online publication. https://doi.org/10.1111/camh.12501 [DOI] [PMC free article] [PubMed]
- Socarras L. R., Potvin J., Forest G. (2021). COVID-19 and sleep patterns in adolescents and young adults. Sleep Medicine, 83, 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields C., Plevinsky J., Psihogios A., Holmbeck G. (2020). Considerations and future directions for conducting research with pediatric populations during the COVID-19 pandemic. Journal of Pediatric Psychology, 45(7), 720–724. 10.1093/jpepsy/jsaa055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields C., Kritikos T. K., Ridosh M. M., Starnes M., Holmbeck G. N. (2021). “We Are Anxious Every Day”: COVID-19 impacts on youth with spina bifida. Journal of Pediatric Psychology, 46(9), 1040–1011. 10.1093/jpepsy/jsab070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud I., Gutman L. M. (2021). Longitudinal changes in the mental health of UK young male and female adults during the COVID-19 pandemic. Psychiatry Research, 303, 114074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2019). Multivariate statistics (7th edn). Pearson. [Google Scholar]
- Tasso A., Sahin N., San Roman G. (2021). COVID-19 disruption on college students: Academic ad socioemotional implications. Psychological Trauma: Theory, Research, Practice and Policy, 13(1), 9–15. [DOI] [PubMed] [Google Scholar]
- Walensky R. P., Walke H. T., Fauci A. S. (2021). SARS-CoV-2 variants of concern in the United States—Challenges and opportunities. JAMA, 325(11), 1037–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson O. W., Holland K. E., Elliott L. D., Duffey M., Bopp M. (2021). The impact of the COVID-19 pandemic on US college students’ physical activity and mental health. Journal of Physical Activity & Health, 18(3), 272–278. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.