Abstract
Direct-to-consumer (DTC) prescription drug advertisements (ads) sometimes include information about the disease condition in addition to information about the advertised product. Although the intent of such information is to educate about the disease condition, in some cases consumers may mistakenly assume that the drug will address all of the potential consequences of the condition mentioned in the ad. We investigated the effects of adding disease information to DTC prescription drug print ads on consumer product perceptions and understanding.
Participants (4,064 adults) viewed one of 15 DTC print ads for fictitious prescription drugs indicated to treat COPD, anemia, or lymphoma that varied in disease information presence, type, and format. Participants answered questions that assessed risk and benefit memory, perception, and behavioral intentions. Results indicate that exposure to disease information as part of DTC prescription drug ads can promote the impression that the drug addresses consequences of the condition that are not part of the drug’s indication.
Keywords: disease awareness, prescription drug advertising, direct-to-consumer
The pharmaceutical industry spent $27 billion promoting their products to American health care professionals and consumers in 2012, of which approximately $3.4 billion was directed toward the consumer market (Cegedim Strategic Data, 2013). Television ads get much of the attention in this area. By 2004, direct-to-consumer (DTC) prescription drug ads comprised approximately 2.4% of all ads on TV, which represented about 16 hours of yearly viewing time (Brownfield, Bernhardt, Phan, Williams, & Parker, 2004). However, print ads remain a strong source of spending, with approximately $1.2 billion dollars spent on newspaper and magazine DTC ads in 2013 (Dobrow, 2014). Because such marketing directly engages consumers and affects interactions between patients and their physicians (Kravitz et al., 2005; Palumbo & Mullins, 2002), it is critical to assess the influence of DTC ads on consumers’ understanding of prescription drug information.
Disease Awareness Ads Versus Product Claim Ads
As a public health agency, FDA encourages the communication of accurate health messages about diseases and treatments. Disease awareness ads are “communications disseminated to consumers or healthcare practitioners that discuss a particular disease or health condition, but do not mention any specific drug or device or make any representation or suggestion concerning a particular drug or device.” (U.S. Food and Drug Administration [FDA], 2014). FDA believes that disease awareness ads can give consumers important information about medical conditions and can encourage them to search for information about treatments. Thus, as a public health agency, FDA encourages the use of disease awareness ads: “Because no drug product is mentioned or implied, this type of ad is not considered to be a drug ad and is not regulated by FDA, but we enthusiastically support their use…” (FDA, 2005).
Product claim advertising, in comparison to disease awareness advertising, is designed to promote a particular drug product. FDA regulations require that product claim ads for prescription drugs contain accurate information about the benefits and risks of the drug advertised (CFR, 2013). Specifically, the advertising must contain the FDA-approved indication for use of the drug for the purpose claimed in the ad (21 C.F.R. 202.1(e)(3)(ii)), and must not be false or misleading with respect to the effectiveness of the drug (21 C.F.R 202.1(e)(5)(i)). For example, the ad must not contain a representation or suggestion that the drug is better, more effective, or useful in a broader range of conditions or patients than has been demonstrated by substantial evidence or substantial clinical experience (21 C.F.R 202.1(e)(6)(i)).
Although product claim advertising is viewed as providing some informational value and increases awareness of available treatments (Aikin, Swasy, & Braman, 2004; Deshpande, Menon, Perri, & Zinkhan, 2004; Weissman et al., 2004; Weissman et al., 2003), opposing views have raised questions about the value of DTC product claim ads relative to their negative effects and potential costs (Mintzes, 2012). Some research has shown that disease-awareness advertising is viewed by consumers as more informative and containing less persuasive intent than product claim advertising (Hall, Jones, & Hoek, 2011; Lee-Wingate & Xie, 2010), and may be useful for generating moderately positive attitudes toward the company among low-involvement consumers (Rollins, King, Zinkhan, & Perri, 2011). Research has also shown that disease awareness ads result in more intent to seek more information, compared to product claim ads (Mendonca, McCaffrey, Banahan, Bentley, & Yang, 2011; Rollins, King, Zinkhan, & Perri, 2010).
Including Disease Awareness Information in Product Claim Ads
In addition to disease awareness ads, sponsors may also choose to include disease information in their product claim ads. Such information is designed to educate consumers about the disease condition. However, it may also influence their perceptions of the drug. For instance, consumers’ intention to ask their doctor about the disease or product is influenced by the number of disease symptoms included in the ad (Lee-Wingate & Xie, 2013).
In some cases a full description of the disease includes information about specific health outcomes that are not part of a drug’s approved indication. When broad disease information accompanies or is included in an ad for a specific drug, researchers have found that consumers may mistakenly assume the drug will address all of the potential consequences of the condition mentioned in the ad by making inferences that go beyond what is explicitly stated in the ad (Burke, DeSarbo, Oliver, & Robertson, 1988; Harris, 1977; Jacoby & Hoyer, 1987). These researchers argue that the success of an advertising campaign may depend on the extent to which consumers infer information about a product beyond what is presented in the advertising copy. The researchers also note that advertisers often craft advertising text to lead consumers to make specific inferences about the product. These elements are called implicit claims, which are plausible conclusions about the product that are not explicitly stated by the advertising but could be inferred by the consumers based on the information presented (Harris, 1977). The combination of broad disease information and product claims in one ad may lead consumers to infer effectiveness of the drug beyond the indications for which it was approved or has been demonstrated. For example, the mention of heart attack in an ad for a drug indicated to lower blood glucose may lead consumers to infer the drug will prevent heart attacks, even if no direct claim is made.
If consumers are able to distinguish between disease information and product claims, then they will not be misled by the inclusion of disease information in a DTC product claim ad. If consumers are unable to distinguish these two, however, then consumers may be misled into believing that a particular drug is effective against certain long-term consequences. The likelihood of connecting the disease information to the product information may be increased by factors that cause consumers to perceive these parts as linked, such as similarity in terms of theme, colors, logos, tag lines, and graphics.
FDA has described situations in which disease awareness communications might be viewed as labeling or advertising and therefore subject to regulation. Although the agency does not have current guidance with regard to disease awareness communications, FDA has considered perceptual similarity (e.g., similarity in color schemes, design layouts, and other presentation elements) between purported disease awareness communications and branded promotional materials as a factor that contributes to these communications being viewed as not distinct from product claim ads which are subject to FDA regulation (FDA, 2010). One way to achieve distinct presentations is by deliberately and clearly separating disease information from product information, both in terms of appearance and proximity.
Our study tested separation in terms of appearance. We examined the effects of adding disease information to DTC prescription drug print ads on consumer perceptions and understanding. We hypothesized that individuals presented with information about the consequences of the disease in a DTC print ad would be more likely to incorrectly believe that the drug would reduce the likelihood of these consequences, compared with individuals who viewed ads without disease information or with information about the disease that was unrelated to disease consequences (i.e., causes of the disease). We also hypothesized that including this information in DTC print ads would have a negative impact on understanding of the actual drug benefits. We hypothesized that including this information in DTC print ads would affect perceptions, including higher perceived efficacy, lower perceived risk, and a risk/benefit balance tilted toward benefits. We expected this information to lead participants to be more likely to search for drug and disease information. In addition, we hypothesized that participants would be more likely to connect the disease information and the product information when it was presented as part of one ad (integrated) versus presented as two ads (separated). We measured risk recall and recognition to determine whether including additional information in a DTC print ad affected these important variables.
Method
Design
The study examined three variables: the presence of disease information, the type of disease information (consequence versus cause information), and the format of this information (integrated versus separated) in a 2 (information type) × 2 (format) + 1 (control) design. The control condition did not include any disease information. Consequence information consisted of consequences of the disease (e.g., fatigue, death). Cause information consisted of risk factors for the disease (e.g., age, exposure to toxic chemicals). The integrated format interspersed disease information and product claims in the same ad using identical fonts and colors for disease and product claims (see Figure 1 for an example of one ad created for the study). The separated format placed disease information on one page and product claims on another page, using different visuals and fonts for disease and product claims to create two distinct ads (see Figure 2 for an example). To examine whether results would generalize across medical conditions, we tested ads in three different medical conditions: chronic obstructive pulmonary disorder (COPD), anemia, and lymphoma. We chose these as exemplars of chronic (COPD, lymphoma) and acute (anemia) medical conditions which had plausible cause and consequence information, and for which the general population was unlikely to have in-depth, pre-existing knowledge.
Figure 1.
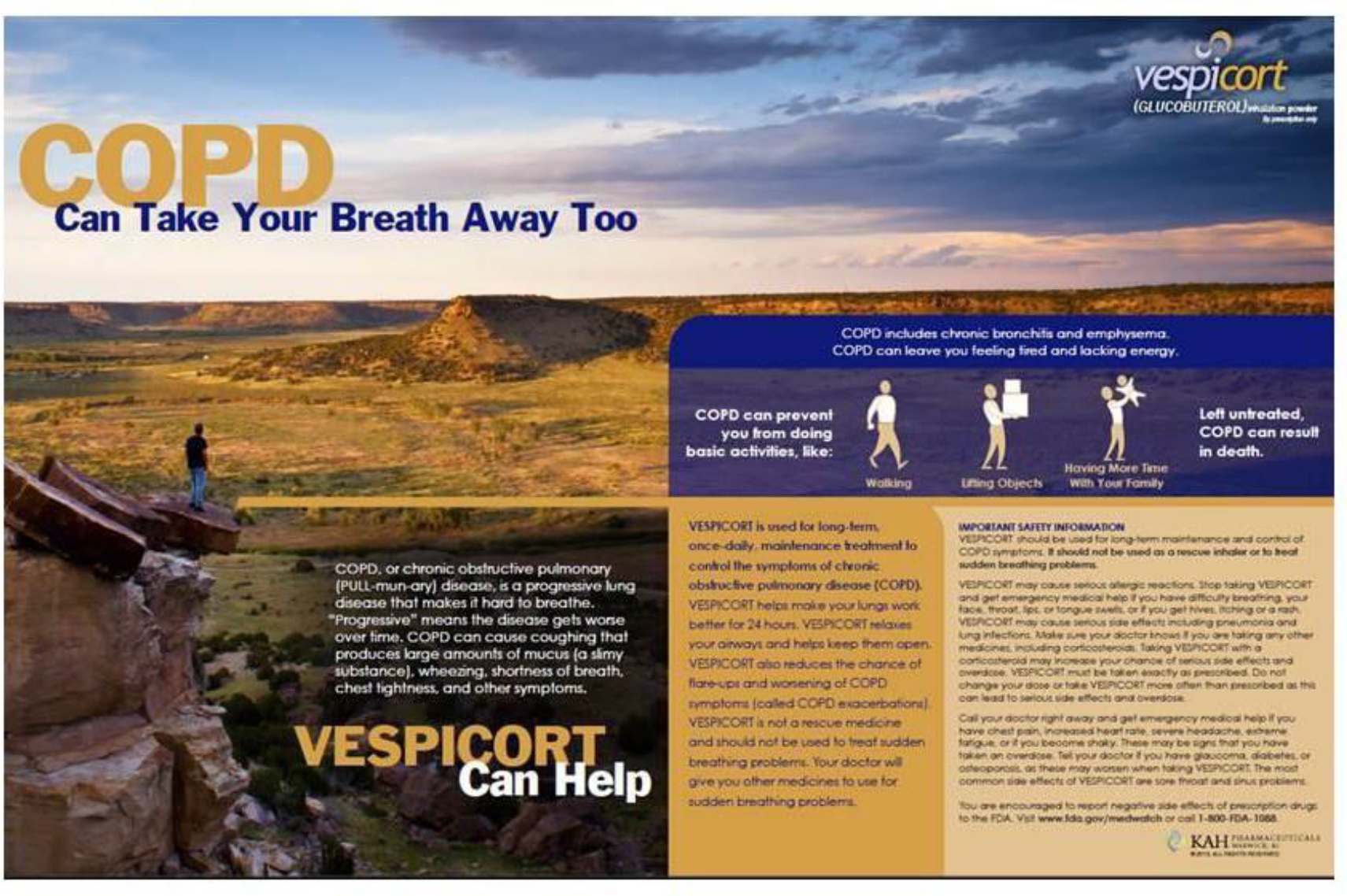
Integrated ad with consequence information
Figure 2.

Separated ad with cause information
Procedure
Participants were recruited from Knowledge Networks Internet panel (GfK Custom Research, 2013). Adults were eligible for the study if they were not healthcare professionals and did not work for a pharmaceutical company, advertising agency, or market research company.
Participants were recruited as part of a general population sample and may or may not have had the condition in the ad (see Table 1). Participants were randomly assigned to one of the 15 experimental conditions. Participants viewed the ad for as long as they liked. Next, participants completed a questionnaire and could view the ad again while completing the questionnaire. We designed the questionnaire using cognitive interviews (Willis, 2005) and three pretests. The same questionnaire was given to all participants, except that the drug name, medical condition, and specific benefit and risks changed depending on the medical condition featured in the ad they viewed.
Table 1.
Participant Characteristics by Medical Condition
| Medical condition treated by fictitious advertised drug | |||
|---|---|---|---|
|
| |||
| Demographic variable | COPD N (%) | Anemia N (%) | Lymphoma N (%) |
|
| |||
| N | 1369 | 1367 | 1328 |
| White | 1121 (81.9) | 1113 (81.4) | 1094 (82.4) |
| Non-White | 248 (18.1) | 254 (18.6) | 234 (17.6) |
| Hispanic | 146 (10.7) | 142 (10.4) | 133 (10.0) |
| Not Hispanic | 1223 (89.3) | 1225 (89.6) | 1195 (90.0) |
| High school or less | 465 (34.0) | 516 (37.7) | 456 (34.3) |
| Some college or more | 904 (66.0) | 851 (62.3) | 872 (65.7) |
| Female | 617 (45.1) | 638 (46.7) | 643 (48.4) |
| Male | 752 (54.9) | 729 (53.3) | 685 (51.6) |
| Diagnosed with [disease] | 76 (5.6) | 161 (11.8) | 8 (0.6) |
|
|
|||
| Mean (SD) | Mean (SD) | Mean (SD) | |
|
|
|||
| Age (in years) | 54.4 (16.12) | 53.5 (16.28) | 53.4 (16.28) |
| How often do you have someone help you read instructions? (1 = always, 5 = never) | 4.37 (1.03) | 4.35 (1.05) | 4.44 (.96) |
| How confident are you filling out medical forms? (1 = not at all, 5 = extremely) | 4.27 (0.99) | 4.20 (0.97) | 4.19 (1.01) |
| Knowledge about COPD (1 = a lot, 5 = nothing at all) | 3.86 (1.02) | 3.88 (1.03) | 3.86 (1.04) |
| Knowledge about Anemia (1 = a lot, 5 = nothing at all) | 3.60 (0.88) | 3.60 (0.92) | 3.57 (0.93) |
| Knowledge about Lymphoma (1 = a lot, 5 = nothing at all) | 4.14 (0.86) | 4.10 (0.87) | 4.11 (0.83) |
Measures
Benefit recall.
Participants were asked “What are the benefits of [Drug X]?” We created three measures from the responses to this open-ended question: (1) the number of correct benefits listed (0–4 in all medical conditions), (2) the number of consequence concepts incorrectly listed as drug benefits (0–4 in COPD, 0–5 in anemia, and 0–3 in lymphoma conditions), and (3) the number of cause concepts incorrectly listed as drug benefits (0–4 in COPD, 0–3 in anemia, and 0–1 in lymphoma conditions).
Benefit recognition.
Participants saw statements about the benefits of the product and indicated if, based on the information in the ad, the statement was a benefit of taking the product (yes/no). Responses were summed to create three indices: (1) the number of drug benefits correctly identified (e.g., “[Drug X] treats iron-deficiency anemia in adults;” 0–4 for COPD and lymphoma, 0–3 for anemia conditions), (2) the number of consequence concepts incorrectly identified as a drug benefit (e.g., “[Drug X] prevents liver damage;” 0–4), and (3) the number of cause concepts incorrectly identified as a drug benefit (e.g., “[Drug X] reduces the chance seniors will get anemia;” 0–4).
Risk recall.
Participants were asked “What are the risks of [Drug X]?” We summed the number of correct risks participants listed in response to this open-ended question (0–12 in COPD, 0–10 in anemia conditions, and 0–9 in lymphoma conditions).
Risk recognition.
Participants saw eight statements about the risks of the product (such as “[Drug X] may cause kidney failure”) and indicated if, based on the information in the ad, the statement was a risk of taking the product (yes/no). Correct responses were summed to create a risk recognition index (0–8).
Perceived efficacy.
We asked participants about their perceptions of the drug’s efficacy both in terms of likelihood (“In your opinion, if 100 people take [Drug X], for what percentage of people would the drug work?”; 0% to 100%) and in terms of magnitude (“In your opinion, if [Drug X] did help a person’s [disease condition], how much would it help?”; 1 = would help [disease condition] a little, 5 = would help [disease condition] a lot).
Perceived risk.
We asked participants about their perceptions of the drug’s risks both in terms of likelihood (“In your opinion, if 100 people take [Drug X], what percentage of people will have any side effects or negative outcomes?”; 0% to 100%) and in terms of magnitude (“In your opinion, if [Drug X] did cause a person with [disease condition] to have side effects or negative outcomes, how serious would they be?”; 1 = not at all serious, 5 = very serious).
Perceived risk/benefit balance.
Participants rated their perception of the balance of risks and benefits of the drug (1 = many more risks than benefits, 5 = many more benefits than risks).
Behavioral intention.
Participants rated the following four statements (1 = not at all likely, 5 = extremely likely):
“If someone with [disease condition] saw this ad, how likely would that person be to ask their doctor about [Drug X]?”
“If someone with [disease condition] saw this ad, how likely would that person be to look for more information about [Drug X]?”
“If someone with [disease condition] saw this ad, how likely would that person be to look for more information about [disease condition]?”
“If one of your family members had [disease condition], how likely would you be to mention [Drug X] to them?”
We created a measure of behavioral intention from the mean of these four items (Cronbach’s α = .86).
Analyses
The sample size was based on a priori power analyses. We conducted 2 × 2 ANOVAs to test the main effects of the disease information’s type (consequence versus cause) and format (integrated versus separated), and the interaction between them. We examined significant interactions by conducting pairwise comparisons among experimental conditions using a Bonferroni-adjusted p-value of .008 (.05/6 comparisons). In addition, we conducted pairwise comparisons between the control condition and each of the four experimental conditions for all variables using a Bonferroni-adjusted p-value of .0125 (.05/4 comparisons). We present Cohen’s f as a measure of effect size. Because some of the recognition and recall variables were not normally distributed, we examined these measures using analyses that took into account their distribution. The pattern of the results was the same as it was with the ANOVA; therefore for ease of interpretation we report only the ANOVA results.
Results
Tables 2, 3, and 4 present the results for the COPD, anemia, and lymphoma conditions, respectively.
Table 2.
COPD: Means (Standard Deviations) of Dependent Variables by Format and Information Type
| Consequence |
Cause |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Integrated | Separated | Total | Integrated | Separated | Total | Integrated | Separated | |
|
| |||||||||
| Benefit recall | |||||||||
| Correctly recalled benefits | 1.56 (1.12) | 1.28 (1.17)* | 1.43 (1.20) | 1.36 (1.19) | 1.33 (1.10) | 1.37 (1.13) | 1.35 (1.12) | 1.31 (1.14) | 1.40 (1.17) |
| Incorrectly listed consequences | 0.41 (0.51) | 0.67 (0.85)*♦^† | 0.48 (0.69) | 0.58 (0.78) | 0.47 (0.57) | 0.51 (0.62) | 0.50 (0.60) | 0.57 (0.73) | 0.50 (0.65) |
| Incorrectly listed causes | 0.41 (0.51) | 0.53 (0.64) | 0.40 (0.57) | 0.47 (0.61) | 0.49 (0.60) | 0.52 (0.62) | 0.50 (0.61) | 0.51 (0.62) | 0.46 (0.59) |
| Benefit recognition | |||||||||
| Correctly identified benefits | 3.61 (0.73) | 3.49 (0.98) | 3.62 (0.80) | 3.56 (0.89) | 3.55 (0.84) | 3.51 (0.88) | 3.53 (0.86) | 3.52 (0.91) | 3.56 (0.84) |
| Incorrectly identified consequences | 1.46 (1.39) | 2.79 (1.35)* | 2.67 (1.35)* | 2.73 (1.35)▲ | 1.62 (1.51) | 1.74 (1.40) | 1.68 (1.45) | 2.21 (1.54) | 2.20 (1.45) |
| Incorrectly identified causes | 0.43 (0.93) | 0.55 (1.02) | 0.51 (1.00) | 0.53 (1.01)▲ | 0.78 (1.03)* | 0.75 (1.05)* | 0.76 (1.04) | 0.66 (1.03) | 0.63 (1.03) |
| Risk recall | 2.61 (1.84) | 2.54 (1.83) | 2.52 (1.77) | 2.53 (1.80) | 2.42 (1.71) | 2.42 (1.60) | 2.42 (1.65) | 2.48 (1.77) | 2.47 (1.68) |
| Risk recognition | 6.13 (1.39) | 5.82 (1.66) | 6.04 (1.54) | 5.93 (1.61) | 5.91 (1.46) | 6.10 (1.47) | 6.01 (1.47) | 5.86 (1.56)● | 6.07 (1.51) |
| Perceived efficacy likelihood | 57.96 (23.13) | 60.15 (20.48) | 56.54 (22.40) | 58.30 (21.54) | 58.16 (21.86) | 59.25 (21.07) | 58.73 (21.44) | 59.17 (21.17) | 57.90 (21.77) |
| Perceived efficacy magnitude | 3.63 (0.87) | 3.61 (0.97) | 3.61 (0.99) | 3.61 (0.98) | 3.49 (0.95) | 3.55 (0.84) | 3.52 (0.89) | 3.55 (0.96) | 3.58 (0.92) |
| Perceived risk likelihood | 34.31 (21.86) | 35.18 (20.81) | 33.64 (21.37) | 34.39 (21.10) | 34.10 (20.12) | 31.58 (19.59) | 32.77 (19.86) | 34.65 (20.46) | 32.60 (20.50) |
| Perceived risk magnitude | 3.48 (1.00) | 3.52 (1.02) | 3.57 (0.97) | 3.54 (1.00) | 3.47 (1.00) | 3.39 (0.97) | 3.43 (0.98) | 3.49 (1.01) | 3.48 (0.97) |
| Perceived risk/benefit balance | 3.25 (1.06) | 3.36 (1.03) | 3.37 (1.03) | 3.36 (1.03) | 3.34 (0.95) | 3.47 (1.05)* | 3.41 (1.00) | 3.35 (0.99) | 3.42 (1.04) |
| Behavioral intention | 3.85 (0.81) | 3.99 (0.80) | 3.87 (0.81) | 3.93 (0.81) | 3.81 (0.84) | 3.92 (0.81) | 3.87 (0.83) | 3.90 (0.83) | 3.90 (0.81) |
Note. Recall and recognition measure range from no benefits or risks recalled or recognized to the maximum number recalled or recognized. Other dependent variables were measured on the following scales: perceived efficacy and risk likelihood (0%-100%), perceived efficacy magnitude (1 = would help a little, 5 = would help a lot), perceived risk magnitude (1 = not at all serious, 5 = very serious), perceived risk/benefit balance (1 = many more risks than benefits, 5 = many more benefits than risks), and behavioral intention (1 = not at all likely, 5 = extremely likely).
Significantly different from control condition (p < .0125 for comparisons to control).
Significantly different from consequence separated condition (p < .008 for pairwise comparisons).
Significantly different from cause integrated condition (p < .008 for pairwise comparisons).
Significantly different from cause separated condition (p < .008 for pairwise comparisons).
Significantly different from total cause condition (p < .05 for main effects).
Significantly different from total separated condition (p < .05 for main effects).
Table 3.
Anemia: Means (Standard Deviations) of Dependent Variables by Format and Information Type
| Consequence | Cause | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Integrated | Separated | Total | Integrated | Separated | Total | Integrated | Separated | |
|
| |||||||||
| Benefit recall | |||||||||
| Correctly recalled benefits | 1.20 (0.66) | 1.03 (0.74)* | 1.17 (0.71) | 1.10 (0.72)▲ | 1.17 (0.73) | 1.21 (0.67) | 1.19 (0.70) | 1.10 (0.73)● | 1.19 (0.69) |
| Incorrectly listed consequences | 0.09 (0.28) | 0.52 (0.94)* | 0.45 (0.85)* | 0.49 (0.89)▲ | 0.25 (0.54) | 0.22 (0.50) | 0.24 (0.52) | 0.39 (0.78) | 0.33 (0.71) |
| Incorrectly listed causes | 0.12 (0.32) | 0.28 (0.49)* | 0.25 (0.46)* | 0.26 (0.47) | 0.28 (0.53)* | 0.27 (0.50)* | 0.28 (0.51) | 0.28 (0.51) | 0.26 (0.48) |
| Benefit recognition | |||||||||
| Correctly identified benefits | 2.52 (0.67) | 2.39 (0.76) | 2.46 (0.79) | 2.42 (0.78) | 2.44 (0.69) | 2.55 (0.68) | 2.49 (0.69) | 2.41 (0.73)● | 2.50 (0.74) |
| Incorrectly identified consequences | 0.41 (0.90) | 2.11 (1.51)* | 1.94 (1.64)* | 2.03 (1.58)▲ | 0.58 (1.08) | 0.63 (1.05) | 0.61 (1.07) | 1.35 (1.52) | 1.29 (1.52) |
| Incorrectly identified causes | 0.75 (1.11) | 1.01 (1.27) | 0.86 (1.19) | 0.93 (1.23)▲ | 2.08 (1.30)* | 1.72 (1.36)* | 1.90 (1.34) | 1.54 (1.39)● | 1.29 (1.35) |
| Risk recall | 2.60 (1.75) | 2.14 (1.74)* | 2.36 (1.58) | 2.25 (1.66) | 2.39 (1.64) | 2.47 (1.65) | 2.43 (1.64) | 2.26 (1.69) | 2.42 (1.61) |
| Risk recognition | 6.11 (1.61) | 5.48 (1.81)* | 5.75 (1.81) | 5.61 (1.82)▲ | 5.91 (1.75) | 5.91 (1.71) | 5.91 (1.72) | 5.69 (1.79) | 5.83 (1.76) |
| Perceived efficacy likelihood | 51.50 (25.74) | 54.32 (23.18) | 53.31 (24.99) | 53.82 (24.09) | 53.46 (25.23) | 55.51 (22.71) | 54.49 (23.99) | 53.90 (24.20) | 54.41 (23.88) |
| Perceived efficacy magnitude | 3.33 (1.09) | 3.50 (0.98) | 3.48 (1.01) | 3.49 (1.00) | 3.42 (1.11) | 3.49 (1.00) | 3.46 (1.06) | 3.46 (1.05) | 3.48 (1.00) |
| Perceived risk likelihood | 37.17 (22.00) | 34.33 (22.79) | 32.99 (21.43) | 33.66 (22.11) | 35.17 (23.81) | 32.89 (21.94) | 34.02 (22.90) | 34.75 (23.28) | 32.94 (21.67) |
| Perceived risk magnitude | 3.55 (1.07) | 3.36 (0.97) | 3.37 (1.03) | 3.37 (1.00) | 3.45 (0.99) | 3.48 (0.99) | 3.47 (0.99) | 3.41 (0.98) | 3.42 (1.01) |
| Perceived risk/benefit balance | 2.95 (1.15) | 3.16 (1.06) | 3.19 (1.02)* | 3.17 (1.04) | 3.15 (1.05) | 3.09 (1.08) | 3.12 (1.07) | 3.15 (1.06) | 3.14 (1.05) |
| Behavioral intention | 3.58 (0.88) | 3.73 (0.82) | 3.74 (0.76) | 3.73 (0.79) | 3.74 (0.80) | 3.73 (0.82) | 3.74 (0.81) | 3.73 (0.81) | 3.74 (0.79) |
Note. Recall and recognition measure range from no benefits or risks recalled or recognized to the maximum number recalled or recognized. Other dependent variables were measured on the following scales: perceived efficacy and risk likelihood (0%-100%), perceived efficacy magnitude (1 = would help a little, 5 = would help a lot), perceived risk magnitude (1 = not at all serious, 5 = very serious), perceived risk/benefit balance (1 = many more risks than benefits, 5 = many more benefits than risks), and behavioral intention (1 = not at all likely, 5 = extremely likely).
Significantly different from control condition (p < .0125 for comparisons to control).
Significantly different from total cause condition (p < .05 for main effects).
Significantly different from total separated condition (p < .05 for main effects).
Table 4.
Lymphoma: Means (Standard Deviations) of Dependent Variables by Format and Information Type
| Consequence |
Cause |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Integrated | Separated | Total | Integrated | Separated | Total | Integrated | Separated | |
|
| |||||||||
| Benefit recall | |||||||||
| Correctly recalled benefits | 0.77 (0.85) | 0.72 (0.90) | 0.68 (0.86) | 0.70 (0.88) | 0.66 (0.83) | 0.73 (0.87) | 0.69 (0.85) | 0.69 (0.87) | 0.70 (0.87) |
| Incorrectly listed consequences | 0.22 (0.42) | 0.25 (0.51) | 0.26 (0.48) | 0.26 (0.49) | 0.21 (0.41) | 0.21 (0.41) | 0.21 (0.41) | 0.23 (0.46) | 0.24 (0.45) |
| Incorrectly listed causes | 0.06 (0.24) | 0.08 (0.27) | 0.08 (0.27) | 0.08 (0.27) | 0.05 (0.22) | 0.09 (0.29) | 0.07 (0.26) | 0.07 (0.25) | 0.09 (0.28) |
| Benefit recognition | |||||||||
| Correctly identified benefits | 3.52 (0.98) | 3.39 (1.06) | 3.51 (1.01) | 3.45 (1.04) | 3.40 (1.06) | 3.43 (1.00) | 3.41 (1.03) | 3.39 (1.06) | 3.47 (1.00) |
| Incorrectly identified consequences | 0.66 (0.93) | 1.22 (1.22)* | 1.17 (1.21)* | 1.19 (1.22)▲ | 0.81 (0.99) | 0.77 (0.93) | 0.79 (0.96) | 1.02 (1.13) | 0.97 (1.10) |
| Incorrectly identified causes | 0.67 (1.10) | 0.88 (1.28) | 0.93 (1.34) | 0.90 (1.31) | 0.86 (1.22) | 0.83 (1.15) | 0.84 (1.18) | 0.87 (1.25) | 0.88 (1.25) |
| Risk recall | 2.19 (1.50) | 1.93 (1.51) | 2.11 (1.54) | 2.02 (1.52)▲ | 2.20 (1.43) | 2.36 (1.52) | 2.29 (1.48) | 2.06 (1.48) | 2.24 (1.53) |
| Risk recognition | 5.59 (1.58) | 5.32 (1.54) | 5.35 (1.44) | 5.33 (1.49)▲ | 5.70 (1.48) | 5.66 (1.52) | 5.68 (1.50) | 5.50 (1.52) | 5.50 (1.49) |
| Perceived efficacy likelihood | 36.65 (21.36) | 39.62 (22.06) | 37.67 (21.16) | 38.62 (21.60) | 38.03 (21.74) | 37.36 (22.59) | 37.68 (22.17) | 38.85 (21.90) | 37.52 (21.85) |
| Perceived efficacy magnitude | 2.94 (1.03) | 3.02 (1.01) | 2.96 (1.05) | 2.99 (1.03)▲ | 2.87 (1.07) | 2.83 (1.09) | 2.85 (1.08) | 2.94 (1.04) | 2.89 (1.07) |
| Perceived risk likelihood | 49.66 (27.44) | 50.42 (23.46) | 52.72 (26.29) | 51.61 (24.97)▲ | 44.47 (25.34) | 51.45 (25.34) | 48.08 (25.55) | 47.53 (24.55)● | 52.10 (25.81) |
| Perceived risk magnitude | 3.66 (0.94) | 3.70 (0.90) | 3.71 (0.98) | 3.71 (0.94) | 3.62 (1.01) | 3.77 (0.88) | 3.70 (0.95) | 3.66 (0.95) | 3.74 (0.93) |
| Perceived risk/benefit balance | 2.58 (1.08) | 2.72 (1.06) | 2.72 (1.09) | 2.72 (1.07)▲ | 2.59 (1.10) | 2.45 (1.12) | 2.52 (1.11) | 2.66 (1.08) | 2.59 (1.11) |
| Behavioral intention | 3.83 (0.93) | 3.75 (0.94) | 3.72 (0.96) | 3.74 (0.95) | 3.74 (0.96) | 3.67 (0.94) | 3.70 (0.95) | 3.74 (0.95) | 3.70 (0.95) |
Note. Recall and recognition measure range from no benefits or risks recalled or recognized to the maximum number recalled or recognized. Other dependent variables were measured on the following scales: perceived efficacy and risk likelihood (0%-100%), perceived efficacy magnitude (1 = would help a little, 5 = would help a lot), perceived risk magnitude (1 = not at all serious, 5 = very serious), perceived risk/benefit balance (1 = many more risks than benefits, 5 = many more benefits than risks), and behavioral intention (1 = not at all likely, 5 = extremely likely).
Significantly different from control condition (p < .0125 for comparisons to control).
Significantly different from total cause condition (p < .05 for main effects).
Significantly different from total separated condition (p < .05 for main effects).
Participants
Participants were 4,064 adults. See Table 1 for participant characteristics.
Benefit recall
COPD.
Correctly recalling benefits.
Participants who saw the control ad correctly recalled more drug benefits than did participants who saw the integrated consequence ad, F(1, 1364) = 8.43, p = .004, f = .08.
Incorrectly listing consequences as drug benefits.
There was a significant interaction between format and information type, F(1, 1073) = 6.86, p = .01, f = .08. Participants who saw the integrated consequence ad incorrectly listed more consequences as drug benefits than did participants in all other conditions, including the control condition: consequence separated, F(1, 1364) = 10.25, p = .001, f = .08; cause integrated, F(1, 1364) = 11.39, p = .001, f = .09; cause separated, F(1, 1364) = 7.50, p = .006, f = .07; and control, F(1, 1364) = 20.84, p < .001, f = .12.
Incorrectly listing causes as drug benefits.
There was a significant interaction between format and information type, F(1, 1076) = 4.49, p = .03, f = .06. However, none of the pairwise comparisons were significant at p < .008.
Anemia.
Correctly recalling benefits.
There were main effects of information type, F(1, 1079) = 4.51, p = .03, f = .06, and format, F(1, 1079) = 4.81, p = .03, f = .06. Participants who saw the cause ad correctly recalled more drug benefits than those who saw the consequence ad. Participants who saw the separated ad correctly recalled more drug benefits than those who saw the integrated ad. In addition, participants who saw the control ad correctly recalled more drug benefits than did participants who saw the integrated consequence ad, F(1, 1362) = 8.96, p = .003, f = .08.
Incorrectly listing consequences as drug benefits.
There was a main effect of information type, F(1, 1079) = 31.77, p < .001, f = .17. Participants who saw the consequence ad incorrectly listed more consequences as drug benefits than those who saw the cause ad. In addition, participants who saw the control ad incorrectly listed fewer consequences as drug benefits than those who saw the integrated consequence ad and those who saw the separated consequence ad, F(1, 1362) = 59.39, p < .001, f = .21, and F(1, 1362) = 41.05, p < .001, f = .17, respectively.
Incorrectly listing causes as drug benefits.
Participants who saw the control ad incorrectly listed fewer causes as drug benefits compared with all other conditions: integrated consequence, F(1, 1362) = 16.97, p < .001, f = .11; separated consequence, F(1, 1362) = 11.29, p = .001, f = .09; integrated cause, F(1, 1362) = 18.14, p < .001, f = .11; and separated cause, F(1, 1362) = 16.25, p < .001, f = .11.
Lymphoma.
There were no significant differences for the three benefit recall measures.
Benefit recognition
COPD.
Correctly identifying benefits.
There were no significant effects.
Incorrectly identifying consequences as drug benefits.
There was a main effect of disease information, F(1, 1073) = 150.70, p < .001, f = .37. Participants who saw the consequence ad incorrectly identified more consequences as drug benefits than participants who saw the cause ad. In addition, participants who saw the control ad incorrectly identified fewer consequences as drug benefits than participants who saw the integrated consequence ad and participants who saw the separated consequence ad, F(1, 1364) = 126.27, p < .001, f = .30, and F(1, 1364) = 105.82, p < .001, f = .28, respectively.
Incorrectly identifying causes as drug benefits.
There was a main effect of information type, F(1, 1073) = 14.08, p < .001, f = .10. Participants who saw the cause ad incorrectly identified more causes as drug benefits than participants who saw the consequence ad. In addition, participants who saw the control ad incorrectly identified fewer causes as drug benefits than participants who saw the integrated cause ad and participants who saw the separated cause ad, F(1, 1364) = 16.46, p < .001, f = .11, and F(1, 1364) = 14.33, p < .001, f = .06, respectively.
Anemia.
Correctly identifying benefits.
There was a main effect of format, F(1, 1079) = 3.93, p = .048, f = .06. Participants who saw the separated ad correctly identified more benefits than participants who saw the integrated ad.
Incorrectly identifying consequences as drug benefits.
There was a main effect of information type, F(1, 1079) = 302.84, p < .001, f = .53. Participants who saw the consequence ad incorrectly identified more consequences as drug benefits than participants who saw the cause ad. In addition, participants who saw the control ad incorrectly identified fewer consequences as drug benefits than participants who saw the integrated consequence ad and participants who saw the separated consequence ad, F(1, 1362) = 250.10, p < .001, f = .43, and F(1, 1362) = 205.58, p < .001, f = .39, respectively.
Incorrectly identifying causes as drug benefits.
There were main effects of information type, F(1, 1079) = 154.02, p < .001, f = .39, and format, F(1, 1079) = 10.57, p = .001, f = .10. Participants who saw the cause ad incorrectly identified more causes as drug benefits than participants who saw the consequence ad. Participants who saw the integrated ad incorrectly identified more causes as drug benefits than participants who saw the separated ad. In addition, participants who saw the control ad incorrectly identified fewer causes as drug benefits than participants who saw the integrated cause ad and participants who saw the separated cause ad, F(1, 1362) = 155.95, p < .001, f = .34, and F(1, 1362) = 83.71, p < .001, f = .25, respectively.
Lymphoma.
Correctly identifying benefits.
There were no significant effects.
Incorrectly identifying consequence concepts as drug benefits.
There was a main effect of information type, F(1, 1051) = 35.59, p < .001, f = .17. Participants who saw the consequence ad incorrectly identified more consequences as drug benefits than participants who saw the cause ad. In addition, participants who saw the control ad incorrectly identified fewer consequences as drug benefits than participants who saw the integrated consequence ad and participants who saw the separated consequence ad, F(1, 1323) = 37.03, p < .001, f = .17, and F(1, 1323) = 31.49, p < .001, f = .15, respectively.
Incorrectly identifying cause concepts as drug benefits.
There were no significant effects.
Risk recall
COPD.
There were no significant effects.
Anemia.
Participants who saw the control ad recalled more risks than participants who saw the integrated consequence ad, F(1, 1362) = 10.67, p = .001, f = .09. There were no other significant effects.
Lymphoma.
There was a main effect of information type, F(1, 1051) = 8.09, p = .005, f = .09. Participants who saw the cause ad recalled more of the drug’s risks than participants who saw the consequence ad. There were no other significant effects.
Risk recognition
COPD.
There was a main effect of format, F(1, 1073) = 4.71, p = .03, f = .06. Participants who saw the separated ad correctly recognized more risks than participants who saw the integrated ad. There were no other significant effects.
Anemia.
There was a main effect of information type, F(1, 1079) = 7.73, p =.01, f = .08. Participants who saw the cause ad recognized more risks than participants who saw the consequence ad. In addition, participants who saw the control ad recognized more risks than participants who saw the integrated consequence ad, F(1, 1362) = 18.54, p < .001, f = .11. There were no other significant effects.
Lymphoma.
There was a main effect of information type, F(1, 1051) = 14.18, p < .001, f = .11. Participants who saw the cause ad recognized more risks than participants who saw the consequence ad. There were no other significant effects.
Perceived efficacy
COPD and Anemia.
There were no significant effects for either perceived efficacy measure.
Lymphoma.
There was a main effect of information type on the perceived efficacy magnitude measure, F(1, 1045) = 4.69, p = .03, f = .06. Participants who saw the consequence ad said the drug would be more effective than participants who saw the cause ad. There were no other significant effects.
Perceived risk
COPD and Anemia.
There were no significant effects for either perceived risk measure.
Lymphoma.
There were main effects of information type, F(1, 1006) = 5.20, p = .02, f = .07, and format, F(1, 1006) = 8.58, p = .003, f = .09, on the perceived risk likelihood measure. Participants who saw the consequence ad said a greater percentage of people would experience a side effect or negative reaction than participants who saw the cause ad. Similarly, participants who saw the separated ad said a greater percentage of people would experience a side effect or negative reaction than participants who saw the integrated ad. There were no other significant effects.
Perceived risk/benefit balance
COPD.
When considering the drug’s balance of risks and benefits, participants in the separated cause condition leaned more toward benefits than did participants in the control condition, F(1, 1353) = 6.59, p = .01, f = .07. There were no other significant effects.
Anemia.
When considering the drug’s balance of risks and benefits, participants in the separated consequence condition leaned more toward benefits than did participants in the control condition, F(1, 1354) = 7.07, p = .01, f = .07. There were no other significant effects.
Lymphoma.
There was a main effect of information type, F(1, 1046) = 8.95, p = .003, f = .09. When considering the drug’s balance of risks and benefits, participants who saw the consequence information leaned more toward benefits than participants who saw the cause information. Notably, the means on this scale were below the midpoint of “equal risks and benefits,” and therefore greater risk than benefit was perceived. There were no other significant effects.
Behavioral intention
COPD.
There was a significant interaction between information type and format, F(1, 1066) = 5.47, p = .02, f = .07. However, none of the pairwise comparisons were significant at p < .008. There were no other significant effects.
Anemia and Lymphoma.
There were no significant effects.
Discussion
We sought to examine whether disease information in DTC prescription drug print ads affects consumer product perceptions and understanding. We investigated the impact of information type; that is, inclusion of cause versus consequence information about the disease. We also investigated the impact of integrating the disease information with the product information in the same ad versus separating it from the product information in two ads presented together. All variations were studied across three medical conditions (COPD, anemia, and lymphoma) and compared to respective control conditions in which no disease information was presented.
Including disease awareness information
Consistent with hypotheses, presenting participants with information about the consequences of the disease promoted false beliefs that the advertised drug prevents these consequences. We also predicted that including disease information would promote higher perceived drug efficacy, lower perceived drug risk, a risk/benefit balance tilted toward benefits, and greater behavioral intentions to seek more information about the product. However, we found varied, and often nonsignificant, outcomes for perceived efficacy, perceived risk, and risk/benefit balance, depending on the experimental conditions examined. Behavioral intentions did not change, regardless of medical condition.
We observed similar trends among participants viewing ads with cause information. As with consequence information, cause information was often assumed to be treated by the drug. For example, in the COPD and anemia conditions, participants who saw cause information incorrectly identified more causes as drug benefits than participants in the respective control conditions. These findings suggest consumers exhibit broad difficulty distinguishing between disease information and product attributes when these elements are presented together.
Integration versus separation
Participants tended to confuse the disease information with the product information most easily when the information was integrated into one ad. As expected, the integrated consequence ads produced the most adverse outcomes overall. Across medical conditions, participants who saw the integrated consequence ads incorrectly identified (recognized) more consequences as drug benefits than did participants who saw the respective control ads. Additionally, participants who saw the COPD and anemia integrated consequence ads incorrectly listed (recalled) more consequences as drug benefits than those who saw the respective control ads.
Separating disease information appears somewhat less problematic than integrating disease information. For anemia, separation resulted in better true benefit recall and recognition compared to integration. For COPD, this strategy resulted in better risk recognition compared to integration. In no comparison did integrating disease information and product information result in better outcomes than separating this information. However, participants who saw the separated consequence ad still confused disease awareness and product information. Compared to the control ad, the separated consequence ad resulted in incorrect consequence recognition in all three medical conditions, and incorrect consequence recall in anemia. This pattern of results suggests that presenting disease awareness information and product information in separate ads side by side is better than integrating this information into the same ad, but still causes confusion.
Limitations
We recognize the limitations of this research. First, participants were recruited from a general population sample, and in most cases did not have the medical condition the drug treated. This sample selection may account for null findings for outcomes such as behavioral intentions. Recruitment of participants with the medical condition advertised would broaden our understanding of how disease information impacts product perceptions and understanding among people who have the condition. Second, specific findings often differed by medical condition. We included three medical conditions to improve generalizability; however, realistic variations in the type and amount of information presented for each medical condition may have differentially affected consumer perceptions and understanding. Third, participants were Internet panelists. Although the panel is constructed to be nationally representative, panelists have agreed in advance to participate in research studies and therefore may be different from individuals who choose not to participate.
Our findings also suggest that explicitly asking whether the drug treats a particular consequence can interfere with consumers’ ability to distinguish between disease information and product information. This outcome may have occurred due to schematic information processing; the consequence-recognition items are consistent with benefits one might expect the drug to treat, and thus it is easy for consumers to inappropriately identify them as drug benefits (Betts & Hinsz, 2013). On the other hand, the open-ended responses show that participants in the integrated ad conditions were more likely to spontaneously recall consequences as product benefits, suggesting that the results cannot be explained away solely as a function of “false memory.”
Implications
This research has implications for policy development. Our results suggest that presenting disease awareness information in a separate ad together with a product information ad is better than integrating the information, but is not sufficient to prevent consumers from confusing disease awareness and product information. Thus, our results lend support to the idea that to avoid confusion, disease information and product information should be distinct in terms of appearance and not conjoined. More extensive separation of information may be required to prevent transference of potential consequences to the product—completely separating the ads in terms of look and proximity, although not examined in this research, may be ideal. Future research should investigate the impact of proximity of disease awareness and product claim materials. The objective of such strategies should be to promote accurate perceptions and understanding about product attributes.
Historically, FDA has supported communication of accurate health messages about diseases and treatments because such communications provide important public health information. This goal remains important, and so pharmaceutical sponsors should exercise care to ensure that drug benefits are appropriately understood and not confused with disease awareness information such as consequences or causes of the disease.
Footnotes
This article reflects the views of the authors and should not be construed to represent FDA’s views or policies.
References
- Aikin K, Swasy J, & Braman A (2004). Patient and Physician Attitudes and Behaviors Associated with Direct to Consumer Promotion of Prescription Drugs: Summary of FDA Survey Research Results. Washington, DC: US Department of Health and Human Services Center for Drug Evaluation and Research. Retrieved November 3, 2014 from http://www.fda.gov/downloads/Drugs/ScienceResearch/ResearchAreas/DrugMarketingAdvertisingandCommunicationsResearch/UCM152860.pdf. [Google Scholar]
- Betts KR, & Hinsz VB (2013). Strong shared representations promote schema-consistent memory errors in groups. Group Processes & Intergroup Relations, 16(6), 734–751. doi: 10.1177/1368430213486206 [DOI] [Google Scholar]
- Brownfield ED, Bernhardt JM, Phan JL, Williams MV, & Parker RM (2004). Direct-to-consumer drug advertisements on network television: an exploration of quantity, frequency, and placement. Journal of Health Communication, 9(6), 491–497. [DOI] [PubMed] [Google Scholar]
- Burke RR, DeSarbo WS, Oliver RL, & Robertson TS (1988). Deception by implication: An experimental investigation. Journal of Consumer Research, 483–494. [Google Scholar]
- Cegedim Strategic Data (2013). 2012 U.S. Pharmaceutical Promotion Spending. http://www.skainfo.com/health_care_market_reports/2012_promotional_spending.pdf: SK&A, A Cegedim Company. [Google Scholar]
- CFR - Code of Federal Regulations Title 21 (2013).
- Deshpande A, Menon A, Perri III M, & Zinkhan G (2004). Direct-to-consumer advertising and its utility in health care decision making: a consumer perspective. Journal of Health Communication, 9(6), 499–513. [DOI] [PubMed] [Google Scholar]
- Dobrow L (2014). DTC report: DTC gets smart. Medical Marketing and Media, April 1, 2014. http://www.mmm-online.com/dtc-report-dtc-gets-smart/article/339357/
- FDA. (2005). Impact of Direct-to-Consumer Drug Advertising on Seniors’ Health and Health Care Costs. Statement of Rachel E. Behrman before the Senate Special Committee on Aging. Retrieved April 21, 2015 from http://www.fda.gov/newsevents/testimony/ucm112706.htm. [Google Scholar]
- FDA. (2010). Novartis Oncology Warning Letter about Gleevec (imatinib mesylate). Retrieved April 27, 2015 from http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/EnforcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalCompanies/ucm259229.htm.
- FDA. (2014). Advertising & Promotional Labeling Questions and Answers. Retrieved May 14, 2015 from http://www.fda.gov/biologicsbloodvaccines/developmentapprovalprocess/advertisinglabelingpromotionalmaterials/ucm117616.htm.
- GfK Custom Research. (2013). KnowledgePanel Design Summary Report. Retrieved from http://www.knowledgenetworks.com/knpanel/docs/knowledgePanel%28R%29-design-summary-description.pdf
- Hall DV, Jones SC, & Hoek J (2011). Direct to consumer advertising versus disease awareness advertising: Consumer perspectives from down under. Journal of Public Affairs, 11(1), 60–69. [Google Scholar]
- Harris RJ (1977). Comprehension of pragmatic implications in advertising. Journal of Applied Psychology, 62(5), 603–608. [Google Scholar]
- Jacoby J, & Hoyer WD (1987). The comprehension and miscomprehension of print communications: an investigation of mass media magazines: Routledge. [Google Scholar]
- Kravitz RL, Epstein RM, Feldman MD, Franz CE, Azari R, Wilkes MS, Hinton L, & Franks P (2005). Influence of patients’ requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. Journal of the American Medical Association, 293(16), 1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee-Wingate SN, & Xie Y (2010). Consumer perceptions of product-claim versus help-seeking direct-to-consumer advertising. International Journal of Pharmaceutical and Healthcare Marketing, 4(3), 232–246. [Google Scholar]
- Lee-Wingate SN, & Xie Y (2013). The influence of the number of presented symptoms in product-claim direct-to-consumer advertising on behavioral intentions. International Journal of Pharmaceutical and Healthcare Marketing, 7(3), 265–284 [Google Scholar]
- Mendonca CM, McCaffrey DJ, Banahan BF, Bentley JP, & Yang Y (2011). Effect of Direct-to-Consumer Drug Advertising Exposure on Information Search. Drug Information Journal, 45(4), 503–515. [Google Scholar]
- Mintzes B (2012). Advertising of prescription-only medicines to the public: does evidence of benefit counterbalance harm? Annual Review of Public Health, 33, 259–277. [DOI] [PubMed] [Google Scholar]
- Palumbo FB, & Mullins CD (2002). The Development of Direct-to-Consumer Prescription Drug Advertising Regulation. Food & Drug Law Journal, 57, 423. [PubMed] [Google Scholar]
- Rollins BL, King K, Zinkhan G, & Perri M (2010). Behavioral intentions and information-seeking behavior: a comparison of nonbranded versus branded direct-to-consumer prescription advertisements. Drug Information Journal, 44(6), 673–683. [Google Scholar]
- Rollins BL, King K, Zinkhan G, & Perri M (2011). Nonbranded or Branded Direct-to-Consumer Prescription Drug Advertising—Which is More Effective? Health Marketing Quarterly, 28(1), 86–98. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Blumenthal D, Silk AJ, Zapert K, Newman M, & Leitman R (2003). Consumers’ reports on the health effects of direct-to-consumer drug advertising. Health Affairs (Project Hope), W3-82-95. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Blumenthal D, Silk AJ, Newman M, Zapert K, Leitman R, & Feibelmann S (2004). Physicians report on patient encounters involving direct-to-consumer advertising. Health Affairs (Project Hope), W4-219-233. [DOI] [PubMed] [Google Scholar]
- Willis GB (2005). Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications. [Google Scholar]


