Abstract
Epidemic-prone diseases have high adverse impacts and pose important threats to global health security. This study aimed to assess levels of health facility preparedness and response to the COVID-19 pandemic in Guinea. This was a cross-sectional study in public and private health facilities/services across 13 Guinean health districts. Managers and healthcare workers (HCWs) from departments in each facility/service were interviewed. Descriptive statistics and comparisons were presented using Pearson’s Chi-Squared Test or Fischer exact test. Totally, 197 managers and 1020 HCWs participated in the study. Guidance documents and dedicated spaces for management/isolation of suspected COVID-19 cases were available only in 29% and 26% of facilities, respectively. Capacities to collect (9%) and safely transport (14%) samples were low. Intensive care units (5%), dedicated patient beds (3%), oxygenators (2%), and respirators (0.6%) were almost lacking. While 36% of facilities/services had received infection prevention and control supplies, only 20% had supplies sufficient for 30 days. Moreover, only 9% of HCWs had received formal training on COVID-19. The main sources of information for HCWs were the media (90%) and the internet (58%). Only 30% of HCWs had received personal protective equipment, more in the public sector (p<0.001) and in Conakry (p=0.022). This study showed low levels of preparedness of health facilities/services in Guinea and highlighted a lack of confidence among HCWs who felt unsafe at their workplace. Better governance to improve and maintain the capacity of the Guinean health system to respond to current and future epidemics is needed.
Key words: COVID-19, health system, preparedness, Guinea, Sub-Saharan Africa
Introduction
Epidemic-prone diseases, especially emerging and re-emerging ones, have high adverse impacts and pose important threats to global health security and the Universal Health Coverage agenda.1,2 On the 15th of May, 2020, the COVID-19 pandemic caused by the novel coronavirus (2019- nCoV), SARS-CoV-2, had 4.3 million confirmed cases in 213 countries with over 294,000 deaths (6.9%).3 Developing countries are particularly impacted given the weaknesses of health systems, poor sanitary and hygiene conditions, and cultural habits.4 In sub-Saharan Africa, community transmission has been contributing to the spread of COVID-19 with a high reproductive number.5
The World Health Organization (WHO) has warned that only strengthened health systems will be able to break chains of community transmission while ensuring the continuity of care for essential services.6 Moreover, in its 2019-nCoV Strategic Preparedness and Response Plan, the WHO has stated that national health systems should have capacities for early detection of suspected cases, rapid sample collection and testing, isolation of all confirmed cases, and quarantine for all close contacts.7
In countries such as Guinea, which experienced the worst-ever Ebola Virus Disease (EVD) outbreak in 2014–2016, development partners such as the World Bank implemented health system-strengthening programmes.8 These initiatives are aimed at increasing local capacities for outbreak preparedness and response through improving human resources for health, infrastructures, finances, and governance pillars of the health system.8-10 Moreover, it stimulated regional and international collaboration for outbreak surveillance, information, communication, and exchange of knowledge.8
In Guinea, this resulted in: i) the establishment of a laboratory network for infectious diseases surveillance and a national agency for health security, coordinating 8 regional and 33 district teams to manage alerts and response to epidemics, ii) the enhancement of community-based surveillance system, iii) the recruitment and deployment of 5,000 health workers in rural areas and health programmes, iv) the building of 33 district-level centres for epidemic treatment and prevention, v) the rehabilitation of several health facilities including the Donka National Hospital, and vi) an increase in the health sector budget from 4% in 2014 to 8% in 2017.11,12
However, since the onset of the COVID-19 pandemic in Guinea, there has been a rapid increase in the incidence and spread of the disease in Conakry and its neighbouring health districts, with many cases originating from community transmission. On the 15th of May, 2020, Guinea had 2,372 confirmed cases, 11 times the numbers in Liberia, and 6 times those of Sierra Leone, the other countries that also experienced the 2014–2016 EVD outbreak.3 This raises questions such as: is the surveillance system in Guinea functioning well and is the health system well prepared to respond to this new challenge posed by COVID-19?
This study aimed to assess the levels of health facility preparedness and response in Guinea to the COVID-19 pandemic.
Materials and methods
Study design
This was a national cross-sectional study using a standard questionnaire.
Setting
This study was conducted in 13 health districts across Guinea, including the 5 urban health districts in the capital, Conakry (Figure 1). Guinea was the epicentre of the 2014–2016 EVD outbreak and its health system is classified among the fragile ones.4 It has an estimated 12.5 million inhabitants, 55% of whom live below the poverty line.13 Of the 38 health districts (Including five in the capital city Conakry) forming the national health system, only those in Conakry had registered clusters of cases with 194 confirmed cases and no deaths at the study start date (April the 10th, 2020).14
Study population
The study population included facility/service managers and healthcare workers (HCWs) from the public and private health sectors, general public, and other actors of the health sector.
Sampling
The 13 health districts included in this study were purposely selected. The selection criteria included were being an important point of connection in the country’s trading network, an active and crowded mining locality, or an entry point from already affected countries. We assumed that the risk of COVID-19 spread would be higher along major mobility axes. In each district, a random sampling of public and private health facilities/services in urban communes was carried out based on a list provided by the Ministry of Health. Within the health facilities, all departments were visited and five to ten managers and HCWs were interviewed.
Study variables
Data variables included selected characteristics of managers and HCWs: locality (Conakry or countryside), gender (male or female), age (in years), duration of professional experience (in years), occupation (nurse/midwife, medical doctor, health technician, student/intern, laboratory staff, or other staff), type of facility/service (health centre, hospital, or management service), and facility unit (e.g., Maternity or Surgery). Variables related to the local environment (e.g. facility) preparedness included: received infection prevention and control (IPC) supplies, duration of supplies being sufficient, the existence of handwashing devices at facility/service entry, water supply, or availability of an Epidemic Response Task Force.
Variables related to facility-level capacities to detect, isolate, refer, and manage suspected COVID-19 cases included: received guidance or instructions related to COVID-19, triage system at facility entrance, training of HCWs, the main source of information, needs for training and priority areas, sample collection protocol and capacity, space to manage suspected cases, equipment, tracing and notification system, transportation capacity, quarantine/isolation capacity, and availability of Integrated Disease Surveillance and Response (IDSR) Technical Guidelines. The HCW-level variables included: feelings of whether concerns are being addressed, feelings of full protection at the workplace, and knowledge about what to do with a suspected case.
Data collection
Data were collected using a standardized, semi-structured questionnaire whose development was guided by the WHO 2019-nCoV Strategic Preparedness and Response Plan.7 Second-year masters in Public Health students and research assistants who received a four-day training on the study protocol and data collection tools, including one day of field testing, administered the questionnaire. An electronic version of the questionnaire was also emailed to the managers of each district using the Ministry of Health’s address repository. The final questionnaire was created in Kobo toolbox software and loaded on Android tablets.
Figure 1.
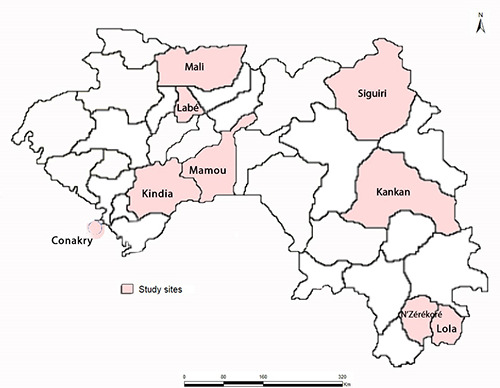
Study sites across Guinea.
Data analysis
Data were exported from the Kobo platform as an MS-Excel file and imported for analysis into Stata 15 Software (Stata Corporation, College Station, TX, USA). Descriptive statistics (proportions and means with standard deviations) were presented for each sub-sample (Managers and HCWs). These proportions were then compared according to the two survey localities (Conakry and countryside) and by health sector (public and private) using the Pearson’s Chi-squared test or the Fischer exact test when applicable with a significance level set at p<0.05.
Results
Facility and service managers
Of the 210 Managers contacted, 197 (94%) participated in the study. Their mean age was 50 years (Standard Deviation, SD=±11 years). A total of 60% of them lived in the countryside, 73% were males, and 80% were from the public health sector (Table 1).
Totally, 77% of the Managers reported that their facility or service had received guidance or instructions related to the prevention and management of COVID-19 from authorities (Table 2). This proportion was lower in the private sector compared to the public sector (p<0.001), and in Conakry compared to the countryside (p=0.006).
Handwashing devices at the facility/service entrances and water supply were available in about 96% and 88% of the facilities/ services respectively. Approximately 36% of the managers said that their facility/ service had received IPC supplies in the preceding 3 months and only 20% reported that the supplies received would be sufficient for the next 30 days. Conakry had received more supplies than the countryside (p<0.001).
Less than half of the facilities/services had an established COVID-19 task force in which religious (26%) and community (35%) leaders were underrepresented.
Only 24% of the Managers said that HCWs in their facilities/services had received training on COVID-19 prevention and diagnosis.
We also examined facility-level capacities to detect, isolate, refer, and manage suspected COVID-19 cases (Table 2). We found that 63% of the facilities had a screening system at the entrance. However, the overall capacity to collect (9%) and safely transport (16%) samples of suspected cases was limited. In addition, only 26% of the facilities had a dedicated space to manage suspected COVID-19 cases, while intensive care units (5%), COVID-19 dedicated beds (3%), oxygenators (2%), and respirators (0.6%) were almost lacking.
Table 1.
Selected characteristics of Facility/service Managers (n=197) and Health Care Workers (n=1020) from 13 health districts in Guinea, April 2020.
| Characteristics | Managers | Health Care Workers | ||
|---|---|---|---|---|
| (n=197) | (n=1020) | |||
| N | % | N | % | |
| Locality | ||||
| Conakry | 79 | 40.0 | 445 | 43.6 |
| Countryside | 118 | 60.0 | 575 | 56.4 |
| Respondent gender | ||||
| Female | 54 | 27.4 | 523 | 51.3 |
| Male | 143 | 72.6 | 497 | 48.7 |
| Age (years; mean±SD) | 49.6±10.9 | 35.1±9.3 | 374 | 36.7 |
| Duration of professional experience (years; mean±SD) | - | 8.0±0.4 | 269 | 26.4 |
| Respondent occupation | ||||
| Nurse/Midwife | - | - | 127 | 12.4 |
| Medical doctor | - | - | 111 | 10.9 |
| Health technician | - | - | 92 | 9.0 |
| Student/Intern | - | - | 47 | 4.6 |
| Laboratory staff | - | - | 323 | 31.7 |
| Other staff* | - | - | 568 | 55.7 |
| Type of facility | ||||
| Health centre | 49 | 24.9 | 129 | 12.6 |
| Hospitals | 81 | 41.1 | - | - |
| Clinics | 39 | 19.8 | 865 | 84.8 |
| Management services | 28 | 14.2 | 155 | 15.2 |
| Health sector | ||||
| Public | 158 | 80.2 | 270 | 26.5 |
| Private | 39 | 19.8 | 186 | 18.2 |
| Facility unit | ||||
| General medicine | - | - | 121 | 11.9 |
| Primary care | - | - | 96 | 9.4 |
| Maternity | - | - | 95 | 9.3 |
| Paediatrics | - | - | 94 | 9.2 |
| Other units** | - | - | 90 | 8.8 |
| Laboratory | - | - | 68 | 6.7 |
| Emergency | - | - | 165 | 16.2 |
| Surgery | - | - | ||
| Respondent’s facility/service reported Ebola cases in 2014-2016 (Yes) | - | - | ||
*Pharmacists, Dentists, and Hygienists
**Pharmacy, Dentistry, Triage, and Nutrition.
Few facilities (38%) had tracing and notification systems in place for suspected cases, and only about 26% had an adequate and functional transportation system for referring such cases. These proportions were lower in the private health sector (p=0.031 and p=0.013 respectively) and in the countryside (p=0.016 and p=0.002 respectively). Overall, the availability of a guidance document for the management and quarantine of suspected COVID-19 cases (29%), and a protocol for sample collection and transportation (14%) were low. The latter was missing in all private facilities (p=0.005).
Healthcare workers
A total of 1020 HCWs out of 1074 contacted (95%) responded to the survey. Their mean age was 35 years (SD=±9 years). A total of 56% of them resided outside Conakry, 51% were females, and 85% were from the public health sector (Table 1).
Overall, 76% of the HCWs said they had received guidance or instructions related to COVID-19 prevention and management from the authorities. However, only 26% (31% in the countryside, p<0.001) knew about the IDSR Technical Guidelines, and only 28% of the facilities/services had a copy of the latest version (Table 3).
The main sources of information for HCWs were the media (90% overall; 92% in the countryside, p=0.027) and the internet (58% overall; 71% in the private sector, p<0.001). However, more HCWs from the private sector had received information from their peers (p=0.001).
Only 16% of HCWs had received orientation and training on IPC in the preceding 3 months and 9% had received formal training on COVID-19 prevention and management, irrespective of the health sector or the locality. Only half the HCWs provided a correct definition of a suspected COVID-19 case with more correct answers from HCWs in the private sector (p=0.010) and Conakry (p=0.017). About 30% of the HCWs had received Personal Protective Equipment (PPE) during the preceding 3 months, more in the public sector (p<0.001) and in Conakry (p=0.022).
Table 2.
Levels of COVID-19 preparedness by Health Sector and Locality according to Facility/Services Managers in 13 health districts in Guinea, April 2020 (n=197).
| Variables | Health Sector | Locality* | |||||
|---|---|---|---|---|---|---|---|
| Total | Public | Private | p-value | Conakry | Countryside | p-value | |
| N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Facility/service preparedness to face the COVID-19 pandemic | n=197 | n=158 | n=39 | n=79 | n=118 | ||
| Facility/service has received guidance or instructions related | 152 (77.2) | 135 (85.4) | 17 (43.6) | <0.001 | 53 (67.1) | 99 (83.9) | 0.006 |
| to COVID-19 prevention and management from authorities (Yes) | |||||||
| Facility/service is implementing these guidelines (Yes) (n=152) | 147 (96.7) | 131 (97.0) | 16 (94.1) | 0.525 | 50 (94.3) | 97 (98.0) | 0.230 |
| HCWs know about IDSR Technical Guidelines (Yes) | 80 (40.6) | 65 (41.1) | 15 (38.5) | 0.760 | 27 (34.2) | 53 (44.9) | 0.133 |
| Latest version of IDSR Technical Guidelines available | 33 (41.3) | 28 (43.1) | 5 (33.3) | 0.490 | 10 (37.0) | 23 (43.4) | 0.585 |
| at facility/service (Yes) (n=80) | |||||||
| Facility/service has handwashing device at facility entrance (Yes) | 192 (97.5) | 154 (97.5) | 38 (97.4) | 0.991 | 78 (98.7) | 114 (96.6) | 0.353 |
| Facility/service has water supply (Yes) | 177 (89.9) | 139 (88.0) | 38 (97.4) | 0.080 | 72 (91.1) | 105 (89.0) | 0.623 |
| Facility/service has received IPC supplies in the preceding | 71 (36.0) | 62 (39.2) | 9 (23.1) | 0.060 | 43 (54.4) | 28 (23.7) | <0.001 |
| 3 months (Yes) | |||||||
| The IPC supplies received sufficient for the next 30 days (Yes) (n=71) | 14 (19.7) | 11 (17.7) | 3 (33.3) | 0.272 | 9 (20.9) | 5 (17.9) | 0.750 |
| Facility/service has an established COVID-19 task force (Yes) | 82 (41.6) | 77 (48.7) | 5 (12.8) | <0.001 | 31 (39.2) | 51 (43.2) | 0.579 |
| The COVID-19 Task Force involves (n=82): | |||||||
| Religious leaders (Yes) | 21 (25.6) | 21 (27.3) | 0 (0.0) | 0.176 | 4 (12.9) | 17 (33.3) | 0.040 |
| Authorities (Yes) | 34 (41.5) | 31 (39.2) | 3 (42.8) | 0.427 | 9 (29.0) | 25 (49.0) | 0.075 |
| Representatives of NGOs (Yes) | 22 (26.8) | 22 (28.6) | 0 (0.0) | 0.162 | 4 (12.9) | 18 (35.3) | 0.026 |
| Community leaders (Yes) | 29 (35.4) | 29 (37.7) | 0 (0.0) | 0.088 | 8 (25.8) | 21 (41.2) | 0.158 |
| HCWs trained to prevent and diagnose COVID-19 (Yes) | 47 (23.9) | 41 (25.9) | 6 (15.4) | 0.166 | 16 (20.3) | 31 (26.3) | 0.331 |
| Facility-level capacities to detect, isolate, refer, and manage | |||||||
| Triage system at entrance to detect suspected cases (Yes) | 125 (63.4) | 104 (65.8) | 21 (53.8) | 0.164 | 51 (64.6) | 74 (62.7) | 0.792 |
| COVID-19 sample collection capacity available (Yes) | 17 (8.6) | 17 (10.8) | 0 (0.0) | 0.032 | 10 (12.7) | 7 (5.9) | 0.099 |
| Capacity to transport samples of suspected COVID-19 cases (Yes) | 31 (15.7) | 29 (18.3) | 2 (5.1) | 0.042 | 10 (12.7) | 21 (17.8) | 0.332 |
| Dedicated space to manage suspected COVID-19 case (Yes) | 52 (26.4) | 45 (28.5) | 7 (18.0) | 19 (24.1) | 33 (28.0) | 0.541 | |
| Equipment to manage suspected COVID-19 cases available (n=169) | 0.181 | ||||||
| Resuscitation unit (Yes) | 9 (5.3) | 5 (3.8) | 4 (10.3) | 0.118 | 6 (8.3) | 3 (3.1) | 0.134 |
| COVID-19 dedicated beds (Yes) | 5 (3.0) | 4 (3.1) | 1 (2.6) | 0.868 | 4 (5.6) | 1 (1.0) | 0.086 |
| Oxygenators with supplies (Yes) | 3 (1.8) | 2 (1.5) | 1 (2.6) | 0.671 | 3 (4.2) | 0 (0.0) | 0.043 |
| Respirators (Yes) | 1 (0.6) | 1 (0.8) | 0 (0.0) | 0.583 | 1 (1.4) | 0 (0.0) | 0.244 |
| Availability of tracing and notification system for suspected COVID-19 | 75 (38.1) | 66 (41.8) | 9 (23.1) | 22 (27.9) | 53 (44.9) | 0.016 | |
| cases at facility/district-level (Yes) | 0.031 | ||||||
| Availability of adequate and functioning transportation mean | 51 (25.9) | 47 (29.8) | 4 (10.3) | 11 (13.9) | 40 (33.9) | 0.002 | |
| for referral of suspected COVID-19 cases (Yes) | 0.013 | ||||||
| Availability of sample collection and transportation protocol | 28 (14.2) | 28 (17.7) | 0 (0.0) | 11 (13.9) | 17 (14.4) | 0.924 | |
| for suspected COVID-19 cases (Yes) | 0.005 | ||||||
| Availability of guidance document for management of suspected | 58 (29.4) | 46 (29.1) | 12 (30.8) | 0.839 | 22 (27.9) | 36 (30.5) | 0.688 |
| COVID-19 cases and quarantine/isolation (Yes) | |||||||
*Conakry was the epicentre of the pandemic at the time of the survey (more than 98% of confirmed cases).
Seventy percent of all HCWs knew what to do in the face of a suspected COVID-19 case, with the private sector and Conakry performing better (p<0.001). Only 41% of the HCWs felt their concerns about COVID-19 were being somehow fully addressed by their facility/service. Those in Conakry had more concerns compared to those from the countryside (p=0.005). Additionally, only 26% of the HCWs felt they were sufficiently protected against COVID-19 at their workplace (less in the public sector, p<0.001). Almost all HCWs (97%) expressed the need for additional information/training on COVID-19 (more in the countryside, p<0.001). The priority areas for such information/training included IPC measures (53%), COVID-19 case management (29%), and all aspects of pandemic control (18%), with more needs expressed by HCWs in the countryside compared to Conakry (p<0.001).
Totally, 94% of the HCWs said that their facilities/services had water supply along with handwashing devices at the facility/service entrance (88%). About 58% had a functioning flashing thermometer in their facility/service and 53% said that hydroalcoholic solution was available in examination rooms. These proportions were all higher in the private sector (p<0.001). Communication materials on COVID-19 prevention measures (flyers, posters, etc.) were available in 39% of all facilities/services. More communication materials were available in Conakry than in the countryside (p<0.001). Overall, only about 26% of the facilities had a dedicated space for quarantine/ isolation of suspected COVID-19 cases, more in the public sector (p=0.002). Furthermore, only 7% of the facilities had equipment and supplies to test for COVID- 19 with testing capacities for COVID-19, higher in Conakry compared to the countryside (p<0.001).
Table 3.
Levels of COVID-19 preparedness according to Health Care Workers in 13 Health Districts in Guinea, April 2020 (n=1020).
| Variables | Health Sector | Locality* | |||||
|---|---|---|---|---|---|---|---|
| Total | Public | Private | p-value | Conakry | Countryside | p-value | |
| N (%) | N (%) | N (%) | N (%) | N (%) | |||
| HCW-level preparedness | n=1020 | n=865 | n=155 | n=445 | n=575 | ||
| HCW has received guidance or instructions related to COVID-19 | 778 (76.3) | 661 (76.4) | 117 (75.5) | 0.802 | 331 (74.4) | 447 (77.7) | 0.211 |
| prevention and management from authorities (Yes) | |||||||
| HCW knows about IDSR Technical Guidelines (Yes) | 268 (26.3) | 226 (26.1) | 42 (27.1) | 92 (20.4) | 177 (30.8) | <0.001 | |
| Main source of information on COVID-19 | |||||||
| Media | 918 (90.0) | 781 (90.3) | 137 (88.4) | 390 (87.6) | 528 (91.8) | 0.027 | |
| Internet | 594 (58.2) | 484 (55.9) | 110 (71.0) | 256 (57.5) | 338 (58.8) | 0.687 | |
| Health authorities | 455 (44.6) | 395 (45.7) | 60 (38.7) | 189 (42.5) | 266 (46.3) | 0.227 | |
| Health professionals (peers) | 257 (25.2) | 202 (23.4) | 55 (35.5) | 116 (26.1) | 141 (24.5) | 0.573 | |
| Has received orientation/training in the preceding 3 months on IPC (Yes) | 160 (15.7) | 27 (17.4) | 133 (15.4) | 73 (16.4) | 87 (15.1) | 0.579 | |
| Has received formal training on prevention and management | 90 (8.8) | 79 (9.1) | 11 (7.1) | 32 (7.2) | 58 (10.1) | 0.106 | |
| of COVID-19 (Yes) | |||||||
| Provide a correct definition of suspected COVID-19 case (Yes) | 555 (54.4) | 456 (52.7) | 99 (63.9) | 261 (58.6) | 294 (51.1) | 0.017 | |
| Has received PPE during the preceding 3 months (Yes) | 299 (29.3) | 275 (31.8) | 24 (15.5) | 147 (33.0) | 152 (26.4) | 0.022 | |
| HCW knows what to do in front of a suspected COVID-19 case (Yes) | 743 (72.8) | 609 (70.4) | 134 (86.4) | 352 (79.1) | 391 (68.0) | <0.001 | |
| HCW feels his/her concerns about COVID-19 are being addressed | 415 (40.7) | 342 (39.5) | 73 (47.1) | 159 (35.7) | 256 (44.5) | 0.005 | |
| by the facility/service (Somehow to fully) (Yes) | |||||||
| HCW feels sufficiently protected against COVID-19 | 266 (26.1) | 203 (23.5) | 63 (40.6) | 114 (25.6) | 152 (26.4) | 0.768 | |
| at his/her workplace (Yes) | |||||||
| Needs additional information/training on COVID-19 (Yes) | 991 (97.2) | 842 (97.3) | 149 (96.1) | 420 (94.4) | 571 (99.3) | <0.001 | |
| Areas in which information/training is most needed | |||||||
| IPC measures | 520 (53.1) | 444 (53.4) | 76 (51.0) | 200 (48.6) | 320 (56.2) | ||
| Management* | 287 (29.3) | 249 (30.0) | 38 (25.5) | 110 (26.8) | 177 (31.1) | <0.001 | |
| All aspects of COVID-19 control** | 173 (17.6) | 138 (16.6) | 35 (23.5) | 101 (24.6) | 72 (12.7) | ||
| Facility-level preparedness | |||||||
| Facility/service has water supply (Yes) | 955 (93.6) | 810 (93.6) | 145 (93.5) | 419 (94.2) | 536 (93.2) | 0.542 | |
| Availability of handwashing device at facility/service entrance (Yes) | 902 (88.4) | 752 (86.9) | 150 (96.8) | 400 (89.9) | 502 (87.3) | 0.201 | |
| Availability of functioning flashing Thermometer (Yes) | 587 (57.6) | 462 (53.4) | 125 (80.7) | 323 (72.6) | 264 (45.9) | <0.001 | |
| Availability of hydroalcoholic solution in examination rooms (Yes) | 544 (53.3) | 436 (50.4) | 108 (69.7) | 276 (62.0) | 268 (46.6) | <0.001 | |
| Availability of IPC material (flyers, posters, etc.) on COVID-19 prevention measures (Yes) | 402 (39.4) | 344 (39.8) | 58 (37.4) | 252 (56.6) | 150 (26.1) | <0.001 | |
| Availability of the latest version of IDSR Technical Guidelines at facility/service (Yes) (n=268) | 74 (27.6) | 64 (28.3) | 10 (23.8) | 28 (30.8) | 46 (26.0) | 0.407 | |
| Availability of a dedicated space for quarantine/isolation of suspected COVID-19 cases (Yes) | 261 (25.6) | 237 (27.4) | 24 (15.5) | 111 (24.9) | 150 (26.1) | 0.678 | |
*Diagnosis and treatment
**Epidemiology, prevention, management, and surveillance.
Discussion
To our knowledge, this is one of the first studies in West Africa to systematically assess the levels of health-system preparedness to the COVID-19 pandemic. It revealed that the levels of preparedness of the Guinean health system were low. In addition, disparities existed according to the health sector (public versus private) and the locality (Conakry versus the countryside). Finally, it showed that HCWs felt unsafe at their workplace. These findings raise a number of concerns that merit further attention.
First, several factors that may explain the low levels of preparedness in Guinea include: i) the lack of a clear protocol and skills to screen, quickly detect, and isolate suspected COVID-19 cases, ii) an inadequate capacity to collect samples and test for COVID-19 (or at least, transport samples), and iii) an inadequate capacity to implement quarantine and disease surveillance around clusters of cases. At the time of the survey, of the four laboratories in Guinea that were conducting about 400 COVID-19 tests totally, three were located in Conakry. This situation has resulted in failures in the national response; dozens of COVID-19 confirmed cases (more than 100) were consistently reported lost to follow- up by the National Sanitarian Security Agency (ANSS), the body coordinating the national COVID-19 response.15 The levels of some key indicators were far below the thresholds suggested by the WHO.7 For instance, healthcare facilities with triage capacity and those with isolation capacity should be at least 80% as per the WHO guidelines, but they were 63% and 26%, respectively, in this study (according to managers and HCWs ). These findings are also in line with previous reports that public health systems of most countries in sub- Saharan Africa are highly vulnerable.16-20 Nonetheless, with all the investments provided by development partners following the EVD outbreak to strengthen Guinea’s health system and make it more resilient, one would have expected a better preparedness level than what we observed.8,11,12 To understand these findings, realistically evaluating the current aid strategies along with contexts of governance and coordination mechanisms and defining a new health system- strengthening approach are needed.21
Second, despite these low levels of preparedness, disparities between the public and private health sectors and between Conakry (the epicentre of the pandemic at the time of the survey) and the countryside were observed. A similar finding from Italy has reported disparities between Northern and Southern regions.22 Our results showed that Conakry and the public health sector had better levels of preparedness, perhaps since efforts by the government and development partners to slow/stop disease progression were focused in Conakry. Added to that are the disparities that existed long before the pandemic, and the situation observed just reflects the perpetuation of a tendency to ignore or systematically exclude the private health sector from Government initiatives. However, given the context, we found it paradoxical that the private sector performed better for indicators such as case definitions, availability of handwashing devices at facility entrances, functioning flashing thermometers, or availability of hydroalcoholic solution. One might posit that formal private facilities have allocated more resources to protect their staff and reassure clients. Besides, contrary to the EVD outbreak where development partners were fully mobilised, this time, their funding, including the required equipment and inputs, has been mostly directed to their own health systems, heavily submerged by the pandemic.
In this context, and given the porosity of the lockdown measures implemented in Conakry, any spread of the disease in the countryside might represent an additional huge threat to the already fragile health system. 4
Third, the HCWs were not confident about their safety at the workplace, regardless of the location (Conakry or countryside) or the health sector (public or private). The concerns raised by the HCWs are legitimate, considering our findings and other studies that have reported prolonged contact with patients, not wearing face masks, and medical procedures that generate aerosols are highly associated with COVID-19 infection among HCWs.23,24 Additionally, there have been clusters of transmission in health facilities with many HCWs infected worldwide, contributing to reluctance by patients to seek care (whether for COVID- 19 or other diseases).25 This recalls the situation during the EVD outbreak where 115 HCWs died of the disease due to high exposure and weak IPC measures in health facilities. 26,27 More concerning is the risk of HCWs getting their information primarily through the media and the internet, given the amount of misinformation and fake news that are circulating, referred to as “infodemics”. If the feeling of being unsafe persists among HCWs, while the pandemic continues to spread across Guinea as reflected by the current trend,28 there is a risk of desertion of health facilities by HCWs. This in turn will jeopardise the continuity of care for essential services such as maternal and child health care, as was observed during the EVD outbreak in West Africa and now during the COVID-19 pandemic. 29-31
Creating an enabling working environment for HCWs irrespective of their location and health sector is needed. This can be achieved through sufficient provision of personal protective equipment, appropriate training and orientation on protocols, and providing guidelines for proper prevention and management of COVID-19 in facilities and services.17,19,23
The main limitations of this study were inherent to the transversal study design that does not allow the exploration of direct causality and is prone to information and social desirability biases. In addition, the study was conducted in an emergency situation that limited movement and might have engendered mistrust towards data collectors coming from the epicentre of the pandemic.32 Despite these limitations, this study has several strengths, including the fact that data were collected from 13 Health Districts representing the most important localities in terms of trade and mining activities, along with vulnerability to affected neighbouring countries. Additionally, it covered 32% of all facilities/services composing the national health system and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline.33
Conclusions
This study showed low levels of preparedness of health facilities and services in Guinea along with disparities by health sector and location and revealed a lack of confidence among HCWs who felt unsafe at their workplace. These findings call for more domestic funding and better governance to improve and maintain the capacity of the Guinean health system to respond to current and future epidemics. In addition, the private health sector should be better engaged in the pandemic response and benefit from public and donor-driven support as well.
Acknowledgements
We thank all our study sites’ managers for their kind collaboration and for facilitating the data collection, as well as study participants for accepting to respond to our questionnaire. We are also grateful to the data collectors for their involvement during the data collection process.
Funding Statement
Funding: The Belgian Development Agency (Enabel) funded the study (agreement number GIN1701311- AP001). The Belgian Directorate of Development Cooperation through the Framework Agreement Four (FA4) provided additional funding, via a Scientific Collaboration between the Institute of Tropical Medicine of Antwerp and the Maferinyah National Training and Research Centre in Rural Health (CNFRSR). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Heymann DL, Chen L, Takemi K, et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet 2015;385:1884-1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature 2008;451:990-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus disease 2019 (COVID-19) - Situation Report – 115; 2020 May 14 [cited 2020 May 24]. Available from: https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200514-covid-19-sitrep-115.pdf?sfvrsn=3fce8d3c_6. [Google Scholar]
- 4.Global Preparedness Monitoring Board. A world at risk: annual report on global preparedness for health emergencies. Geneva. World Health Organization; Licence: CC BY-NC-SA 3.0 IGO. Available from: https://apps.who.int/gpmb/assets/annual_report/GPMB_annualreport_2019.pdf. [Google Scholar]
- 5.Choi S, Ki M. Estimating the reproductive number and the outbreak size of COVID-19 in Korea. Epidemiol Health 2020:e2020011-2020010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Strengthening the health system response to COVID-19: Recommendations for the WHO European Region - Policy brief (2020 April 1) [cited 2020 May 24]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0003/436350/strengthening-health-system-response-COVID-19.pdf?ua=1. [Google Scholar]
- 7.World Health Organization. Novel Coronavirus (2019-nCoV): Strategic Preparedness and Response Plan (2020 February) [cited 24 May 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdf?ua=1. [Google Scholar]
- 8.Govindaraj R, Herbst CH, Ajumobi OB, et al. Strengthening Post-Ebola Health Systems: From Response to Resilience in Guinea, Liberia, and Sierra Leone. World Bank Group, Washington, D.C [cited 2020 May 24]. Available from: http://documents.worldbank.org/curated/en/707921513841518782/Strengthening-Post-Ebola-Health-Systems-From-Response-to-Resilience-in-Guinea-Liberia-and-Sierra-Leone. [Google Scholar]
- 9.Jamieson D, Kellerman SE. The 90 90 90 strategy to end the HIV Pandemic by 2030: Can the supply chain handle it? J Int AIDS Soc 2016;19:20917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shoman H, Karafillakis E, Rawaf S. The link between the West African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: a systematic review. Global Health 2017;13:1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delamou A, Delvaux T, El Ayadi AM, et al. Public health impact of the 2014-2015 Ebola outbreak in West Africa: seizing opportunities for the future. BMJ Glob Health 2017:e000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolie D, Delamou A, van de Pas R, et al. 'Never let a crisis go to waste': post- Ebola agenda-setting for health system strengthening in Guinea. BMJ Glob Health 2019;4:e001925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institut National de la Statistique (INS). Ministère du Plan et de la Coopération Internationale. Annuaire statistique 2018 [cited 2020 May 24]. Available from: http://www.statguinee.org/images/Publications/INS/annuelles/Annuaire_INS_2018-VF5.pdf(French). [Google Scholar]
- 14.World Health Organization. Coronavirus disease 2019 (COVID-19) - Situation Report – 81; 2020 April 10 [cited 2020 May 24]. Available from: https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200410-sitrep-81-covid-19.pdf?sfvrsn=ca96eb84_2. [Google Scholar]
- 15.Valade C. En Guinée, l’effet révélateur du coronavirus. rfi. (2020 May 3) [cited 2020 May 24]. Available from: http://www.rfi.fr/fr/afrique/20200503-en-guin%C3%A9e-l-effet-r%C3%A9v%C3%A9lateur-coronavirus(French). [Google Scholar]
- 16.Christopher DJ, Isaac BT, Rupali P, Thangakunam B. Health-care preparedness and health-care worker protection in COVID-19 pandemic. Lung India 2020;37:238-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilbert M, Pullano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet 2020;395:871-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanwar A, Heppler S, Kanwar K, Brown C. A Survey of SARS-CoV-2 Preparedness Among Hospitals in Idaho. Infect Control Hosp Epidemiol 2020;41:1003-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucero-Prisno DE, Adebisi YA, Lin X. Current efforts and challenges facing responses to 2019-nCoV in Africa. Glob Health Res Policy 2020;5:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suleiman A, Bsisu I, Guzu H, et al. Preparedness of Frontline Doctors in Jordan Healthcare Facilities to COVID- 19 Outbreak. Int J Environ Res Public Health 2020;17:3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanefeld J, Mayhew S, Legido-Quigley H, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan 2018;33:1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carinci F. Covid-19: preparedness, decentralisation, and the hunt for patient zero. BMJ 2020;368:799. [DOI] [PubMed] [Google Scholar]
- 23.Canova V, Lederer Schlapfer H, Piso RJ, et al. Transmission risk of SARSCoV- 2 to healthcare workers -observational results of a primary care hospital contact tracing. Swiss Med Wkly 2020;150:w20257. [DOI] [PubMed] [Google Scholar]
- 24.Heinzerling A, Stuckey MJ, Scheuer T, et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient - Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep 2020;69:472-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC, COVID-19 Response Team. Characteristics of Health Care Personnel with COVID-19 - United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:477-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delamou A, Beavogui AH, Konde MK, et al. Ebola: better protection needed for Guinean health-care workers. Lancet 2015;385:503-504. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. Ebola situation report (2015 May 20) [cited 2020 May 24]. Available from: https://apps.who.int/iris/bitstream/handle/10665/171812/roadmapsitrep_20May15_eng.pdf?sequence=1. [Google Scholar]
- 28.World Health Organization. Coronavirus disease 2019 (COVID-19) - Situation Report – 122; 2020 May 21 [cited 2020 May 24]. Available from: https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200521-covid-19-sitrep-122.pdf?sfvrsn=24f20e05_4. [Google Scholar]
- 29.Delamou A, Ayadi AME, Sidibe S, et al. Effect of Ebola virus disease on maternal and child health services in Guinea: a retrospective observational cohort study. Lancet Glob Health 2017;5:e448-e457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leno NN, Delamou A, Koita Y, et al. Ebola virus disease outbreak in Guinea: what effects on prevention of motherto- child transmission of HIV services? Reprod Health 2018;15:60-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Semaan AT, Audet C, Huysmans E, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. medRxiv 2020:20093393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoechner H. In northern Nigeria, distrust jeopardises the response to coronavirus. The Conversation (2020 April 15) [cited 2020 May 24]. Available from: https://theconversation.com/innorthern-nigeria-distrust-jeopardisesthe-response-to-coronavirus-135347. [Google Scholar]
- 33.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-1499. [DOI] [PubMed] [Google Scholar]


