Abstract
Purpose:
To report the prevalence, clinical profile, investigations, and visual outcomes of sarcoid intermediate uveitis in a tertiary eye care center in South India.
Methods:
Retrospective, observational case series. Records of 29 patients with sarcoid intermediate uveitis were retrieved. Complete ophthalmic evaluation and systemic examination by a pulmonologist with appropriate laboratory investigations were done. Results were analyzed using SPSS software.
Results:
Mean age group was 42.14 ± 11.31 years. The bilateral presentation was more common and females were more affected than males. Anterior chamber cells and flares in 22.4% of cases (N = 11 eyes), posterior synechiae in 20.4% (N = 10 eyes), and both small and mutton fat keratic precipitates in 14.2% of cases (N = 7 eyes) were noted; only one eye had Busacca nodules similar to other granulomatous uveitis. Cystoid macular edemas were present in three eyes. Treatment with oral steroids and systemic immunosuppression resulted in good visual recovery. The mean presenting visual acuity in right and left eye were 0.2 and 0.3, respectively. The mean final visual acuity in right and left eye was 0.1 and 0.3, respectively.
Conclusion:
Sarcoid intermediate uveitis is quite common in a tuberculosis endemic country like India. A complete review of systems with appropriate investigations is essential to prevent visual complications.
Keywords: High resolution computed tomography of chest, intermediate uveitis, sarcoid, serum angiotensin converting enzyme, snowball exudates
Sarcoidosis is a chronic multisystem granulomatous disorder as a result of an exaggerated cellular immune response to a variety of self- and non-self-antigens in a genetically predisposed individual.[1,2] Diagnosis is made based on the combination of typical clinical features and positive chest X-ray, HRCT chest or biopsy of affected tissue after ruling out conditions that can mimic clinical, radiological, and pathological changes.[1,2] Sarcoidosis has been reported in various series of uveitis.[3,4,5] However, it is now properly diagnosed due to the awareness of the disease and availability of newer investigation modalities.[3,4,5] In this study, we analyzed the prevalence, clinical profile, investigations, and visual outcomes of sarcoid intermediate uveitis (SIU) in a tertiary eye care center in South India.
Methods
This is a retrospective, observational study of 29 patients from January 2019 to June 2021. All medical records of the patients identified from the hospital database as intermediate uveitis were retrieved. The criteria set by the International Workshop On Ocular Sarcoidosis (IWOS) 2019 for the diagnosis of ocular sarcoidosis, proposed by Mochizuki M, et al.,[6] was retrospectively applied for defining patients with SIU. All patients underwent a complete ophthalmic evaluation and systemic examination by a pulmonologist. Tailored laboratory investigations were done to rule out infections and other known uveitis entities.
The following information was retrieved from the clinical records: age, gender, systemic and ocular complaints, associated systemic diseases, family history of sarcoidosis, laterality and duration of uveitis, details of ophthalmic examination, pre- and post-treatment best-corrected visual acuity (BCVA), presence and type of keratic precipitates, iris granulomas, posterior synechiae, anterior chamber reaction, cataract, vitreous reaction, intraocular pressure, retinal vasculitis, exudates in the retinal periphery, snow banking, cystoid macular edema, epiretinal membrane, vascular occlusions, and vitreous hemorrhage. The standardization of uveitis nomenclature[7] (SUN criteria) was applied for grading of the anterior chamber and vitreous reaction.
Details of systemic evaluation, including history, review of systems, and investigations done were recorded. Laboratory investigations like the Mantoux test, serum angiotensin converting enzyme, QuantiFERON TB (QTB) gold test were done. Chest X-ray and high-resolution computed tomography (HRCT) of the chest were also done to support the diagnosis. Duration of uveitis along with treatment history and response to treatment, and follow-up period were recorded. Statistical analyses including descriptive statistics like mean, standard deviation, and range were calculated.
Chi-squared tests were applied for correlation between age, sex, serum angiotensin converting enzyme, and initial presentation with independent variables. The analysis was done using SPSS version 15 (SPSS Inc., Chicago, Illinois) at a 5% level of significance.
Results
Out of the 134 patients with intermediate uveitis, 29 (21.6%) met the criteria for sarcoid intermediate uveitis. Out of a total of 50 patients diagnosed to have sarcoid uveitis, 4 patients had sarcoid anterior uveitis, 29 had sarcoid intermediate uveitis, 13 were having sarcoid posterior uveitis, 3 had sarcoid panuveitis while only one patient had anterior uveitis with intermediate uveitis. Data of 29 patients (N = 49 eyes) evaluated by the single uvea specialist were taken for the study. The mean age group was 42.14 ± 11.34 years range (20–61 years). While categorizing according to age, we found in our study 5 patients in the age group of 20–30 years, 7 patients each in 31–40 and 41–50 years, and 9 patients were there in the age group of 50 years and more. Females (15, 51.7%) were more affected than males (14, 48.3). Two patients had biopsy-proven sarcoidosis.
Diminution of vision was the most common ocular complaint followed by floaters (30%), redness (12.2%), pain in eyes (8.1%), and vitreous cells (30%) [Fig. 1]. Seventeen patients (34 eyes, 58.6%) had bilateral involvement while 12 patients (41.3%) had unilateral involvement. Mean presenting visual acuity in right and left eye were 0.2 and 0.3, respectively. Anterior segment cells and flare were graded according to SUN classification.[4] Anterior chamber cells and flares in 22.4% of cases (N = 11 eyes), posterior synechiae in 20.4% (N = 10 eyes), and both small and mutton fat keratic precipitates in 14.2% of cases (N = 7 eyes) were noted; only one eye had Busacca nodules similar to other granulomatous uveitis. Four patients had trabecular meshwork precipitates along with keratic precipitates. Posterior segment signs including vitreous exudates in 18.3% of cases (N = 9 eyes), Snowball opacities in 10.2% (N = 5 eyes), [Fig. 2] and candle wax dripping of retinal vessels was found in one eye at the inferior quadrant. Two patients were categorized as definite sarcoid, 21 patients as presumed sarcoid, and 6 as probable sarcoid.
Figure 1.

Indexed case showing vitreous exudates in sarcoid intermediate uveitis
Figure 2.
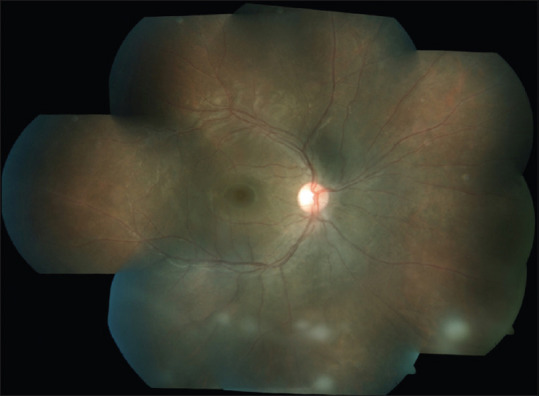
Indexed case showing multiple vitreous opacities in sarcoid intermediate uveitis
Swept source optical coherence tomography (SS-OCT) showed epiretinal membrane (ERM) in 10 eyes (20.4%), cystoid macular edema (CME) in 3 eyes (6%), and choroidal neovascular membrane (CNVM) in only 1 eye. Three patients had retinal neovascularization, Fundus Fluorescein Angiography (FFA) was performed in selected cases (N = 9 patients) and found to have peripheral vascular leakage in 3 cases (33%). Ultrasound bio-microscopy (UBM) was performed in one patient, and thin pars plana membrane was noted in it. UBM was preferred in the case of a small pupil with the presence of a cataract obscuring the view of the peripheral fundus.
Laboratory investigations
Raised serum angiotensin converting enzyme was found in 24 patients (82.7%). Mantoux positivity was seen in 4 patients (13.7%) and QTB gold test positivity in 6 patients (20.6%). HRCT of the chest showed abnormality in the form of sub-centimeter lymphadenopathy in 12 patients (41.3%) [Fig. 3]. Biopsy was done in 2 cases: in the first, CT-guided mediastinal lymph node biopsy was done, while in the second, skin biopsy of the leg was done. Out of 29 patients, 6 patients had lymphopenia.
Figure 3.

Indexed case showing bilateral hilar lymphadenopathy in high resolution computed tomography chest imaging
Thirteen patients (44.8%) were given a combination of oral steroids and immunosuppressants (mycophenolate mofetil or methotrexate), 10 patients (34.4%) were treated with oral steroids alone, 4 patients (13.7%) with both topical and oral steroids, and 2 patients (6.89%) were given posterior sub-tenon injection of triamcinolone acetonide. 30% of patients maintained their BCVA over a mean duration of 15 months with SD 13.11. 75.8% of the patients showed a good response to the treatment while 6.8% of the patients did not respond to the treatment. Visual outcomes, pre-treatment and post-treatment, were analyzed, for normality distribution. As the data were not normally distributed, a non-parametric test like Wilcoxon signed-rank test was done. Pre-treatment visual acuity and post-treatment visual acuity comparison was done and was found to be statistically insignificant in both eyes (right eye P-0.199, left eye P-0.685). Our study showed glaucoma (27.5%) to be more common than cataract formation (17.2%). The mean intraocular pressure (IOP) in our study was 15.55 ± 5.8 in Right eye (RE) and 16.10 ± 10.6 in Left eye (LE). Eight patients were found to have glaucoma but ocular hypertension was found in only one patient.
Results of laboratory investigations are shown in Table 1 and Fig. 4.
Table 1.
Laboratory investigations of Mantoux, QuantiFERON TB gold and serum angiotensin-converting enzyme (ACE)
| Mantoux test | Sarcoid intermediate uveitis n (% cases) (Total n=29) |
|---|---|
| Positive | 4 (13.7%) |
| Negative | 11 (37.9%) |
|
| |
| QuantiFERON gold TB test | Sarcoid intermediate uveitis n (% cases) (Total n=29) |
|
| |
| Positive | 6 (20.6%) |
| Negative | 13 (44.8%) |
|
| |
| Serum ACE | Sarcoid intermediate uveitis n (% cases) (Total n=29) |
|
| |
| High Serum ACE | 24 (82.7%) |
Figure 4.

Graphical representation of laboratory investigation
Discussion
In our series, intermediate uveitis was the most common manifestation in sarcoid uveitis (58%). Out of a total of 50 patients diagnosed to have sarcoid uveitis, 4 had sarcoid anterior uveitis, 29 had sarcoid intermediate uveitis, 13 were having sarcoid posterior uveitis, 3 had sarcoid panuveitis while only 1 patient had anterior uveitis with intermediate uveitis. This is in contrast with most studies, which report anterior uveitis as the most common manifestation.[1,2,8] Out of total intermediate uveitis patients, 21.6% were SIU. It is predominantly seen in adults, with most patients being in their 4th–6th decade. Other studies on ocular sarcoidosis from the West shows two peaks, one at 20–30 years and another at 50–60 years.[1,2] A female preponderance (51.7%) was seen in our study, which is in contrast to a study from North India that showed male preponderance.[3] The reason for female preponderance and an exact correlation could not be established. In other studies, sarcoidosis also found female preponderance but the exact reason could not be found.[9] From our study, the most common ocular complaint was found to be the diminution of vision (51%) followed by floaters (30%) and redness of the eye (12%). On analyzing signs, 24% of our cases had anterior chamber reaction, 22.4% had keratic precipitates, and 20.4% had posterior synechiae. Mutton fat keratic precipitates (large and small) and/or iris nodules at the pupillary margin (Koeppe) or in the stroma (Busacca) were seen in 14.2% of cases. Vitreous cells and snowballs/string of pearls vitreous opacities were seen in 10.2% along with pars plana exudates while the rest 89.8% had only dispersed vitritis [Figs. 1 and 2].
Systemic involvement in our series was mostly asymptomatic chest involvement. In our series, an HRCT of the thorax was more helpful in detecting mediastinal lymphadenopathy and the pulmonary changes in comparison to chest X-ray [Fig. 3]. We recommend HRCT thorax to chest X-ray whenever possible, as it is more sensitive. Raised ESR and elevated serum angiotensin-converting enzyme were seen in 82.7% of our patients with SIU.[10] The majority of our cases had a negative Mantoux reaction (80%). All of our patients had normal serum calcium and liver function tests. On analysis, it was found that posterior synechiae, granulomatous keratic precipitates, reactive anterior chamber reaction, and cystoid macular edema were more common. This may be due to the chronic nature of the disease. No significant association of independent variables in clinical presentation with age, sex, and increased angiotensin converting enzyme was noted. Our study suggests that all patients with SIU require treatment and have a favorable prognosis. 75.8% of the patients in our series showed a good response to the treatment while 6.8% of the patients did not respond to the treatment. In addition to topical steroids like prednisolone acetate 1% and topical cycloplegics for spill over anterior uveitis, oral steroids with immunosuppressive medications (methotrexate, mycophenolate mofetil, azathioprine and cyclosporine) were the mainstay of treatment. Periocular sub-tenon steroid injections of triamcinolone acetonide in cases of unilateral disease should be considered. IWOS consensus guidelines also recommended the use of TNF-α inhibitor, adalimumab, if necessary.[11] However, none of our cases required a TNF-α inhibitor. Regular intraocular pressure evaluation for steroid-response glaucoma should be done and treatment with anti-glaucoma medication should be done as and when required. Glaucoma (27.5%) followed by cataracts (17.2%) were the most common cause of the diminution of vision in our series. This was partly due to the posterior segment inflammation and partly due to steroid use. Contrary to other studies which report CME (51.3%) as the most common complication,[12] our study showed glaucoma (27.5%) to be the most common complication. Despite the many complications in SIU, the overall prognosis is encouraging. Most patients have retained BCVA (38%) in our series.
PubMed and Medline searches have not shown any study on sarcoid intermediate uveitis. Our study is the first to report the prevalence, longitudinal course, management, and visual outcomes in patients with sarcoid intermediate uveitis from India.
Limitations of our study are its retrospective nature and a relatively small number of patients, compared to multicenter, population-based cohort studies. Also, the grading of radiological findings was not done.
Conclusion
In conclusion, sarcoidosis is a common cause of intermediate uveitis in a tuberculosis endemic country like India. Early diagnosis and management with systemic steroids and immunosuppressives help in restoring good vision.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Authors acknowledge the help of Miss Esther Sunitha, content writer of Sankara Nethralaya for English correction
References
- 1.Rothova A. Ocular involvement in sarcoidosis. Br J Ophthalmol. 2000;84:110–6. doi: 10.1136/bjo.84.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones NP. Sarcoidosis and uveitis. Ophthalmol Clin N Am. 2002;15:319–26. doi: 10.1016/s0896-1549(02)00021-4. [DOI] [PubMed] [Google Scholar]
- 3.Bambery P, Behera D, Gupta AK, Kaur U, Jindal SK, Deodhar SD, et al. Sarcoidosis in north India:The clinical profile of 40 patients. Sarcoidosis. 1987;4:155–8. [PubMed] [Google Scholar]
- 4.Ganesh SK, Agarwal M. Clinical and investigative profile of biopsy-proven sarcoid uveitis in India. Ocul Immunol Inflamm. 2008;16:17–22. doi: 10.1080/09273940801904150. [DOI] [PubMed] [Google Scholar]
- 5.Khanna A, Sidhu U, Bajwa G, Malhotra V. Pattern of ocular manifestations in patients with sarcoidosis in developing countries. Acta Ophthalmol Scand. 2007;85:609–12. doi: 10.1111/j.1600-0420.2006.00791.x. [DOI] [PubMed] [Google Scholar]
- 6.Mochizuki M, Smith JR, Takase H, Kaburaki T, Acharya NR, Rao NA International workshop on ocular sarcoidosis study group. Revised criteria of International workshop on ocular sarcoidosis (IWOS) for the diagnosis of ocular sarcoidosis. Br J Ophthalmol. 2019;103:1418–22. doi: 10.1136/bjophthalmol-2018-313356. [DOI] [PubMed] [Google Scholar]
- 7.Jabs DA, Nussenblatt RB, Rosenbaum JT Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data:Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans M, Sharma O, LaBree L, Smith RE, Rao NA. Differences in clinical findings between Caucasians and African Americans with biopsy-proven sarcoidosis. Ophthalmology. 2007;114:325–33. doi: 10.1016/j.ophtha.2006.05.074. [DOI] [PubMed] [Google Scholar]
- 9.Pasadhika S, Rosenbaum JT. Ocular sarcoidosis. Clin Chest Med. 2015;36:669–83. doi: 10.1016/j.ccm.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cotte P, Pradat P, Kodjikian L, Jamilloux Y, Seve P. Diagnostic value of lymphopaenia and elevated serum ACE in patients with uveitis. Br J Ophthalmol. 2021;105:1399–404. doi: 10.1136/bjophthalmol-2020-316563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acharya NR, Browne EN, Rao N, Mochizuki M International Ocular Sarcoidosis Working Group. Distinguishing features of ocular sarcoidosis in an international cohort of uveitis patients. Ophthalmology. 2018;125:119–26. doi: 10.1016/j.ophtha.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Parchand S, Tandan M, Gupta V, Gupta A. Intermediate uveitis in Indian population. J Ophthalmic Inflamm Infect. 2011;1:65–70. doi: 10.1007/s12348-011-0020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


