Diffuse large B cell lymphoma (DLBCL) constitutes around 30% of non-Hodgkin’s lymphomas. Extra nodal involvement is commonly seen in DLBCL. Gastrointestinal tract, head and neck are the most common extranodal sites involved by DLBCL.[1] Lymphoma primarily involving the lacrimal sac is extremely rare, usually reported in the elderly. Only case reports and few case series have been reported so far globally.[2] This entity is often misdiagnosed as benign or inflammatory pathology due to its rarity; hence the remote possibility of lymphoma should be kept in mind while evaluating medial canthus swelling. We report a case of primary lacrimal sac DLBCL in a 43-year-old lady, its clinical features, diagnosis, and management along with a brief review of the literature as it is very rarely seen in routine oncological practice.
A 43-year-old female was evaluated for left nasal block, headache, medial canthus swelling in left side and left eye epiphora of one year duration. No history of any purulent or bloody discharge from left eye or history of any trauma. There was a small non-tender swelling with firm consistency of size 1.5 × 1 cm just below the medial canthus of the left eye in the lower palpebral region. The patient had no history of night sweats, fever or weight loss (B-symptoms); there were no regional lymph node enlargement, and her systemic examinations were within normal limits. Anterior rhinoscopy showed deviated nasal septum with spur on left side and a pinkish smooth mucosa-covered lesion in inferior meatus. Computed tomography (CT) scan of paranasal sinus showed a dumbbell-shaped lesion involving the left lacrimal sac involving the nasolacrimal duct and inferior meatus. Lacrimal sac component measured 1.7 × 1.3 × 1.5 cm and inferior component of dumbbell measured 1.9 × 1.5 × 1.9 cm, causing minimal remodeling of adjacent lacrimal bone. There was no evidence of bony erosion in imaging. The possible differential diagnoses were chronic dacryocystitis and secondary dacryostenosis, Inflammatory or granulomatous involvement of lacrimal sac and benign papilloma or adenomas. In view of long-standing history of swelling, squamous cell carcinoma of lacrimal sac was also considered as a remote possibility. She underwent diagnostic nasal endoscopy and biopsy from the inferior component of the lesion. Intraoperatively, there was a mucosa-covered friable mass in the left inferior meatus eroding the lateral wall of lacrimal bone. Histopathology examination showed dense infiltrate of atypical lymphoid cells with moderate amount of cytoplasm and vesicular nuclei and nucleoli in subepithelial stroma, with a MIB1 labelling index of 80%. On immunohistochemistry, these cells were positive for CD10, CD20, BCL2, BCL6 and negative for CD23, cMYC, TdT. The picture was suggestive of DLBCL Germinal Center B Cell (GCB) like [Fig. 1].
Figure 1.
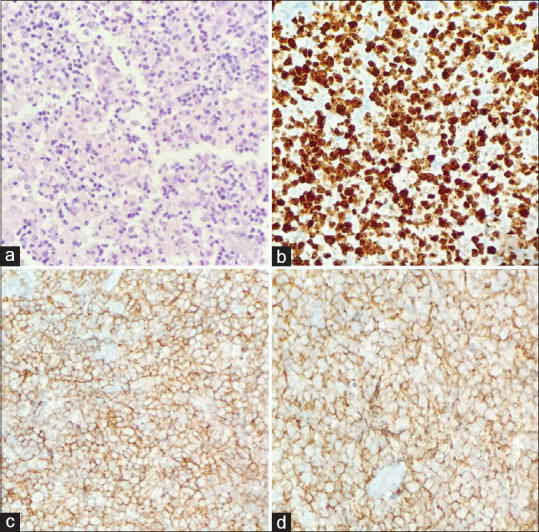
Histopathology images of the tumor. (a) H and E staining showing large cells with moderate cytoplasm, large vesicular nuclei and are seen admixed with small lymphoid cells. (b) MIB1 labelling index is 80%. Tumor cells are positive for (c) CD20, (d) CD10
As a part of the lymphoma work-up, a whole body positron emission tomography and computed tomography (PET CT) scan was done, which showed an uptake only at the primary site with an SUV max of 12.3; there were no other PET avid active disease elsewhere [Fig. 2]. Her complete hemogram and serum biochemistry were within normal limits. Her serum LDH was 168 IU/L and bone marrow study was within normal limits. She was diagnosed as having primary DLBCL involving the left lacrimal sac and nasolacrimal duct, stage I (Ann Arbor Staging) with a Lymphoma International Prognostic (IPI) score of zero (low risk). Since there was bone erosion, as per AJCC staging, it was T4N0M0 disease. She was planned for systemic chemotherapy with R-CHOP ×3 cycles (Rituximab, Cyclophosphamide, Doxorubicin Vincristine and Prednisolone) followed by involved field radiation. She completed 3 cycles of chemotherapy; her response assessment PET scan was suggestive of complete metabolic response. She underwent adjuvant-involved field radiation of dose 30 Gray in 15 fractions. At present, she completed 9 months of follow up and clinically, there is now evidence of any disease.
Figure 2.
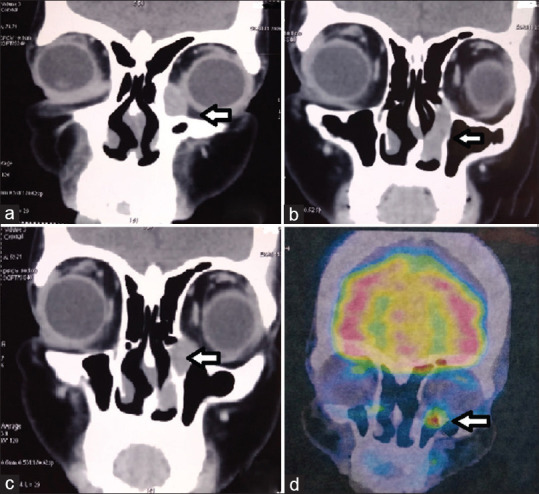
Sagittal sections of face in PET- CT images showing PET avid lesion occupying the medial canthus of left eye (bold arrow) extending to the nasolacrimal duct
Discussion
Lacrimal sac tumors are extremely rare. Less than 800 cases have been reported worldwide till date. About 55% of lacrimal sac tumors are malignant; epithelial tumors constitute 71% of cases. Lacrimal sac lymphomas accounts for about 2%–8% of tumors.[3] European Organization for Research and Treatment of Cancer (EORTC) ophthalmic oncology task force study on lacrimal sac lymphoma have shown that DLBCL and extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT) were the most common histologies, both constituting 33% each.[4] Whereas in a case series among a Chinese population, all patients were having MALT lymphoma, and among Japanese population, 37.5% (3 out of 8 patients) were DLBCL.[5]
Most of the reported cases of lacrimal lac lymphomas originate from the elderly population. Median age in a previous case series was 71 years and majority of them were females.[3] Even though lacrimal sac lymphomas are considered as a disease of the elderly, it is very rarely seen in children. So far, only two cases of primary lacrimal sac lymphomas in pediatric population have been reported.[6] Most of the patients had symptoms suggestive of long-standing chronic dacryocystitis or dacryostenosis. Most common presenting symptoms were unilateral epiphora and palpable painless mass in medial canthus. Blood-stained tear which is considered as the tell-tale sign of malignancy was not very common in lacrimal sac lymphomas.[3]
Long-standing inflammation is the proposed mechanism of lacrimal sac lymphoma. Even though MALT lymphomas are supposed to be common in lacrimal sac, primary DLBCL has also been reported in equal frequency in literature. DLBCL is considered to be an aggressive lymphoma. Advanced stage DLBCL with ocular involvement is associated with inferior survival.[7] But in localized primary ocular DLBCL, 5-year survival is as high as 90.9%. Altogether, among lacrimal sac lymphomas, 5-year overall survival is 65%.[4]
Most of the patients with lacrimal sac lymphoma underwent surgery followed by adjuvant treatment as most of them were misdiagnosed as benign inflammatory lesions, and lacrimal sac is an unusual site for lymphoma. As there are only cases series reported so far, no standard recommendations were seen in literature regarding treatment of primary DLBLC of lacrimal sac. Most commonly employed treatment modalities after diagnosis were R-CHOP chemotherapy, local radiation or combination of both. Elderly, frail patients were treated with local radiotherapy alone, with a dose ranged of 30 Gy to a maximum of 50 Gy depending on tolerance. Young, fit patients underwent R-CHOP chemotherapy alone or combination of chemotherapy and radiation.[8] There were no direct comparison of various treatment modalities, all patient had excellent disease control irrespective of the treatment modalities. Most of the elderly patients died of causes other than disease progression.
Primary lacrimal sac lymphomas are extremely rare. Diagnosis is usually delayed due to its unusual presentation. Most of the time, patients are diagnosed after excision which is done as a part of evaluation of other benign or inflammatory pathology. Even though primary lacrimal sac lymphoma is a disease of the elderly, it can be seen in young adults also. Most of them are localized, present at an early stage, and have excellent local control with chemotherapy, radiation or both in combination. Hence, it should always be considered as a possible differential diagnosis while evaluating medial canthus swelling.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Castillo JJ, Winer ES, Olszewski AJ. Sites of extranodal involvement are prognostic in patients with diffuse large B-cell lymphoma in the rituximab era:An analysis of the surveillance, epidemiology and end results database. Am J Hematol. 2014;89:310–4. doi: 10.1002/ajh.23638. [DOI] [PubMed] [Google Scholar]
- 2.Venkitaraman R, George M. Primary non Hodgkin's lymphoma of the lacrimal sac. World J Surg Oncol. 2007;5:127. doi: 10.1186/1477-7819-5-127. doi:10.1186/1477-7819-5-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krishna Y, Coupland SE. Lacrimal sac tumors--A review. Asia Pac J Ophthalmol (Phila) 2017;6:173–8. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 4.SjöLD, Ralfkiaer E, Juhl BR, Prause JU, Kivelä T, Auw-Haedrich C, et al. Primary lymphoma of the lacrimal sac:An EORTC ophthalmic oncology task force study. Br J Ophthalmol. 2006;90:1004–9. doi: 10.1136/bjo.2006.090589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kakutani S, Takahashi Y, Valencia MRP, Kakizaki H. Diffuse large b-cell lymphoma of the lacrimal sac in a Japanese patient. Case Rep Ophthalmol. 2018;9:516–9. doi: 10.1159/000495745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schefler AC, Shields CL, Shields JA, Demirci H, Maus M, Eagle RC. Lacrimal sac lymphoma in a child. Arch Ophthalmol. 2003;121:1330–3. doi: 10.1001/archopht.121.9.1330. [DOI] [PubMed] [Google Scholar]
- 7.Tsao WS, Huang TL, Hsu YH, Chen N, Tsai RK. Primary diffuse large B cell lymphoma of the lacrimal sac. Taiwan J Ophthalmol. 2016;6:42–4. doi: 10.1016/j.tjo.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakamura K, Uehara S, Omagari J, Kunitake N, Kimura M, Makino Y, et al. Primary non-Hodgkin's lymphoma of the lacrimal sac. Cancer. 1997;80:2151–5. doi: 10.1002/(sici)1097-0142(19971201)80:11<2151::aid-cncr15>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]


