Abstract
Purpose:
To evaluate the outcomes of surgical intervention in cases of ectopia lentis.
Methods:
This retrospective study included all cases of ectopia lentis that presented between June 2015 and March 2019 in a tertiary care center. They were reviewed retrospectively. The corrected distance visual acuity (CDVA), severity of lens subluxation, type of surgery, intra-operative and post-operative complication, and specular count were recorded.
Results:
Seventy-eight eyes of 57 cases with a mean age at surgery of 14.73 years were analyzed. Intra-lenticular lens aspiration was the most common (n-62/78; 79.5%) surgical procedure followed by lens aspiration, intra-capsular cataract extraction, phaco-aspiration, and pars-plana lensectomy. Simultaneous intra-ocular lens (IOL) implantation was performed in 46.2% (n-32/78) of the eyes. The mean CDVA improved from 0.85 ± 0.55 logMAR to 0.44 ± 0.29 logMAR at 6 weeks follow-up. The post-operative CDVA was significantly better in the pseudo-phakic group compared to the aphakic group (p-0.02). The patient’s age at the time of surgery and the degree of subluxation did not impact the final visual outcome. Intra-operative complication included vitreous hemorrhage (n-1) and lens matter drop (n-1). Post-operative complications were noted in 26.9% of the eyes (n-21/78) with a higher complication rate in the pseudo-phakic group (p-0.00). A second intervention was required in 7.7% of the eyes (n-6/78).
Conclusion:
Age and degree of subluxation at the time of surgery do not influence the final visual outcome in cases of ectopia lentis undergoing lens extraction surgery. IOL implantation results in better visual outcomes but is associated with a high complication rate.
Keywords: Anterior chamber intra-ocular lens, ectopia lentis, intra-lenticular lens aspiration, marfan syndrome, scleral fixated intra-ocular lens, subluxated lens
Ectopia lentis, first described by Stellwag, refers to congenital dislocation of lenses.[1] Zonular weakness in these cases results in lenticular curvature changes inducing lenticular myopia and astigmatism.[1] The early cases of ectopia lentis usually perform well with spectacles; however, most of the patients eventually require surgical intervention because of the progressive course of this disorder.[2,3] Surgery is indicated in cases of ectopia lentis with the edge of the lens bisecting the pupil; the best corrected visual acuity is not achieved with spectacles, cataract, imminent complete luxation of the lens, and secondary glaucoma or uveitis.[1]
Surgical management of cases of ectopia lentis is often difficult and is associated with several challenges. The various surgical techniques described in the literature for the management of subluxated lenses include lensectomy (limbal/pars plana), lens aspiration, in the bag bimanual irrigation-aspiration of the lens, phaco-aspiration, intra-lenticular lens aspiration (ILLA), and intra-capsular cataract extraction (ICCE).[3,4,5,6,7,8] The options for intra-ocular lens (IOL) implantation in these cases include anterior chamber IOL (ACIOL), iris clawed IOL, scleral-fixated IOL (SFIOL), and posterior chamber IOL (PCIOL) with capsular supporting devices.
The largest series up to date has been described by Fan et al., followed by Khokhar et al. and Manning et al. in 64, 32, and 30 eyes of ectopia lentis undergoing surgical management.[9,10,11] In this series, we report the outcomes of different surgeries including ILLA, lens aspiration, ICCE, and pars-plana lensectomy (PPL) in 78 eyes of 57 patients, which is perhaps the largest case series to the best of our knowledge.
Methods
This retrospective review included 78 eyes of 57 consecutive cases of ectopia lentis that underwent surgical management for visual rehabilitation at a tertiary eye care center in North India between June 2015 and March 2019. The study adhered to the declaration of Helsinki. Approval for conducting the study was obtained from the institutional review board/ethics committee.
The medical records of all the cases were evaluated, and the following parameters were recorded: uncorrected distance visual acuity (UCVA), spectacle-corrected distance visual acuity (CDVA), intra-ocular pressure (IOP), corneal diameter, presence of strabismus and nystagmus, direction and severity of lens subluxation, presence of cataract, cataract morphology, fundus findings, axial length, and keratometry [Table 1]. A careful review of surgical notes was performed to record the various intra-operative difficulties and or complications. CDVA at the last follow-up after surgery and development of post-operative complications such as glaucoma, visual axis opacification, IOL decentration, and posterior segment complications were also recorded.
Table 1.
Baseline characteristics and post-operative outcomes of cases (n-78) with ectopia lentis undergoing surgery
| Parameters | Values |
|---|---|
| Age (years) (mean, range) | 14.73±9.5 (3-40) |
| Sex (M/F) | 47/10 |
| Systemic features (%, n) | 52.6% (28) |
| Marfan syndrome | 22.8% (13) |
| Marfanoid habitus | 22.8% (13) |
| WAGR syndrome | 1.7% (1) |
| Homocystinuria | 1.7% (1) |
| UCVA (logMAR) (Mean±SD) | 1.47±0.44 |
| CDVA (logMAR) (Mean±SD) | 0.85±0.55 |
| IOP (mm of Hg) (Mean±SD) | 15.55±3.6 |
| MRSE (D) (Mean±SD) (Median, range) | 6.92±10.5 (10.5, -22 to 19.5) |
| Subluxation extent (clock hour) (Mean±SD) | 7.11±1.44 |
| Cataract (%, n) | 20.5% (16) |
| Mean K (D) (Mean±SD) | 41.42±2.04 |
| Axial length (mm) (Mean±SD) | 24.29±2.23 |
| Pre-op ECD (n-25) (cells/mm2) (Mean±SD) | 3585.96±342.27 |
| Post-op ECD (n-18) (cells/mm2) (Mean±SD) | 3505.66±448.17 |
| Surgery (%, n) | |
| ILLA | 50% (39) |
| Lens aspiration | 2.6% (2) |
| ILLA + SFIOL | 24.4% (19) |
| ICCE + SFIOL | 2.6% (2) |
| Lens aspiration + IOL | 11.5% (9) |
| ILLA + ACIOL | 5.1% (4) |
| PPL | 1.3% (1) |
| Phaco + ACIOL | 2.6% (2) |
| IOL status (%, n) | |
| Aphakia | 53.8% (42) |
| ACIOL | 7.7% (6) |
| SFIOL | 26.9% (21) |
| PCIOL + CTR | 11.5% (9) |
| Intra-operative complication (%, n) | 2.6% (2) |
| VH | 1.3% (n-1) |
| Cortical matter drop | 1.3% (n-1) |
| CDVA at the last follow-up (logMAR) (Mean±SD) | 0.42±0.31 (0.48, 0 to 1.78) |
| Post-op IOP (mm of Hg) (Mean±SD) (range) | 14.1±4.79 (6-26) |
| Post-operative complications (%, n) | 26.9% (21) |
| Vitreous in AC | 5.1% (4) |
| Decentered IOL | 3.8% (3) |
| Optic capture | 1.3% (1) |
| VAO | 1.3% (1) |
| Transient IOP rise | 10.3% (8) |
| Vitreous hemorrhage | 1.3% (1) |
| Endophthalmitis | 1.3% (1) |
| Re-intervention (%, n) | 8.9% (7) |
| Nd-YAG vitreolysis | 3.8% (3) |
| IOL explant with SFIOL | 2.6% (2) |
| IOL tapping with pupilloplasty | 1.3% (1) |
| Intravitreal antibiotic injection | 1.3% (1) |
| Nd-YAG capsulotomy | 1.3% (1) |
| Secondary IOL implantation | 11.5% (9) |
M- male; F- female; UCVA- uncorrected visual acuity; CDVA- corrected distance visual acuity; IOP- intra-ocular pressure; MRSE- manifest refractive spherical equivalent; ECD- endothelial cell density; ILLA- intra-lenticular lens aspiration; SFIOL- scleral fixated intra-ocular lens; IOL- intra-ocular lens; ACIOL- anterior chamber intra-ocular lens; PPL- pars-plana lensectomy; CTR- capsular tension ring; VH- vitreous hemorrhage; AC- anterior chamber; VAO- visual axis opacification
Results
A total of 78 eyes of 57 cases of ectopia lentis that underwent surgery were included. The mean age at the time of surgery was 14.73 ± 9.5 years (range, 3-40 years) with ten females and 47 males. The mean UCVA, CDVA, and IOP at presentation were 1.47 ± 0.44 logMAR units (range, 0.48 to 2.3 logMAR), 0.85 ± 0.55 logMAR units (range, 0 to 2.3 logMAR), and 15.55 ± 3.6 mm of Hg (range, 10 to 34 mm of Hg), respectively. The manifest refractive spherical equivalent (MRSE) at presentation was 6.92 ± 10.5 D (range, -22 to 19.5 D). Strabismus was observed in 17.9% (n-14/78) of the cases. The mean axial length was 24.29 ± 2.23 mm (range, 19.6 to 29.4 mm). The mean keratometry was 41.42 ± 2.04 D (range, 37.25 to 46.38 D). Lens subluxation was bilateral in all the cases. The direction of lens subluxation was supero-temporal (n-20/78; 25.6%), supero-nasal (n-20/78; 25.6%), superior (n-13/78; 16.7%), temporal (n-11/78; 14.1%), and others (n-14/78; 18%). The mean subluxation was 7.11 ± 1.44 clock hours (range 3 to 10 clock hours). Cortical cataract was present in 20.5% (n-16/78) of the eyes. Fundus findings revealed foveal hypoplasia in five, with glaucomatous cupping and retinal lattices in the two eyes each. Prophylactic laser delimitation of lattice degeneration was performed before surgery. Systemic association was observed in 52.6% (n-28/57) of the cases, which included Marfan syndrome in 22.8% (n-13/57), leptosomic features of Marfan syndrome but with the Ghent diagnostic criteria (marfanoid habitus) not met in 22.8% (n-13/57), WAGR syndrome in 1.7% (n-1/57), and homocystinuria in 1.7% (n-1/57) [Table 1].
Intra-operative findings
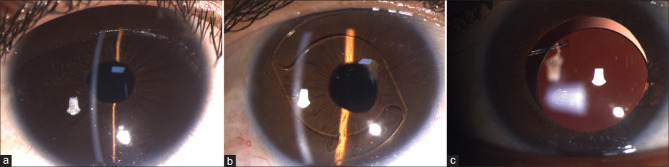
ILLA was the most common surgical procedure performed in 79.5% of the eyes (n-62/78). The other procedures included lens aspiration in 14.1% (n-11/78), phaco-aspiration in 2.6% (n-2/78), ICCE in 2.6% (n-2/78), and PPL in 1.3% of eyes (n-1/78). Simultaneous IOL implantation was performed in 46.2% of the eyes (n-36/78). SFIOL was implanted in 26.9% of the eyes (n-21/78), PCIOL was implanted in 11.5% of the eyes (n-9/78) with capsular tension ring (CTR) implantation, and ACIOL was implanted in 7.7% of the eyes (n-6/78) [Fig. 1a-c]. SFIOL was performed by intra-scleral fixation of haptic. Pre-operatively, aphakia was planned for 51.3% (n-40/78) of the eyes. The factors for deciding aphakia were largely based on the surgeons’ individual preferences that included various factors such as the patient’s age (n-18/78), progressive myopia (n-13/78), staged procedure (n-8/78), and other eye lens statuses (n-2/78). Intra-operative vitreous hemorrhage was noted in one case that underwent simultaneous SFIOL implantation. Cortical matter drop was noted in one case that underwent ILLA [Table 1].
Figure 1.
Slit-lamp image of cases with ectopia lentis that underwent intra-lenticular lens aspiration: (a) aphakia, (b) pseudo-phakia with a well-centered ACIOL, and (c) pseudo-phakia with a scleral-fixated IOL
Post-operative outcome
The post-operative mean CDVA at 6 weeks and the last follow-up (8.1 ± 10.7 months, range 1.5 to 36 months) was 0.44 ± 0.29 logMAR and 0.42 ± 0.30 logMAR, respectively. There was a significant change in CDVA after surgery (p = 0.001).
Regression analysis was performed to assess the parameters that affect the final visual outcome (CDVA at the last follow-up). The age at surgery, UCVA at presentation, CDVA at presentation, the extent of subluxation, and IOL implantation during surgery were assessed. A significant correlation was observed between UCVA at presentation (correlation coefficient = 0.19, 95% CI = 0.04 to 0.34, p – 0.013), CDVA at presentation (correlation coefficient = 0.23, 95% CI = 0.12 to 0.34, p- 0.000), and IOL implantation at the time of surgery (correlation coefficient = –0.15, 95% CI = -0.28 to -0.02, p = 0.028) with CDVA at the last follow-up (in logMAR).
Post-operative complications were noted in 26.9% (n-21/78) of the eyes. Post-operative complications are summarized in the supplementary table and included pupillary peaking with a vitreous strand in the anterior chamber [Fig. 2a and b], decentered PCIOL [Fig. 2c and d], optic capture, and endophthalmitis. Nd-YAG capsulotomy was performed in one case for visual axis opacification. Secondary IOL implantation was performed in 28.12% of the aphakic cases (n-9/32). SFIOL was implanted in all these cases by the intra-scleral haptic fixation technique. None of the cases developed any posterior segment complication on follow-up.
Figure 2.
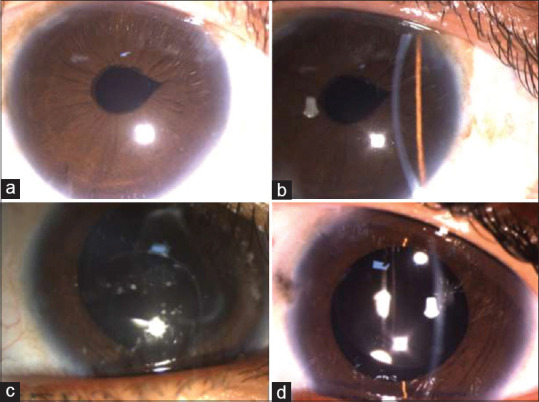
Slit-lamp image of the right eye of a case with ectopia lentis that underwent intra-lenticular lens aspiration with SFIOL showing (a) pupillary peaking in diffuse illumination and (b) vitreous strand in the anterior chamber in focal slit illumination. Slit-lamp image of the right eye of another case (c) showing visually significant inferior decentration of the IOL with haptic in the anterior chamber after 1 year of lens aspiration and PCIOL implantation with CTR and (d) two months after explanation of the decentred PCIOL and simultaneous SFIOL implantation
Long-term results were available for a small subset of patients (36 eyes of 23 cases). The mean follow-up duration was 15.7 ± 10.6 months (range – 6 to 36 months). The mean CDVA improved from the baseline value of 0.80 ± 0.55 logMAR (median = 0.6; range = 0 to 1.9 logMAR) to 0.37 ± 0.38 logMar units (median = 0.3; range = 0 to 1.78 logMAR) at final follow-up (p = <0.00001; Wilcoxon signed-rank test). The mean IOP was 13.7 ± 3.0 mm of Hg (range 6 to 21), and none of the cases had IOP >21 mm of Hg at the last follow-up. The mean MRSE improved from 9.04 ± 7.48 D (median = 10.5 D; range = -2 to 16.5 D) at the baseline to 4.21 ± 5.78 D (median = 1.6 D; range = -2 to 16.5 D) at the final follow-up (p = 0.003; Wilcoxon signed-rank test). Secondary IOL implantation (SFIOL) was performed in four eyes during the follow-up period.
Discussion
Management of cases with ectopia lentis is often challenging. The final visual outcome in such cases depends on a lot of factors including timing of surgery, type of surgery, visual rehabilitation method, and parent’s compliance.
We compared the visual outcomes in cases that were operated either before or after the age of plasticity (8 years of age) to assess if age of surgery impacts the final CDVA [Table 2]. The CDVA at the last follow-up in both the groups (age at surgery <8 years and >8 years) were comparable (p-0.68). This suggests that the risk of developing amblyopia in these cases, unlike those with bilateral cataract, is relatively less. It may be because the lens is clear, and the extent of subluxation may be mild to begin with, in most of the cases. Another factor is spectacle correction of the refractive error at an early age, which was there in most of our cases.
Table 2.
Comparison of baseline characteristics and post-operative outcomes based on groups classified on the age of plasticity
| Age <8 years (n-27 eyes; 18 cases) | Age >8 years (n-51 eyes of 39 cases) | P | |
|---|---|---|---|
| Age (years) | 5.7±1.3 | 19.52±8.4 | 0.00 |
| UCVA (logMAR) | 1.43±0.46 | 1.49±0.43 | 0.76 |
| CDVA (logMAR) | 0.89±0.56 | 0.82±0.55 | 0.42 |
| MRSE (D) | 9.82±9.79 (-22 to 18) | 5.58±10.64 (-19.5 to 19.5) | 0.06 |
| IOP (mm of Hg) | 15.07±2.98 | 15.8±3.89 | 0.39 |
| Subluxation extension (clock hours) | 6.9±1.7 | 7.2±1.3 | 0.41 |
| Axial length (mm) | 23.48±1.77 | 24.72±2.35 | 0.01 |
| Mean keratometry (D) | 41.36±1.9 | 41.45±2.13 | 0.85 |
| Squint | 22.2% (6) | 15.7% (8) | 0.54 |
| Pupillary zone - Aphakia | 70.4% (19) | 70.6% (36) | 1 |
| Pupillary zone - Phakic | 29.6% (8) | 29.4% (15) | 1 |
| Nystagmus | 11.1% (3) | 5.9% (3) | 0.41 |
| Cataract | 14.8% (4) | 23.5% (12) | 0.55 |
| Surgery | |||
| ILLA | 70.4% (19) | 39.2% (20) | |
| Lens aspiration | 3.7% (1) | 1.9% (1) | |
| ILLA + SFIOL | 7.4% (2) | 33.3% (17) | |
| ICCE + SFIOL | 0% (0) | 3.9% (2) | |
| Lens aspiration+IOL | 18.5% (5) | 7.8% (4) | |
| ILLA + ACIOL | 0 (0) | 7.8% (4) | |
| PPL | 0 (0) | 1.9% (1) | |
| Phaco + ACIOL | 0 (0) | 3.9% (2) | |
| IOL status | |||
| Aphakia | 74.1% (20) | 43.1% (22) | |
| ACIOL | 0 (0) | 11.8% (6) | |
| SFIOL | 7.4% (2) | 37.3% (19) | |
| PCIOL + CTR | 18.5% (5) | 7.8% (4) | |
| Intra-op Complication | 0% | 3.9% (2) | 1 |
| Re-intervention | 3.7% (1) | 9.8% (5) | 0.66 |
| Post-op complication | 7.4% (2) | 37.3% (19) | 0.04 |
| VH | 0 | 5.9% (3) | |
| Vitreous in AC | 0 | 7.8% (4) | |
| Decentered IOL | 3.7% (1) | 3.9% (2) | |
| Optic capture | 0 | 1.9% (1) | |
| VAO | 3.7% (1) | 0 | |
| Endophthalmitis | 0 | 1.3% (1) | |
| Transient IOP rise | 0 | 15.7% (8) | |
| CDVA last follow-up | 0.41±0.28 | 0.43±0.31 | 0.68 |
| Change in CDVA (from the baseline to the last follow-up) | 0.48±0.49 | 0.39±0.51 | 0.33 |
UCVA- uncorrected visual acuity; CDVA- corrected distance visual acuity; MRSE- manifest refractive spherical equivalent; IOP- intra-ocular pressure; ILLA- intra-lenticular lens aspiration; SFIOL- scleral fixated intra-ocular lens; IOL-intra-ocular lens; ACIOL- anterior chamber intra-ocular lens; PPL- pars-plana lensectomy; CTR- capsular tension ring; VH- vitreous hemorrhage; AC- anterior chamber; VAO- visual axis opacification
Another aspect that we explored in this study was the impact of IOL implantation on the long-term visual outcome and post-operative complication rate in these cases [Supplementary file]. We observed that the CDVA improved in both aphakic and pseudo-phakic groups after surgery; however, the CDVA at the last follow-up was significantly better in the pseudo-phakic group when compared to the aphakic group (p-0.02). The better outcome in the pseudo-phakic group can be explained by the fact that compliance with aphakic spectacles in young patients is often difficult. The heavy weight of the glasses, the poor quality of vision, and the restricted field of vision are the major concerns with aphakic spectacles. As a result, even in the post-operative period, the young patients are at risk of ametropic amblyopia. It is important to note that the post-operative complications were more common in the pseudo-phakic group when compared to the aphakic group (p-0.000). However, all the complications could be managed well with good visual outcomes. Thus, we suggest that every attempt must be made to implant IOL in these cases rather than leaving them aphakic. Scleral fixation of IOL (SFIOL) has been described as a viable option for correction of aphakia in such cases. In our series, all patients underwent SFIOL using fibrin glue without any complications. Although suture fixation of SFIOL is rarely practised nowadays, the potential risk of degradation of suture material over time compromising lens stability must be kept in mind.
Supplementary file.
Table showing comparison of baseline characteristics and post-operative outcome based on groups classified on the basis of IOL implantation
| Aphakia (n-42) | IOL (n-36) | p value | ||
|---|---|---|---|---|
| Age (years) | 10.9 ± 7.8 | 19.19 ± 9.5 | 0.00 | |
| UCVA(logMAR) | 1.47 ± 0.42 | 1.47 ± 0.46 | 0.88 | |
| CDVA (logMAR) | 0.89 ± 0.55 | 0.78 ± 0.55 | 0.29 | |
| MRSE (D) | 7.09 ± 10.87 | 6.72 ± 10.22 | 0.84 | |
| IOP (mm of Hg) | 15.69 ± 4.36 | 15.38 ± 2.49 | 0.71 | |
| Subluxation (clock hrs) | 7.14 ± 10.87 | 7.07 ± 1.56 | 0.83 | |
| Axial length(mm) | 24.66 ± 2.29 | 23.86 ± 2.12 | 0.12 | |
| Mean keratometry (D) | 41.61 ± 1.91 | 41.21 ± 2.19 | 0.39 | |
| Squint | 23.8% (10) | 11.1% (4) | 0.23 | |
| Nystagmus | 11.9% (5) | 2.8% (1) | 0.21 | |
| Cataract | 19°% (8) | 22.2% (8) | 0.78 | |
| Pupillary zone-Aphakia | 76.2°% (32) | 63.9% (23) | 0.32 | |
| Pupillary Zone - Phakic | 23.8% (10) | 36.1% (13) | 0.32 | |
| Surgery | ILLA | 92.9% (39) | - | |
| Lens aspiration | 4.8% (2) | - | ||
| PPL | 2.4% (1) | - | ||
| ILLA + SFIOL | - | 52.8% (19) | ||
| ICCE + SFIOL | - | 5.6% (2) | ||
| Lens aspiration + IOL | - | 25% (9) | ||
| ILLA + ACIOL | - | 11.1% (4) | ||
| Phaco +ACIOL | - | 5.56% (2) | ||
| Intra-op Complication | 2.4% (1) | 2.8% (1) | 1 | |
| Re-intervention | 6.6% (2) | 35.4% (17) | 0.006 | |
| Post-op complication | 0.000 | |||
| VH | - | 6.4% (3) | ||
| Vitreous in AC | - | 11.1% (4) | ||
| Decentered IOL | 3.33% (1) | 8.3% (3) | ||
| Optic capture | - | 2.8%(1) | ||
| VAO | - | 3.3% (1) | ||
| Endophthalmitis | - | 2.8% (1) | ||
| Transient IOP rise | 11.9% (5) | 8.3% (3) | ||
| CDVA last follow up (logMAR) | 0.49 ± 0.32 | 0.34 ± 0.27 | 0.025 |
UCVA- uncorrected visual acuity; CDVA- corrected distance visual acuity; MRSE- manifest refractive spherical equivalent; IOP- intra-ocular pressure; ILLA- intra-lenticular lens aspiration; SFIOL- scleral fixated intra-ocular lens; IOL-intra-ocular lens; ACIOL- anterior chamber intra-ocular lens; PPL- pars plana lensectomy; CTR- capsular tension ring; VH- vitreous hemorrhage; AC- anterior chamber; VAO- visual axis opacification
Hence, a better UCVA or CDVA at presentation would result in better post-operative visual outcomes. Also, a simultaneous IOL implantation at the time of primary surgery results in better visual outcomes and should therefore be preferred wherever feasible.
Various studies by different authors in the past have evaluated the visual outcome in cases of ectopia lentis undergoing surgery[5,9,10,11,12] [Table 3]. However, to the best of our knowledge, none of these studies have evaluated factors that predict the post-operative visual outcome in these cases. Herein, we have attempted to assess the pre-operative factors that predict the post-operative outcome in these cases.
Table 3.
Review of the literature
| Fan et al.[9] | Khokhar et al.[10] | Manning et al.[11] | Hsu et al.[5] | Catala-Mora et al.[12] | Current | |
|---|---|---|---|---|---|---|
| N (eyes) | 64 | 32 | 30 | 13 | 21 | 78 |
| M: F | 28/11 | 10/6 | 11/4 | 3/4 | 5/7 | 47/10 |
| Mean age (years) | 16.5 | 9.37 | 4.6 | 5.8 | 8 | 14.73 |
| Follow-up (months) | 36 | 3 | 13.8 yrs | 23.8 | 39.3 | 8.1±10.7 |
| Etiology | Marfan’s Syndrome 100% | Marfans-56.2% | Marfan’s syndrome- 100% | Familial ectopia lentis- 42.8% | Marfan syndrome - 58.3% | Marfan syndrome- 22.8% |
| Marfanoid habitus- 25% | Marfan syndrome- 42.8% | Idiopathic- 25% | Marfanoid habitus- 22.8% | |||
| Microspherophakia-18.7% | Idiopathic- 14.2% | Megalophthalmos-glaucoma-8.3% | WAGR syndrome- 1.7% | |||
| Ectopia lentis et pupillae- 8.3% | Homocystinuria- 1.7% | |||||
| Idiopathic - 51% | ||||||
| Mean extent of subluxation | Moderate- 65.6% | 7.11±1.44 clock hours | ||||
| Severe- 34.4% | ||||||
| Intervention | Lensectomy-vitrectomy, limbal 79.6%; pars-plana 20.4%, | Endocapsular lens aspiration | Pars-plana lensectomy | Limbal approach lensectomy vitrectomy and SFIOL (sutured) | 23 gauge PPV lensectomy artisan IOL | ILLA- 79.5% |
| lens aspiration- 14.1% | ||||||
| Phaco-aspiration- 2.6% | ||||||
| ICCE- 2.6% | ||||||
| PPL-1.3% | ||||||
| IOL implantation | 64.1% (SFIOL- 42.2%; ACIOL-28.1%) | 68.7% (all ACIOL) | 53.3% (Artisan aphakic iris fixated IOL) | 100% (SFIOL) | 85.7% (Artisan aphakic iris fixated IOL) | 46.2% (ACIOL-6, SFIOL- 21, PCIOL-9) |
| ECD loss | - | 7.1% | 15.4% | - | 5% | - |
| Corneal de-compensation | Nil | Nil | Nil | Nil | None | |
| Post-segment complications | RD - 17.2% | Nil | Nil | Nil | Mild VH- 28.5% | VH- 3.8% |
| RD- 4.7% | Endophthalmitis- 1.3% | |||||
| CME- 4.7% | ||||||
| Mean BCVA before surgery (LogMAR) | 0.5 | 0.6 | 0.66 | 0.86 | 0.91 | 0.85 |
| Mean BCVA after surgery (LogMAR) | 0.3 | 0.47 | 0.11 | 0.23 | 0.18 | 0.42 |
| AL (mm) | 26.2 | 25.3 | 24.29 | |||
| IOP rise | 3.1% | Nil | 3.3% | 7.7% | 10.3% | |
| Complications | IOL dislocation- 4.7% | IOL dislocation- 3.3% | Corectopia -38% (IOL incarceration- 2; vitreous in AC-1); optic capture - 31% | IOL dislocation with RD-1 | Vitreous in AC-5.1% | |
| Delefted IOL- 3.8% | ||||||
| Optic capture- 1.3% | ||||||
| VAO - 1.3% | ||||||
| Additional surgery/Procedure (n=eyes) | Nd-YAG capsulotomy- 1 | Nd-YAG capsulotomy- 1 | Vitrectomy with IOL refixation-1 case | Nd-YAG vitreolysis- 4 | ||
| IOL re-enclavation-1 | IOL explant with SFIOL-1 | |||||
| Secondary IOL -4 | IOL tapping with pupilloplasty-1, intravitreal antibiotic -1 | |||||
| Nd-YAG capsulotomy-1 | ||||||
| Comment | No difference in RD between aphakic and pseudo-phakic groups | No difference in CDVA between aphakic and pseudo-phakia groups | High incidence of amblyopia | No impact of age and extent of subluxation on post-operative CDVA. | ||
| Better visual outcome in the pseudo-phakia group. |
SFIOL- scleral fixated intra-ocular lens; PPV- pars-plana vitrectomy; IOL-intra-ocular lens; ILLA- intra-lenticular lens aspiration; ICCE- intra-capsular cataract extraction; PPL- pars-plana lensectomy; ACIOL- anterior chamber intra-ocular lens; PCIOL- posterior chamber intra-ocular lens; VA-visual acuity; RD- retinal detachment; VH- vitreous hemorrhage; CME- cystoid macular edema; AC- anterior chamber; VAO- visual axis opacification
The study has several limitations, including that of the retrospective nature and a shorter follow-up. Also, the surgeries were performed by different surgeons who differed in their experience. Besides, minute details of the surgery were not available in all the cases. All these could have had some impact on the outcome of this study. However, considering the rarity of this condition, we believe that the results of this study will supplement the available literature.
Conclusion
Hence, it can be concluded from the above discussion that both UCVA and CDVA should be considered as essential criteria when assessing cases of ectopia lentis and deciding for surgery in these cases. The age at the time of surgery has no impact on the final visual outcome if visual rehabilitation with spectacles has been performed during the period of plasticity. IOL implantation should be performed in all cases, if feasible, for the best visual outcome; however, a careful and vigilant follow-up is necessary to manage the post-operative complications which are higher in the pseudo-phakic eyes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nelson LB, Maumenee IH. Ectopia lentis. Surv Ophthalmol. 1982;27:143–60. doi: 10.1016/0039-6257(82)90069-8. [DOI] [PubMed] [Google Scholar]
- 2.Neely DE, Plager DA. Management of ectopia lentis in children. Ophthalmol Clin North Am. 2001;14:493–9. doi: 10.1016/s0896-1549(05)70247-9. [DOI] [PubMed] [Google Scholar]
- 3.Simon MA, Origlieri CA, Dinallo AM, Forbes BJ, Wagner RS, Guo S. New management strategies for ectopia lentis. J Pediatr Ophthalmol Strabismus. 2015;52:269–81. doi: 10.3928/01913913-20150714-02. [DOI] [PubMed] [Google Scholar]
- 4.Sinha R, Sharma N, Vajpayee RB. Intralenticular bimanual irrigation:Aspiration for subluxated lens in Marfan's syndrome. J Cataract Refract Surg. 2005;31:1283–6. doi: 10.1016/j.jcrs.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 5.Hsu HY, Edelstein SL, Lind JT. Surgical management of non-traumatic pediatric ectopia lentis:A case series and review of the literature. Saudi J Ophthalmol. 2012;26:315–21. doi: 10.1016/j.sjopt.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shortt AJ, Lanigan B, O'Keefe M. Pars plana lensectomy for the management of ectopia lentis in children. J Pediatr Ophthalmol Strabismus. 2004;41:289–94. doi: 10.3928/01913913-20040901-03. [DOI] [PubMed] [Google Scholar]
- 7.Sahay P, Shaji KR, Maharana PK, Titiyal JS. Spontaneous anterior dislocation of lens in a case of ectopia lentis et pupillae:A rare entity treated by a novel technique of Microscope integrated optical coherence tomography (MIOCT) guided intralenticular lens aspiration. BMJ Case Rep. 2019;12 doi: 10.1136/bcr-2018-227047. bcr-2018-227047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahay P, Maharana PK, Shaikh N, Goel S, Sinha R, Agarwal T, et al. Intra-lenticular lens aspiration in paediatric cases with anterior dislocation of lens. Eye (Lond) 2019;33:1411–7. doi: 10.1038/s41433-019-0426-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khokhar S, Aron N, Yadav N, Pillay G, Agarwal E. Modified technique of endocapsular lens aspiration for severely subluxated lenses. Eye (Lond) 2018;32:128–35. doi: 10.1038/eye.2017.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manning S, Lanigan B, O'Keefe M. Outcomes after lensectomy for children with Marfan syndrome. J AAPOS. 2016;20:247–51. doi: 10.1016/j.jaapos.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Fan F, Luo Y, Liu X, Lu Y, Zheng T. Risk factors for postoperative complications in lensectomy-vitrectomy with or without intraocular lens placement in ectopia lentis associated with Marfan syndrome. Br J Ophthalmol. 2014;98:1338–42. doi: 10.1136/bjophthalmol-2013-304144. [DOI] [PubMed] [Google Scholar]
- 12.Català-Mora J, Cuadras D, Díaz-Cascajosa J, Castany-Aregall M, Prat-Bartomeu J, García-Arumí J. Anterior iris-claw intraocular lens implantation for the management of nontraumatic ectopia lentis:Long-term outcomes in a paediatric cohort. Acta Ophthalmol. 2017;95:170–4. doi: 10.1111/aos.13192. [DOI] [PubMed] [Google Scholar]