Abstract
BACKGROUND
Fetal posterior cerebral artery occlusion is rare and often presents with severe neurological symptoms. Although acute recanalization therapy is commonly used for cerebral vessel occlusion, unruptured cerebral aneurysms can be hidden distal to the occluded vessels.
OBSERVATIONS
An 87-year-old man presented with consciousness disturbance and right hemiparesis. The authors diagnosed left fetal posterior cerebral artery occlusion and performed mechanical thrombectomy. A stent retriever was deployed from the middle cerebral artery M1 segment across the mural thrombus of the internal carotid artery. After the first pass, the fetal posterior cerebral artery remained occluded, with confirmation of a contrast effect around the thrombus. Because the anatomical course of the fetal posterior cerebral artery was unidentified, the procedure was stopped. At 1-week recovery, magnetic resonance imaging revealed complete recanalization and a fetal posterior cerebral artery aneurysm hidden within the occluded site. Blood flow was directed to the aneurysm, and the thrombus within the aneurysm simultaneously occluded the fetal posterior cerebral artery.
LESSONS
To avoid critical complications following mechanical thrombectomy for fetal posterior cerebral artery occlusion, hidden aneurysms should be suspected when a “fried egg–like” contrast effect is observed around the thrombus.
Keywords: mechanical thrombectomy, fetal posterior cerebral artery occlusion, posterior communicating artery, cerebral aneurysm, hidden aneurysm
ABBREVIATIONS : FPCA = fetal posterior cerebral artery, FPCO = fetal posterior cerebral artery occlusion, ICA = internal carotid artery, MCA = middle cerebral artery, MRI = magnetic resonance imaging, MT = mechanical thrombectomy, PCA = posterior cerebral artery
A fetal posterior cerebral artery (FPCA) is defined by continuation of the posterior communicating artery to the P2 segment of the posterior cerebral artery (PCA), with a hypoplastic P1 segment.1 FPCA occlusion (FPCO) is rare but can cause severe neurological symptoms because the FPCA supplies the ipsilateral diencephalon and posterior lobe. Reperfusion therapy for large-vessel occlusion is well established clinically. Use of mechanical thrombectomy (MT) for an FPCO has also been reported.2 However, for safe use of MT, it is important to consider unruptured cerebral aneurysms, which can be hidden distal to the occluded vessels. Herein, we present a case of a hidden aneurysm that was confirmed at the occluded site after MT for an FPCO.
Illustrative Case
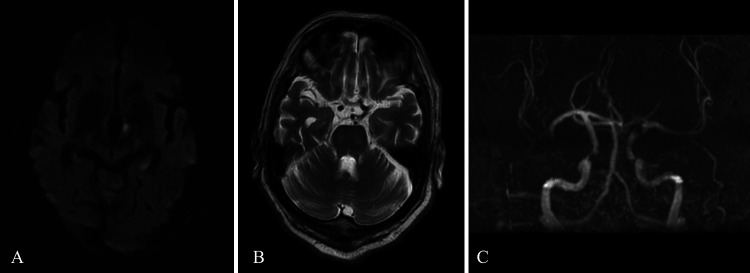
An 87-year-old man with a medical history of arterial fibrillation presented with consciousness disturbance and right hemiparesis. His initial National Institutes of Health Stroke Scale score was 17. Magnetic resonance imaging (MRI) showed infarction of the left hypothalamus and thalamus (Fig. 1A). A T2* sequence showed a susceptibility vessel sign at the left internal carotid artery (ICA). A T2-weighted sequence revealed a bold flow void along the course of the posterior communicating artery, and no aneurysm was detected (Fig. 1B). Magnetic resonance angiography showed a left ICA defect (Fig. 1C), with hypoplasia of the left PCA from the P1 segment. Cerebral angiography revealed a mural thrombus on the C2 segment of the left ICA (Fig. 2A). Thus, we diagnosed a left FPCO and performed MT.
FIG. 1.
Imaging findings on presentation. A: Admission MRI shows acute ischemic stroke of the left hypothalamus. B: T2-weighted MRI sequence shows a bold flow void along the course of the left posterior communicating artery. An aneurysm was not confirmed. C: Magnetic resonance angiography shows a left ICA defect.
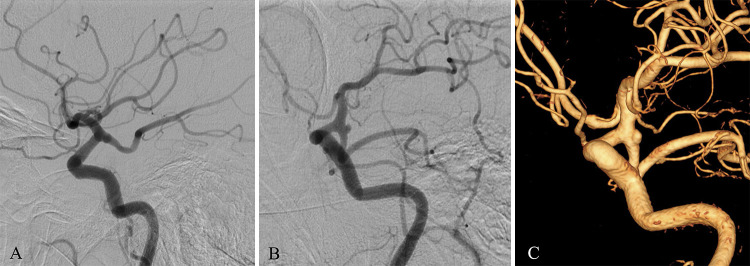
FIG. 2.
Intraprocedural angiographic findings. A: Preprocedural angiography shows a mural thrombus on the C2 segment of the ICA. B: A stent retriever was deployed from the M1 segment of the MCA across the mural thrombus. The aspiration catheter was inserted proximal to the thrombus. C: Angiography after the first pass shows a fried egg–like contrast effect around the thrombus. D: Antegrade and retrograde collateral flow from MCA to PCA territory was confirmed (arrowheads).
We were unable to insert a microcatheter into the FPCA, because the FPCA orifice was not detected. A microcatheter (Phenom 27, Medtronic) was advanced to the M1 segment of the middle cerebral artery (MCA) along a microwire (ASAHI CHIKAI 14, Asahi Intecc Co. Ltd.). We deployed a stent retriever (6 × 40 mm, Solitaire Platinum, Medtronic) from the M1 segment of the MCA across the mural thrombus. The stent retriever was withdrawn with an aspiration catheter (ACE 68, Penumbra Inc.) inserted just proximal to the thrombus (Fig. 2B). Although a red thrombus was removed, the FPCA remained occluded.
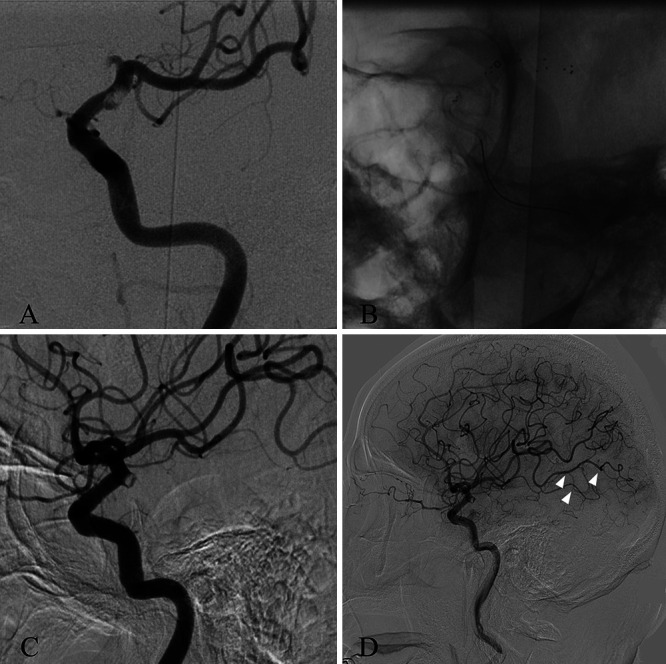
Intraoperative angiography after the first pass detected the FPCA orifice. A “fried egg–like” contrast effect was observed around the thrombus, which differed from the general findings of embolic vessel occlusion (e.g., the “claw sign”) (Fig. 2C). Because the anatomical course of the FPCA was unidentified and collateral flow to the ipsilateral PCA territory was confirmed (Fig. 2D), the procedure was ended. After MT, the patient’s National Institutes of Health Stroke Scale score was improved to 11. At 1 week after the procedure, MRI revealed complete recanalization and an unruptured FPCA aneurysm at the occluded site. Follow-up digital subtraction angiography showed the anatomical relationship between the aneurysm and the FPCA (Fig. 3A–C).
FIG. 3.
Follow-up angiographic findings. A: Cerebral angiography shows an FPCA aneurysm that was hidden in the occlusion site. The aneurysm and the FPCA were not separated in the angiographic working projection. B and C: Blood flow was directed to the aneurysm. The aneurysm orifice was located on the FPCA.
Discussion
Observations
We report a rare case of an FPCO with a hidden unruptured cerebral aneurysm. The fried egg–like contrast effect is an important finding for detecting a hidden aneurysm. The prevalence of hidden aneurysms was reported to be 3.7%.3 A few studies have also reported critical complications associated with rupture of hidden aneurysms due to mechanical stimulation of the stent retriever or thrombolysis.4,5 Hidden cerebral aneurysms are frequently bifurcating (e.g., of the MCA and basilar artery tip), which is likely because blood flow is directed toward the aneurysms.4 As such, sidewall-type hidden aneurysms are rare. A case of a sidewall-type ICA aneurysm hidden distal to the ICA occlusion was previously reported.6 However, to our knowledge, there are no reports of an FPCO in which the thrombus located within the ICA aneurysm secondarily occluded the FPCA. Thus, clinicians should be aware of hidden aneurysms at the occluded site when performing MT for FPCO.
It is rare for a thrombus to occlude only the FPCA, which is a sidewall branch of the ICA. The posterior communicating artery originates from the posterior wall of the C2 segment of the ICA and runs posterior medially to anastomose with the ipsilateral PCA. According to flow dynamics and the thrombus trajectory, FPCO alone is improbable.7 Nevertheless, Matz et al.8 reported a case of FPCO caused by changes in flow dynamics, which involved increasing blood flow to the FPCA with ipsilateral chronic MCA occlusion. In the present case, the C2 to C1 segments of the left ICA were positioned more upright than normal, and the FPCA originated vertically from the ICA. The aneurysm was located on the FPCA, and blood flow was directed to the aneurysm rather than to the MCA or the FPCA. Thus, the thrombus was located within the aneurysm and also occluded the FPCA.
At initial angiography of the present case, it was impossible to detect the hidden aneurysm because the FPCA was completely occluded. For an FPCA with a tortuous course, catheter insertion distal to the FPCA is often difficult. In many cases of FPCO with a catheter introduced into the FPCA, the running course of the FPCA was at least partially confirmed.9 In the present case, we deployed a stent retriever from the MCA across the mural thrombus. Angiography after the first pass showed a fried egg–like contrast effect, which represents an aneurysmal dome that is slightly larger than the thrombus. In the present case, the hidden aneurysm was actually small, but the thrombus was fitted across both the FPCA and the aneurysm, so a fried egg–like contrast effect appeared. Additionally, because the aneurysm and the FPCA were not separated on the angiographic working projection, catheter insertion may have perforated the aneurysm. Although we were not aware of a hidden aneurysm in the occluded site when performing MT, the microcatheter was not inserted distal to the FPCA. The procedure was ended because the fried egg–like contrast effect, which was not observed in the single vessel embolic occlusion, was confirmed, and fortunately the collateral flow from MCA to PCA territory was confirmed. If a hidden aneurysm is suspected, three-dimensional digital subtraction angiography should be considered. The fried egg–like contrast effect is an angiographic sign suggestive of a hidden aneurysm, which is different from the characteristic “claw sign” observed in embolic stroke.10 Detection of this sign is important for avoiding critical complications associated with MT in patients with hidden aneurysms.
Lessons
Because the ICA-FPCA bifurcation is the common site of cerebral aneurysms, an FPCO can coexist with a hidden aneurysm. To avoid a critical complication in MT for FPCO, a hidden aneurysm should be suspected when a contrast effect is observed around the thrombus.
Acknowledgments
We thank Daisuke Mori, Tamio Ito, and Yoshihiro Sumi for their support. We also thank Edanz for editing a draft of the manuscript.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Ishikawa, Endo, Shindo. Acquisition of data: Ishikawa, Endo. Analysis and interpretation of data: Ishikawa, Endo, Nomura. Drafting the article: Ishikawa, Endo. Critically revising the article: Ishikawa, Endo, Shindo, Nomura. Reviewed submitted version of manuscript: Ishikawa, Endo, Nomura. Approved the final version of the manuscript on behalf of all authors: Ishikawa. Administrative/technical/material support: Endo, Shindo, Nomura. Study supervision: Endo, Oka, Nakamura.
References
- 1. Shaban A, Albright KC, Boehme AK, Martin-Schild S. Circle of Willis variants: fetal PCA. Stroke Res Treat. 2013;2013:105937. doi: 10.1155/2013/105937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Abdalkader M, Sahoo A, Dmytriw AA, et al. Mechanical thrombectomy of the fetal posterior cerebral artery. Stroke Vasc Interv Neurol. 2021;1:e000115. [Google Scholar]
- 3. Zibold F, Kleine JF, Zimmer C, Poppert H, Boeckh-Behrens T. Aneurysms in the target vessels of stroke patients subjected to mechanical thrombectomy: prevalence and impact on treatment. J Neurointerv Surg. 2016;8(10):1016–1020. doi: 10.1136/neurintsurg-2015-012079. [DOI] [PubMed] [Google Scholar]
- 4. Torikoshi S, Akiyama Y. A concealed intracranial aneurysm detected after recanalization of an occluded vessel: a case report and literature review. Intervent Neurol. 2016;4(3–4):90–95. doi: 10.1159/000443220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nozaki T, Noda M, Ishibashi T, Morita A. Ruptured hidden intracranial aneurysm during mechanical thrombectomy: a case report. Surg Neurol Int. 2020;11:446. doi: 10.25259/SNI_789_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saito N, Hayashi N, Okubo T, et al. Internal carotid artery aneurysm visualized during successful endovascular treatment of carotid embolism. AJNR Am J Neuroradiol. 2000;21(3):546–548. [PMC free article] [PubMed] [Google Scholar]
- 7. Ryu JC, Kim JS. Mechanisms of stroke in patients with fetal posterior cerebral artery. J Stroke Cerebrovasc Dis. 2022;31(8):106518. doi: 10.1016/j.jstrokecerebrovasdis.2022.106518. [DOI] [PubMed] [Google Scholar]
- 8. Matz K, Apetroe A, Chemelli A, Brunner C, Nasel C. Flow dynamics in acute ischemic stroke due to embolic occlusion of a fetal posterior cerebral artery treated with endovascular thrombectomy - report of two cases. Radiol Case Rep. 2022;17(5):1727–1733. doi: 10.1016/j.radcr.2022.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abdalkader M, Sahoo A, Shulman JG, et al. Acute occlusion of the fetal posterior cerebral artery: diagnosis and management paradigms. Neuroradiol J. doi: 10.1177/19714009211019383. Published online June 6, 2021. doi: 10.1177/19714009211019383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yamamoto Y, Yamamoto N, Kanematsu Y, et al. The claw sign: an angiographic predictor of recanalization after mechanical thrombectomy for cerebral large vessel occlusion. J Stroke Cerebrovasc Dis. 2019;28(6):1555–1560. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.007. [DOI] [PubMed] [Google Scholar]