Abstract
Aim and Objective:
Our study was an observational and evolutional to analyze the significance of orbital volume calculation in predicting the probability or tendency of developing late enopthalmous on patients with unilateral orbital fracture with or without associated midface injury reported to our hospital.
Materials and Methods:
The subjects in our study included fifteen patients between18 and 60years. They were treated surgically and conservatively. Patients were exposed to series of examination from the day of injury or reporting for a consecutive period of up to six months following injury. CT was taken prior to treatment following management to evaluate the volume change in orbit. Its correlation and significance to treatment outcome were analyzed using MIMICS software by Materialise by comparing injured orbit to opposite side normal eye.
Result:
Conclusive of clinical examination and summary of statistical analysis patients were categorized into three groups: Low (with volume change of less than 2%), Medium (volume change between 2 to 20%) and High (volume change more than 20%) by comparing fractured orbit to uninjured orbit and a statistically significant mean value of 27.7 ± 2.6 cu. mm for fractures eye and 25.9 ± 2.6 cu. mm for normal eye was found (P ≤ 0.05).
Conclusion:
Orbital volume can be considered as useful criteria in evaluation of patients with orbital fracture. Evaluation and follow up in correlation with resultant volume assessment provide a better indicator for assessment of prognosis and enopthalmous. Unlike other methods for volume assessment MIMICS software by Materialise provide a better method and it can be incorporated to working station in hospital. Every CT assessment in orbital trauma should include orbital volume as a parameter and this software is easy and user-friendly software that does not require its technical knowledge for application.
Keywords: Enopthalmous, middle third face fracture, midface fracture, MIMICS, orbit, orbital volume, zygomaticomaxillary complex fracture
INTRODUCTION
Orbital fractures are observed in most maxillofacial traumas involving the fracture of the midface. Although the orbit is of limited extent, treatment is important because of its influence on esthetics and function. The complications following orbital wall fracture vary, and hence, its treatment is influenced by a varying number of factors. The most common features following orbital injury are limitation of ocular movements, diplopia, and enophthalmos. Surgical treatment is not always necessary in the treatment of orbital fracture (isolated or with associated injury), especially when other areas demand primary intervention to restore the airway and other functions. Orbital fracture patients with good ocular mobility and no significant enophthalmos may be conservatively managed and observed clinically.[1,2,3,4,5,6,7,8]
It is well established that early surgical intervention is preferable when there is entrapment of an extraocular muscle or when there are large defect or fracture, enophthalmos, and diplopia causing impaired ocular mobility.[9,10] The decision of addressing orbit is often challenging because of posttraumatic edema following a fracture and the presence of orbital emphysema that may cause underestimation of the amount of late enophthalmos, which may result in unnecessary intervention in cases that resolve in weeks following trauma.[11,12,13] However, in the primary, if surgery is delayed, it may result in unsatisfactory result. However, in patients with midface injury associated with orbital injury (with no blow out fracture), addressing the orbit along with other fractures can be bailing against the complication of enophthalmos at a later stage. Although not an indication, it is a necessity to stabilize a fracture in a certain condition (e.g., ZOC fracture). Hence, in this scenario, esthetics is also improved (by reducing the enophthalmos) and functional recouping is found to be better.
This study intends to focus on patients with unilateral orbital fracture (with or without associated midface injury) reported to our hospital. They are treated surgically or conservatively following thorough clinical and radiographic (computed tomography [CT]) evaluation, based on the study protocol. Later, a comparative analysis is done on the outcome of Management. This is done by comparingof injured orbit to the opposite side normal eye and this data is clinically correlated to patient's prognosis and surgical outcome. Patients are exposed to series of examination from the day of injury or from the day of reporting to a consecutive period of up to 6 months following injury and are analyzed. These patients are exposed to CT (before treatment to confirm the extent of injury and fracture) and postoperative CT following management to evaluate the volume change in the orbit and its significance to treatment outcome is analyzed.
MATERIALS AND METHODS
Patients included in this study were from September 2014 to May 2016 for 20 months. Eighteen patients were reported with a fracture of middle third of the face (including zygomatico-maxillary complex fracture, Lefort II fracture, Lefort 1 fracture combined with frontozygomatic fracture, and orbital rim fracture). Fifteen patients were included as they satisfied the proposed criteria.
Any patient with maxillofacial trauma with associated orbital fracture (unilateral) coming to our hospital under any age group with or without associated facial injury were included in the study.
Patients with bilateral orbital fractures, with a previous orbital injury with or without surgical intervention, with associated skull base injury with other neurological deficit, and with pre-existing ophthalmic or neurological disease were excluded from the study. Patient consent was obtained. Ethical committee clearance was obtained on 19/12/2014 from SRI Ramakrishna Dental College and Hospital Ethical Committee, with reference no. SRDCH0119.
Tool of database collection
A collection of demographic data, clinical data after patient evaluation which inclided clinical, radiographic and opthalmolagic evaluation while the patient is admitted to hospital or directly reported to dental college between 24 to within 48 hours after injury. On admission, confirmation that the patient has been symptomatic for less than 72 h and has unilateral orbital fracture was established using the inclusion criteria. Pain characteristics of orbital trauma assessment with clinical signs and symptoms were made (The attached data form containing demographic, clinical, and laboratory data and GCS score was taken within the first 24th and 48th h). Confirmation was made with CT. Patients were evaluated at 48th and 72nd h. Orbital evaluation and assessment were made with a set of preformed examination and charts for analyzing the ophthalmologic status of the patient which included inspection, palpation, and specific ophthalmoscopic examination. An ophthalmologist verified and confirmed these tests. A set of predetermined tests were carried out to rule out other soft tissue injuries and associated nerve injuries that did not confine to maxillofacial intervention. Appropriate management/intervention was initiated as per the study algorithm.
In suspected optic nerve injury, bolus of the steroid was administered initially, reassessment was made after the edema was reduced, and surgical intervention for open reduction and internal fixation was carried out if indicated (by the surgeon's choice).
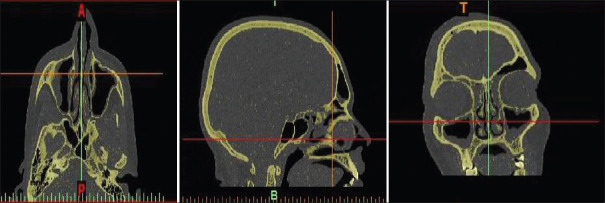
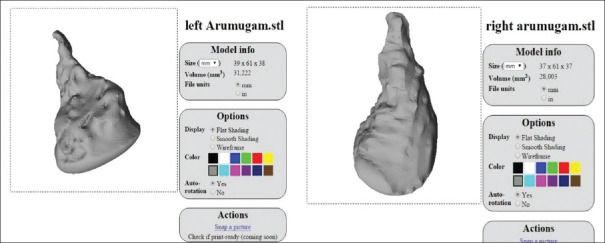
At discharge, the severity and clinical signs and symptoms were re-evaluated. Patients were recalled in consecutive days for a period of 3 weeks followed by regular monthly follow-up for 1.5 years (1 week, 1 month, and follow-up for 6 months up to 1.5 years) as an outpatient in our hospital or dental college. Specificity and sensitivity were calculated and statistically analyzed. The orbital volume and changes in the fractured orbit to the normal orbit with computer-aided software MIMICS by Materialise were used for this purpose [Figures 1-3] show the volume assessment obtained from CT]. MIMICS data were then compared and evaluated to the clinical assessment and the significance of orbital volume (hard tissue) restoration in restoring the function and esthetics.
Figure 1.
Axial, coronal, and sagittal view from computed tomography determining the extend of the three-dimensional image
Figure 3.
Separating the right and left orbit and estimating the volume
Figure 2.
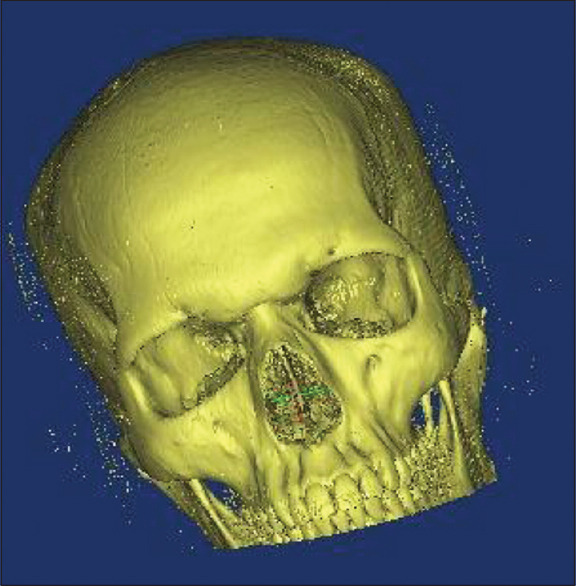
Three-dimensional image constructed from the computed tomography
RESULTS
The subjects in our study were inclusive of 15 patients, who were all male patients reported to our hospital. They were divided into Group A who were managed surgically and Group B patients who were treated conservatively.
Road traffic accidents were the etiologic factor for all of them [Table 1]. All patients who underwent surgery had GCS above 10 for surgery. The interval between trauma evaluation and surgery [Table 2] was 0–7 days and for those who have been treated conservatively [Table 3] was monitored for 5–7 days. The postsurgical or management evaluation was followed for a period of 6 months with a consecutive interval of 1 week for a period of 2 months, following which CT which was taken postoperatively was correlated with clinical evaluation and was monitored at an interval of 1 month for a period of 6 months. Patients included in the study were all males with mean age of 36.9333 ± 12.775 (18–60) years. Of the 15 patients, two patients developed an enophthalmos of 4 mm3 and 2 mm3, respectively. Mean orbital volume of normal orbit in all the patients was found to be 25.9 mm3 and the mean orbital volume of the fractured orbit was found to be 24.7 mm3 with no significant difference in orbital volume. And hence, all patients showed a satisfactory posttreatment result, except for two patients mentioned above. The difference between the normal orbital volume and fractured orbitals volume was determined, and the percentage of orbital expansion (increase in volume) was analyzed. On the data obtained, they were broadly classified into three groups as given below [Table 4 and Graph 1]:
Table 1.
Etiology of fracture in Group A and Group B patients
| Diagnosis | Count percentage within the group | Group A (n=6) | Group B (n=9) | Total (n=15) |
|---|---|---|---|---|
| Unilateral Lefort II | 40 | 3 | 3 | 6 |
| Panfacial trauma with orbital fracture | 6.67 | 1 | 0 | 1 |
| ZMC fracture | 33.33 | 1 | 4 | 5 |
| Isolated orbital fracture | 20 | 1 | 2 | 3 |
ZMC: Zygomaticomaxillary complex
Table 2.
Volume assessment in patients managed surgically
| Patient number | Volume of fractured orbit (mm3) | Volume of contralateral normal orbit (mm3) | Difference (mm3) |
|---|---|---|---|
| 1 | 23.735 | 24.079 | 0.344 |
| 2 | 18.374 | 18.374 | 0.00 |
| 3 | 23.501 | 23.500 | 0.001 |
| 4 | 19.128 | 21.508 | 2.380 |
| 5 | 28.436 | 27.925 | 0.511 |
| 6 | 19.618 | 30.146 | 10.528 |
| 7 | 25.677 | 30.714 | 5.037 |
| 8 | 27.393 | 26.986 | 0.407 |
| 9 | 22.641 | 19.191 | 3.450 |
Table 3.
Volume assessment in patients managed conservatively
| Patient number | Volume of fractured orbit (mm3) | Volume of contralateral normal orbit (mm3) | Difference (mm3) |
|---|---|---|---|
| 1 | 20.294 | 20.356 | 0.062 |
| 2 | 23.322 | 27.078 | 3.756 |
| 3 | 28.003 | 31.954 | 3.954 |
| 4 | 22.569 | 24.238 | 1.669 |
| 5 | 33.891 | 34.726 | 0.835 |
| 6 | 34.227 | 28.003 | 6.224 |
Table 4.
Classification patient in to low-, medium-, and high-expansion groups on percentage of volume change
| Orbital expansion | Total | |||
|---|---|---|---|---|
|
| ||||
| Low (<2%) | Medium (2%-20%) | High (>20%) | ||
| Enopthalmous | ||||
| Absent | ||||
| Count | 6 | 7 | 0 | 13 |
| Percentage within enopthalmous | 46.2 | 53.8 | 0.0 | 100.0 |
| Present | ||||
| Count | 0 | 0 | 2 | 2 |
| Percentage within enopthalmous | 0.0 | 0.0 | 100.0 | 100.0 |
| Total | ||||
| Count | 6 | 7 | 2 | 15 |
| Percentage within enopthalmous | 40.0 | 46.7 | 13.3 | 100.0 |
Graph 1.
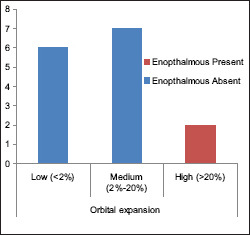
Graph depicting the number of patients and the percentage of rbital expansion (increase in volume) compared to the contralateral eye
Low (with volume change of less than 2%)
Medium (volume change between 2% and 20%)
High (volume change more than 20%).
Conclusive of clinical examination and summary of statistical analysis the result were summarized as:
Patients with the enlarged orbital volume of less than 2% were on the safe side and did not require any surgical intervention and have a minimum or relatively no tendency of developing late enophthalmos
Patients with volume enlargement from 2% to 20% required close evaluation and were at moderate risk of developing enophthalmos though most patients tend showed prognosis following resolution of edema and hematoma
Patients with the orbital expansion of more than 20% developed enophthalmos, and hence, preoperative assessment of this gross volume change was a suggestive indication for surgery to restore the orbital volume to minimize the complication of late enophthalmos.
DISCUSSION
Various authors have stated that there is no significance difference between the volume of right and left orbits, and therefore, it is logical to use the volume of uninjured orbit as control to compare the volume to contralateral injured orbit. However, an individual volume difference of 7%–8% can limit the comparison, as suggested by Forbes et al. in 1985.[18]
Orbital volume measurement provides valuable and significant data in analyzing the severity of the injury. This helps in the prevention of possible complications caused by enopthalmous after orbital fracture in maxillofacial trauma.[13] Various authors have suggested different methods for calculation of orbital volume from CT scan using stereolithography, manual segmentation, and geometric calculation with definite formulas from the area of interest.[14,15,16] Of all these methods though most of them were reliable. But they possessed challenges because of the time and tedious manual effort required in obtaining the data.[1,17,18,19] Regensburg et al.[3] conducted a study to investigate the purpose of MIMICS software to validate their technique in measuring orbital volume with intraobserver and interobserver variability using CT scans, and they found that the software to be very useful, because previously there was no consensus on how volume of orbit is calculated, with many authors validating different approaches.
MIMICS software by Materialise Company proves a very useful tool because it does not require any well to do knowledge about the software and can be used outside the radiology department. CD or DVD is used for loading images, can process any stacks of images, and is independent of scanner. In the study conducted by Regensburg et al.,[3] the intraobserver and interobserver variability was found to be less than 5%, and hence, MIMICS was found to be a more reliable to for this study. The three-dimensional reconstruction facility of this program enables the user to correct the segmentation, and hence, no technical knowledge is required. Most authors have suggested the use of axial sections. However, in our study, coronal, axial, and sagittal sections of the patients were taken to determine the extent of fracture on all dimensions.[4,5,6,7,8,20,21,22]
In our study, it was noted that patients with mild orbital expansion of less than 4 mm3 has less tendency for developing late enopthalmous in either groups managed surgically or conservatively. In patients with bony orbital viume enlargement of more than 5 mm3, there was enopthalmous of about 2 mm3. though this value is not large, patients with large volume expansion of fractured orbit with more than 10 mm3, it is advisable to consider surgical exploration for volume restoration and decompression.
Our study is an observational and evolutional study to analyze the significance of orbital volume calculation in predicting the probability or tendency of developing late enopthalmous and is not a prospective study and hence does not interfere with the decision-making in any of the patients. The intention of the study was to consider to scope of orbital volume as a parameter in patients, especially in unilateral orbital volume where the control orbit can be used as guidance in comparing the posttreatment outcome, to help in reducing the postoperative enopthalmous, and also in predicting the tendency to develop enopthalmous. This knowledge can help not only to guide the treatment and intervene at appropriate time but also to avoid unrequired intervention.
The following conclusions could be drawn from our study.
Orbital volume can be considered as useful criteria in evaluation of patients with orbital fracture
Evaluation and follow-up in correlation with resultant volume assessment provide a better indicator for assessment of prognosis and enopthalmous
In patients requiring early intervention, where initial assessment is difficult due to edema, orbital volume can be considered as a tool in decision-making along with other criteria
Evaluation of orbital volume avoids possibility of late intervention and helps in early management of patients with orbital fracture requiring immediate intervention
Postoperative long-term follow-up is reduced and more precision in predicting the surgical outcome that can cause enopthalmous
Conformation of surgical restoration of volume is possible in patients by comparing the volume of treated eye to the contralateral normal eye even before the actual surgery. This gives a better surgical planning, as the amount of volume to be restored is predetermined. Estimation of volume restored following treatment helps in predicting late enopthalmous. It is suggestive of evaluation before and after the surgery for the treated eye for better result
It is easy to use, and no patient involvement required
Unlike other methods for volume assessment, MIMICS software by Materialise provides a better method and it can be incorporated to working station in hospital
Every CT assessment in orbital trauma should include orbital volume as a parameter and this software is easy and user-friendly software that does not require its technical knowledge for application
The mean orbital volume of normal eye in our study population was 25.9 mm3
Although orbital volume assessment is a very promising evaluation criterion before intervention, clinical correlation with functional impairment needs to be correlated in decision-making
Restoration of hard tissue volume of the orbit is more significant in reducing enopthalmous and is under operator control, but intervention is not mandatory with a difference of less than 20%.
CONCLUSION
MIMICS software by Materialise Company proves a very useful tool because it does not require any well to do knowledge about the software and can be used outside the radiology department by any person with basic l knowlege of anatomical interpretation in CT.
Our study is an observational and evolutional study to analyze the significance of orbital volume calculation in predicting the probability or tendency of developing late enopthalmous and is not a prospective study and hence does not interfere with the decision making in any of the patients. The intention of the study was to consider to scope of orbital volume as a parameter in patients, especially in unilateral orbital volume where the control orbit can be used as aguidancein comparing the post treatment outcome, to help in reducing the post-operative enopthalmous and also in predicting the tendency to develop enopthalmous. This knowledge can help in guiding the treatment and intervene at appropriate time but also to avoid unrequired intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ahn HB, Ryu WY, Yoo KW, Park WC, Rho SH, Lee JH, et al. Prediction of enophthalmos by computer-based volume measurement of orbital fractures in a Korean population. Ophthalmic Plast Reconstr Surg. 2008;24:36–9. doi: 10.1097/IOP.0b013e31815eb7ce. [DOI] [PubMed] [Google Scholar]
- 2.Saiepour D, Messo E, Hedlund AJ, Nowinski DJ. Radiologic and long-term clinical outcome from treatment of isolated medial orbital wall blowout fractures. J Craniofac Surg. 2012;23:1252–5. doi: 10.1097/SCS.0b013e31825e4e8e. [DOI] [PubMed] [Google Scholar]
- 3.Regensburg NI, Kok PH, Zonneveld FW, Baldeschi L, Saeed P, Wiersinga WM, et al. A new and validated CT-based method for the calculation of orbital soft tissue volumes. Invest Ophthalmol Vis Sci. 2008;49:1758–62. doi: 10.1167/iovs.07-1030. [DOI] [PubMed] [Google Scholar]
- 4.Charteris DG, Chan CH, Whitehouse RW, Noble JL. Orbital volume measurement in the management of pure blowout fractures of the orbital floor. Br J Ophthalmol. 1993;77:100–2. doi: 10.1136/bjo.77.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris GJ, Garcia GH, Logani SC, Murphy ML, Sheth BP, Seth AK. Orbital blow-out fractures: Correlation of preoperative computed tomography and postoperative ocular motility. Trans Am Ophthalmol Soc. 1998;96:329–47. [PMC free article] [PubMed] [Google Scholar]
- 6.Bite U, Jackson IT, Forbes GS, Gehring DG. Orbital volume measurements in enophthalmos using three-dimensional CT imaging. Plast Reconstr Surg. 1985;75:502–8. doi: 10.1097/00006534-198504000-00009. [DOI] [PubMed] [Google Scholar]
- 7.McGurk M, Whitehouse RW, Taylor PM, Swinson B. Orbital volume measured by a low-dose CT scanning technique. Dentomaxillofac Radiol. 1992;21:70–2. doi: 10.1259/dmfr.21.2.1397459. [DOI] [PubMed] [Google Scholar]
- 8.Jansen J, Schreurs R, Dubois L, Maal TJ, Gooris PJ, Becking AG. Orbital volume analysis: Validation of a semi-automatic software segmentation method. Int J Comput Assist Radiol Surg. 2016;11:11–8. doi: 10.1007/s11548-015-1254-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koo L, Hatton MP, Rubin PA. When is enophthalmos “significant”? Ophthalmic Plast Reconstr Surg. 2006;22:274–7. doi: 10.1097/01.iop.0000226865.22184.6a. [DOI] [PubMed] [Google Scholar]
- 10.Parsons GS, Mathog RH. Orbital wall and volume relationships. Arch Otolaryngol Head Neck Surg. 1988;114:743–7. doi: 10.1001/archotol.1988.01860190047020. [DOI] [PubMed] [Google Scholar]
- 11.Putterman AM, Stevens T, Urist MJ. Nonsurgical management of blow-out fractures of the orbital floor. Am J Ophthalmol. 1974;77:232–9. doi: 10.1016/0002-9394(74)90679-5. [DOI] [PubMed] [Google Scholar]
- 12.Hartstein ME, Roper-Hall G. Update on orbital floor fractures: Indications and timing for repair. Facial Plast Surg. 2000;16:95–106. doi: 10.1055/s-2000-12571. [DOI] [PubMed] [Google Scholar]
- 13.Kwon J, Barrera JE, Jung TY, Most SP. Measurements of orbital volume change using computed tomography in isolated orbital blowout fractures. Arch Facial Plast Surg. 2009;11:395–8. doi: 10.1001/archfacial.2009.77. [DOI] [PubMed] [Google Scholar]
- 14.Kwon J, Barrera JE, Most SP. Comparative computation of orbital volume from axial and coronal CT using three-dimensional image analysis. Ophthalmic Plast Reconstr Surg. 2010;26:26–9. doi: 10.1097/IOP.0b013e3181b80c6a. [DOI] [PubMed] [Google Scholar]
- 15.Manson PN, Grivas A, Rosenbaum A, Vannier M, Zinreich J, Iliff N. Studies on enophthalmos: II. The measurement of orbital injuries and their treatment by quantitative computed tomography. Plast Reconstr Surg. 1986;77:203–14. [PubMed] [Google Scholar]
- 16.Ploder O, Klug C, Voracek M, Burggasser G, Czerny C. Evaluation of computer-based area and volume measurement from coronal computed tomography scans in isolated blowout fractures of the orbital floor. J Oral Maxillofac Surg. 2002;60:1267–72. doi: 10.1053/joms.2002.35722. [DOI] [PubMed] [Google Scholar]
- 17.Wi JM, Sung KH, Chi M. ‘Orbital volume restoration rate after orbital fracture’; a CT-based orbital volume measurement for evaluation of orbital wall reconstructive effect. Eye (Lond) 2017;31:713–9. doi: 10.1038/eye.2016.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forbes G, Gehring DG, Gorman CA, Brennan MD, Jackson IT. Volume measurements of normal orbital structures by computed tomographic analysis. AJR Am J Roentgenol. 1985;145:149–54. doi: 10.2214/ajr.145.1.149. [DOI] [PubMed] [Google Scholar]
- 19.Choi SH, Kang DH. Prediction of late enophthalmos using preoperative orbital volume and fracture area measurements in blowout fracture. J Craniofac Surg. 2017;28:1717–20. doi: 10.1097/SCS.0000000000003765. [DOI] [PubMed] [Google Scholar]
- 20.Raskin EM, Millman AL, Lubkin V, della Rocca RC, Lisman RD, Maher EA. Prediction of late enophthalmos by volumetric analysis of orbital fractures. Ophthalmic Plast Reconstr Surg. 1998;14:19–26. doi: 10.1097/00002341-199801000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Schuknecht B, Carls F, Valavanis A, Sailer HF. CT assessment of orbital volume in late post-traumatic enophthalmos. Neuroradiology. 1996;38:470–5. doi: 10.1007/BF00607281. [DOI] [PubMed] [Google Scholar]
- 22.Gellrich NC, Schramm A, Hammer B, Rojas S, Cufi D, Lagrèze W, et al. Computer-assisted secondary reconstruction of unilateral posttraumatic orbital deformity. Plast Reconstr Surg. 2002;110:1417–29. doi: 10.1097/01.PRS.0000029807.35391.E5. [DOI] [PubMed] [Google Scholar]