Abstract
Background
Long‐acting beta2‐agonists (LABA) in combination with inhaled corticosteroids (ICS) are increasingly prescribed for children with asthma.
Objectives
To assess the safety and efficacy of adding a LABA to an ICS in children and adolescents with asthma. To determine whether the benefit of LABA was influenced by baseline severity of airway obstruction, the dose of ICS to which it was added or with which it was compared, the type of LABA used, the number of devices used to deliver combination therapy and trial duration.
Search methods
We searched the Cochrane Airways Group Asthma Trials Register until January 2015.
Selection criteria
We included randomised controlled trials testing the combination of LABA and ICS versus the same, or an increased, dose of ICS for at least four weeks in children and adolescents with asthma. The main outcome was the rate of exacerbations requiring rescue oral steroids. Secondary outcomes included markers of exacerbation, pulmonary function, symptoms, quality of life, adverse events and withdrawals.
Data collection and analysis
Two review authors assessed studies independently for methodological quality and extracted data. We obtained confirmation from trialists when possible.
Main results
We included in this review a total of 33 trials representing 39 control‐intervention comparisons and randomly assigning 6381 children. Most participants were inadequately controlled on their current ICS dose. We assessed the addition of LABA to ICS (1) versus the same dose of ICS, and (2) versus an increased dose of ICS.
LABA added to ICS was compared with the same dose of ICS in 28 studies. Mean age of participants was 11 years, and males accounted for 59% of the study population. Mean forced expiratory volume in one second (FEV1) at baseline was ≥ 80% of predicted in 18 studies, 61% to 79% of predicted in six studies and unreported in the remaining studies. Participants were inadequately controlled before randomisation in all but four studies.
There was no significant group difference in exacerbations requiring oral steroids (risk ratio (RR) 0.95, 95% confidence interval (CI) 0.70 to 1.28, 12 studies, 1669 children; moderate‐quality evidence) with addition of LABA to ICS compared with ICS alone. There was no statistically significant group difference in hospital admissions (RR 1.74, 95% CI 0.90 to 3.36, seven studies, 1292 children; moderate‐quality evidence)nor in serious adverse events (RR 1.17, 95% CI 0.75 to 1.85, 17 studies, N = 4021; moderate‐quality evidence). Withdrawals occurred significantly less frequently with the addition of LABA (23 studies, 471 children, RR 0.80, 95% CI 0.67 to 0.94; low‐quality evidence). Compared with ICS alone, addition of LABA led to significantly greater improvement in FEV1 (nine studies, 1942 children, inverse variance (IV) 0.08 L, 95% CI 0.06 to 0.10; mean difference (MD) 2.99%, 95% CI 0.86 to 5.11, seven studies, 534 children; low‐quality evidence), morning peak expiratory flow (PEF) (16 studies, 3934 children, IV 10.20 L/min, 95% CI 8.14 to 12.26), reduction in use of daytime rescue inhalations (MD ‐0.07 puffs/d, 95% CI ‐0.11 to ‐0.02, seven studies; 1798 children) and reduction in use of nighttime rescue inhalations (MD ‐0.08 puffs/d, 95% CI ‐0.13 to ‐0.03, three studies, 672 children). No significant group difference was noted in exercise‐induced % fall in FEV1, symptom‐free days, asthma symptom score, quality of life, use of reliever medication and adverse events.
A total of 11 studies assessed the addition of LABA to ICS therapy versus an increased dose of ICS with random assignment of 1628 children. Mean age of participants was 10 years, and 64% were male. Baseline mean FEV1 was ≥ 80% of predicted. All trials enrolled participants who were inadequately controlled on a baseline inhaled steroid dose equivalent to 400 µg/d of beclomethasone equivalent or less.
There was no significant group differences in risk of exacerbation requiring oral steroids with the combination of LABA and ICS versus a double dose of ICS (RR 1.69, 95% CI 0.85 to 3.32, three studies, 581 children; moderate‐quality evidence) nor in risk of hospital admission (RR 1.90, 95% CI 0.65 to 5.54, four studies, 1008 children; moderate‐quality evidence).
No statistical significant group difference was noted in serious adverse events (RR 1.54, 95% CI 0.81 to 2.94, seven studies, N = 1343; moderate‐quality evidence) and no statistically significant differences in overall risk of all‐cause withdrawals (RR 0.96, 95% CI 0.67 to 1.37, eight studies, 1491 children; moderate‐quality evidence). Compared with double the dose of ICS, use of LABA was associated with significantly greater improvement in morning PEF (MD 8.73 L/min, 95% CI 5.15 to 12.31, five studies, 1283 children; moderate‐quality evidence), but data were insufficient to aggregate on other markers of asthma symptoms, rescue medication use and nighttime awakening. There was no group difference in risk of overall adverse effects, A significant group difference was observed in linear growth over 12 months, clearly indicating lower growth velocity in the higher ICS dose group (two studies: MD 1.21 cm/y, 95% CI 0.72 to 1.70).
Authors' conclusions
In children with persistent asthma, the addition of LABA to ICS was not associated with a significant reduction in the rate of exacerbations requiring systemic steroids, but it was superior for improving lung function compared with the same or higher doses of ICS. No differences in adverse effects were apparent, with the exception of greater growth with the use of ICS and LABA compared with a higher ICS dose. The trend towards increased risk of hospital admission with LABA, irrespective of the dose of ICS, is a matter of concern and requires further monitoring.
Plain language summary
Addition of long‐acting beta2‐agonists to inhaled corticosteroids for chronic asthma in children
Background
Most consensus statements recommend use of long‐acting beta2‐agonists (LABA) as adjunct therapy to inhaled corticosteroids (ICS) for poorly controlled asthma, despite the use of low‐dose ICS.
Review question
What are the benefits and safety of the combination of LABA and ICS in children with persistent asthma when compared with the same dose or a higher dose of ICS alone?
What evidence did we find?
From available evidence until January 2015, we found 39 eligible studies evaluating the combination of LABA and ICS in children with persistent asthma. Of these, 28 studies compared LABA with the same dose of ICS, and the remaining studies compared LABA with a larger dose of ICS.
The number of people who had an exacerbation (worsening of symptoms) that required treatment with oral steroids was not significantly different. However, lung function improved in people taking LABA and steroids compared with the same dose of steroids only or larger doses of steroids. No evidence suggested increased serious adverse events or adverse events (also known as side effects) with the addition of LABA.
Compared with the same dose of ICS, people used less of their rescue/relief bronchodilator treatment. There was no benefit for control of asthma symptoms when LABA added to ICS was compared with higher doses of ICS. The higher dose of ICS was associated with 1.2 cm per year lower growth than was observed with the combination of LABA and a lower dose of ICS.
Conclusion
In children with persistent asthma, the combination of LABA and ICS did not reduce the risk of exacerbations requiring steroid treatment but did improve lung function when compared with the same, or a higher, dose of ICS. No differences in adverse effects were apparent, with the exception of better growth with use of ICS and LABA compared with a higher ICS dose. The trend towards increasing chances of hospital admission indicates the need for continuous monitoring and additional trials in children.
Quality of the evidence
Overall, we judged the quality of evidence to be moderate. Most outcomes showed wide confidence intervals, which led to downgrading of the quality of evidence to moderate. In a few outcomes for which open‐label studies contributed data, we further downgraded evidence quality to low.
Summary of findings
Background
Description of the condition
Inhaled corticosteroids (ICS) are the most effective treatment for long‐term control of asthma in children (Adams 2005; Manning 2008; Adams 2008a; Chauhan 2012). They are recommended as first‐line agents for the management of childhood asthma in all national and international consensus statements (NAEPP 2011; Lougheed 2012; BTS 2014; GINA 2015). When ICS alone are insufficient to achieve asthma control, various options may be considered, such as increasing the dose of ICS (Adams 2008b) or adding a second drug such as a long‐acting beta2‐agonist (LABA) or a leukotriene receptor antagonist (LTRA) (Chauhan 2014).
Description of the intervention
In adults with unsatisfactory asthma control, international guidelines clearly favour the addition of LABA to low or moderate doses of ICS over other options such as increasing the dose of steroids or adding other agents (NAEPP 2011; BTS 2014; GINA 2015). In children five to 12 years of age with insufficient control on ICS, however, recommendations regarding the preferred step 3 strategy and the dose of ICS to which LABA should be added differ markedly across countries. The International Australian and Canadian guidelines recommend increasing the dose of ICS to medium dose (201 to 400 μg beclomethasone equivalent) rather than adding LABA or LTRA to low‐dose ICS in children six to 11 years of age (Lougheed 2012; NAC Guidelines 2014). British Thoracic Society guidelines recommend combination therapy at a low dose (200 to 400 µg/d beclomethasone equivalent) (BTS 2014). Global Initiative for Asthma (GINA) and Australian guidelines recommend increasing the dose of ICS over adding LABA to a higher dose of ICS (400 µg/d) (NAC Guidelines 2014; GINA 2015). American guidelines reveal no clear preference for adding LABA to a low dose of ICS or increasing the dose of ICS for children five to 11 years of age with uncontrolled asthma and taking a low dose of ICS (NAEPP 2011). No formal recommendation is available for their use in preschool‐age children.
How the intervention might work
Data from paediatric clinical trials have been included in few previous meta‐analyses assessing the efficacy and safety of LABA in combination with ICS (Ducharme 2010; Ducharme 2010a). However, Bisgaard 2003 cautioned against routine use of LABA in children, as they did not offer protection against exacerbations and led to increased risk of hospital admission. Other outcomes such as adverse effects, lung function and symptoms were not examined.
Why it is important to do this review
The wide divergence of recommendations likely stems from lack of solid evidence in children to support international asthma guidelines and justifies a systematic review of the topic. In 2010, we published a Cochrane review conducted to compare LABA added to ICS of the same dose, or a higher dose, for adults and children with chronic persistent asthma, which demonstrated that LABA and ICS led to a significant reduction in risk of exacerbations requiring oral steroids (Ducharme 2010; Ducharme 2010a). The Cochrane Collaboration had published a separate paediatric systematic review on the same topic in the year 2009 (Ni Chroinin 2009). Since that time, additional published and unpublished paediatric trials have become available, enabling us to update the review to include newly available evidence and to shed more light on the role of LABA as adjunct therapy to ICS for children with partial control when taking ICS alone.
Objectives
To assess the safety and efficacy of adding a LABA to an ICS in children and adolescents with asthma. To determine whether the benefit of LABA was influenced by baseline severity of airway obstruction, the dose of ICS to which it was added or with which it was compared, the type of LABA used, the number of devices used to deliver combination therapy and trial duration.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials conducted in children for whom a LABA was added to an ICS were eligible.
Types of participants
Children and adolescents two to 18 years of age with persistent asthma who had received daily ICS therapy for at least four weeks before study entry.
Types of interventions
LABA (salmeterol or formoterol) versus placebo administered daily for at least four weeks. LABA added to ICS was compared:
with the same ICS dose; or
with an increased dose of ICS.
Studies in which maintenance ICS therapy was interrupted for the purposes of run‐in were not eligible for the review. Other co‐interventions such as xanthines, anticholinergics and other anti‐asthmatic medications were permitted, provided that the dose remained unchanged throughout the study. Inhaled short‐acting beta2‐agonists (SABA) and short courses of systemic steroids were allowed as rescue medications.
Types of outcome measures
Primary outcomes
Number of asthma exacerbations of moderate intensity, that is, requiring a short course of systemic corticosteroids.
Secondary outcomes
Admissions to hospital.
Urgent care visits.
Pulmonary function tests (morning and evening peak expiratory flow (PEF) or forced expiratory flow rate in one second (FEV1)).
Symptoms.
Quality of life scores.
Use of rescue SABA.
Nighttime awakening.
Changes in measures of inflammation such as serum eosinophil cationic protein and sputum eosinophils.
Rates of clinical and biochemical adverse effects.
Any adverse effects including growth suppression, adrenal suppression, bone mineral loss and others. A suite of related Cochrane reviews considered serious adverse effects related to LABA (Cates 2008a; Cates 2009a; Cates 2009b).
Search methods for identification of studies
Electronic searches
We carried out an electronic literature search of the Cochrane Airways Group Specialised Register of asthma trials, which is derived from systematic searches of bibliographic databases including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and we handsearched respiratory journals and meeting abstracts (see Appendix 1 for additional details). This Register also includes a variety of studies published in foreign languages. We did not exclude trials on the basis of language. In Appendix 2, we have detailed search methods used in the previous version of this review. For this update, we searched the Register from May 2008 to January 2015, using the strategy presented in Appendix 3.
Searching other resources
We checked reference lists of all included studies and reviews to identify potentially relevant citations.
We searched manufacturers' and clinical trial websites (Glaxo Smith Kline clinical trials website ; AstraZeneca clinical trials website; Novartis clinical trial results website; Clinical Study Results) to identify other published or unpublished study data.
Data collection and analysis
Selection of studies
From the title, abstract or descriptors, two of three review authors (BC, MNC, SM) independently reviewed the literature searches. We excluded all studies that were not randomised controlled trials or that clearly did not fit the inclusion criteria. Two review authors independently reviewed all other citations in full text to assess eligibility.
Data extraction and management
Two of four review authors (BC, MNC, CC, SM) independently extracted data from included trials onto Excel spreadsheets and entered data into the Cochrane software program, Review Manager 5.3 (Review Manager (RevMan)). When necessary, we expanded graphic reproductions and estimations from other data presented in the paper. We contacted primary authors or sponsors to request confirmation of methods and data extraction and to ask for additional information, when needed.
We recorded the following as a 'User defined order'.
Mean daily dose of ICS in trials in which both intervention and control groups used the same dose of ICS.
Dose difference between groups in studies that compared LABA added to ICS with an increased dose of ICS. Researchers reported both values in chlorofluorocarbon (CFC)‐propelled beclomethasone‐equivalents, where 1 µg of beclomethasone dipropionate equates to 1 µg of budesonide and 0.5 µg of fluticasone propionate (NAEPP 2011), and all doses of inhaled medications as ex‐valve, rather than ex‐inhaler, values.
Assessment of risk of bias in included studies
We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
For each domain, we judged risk of bias as low, unclear or high, in line with recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We judged the study to have high methodological quality when reported randomisation procedures and blinding were adequate and low and balanced group attrition was noted, supporting low risk of bias.
Measures of treatment effect
We calculated treatment effects for dichotomous variables as pooled risk ratios (RRs) with 95% confidence intervals (CI). For continuous outcomes, such as pulmonary function tests, we calculated pooled statistics as mean differences (MD) or standardised mean differences (SMD) if results were reported on different scales and were reported with 95% CIs. When standard deviations were not presented but could be estimated from an effect estimate and use of confidence intervals, standard error or P value, we combined the MD with the generic inverse variance function (GIV) in Review Manager.
Unit of analysis issues
We excluded cross‐over studies from contributing data to dichotomous measurements of exacerbations, as we used analyses that assumed measurements were taken from independent samples.
Dealing with missing data
We directly contacted study investigators (or study sponsors when trials had pharmaceutical company sponsorship) to request confirmation of methods and to ask for data missing from the original trial report, if needed.
Assessment of heterogeneity
We examined homogeneity of effect sizes between pooled studies by using the I2 statistic, with 50% or more as the cutoff for exploring possible causes of heterogeneity (Higgins 2003; Higgins 2011). In the absence of heterogeneity, we used the fixed‐effect model; otherwise, we applied the Dersimonian and Laird random‐effects model (DerSimonian 1986) to the summary estimates. We reported results of the fixed‐effect model unless otherwise stated in the text.
Assessment of reporting biases
We planned to use funnel plots to check for indications of possible publication bias and small‐study effects, if we had been able to pool data from 10 or more studies.
Data synthesis
We performed meta‐analyses using the Cochrane statistical package RevMan 5 (Review Manager (RevMan)) and assumed equivalence if the risk ratio estimate and its confidence interval were between 0.9 and 1.1.
We performed the analysis to examine two main comparisons, namely, the combination of LABA and ICS versus:
a similar dose of ICS with placebo, representing step 2 of the BTS guidelines; or
an increased dose of ICS with placebo, representing step 3 of the BTS guidelines.
When a trial included more than two arms, we considered additional control‐intervention group comparisons for this review. If the same group was used twice as a comparator in a three‐arm study, we halved the number of participants in the group used twice to avoid over‐representation. For event rates, we halved the denominator in the control group (Verberne 1998a; Verberne 1998b; Zimmerman 2004a; Zimmerman 2004b; Pohunek 2006a; Pohunek 2006b; Morice 2008a; Morice 2008b; Eid 2010a; Eid 2010b; SAM40012a; SAM40012b).
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses to explore possible reasons for heterogeneity and, in the absence of heterogeneity, to identify potential effect modifiers when the magnitude of benefit may vary according to baseline characteristics. We examined the following a priori defined subgroups.
Magnitude of airway obstruction at baseline as determined by the mean percent predicted FEV1: classified as mild (80% of predicted or more), moderate (61% to 79% of predicted) or severe (60% of predicted or less) (GINA 2015).
Mean dose (ex‐valve) of ICS in comparison 1 when LABA + ICS was compared with placebo + ICS, and the dose difference in comparison 2 when LABA + ICS was compared with increased doses of ICS, both reported in CFC‐propelled beclomethasone‐equivalent doses (µg/d) and portrayed as the user‐defined number.
Usual versus higher than usual dose (reported as ex‐valve in µg) of the LABA (salmeterol or formoterol).
Type of LABA given (salmeterol vs formoterol).
Use of one or two devices to deliver the combination of ICS and LABA.
Trial duration with trials ≤ 16 weeks compared with those ≥ 24 weeks.
Sensitivity analysis
We performed sensitivity analyses to assess whether results for our primary outcome were sensitive to blinding, publication status and funding.
Results
Description of studies
Results of the search
See Figure 1 for an overview of the literature search results, their assessment and inclusion of studies in the review. Updated electronic and additional handsearches from May 2008 to January 2015 yielded 283 additional citations. We included eight new trials, resulting in a total of 33 eligible trials representing 39 control‐intervention comparisons.
1.
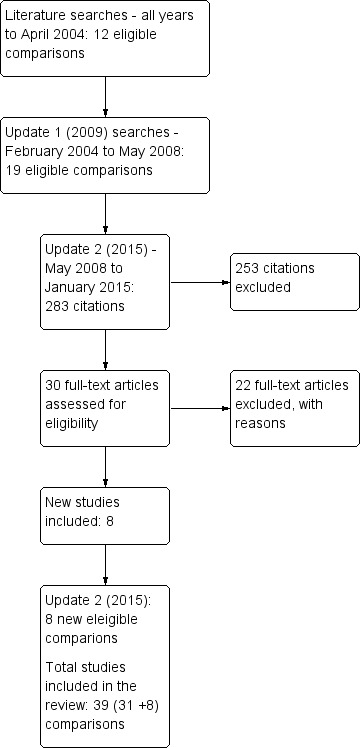
Study flow diagram.
Please note that some of the study names have changed since the last published version to reflect the Cochrane study naming convention: SAM104926, SFA 100314, SD 039 0719, SD 039 0725a, SD 039 0725b, and SFA100316 and were replaced with De Blic 2009; Pearlman 2009; Berger 2010; Eid 2010a; Eid 2010band Murray 2011, respectively.
Six trials generated an additional control‐intervention comparison. Three trials (representing six control‐intervention comparisons) assessed two forms of additive therapy (ICS and LABA via one inhaler or via two inhaler devices against one dose of ICS): Pohunek 2006a; Pohunek 2006b; Morice 2008a; Morice 2008b; Eid 2010a; Eid 2010b. Three trials (representing six control‐intervention comparisons) assessed one form of ICS and LABA versus two doses of ICS (Verberne 1998a; Verberne 1998b; Zimmerman 2004a; Zimmerman 2004b; SAM40012a; SAM40012b). The review therefore lists 39 control‐intervention comparisons.
Included studies
A total of 33 trials randomly assigned 6381 children. Twenty‐seven trials were available as full‐text publications, and six trials were published as abstracts or were presented in unpublished reports of trials accessed through pharmaceutical company trial registries.
Most (69.7%) studies were funded by producers of both LABA and ICS inhalers: 13 were supported by GSK; nine by AstraZeneca; and one by Allen & Hanburys, a subsidiary of GSK in the United Kingdom (Russell 1995). Two were supported by grant agencies (Lemanske 2010; Lenney 2013), two were independently supported by a charitable organization (Langton Hewer 1995; Stelmach 2007) and five failed to identify the source of funding (Ortega‐Cisneros 1998; Heuck 2000; Zimmerman 2004a; Zimmerman 2004b; Teper 2005; Stelmach 2008).
We classified studies into one of two comparisons according to the research question addressed. In accordance with therapeutic management as recommended by GINA 2015 and BTS 2014, we considered participants given low‐dose ICS alone as receiving step 2 therapy. We referred to the comparison of LABA versus placebo added to the same ICS dose as step 3 versus step 2 comparison (28 control‐intervention comparisons). Hereafter, we refer to comparisons testing the combination of LABA and ICS versus a double dose of ICS used before randomisation as a step 3 versus step 3 comparison (11 control‐intervention comparisons). Bisgaard 2006 examined LABA added to a lower dose of ICS (BDP 100 µg) than has been advocated by international guidelines as step 3 and included this in the step 3/step 3 comparison.
We describe hereafter characteristics of studies that contributed outcome data to one or more comparisons in the review. For a full description of each eligible study, see Characteristics of included studies.
LABA + ICS versus same dose of ICS as used before randomisation (step 3 vs step 2)
Twenty‐eight control‐intervention comparisons randomly assigned 4753 children to assessLABA versus placebo added to the same dose of ICS in both groups (Langton Hewer 1995; Meijer 1995; Russell 1995; Simons 1997; Verberne 1998a; Akpinarli 1999; Tal 2002; Zimmerman 2004a; Zimmerman 2004b; Malone 2005; Teper 2005; Pohunek 2006a; Pohunek 2006b; Stelmach 2007; Morice 2008a; Morice 2008b; Stelmach 2008; Pearlman 2009; Rutkowski 2009; Berger 2010; Carroll 2010; Eid 2010a; Eid 2010b; Murray 2011; SAM40012a; Lenney 2013; SD 039 0714; SD 039 0718).
Participants
The mean age of participants was 11 years, and males accounted for 59% of study populations. Mean FEV1 % predicted at baseline was ≥ 80% in 19 control‐intervention comparisons: Morice 2008a; Morice 2008b; Langton Hewer 1995; Meijer 1995; Simons 1997; Verberne 1998a; Verberne 1998b; Malone 2005; Teper 2005; Pohunek 2006a; Pohunek 2006b; Stelmach 2007; Stelmach 2008; Pearlman 2009; Berger 2010; Carroll 2010; Murray 2011; Lenney 2013; SD 039 0718); 61% to 79% of predicted in six control‐intervention comparisons (Russell 1995; Akpinarli 1999; Tal 2002; Zimmerman 2004a; Zimmerman 2004b; SD 039 0714) and unreported in the remaining studies. Participants were inadequately controlled before randomisation in all but four studies in which they were described as well controlled (Meijer 1995; Simons 1997; Pohunek 2006a; Pohunek 2006b), or when control was not reported (Teper 2005; Stelmach 2008; Rutkowski 2009; Berger 2010; Eid 2010a; Eid 2010b).
Interventions
Salmeterol was assessed in 12, and formoterol in 16, control‐intervention comparisons. All but one comparison tested the usual recommended dose of the LABA (i.e. salmeterol 50 µg twice daily, formoterol 4.5, 6 or 12 µg twice daily); Langton Hewer 1995 used salmeterol 100 µg twice daily. The dose of ICS (beclomethasone‐equivalent) was 200 μg/d in five studies (Stelmach 2007; Stelmach 2008; Eid 2010a; Eid 2010b; SD 039 0718); 400 µg/d in 13 control‐intervention comparisons (Verberne 1998a; Tal 2002; Malone 2005; Pohunek 2006a; Pohunek 2006b; Morice 2008a; Morice 2008b; Pearlman 2009; Carroll 2010; Murray 2011; SAM40012a; Lenney 2013; SD 039 0714), 500 µg/d in two studies (Meijer 1995; Teper 2005), 800 µg/d in two studies (Rutkowski 2009; Berger 2010) and unspecified or varied in six studies (Langton Hewer 1995; Russell 1995; Simons 1997; Akpinarli 1999; Zimmerman 2004a; Zimmerman 2004b). Eighteen (46%) control‐intervention comparisons assessed the combination of LABA and ICS in a single device; the remainder assessed the efficacy and safety of a LABA administered separately from an ICS.
Trial duration ranged from eight weeks or less in nine studies (Langton Hewer 1995; Simons 1997; Akpinarli 1999; Stelmach 2007; Stelmach 2008; Rutkowski 2009; Pearlman 2009; Carroll 2010; Murray 2011), to 12 to 16 weeks in 14 control‐intervention comparisons (Meijer 1995; Russell 1995; Tal 2002; Zimmerman 2004a; Zimmerman 2004b; Malone 2005; Pohunek 2006a; Pohunek 2006b; Morice 2008a; Morice 2008b; Eid 2010a; Eid 2010b; SD 039 0718; SD 039 0714), to 24 to 26 weeks in two studies (Berger 2010; SAM40012a) to 48 to 52 weeks in three studies (Verberne 1998a; Teper 2005; Lenney 2013).
Although co‐intervention with other prophylactic medications was permitted, trial protocols stipulated that their doses should remain unchanged throughout. The proportion of participants given additional therapy was not consistently reported. Permitted drugs included systemic steroids, anticholinergics and xanthines (Langton Hewer 1995), immunotherapy (Zimmerman 2004a; Zimmerman 2004b) and unspecified agents (Russell 1995). Other preventative medications were not permitted in the other studies except for Teper 2005, in which this was unspecified. Rescue medications such as inhaled SABA and systemic steroids were permitted in all studies.
Outcomes
The primary outcome ‐ the number of children with at least one exacerbation requiring systemic steroids ‐ was reported by 12 studies. When data were not reported, or were described only in a format we could not use directly, we asked study sponsors to provide further information, if possible. Our requests for data on exacerbations requiring rescue oral steroids for Pohunek 2006a; Pohunek 2006b; Stelmach 2007; Morice 2008a; Morice 2008b; SD 039 0718 and SD 039 0714 yielded no response.
Hospital admission data were available for seven studies. Measurement of lung function was reported in most studies. Many studies reported other secondary outcomes. Withdrawals were reported in all but five studies (Meijer 1995; Akpinarli 1999; Teper 2005; Stelmach 2008; Rutkowski 2009). Adverse events were reported in all studies except Stelmach 2008; Rutkowski 2009; Berger 2010; Carroll 2010; Lemanske 2010 and Lenney 2013.
LABA + ICS versus increased dose of ICS (step 3/step3)
A total of 11 studies, representing 1628 children, assessed the addition of LABA versus placebo to ICS therapy with increased dose of ICS in the control group (Ortega‐Cisneros 1998; Verberne 1998b; Heuck 2000; Bisgaard 2006; De Blic 2009; Gappa 2009; Lemanske 2010; Murray 2010; Vaessen‐Verberne 2010; SAM40100; SAM40012b). Three studies did not contribute data (Ortega‐Cisneros 1998; Heuck 2000; Lemanske 2010).
Participants
The mean age of participants was 10 years and 64% were male. Baseline airway obstruction was reported in seven of the 11 studies (Verberne 1998b; Heuck 2000; Bisgaard 2006: Gappa 2009; Lemanske 2010; Murray 2010; Vaessen‐Verberne 2010). Mean FEV1 % predicted at baseline was ≥ 80% in five control‐intervention comparisons (Verberne 1998b; Gappa 2009; Lemanske 2010; Murray 2010; Vaessen‐Verberne 2010).
Interventions
Salmeterol and formoterol were evaluated in eight and three studies, respectively. All comparisons tested the usual recommended dose of the LABA (i.e. salmeterol 50 µg twice daily, formoterol 6 or 12 µg twice daily). Intervention groups in eight studies received BDP equivalent doses of 400 µg/d (Verberne 1998b; De Blic 2009; Gappa 2009; Lemanske 2010; Murray 2010; Vaessen‐Verberne 2010; SAM40100; SAM40012b). BDP at 100 µg/d was used in Bisgaard 2006, and 200 µg/d was used in Heuck 2000. Respective control groups received twice the dose of ICS administered to the intervention group. Four studies assessed LABA and ICS as a single inhaler administration (Bisgaard 2006; De Blic 2009; SAM40100; SAM40012b).
Study duration was six to eight weeks in three studies (Gappa 2009; Murray 2010; SAM40100), 12 to 16 weeks in four studies (Heuck 2000; Bisgaard 2006; De Blic 2009; Lemanske 2010), 26 weeks in two comparisons (Vaessen‐Verberne 2010; SAM40012b), and one year in one study (Verberne 1998b).
All studies recruited children who were taking an ICS at baseline. Rescue medications such as inhaled SABA and systemic steroids were permitted in all trials.
Outcome data (obtaining data from trial authors)
Data on the primary outcome were available from three studies (Verberne 1998b; De Blic 2009; Vaessen‐Verberne 2010). When data were not reported, or were described for an undefined exacerbation or composite of types of exacerbations, we requested study sponsors to provide further information. Our requests for data on exacerbations requiring rescue oral corticosteroids (OCS) from study sponsors for Bisgaard 2006, SAM40012b and SAM40100 have not been successful.
Hospital admission data were available for four studies. Lung function outcomes were available for all studies. Most studies provided data on symptoms, SABA use, adverse events and withdrawals. Two studies provided data on linear growth (Verberne 1998b; Bisgaard 2006).
Excluded studies
Details of 85 excluded studies, for which full‐text articles were examined to judge eligibility, are listed in Characteristics of excluded studies along with reasons for their exclusion (this number is drawn from searches over all years January 2015 across this review).
Risk of bias in included studies
We have provided an overview of judgements on domains related to risk of bias in Figure 2. We have summarised our findings below.
2.
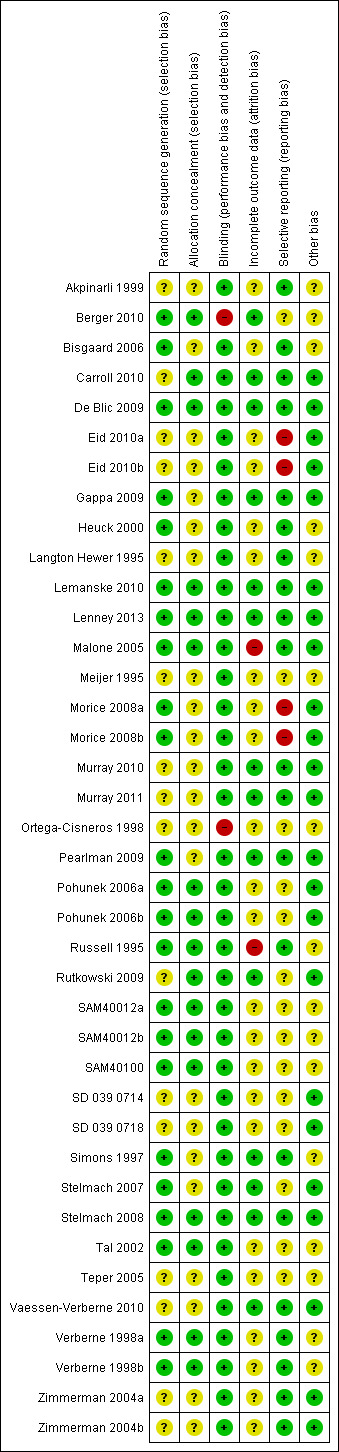
Methodological quality summary: review authors' judgments about each methodological quality item for each included study.
We verified with study authors study details for six control‐intervention comparisons (Russell 1995; Simons 1997; Verberne 1998a; Verberne 1998b; Pohunek 2006a; Pohunek 2006b). Information on the design of GSK‐sponsored studies was provided in correspondence (Appendix 4). A total of 23 comparisons reported the randomisation technique in adequate detail, and we assessed remaining studies as unclear on the basis of inadequate reporting of the randomisation technique.
Allocation
Seventeen studies reported adequate details on allocation concealment of intervention treatment, and 22 provided unclear information.
Blinding
Double‐dummy designs or use of identical inhaler devices in 37 comparisons maintained blinding of the intervention. Two studies had an open‐label design (Ortega‐Cisneros 1998; Berger 2010).
Incomplete outcome data
Information on the definition of intention‐to‐treat principle used across studies was insufficient. Our judgement of this aspect of the studies reflects uncertainty over the reliability of stated methods. However, on the basis of our judgements, we designated 14 comparisons as high‐quality trials reporting complete outcomes, 23 as unclear and two as having high risk of bias (Russell 1995; Eid 2010a; Eid 2010b).
Selective reporting
We did not find major selective reporting bias in included studies. Availability of our prespecified primary outcome ‐ participants with exacerbations requiring rescue systemic steroids ‐ from trial reports was limited. This can be explained in part by the different definitions of exacerbation used by investigators across studies. Despite extensive efforts to obtain data for our primary outcome, we obtained a limited quantity of available data for analysis. We remain uncertain as to whether data for this endpoint were collected in nine studies (Langton Hewer 1995; Meijer 1995; Ortega‐Cisneros 1998; Tal 2002; Pohunek 2006a; Pohunek 2006b; Teper 2005; Stelmach 2007; SAM40100); 21 were at low risk, 14 at unclear risk and four at high risk.
Other potential sources of bias
In all, 23 studies were at low risk and 16 were at unclear risk.
Effects of interventions
for the main comparison.
| LABA + ICS compared with same dose of ICS for children with chronic asthma | ||||||
|
Patient or population: children with chronic asthma Settings: outpatients Intervention: LABA + ICS Comparison: same dose of ICS | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Increased dose of ICS | LABA + ICS | |||||
| Number of participants with exacerbations requiring systemic steroids | 86 per 1000 | 94 per 1000 | RR 0.95 (0.70 to 1.28) | 1669 (12 studies) | ⊕⊕⊕⊝ Moderatea | |
| Number of participants with exacerbations requiring hospitalisation | 19 per 1000 | 33 per 1000 | RR 1.74 (0.90 to 3.36) | 1292 (6 studies) | ⊕⊕⊕⊝ Moderatea | |
| Serious adverse events | 16 per 1000 | 18 per 1000 | RR 1.17 (0.75 to 1.85) | 4022 (16 studies) | ⊕⊕⊕⊝ Moderatea | |
| Total number of withdrawals | 127 per 1000 | 94 per 1000 | RR 0.80 (0.67 to 0.94) | 4374 (23 studies) | ⊕⊕⊝⊝ Lowa,b | |
| Change in FEV1 (L) at endpoint | Baseline mean FEV1 ranged from 1.65 L to 1.9 L (baseline data reported in 4 studies only) | Mean FEV1 change from baseline with LABA + ICS was 0.08 L higher (0.06 to 0.1 higher) | 1942 (9 studies) | ⊕⊕⊝⊝ Lowa,b | ||
| Change in morning PEF (L/min) at endpoint | Illustrative post‐treatment PEFs range from 235 to 290 L/min (data from 3 recent studies) | Mean PEF change from baseline with LABA + ICS was 10.20 L/min higher (8.14 to 12.26 higher) | 3934 (16 studies) | ⊕⊕⊕⊝ Moderatea | ||
| Total number of adverse events | 547 per 1000 | 568 per 1000 | RR 1.04 (0.98 to 1.10) | 3284 (15 studies) | ⊕⊕⊕⊝ Moderateb | |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; FEV1: Forced expiratory volume in 1 second;ICS: Inhaled corticosteroids; LABA: Long‐acting beta2‐agonists; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aLarger sample size may change the outcome.
bOpen‐label study contributed data.
2.
| LABA + ICS compared with increased dose of ICS for children with chronic asthma | ||||||
|
Patient or population: children with chronic asthma Settings: outpatients Intervention: LABA + ICS Comparison: increased dose of ICS | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Increased dose of ICS | LABA + ICS | |||||
| Number of participants with exacerbations requiring systemic steroids | 41 per 1000 | 69 per 1000 | RR 1.69 (0.85 to 3.32) | 581 (3 studies) | ⊕⊕⊕⊝ Moderatea | |
| Number of participants with exacerbations requiring hospitalisation | 8 per 1000 | 18 per 1000 | RR 1.90 (0.65 to 5.54) | 1008 (4 studies) | ⊕⊕⊕⊝ Moderatea | |
| Serious adverse events | 24 per 1000 | 39 per 1000 | RR 1.54 (0.81 to 2.94) | 1343 (7 studies) | ⊕⊕⊕⊝ Moderatea | |
| Total number of withdrawals | 70 per 1000 | 67 per 1000 | RR 0.96 (0.67 to 1.37) | 1491 (7 studies) | ⊕⊕⊕⊝ Moderatea | |
| Change in FEV1 (L) at endpoint | Mean baseline FEV1 ranged from 1.6 to 1.7 L | Mean FEV1: change from baseline with LABA + ICS was 0.01 L higher (‐0.03 to 0.05 higher) | 526 (2 studies) | ⊕⊕⊕⊝ Moderatea | ||
| Change in morning PEF (L/min) at endpoint | Mean change in end of treatment PEF ranged from 16.7 to 39.2 L/min | Mean PEF: change from baseline with LABA + ICS was 8.73 L/min higher (5.15 to 12.31 higher) | 1283 (5 studies) | ⊕⊕⊕⊝ Moderatea | ||
| Total number of adverse events | 569 per 1000 | 576 per 1000 | RR 1.01 (0.92 to 1.10) | 1254 (6 studies) | ⊕⊕⊕⊕ High | |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; FEV1: Forced expiratory volume in 1 second; ICS: Inhaled corticosteroids; LABA: Long‐acting beta2‐agonists; PEF: Peak expiratory flow; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aLarger sample size may change the outcome.
LABA + ICS versus same dose of ICS (step 3 vs step 2)
Primary outcome: participants with at least one exacerbation requiring systemic steroids
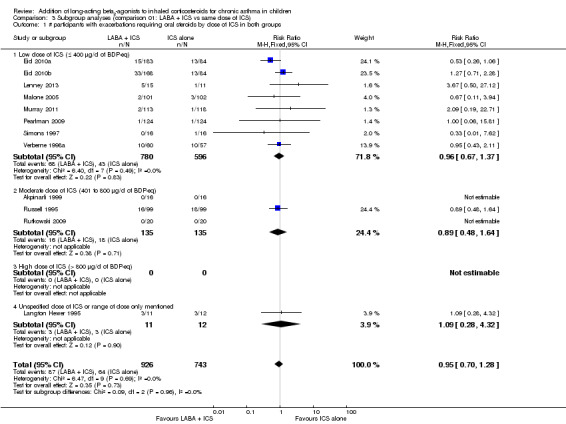
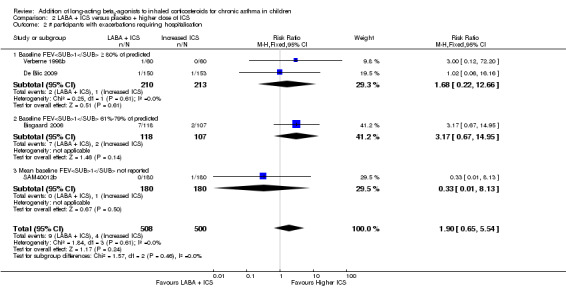
Investigators reported no statistically significant differences between treatments in the number of participants with exacerbations requiring systemic corticosteroids (12 studies; RR 0.95, 95% CI 0.70 to 1.28, N = 1669; Analysis 1.1; Figure 3).
1.1. Analysis.
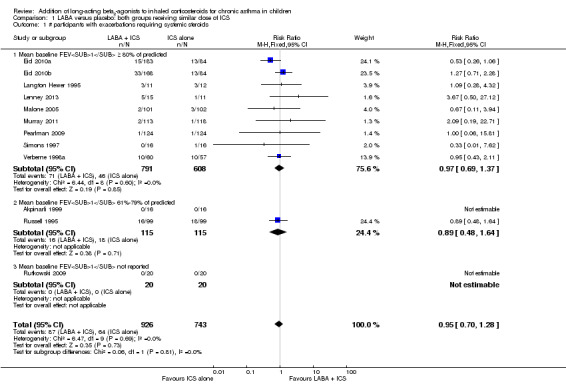
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 1 # participants with exacerbations requiring systemic steroids.
3.
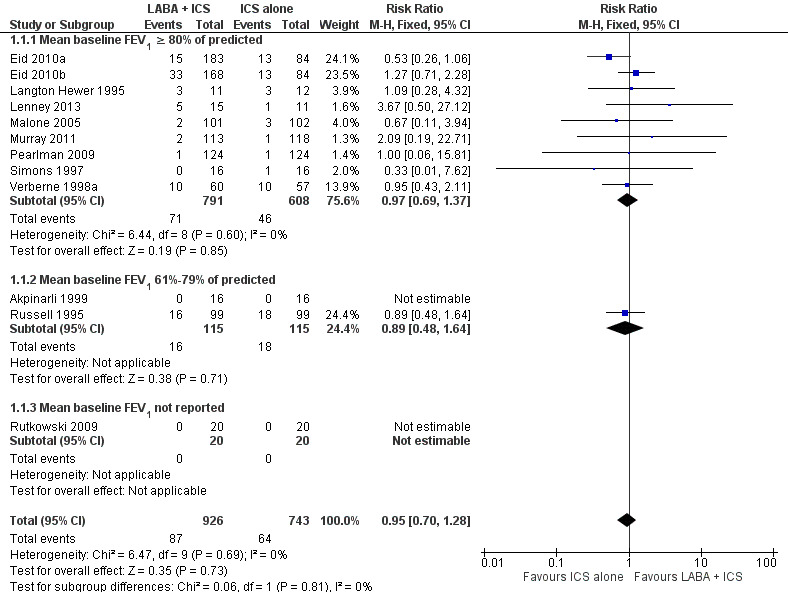
Forest plot of comparison: 1 LABA versus placebo: both groups receiving similar dose ICS, outcome: 1.1 # participants with exacerbations requiring systemic steroids.
Subgroup analysis
We performed subgroup analysis based on characteristics of participants and interventions to evaluate their influence on the magnitude of the primary outcome. Airway obstruction as determined by baseline mean FEV1 (Analysis 1.1), dose of ICS (Analysis 3.1), dose of LABA (Analysis 3.2), type of LABA (Analysis 3.3), use of single versus separate inhaler(s) to deliver LABA and ICS (Analysis 3.4) and trial duration (Analysis 3.5) did not influence the magnitude of response.
3.1. Analysis.
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 1 # participants with exacerbations requiring oral steroids by dose of ICS in both groups.
3.2. Analysis.
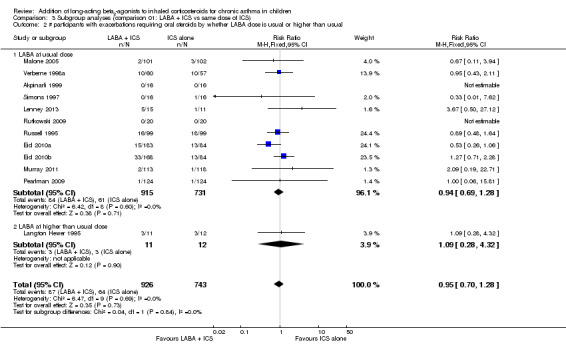
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 2 # participants with exacerbations requiring oral steroids by whether LABA dose is usual or higher than usual.
3.3. Analysis.
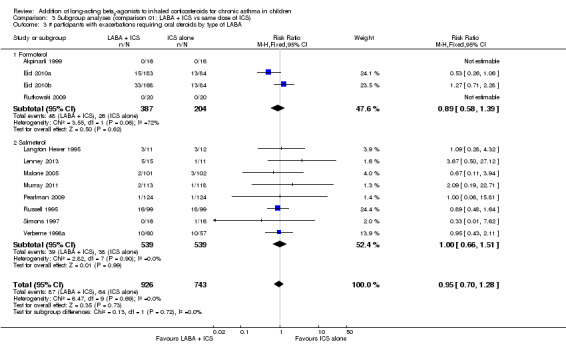
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 3 # participants with exacerbations requiring oral steroids by type of LABA.
3.4. Analysis.
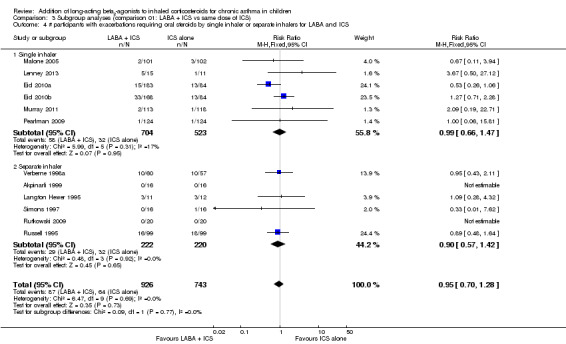
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 4 # participants with exacerbations requiring oral steroids by single inhaler or separate inhalers for LABA and ICS.
3.5. Analysis.
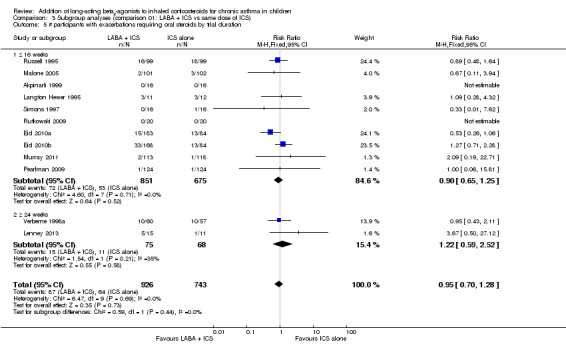
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 5 # participants with exacerbations requiring oral steroids by trial duration.
Sensitivity analysis
We performed a sensitivity analysis on the primary outcome. The primary outcome was robust and was not influenced by the funding source (Analysis 3.6) or by publication status (Analysis 3.7). All studies contributing data to the primary outcome were double‐blinded, thus preventing exclusion of unblinded trials.
3.6. Analysis.
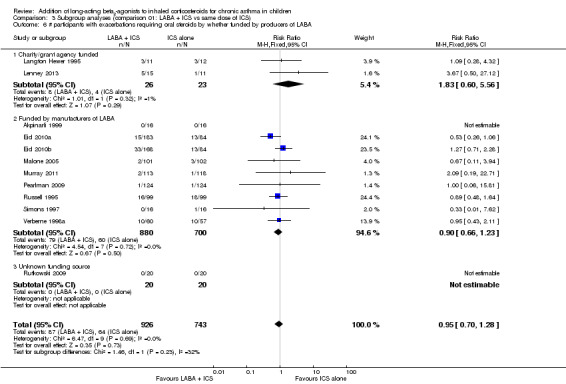
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 6 # participants with exacerbations requiring oral steroids by whether funded by producers of LABA.
3.7. Analysis.
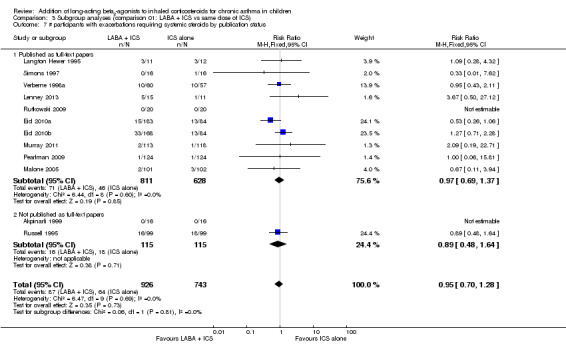
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 7 # participants with exacerbations requiring systemic steroids by publication status.
Secondary outcomes
Hospital admission, urgent care visit, withdrawal
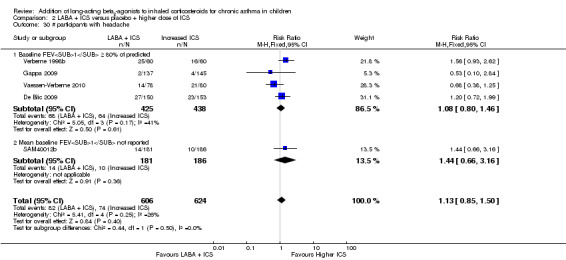
Researchers found no statistically significant differences in numbers of participants with exacerbations requiring hospital admission (seven studies, RR 1.74, 95% CI 0.90 to 3.36, N = 1292; Analysis 1.2; Figure 4), numbers of participants with exacerbations requiring urgent care visit (one study, RR 0.29, 95% CI 0.09 to 0.96, N = 186; Analysis 1.3), withdrawals due to poor asthma control (14 studies, RR 0.81, 95% CI 0.57 to 1.16, N = 2255; Analysis 1.6), withdrawals due to adverse events (18 studies, RR 0.79, 95% CI 0.52 to 1.21, N = 4117; Analysis 1.7) or withdrawals due to serious non‐respiratory events (two studies, RR 4.66, 95% CI 0.23 to 96.30; N = 318; Analysis 1.8). Withdrawals for any reason were significantly fewer with LABA than with placebo (23 studies, RR 0.80, 95% CI 0.67 to 0.94, N = 4374; Analysis 1.5).
1.2. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 2 # participants with exacerbations requiring hospitalisation.
4.
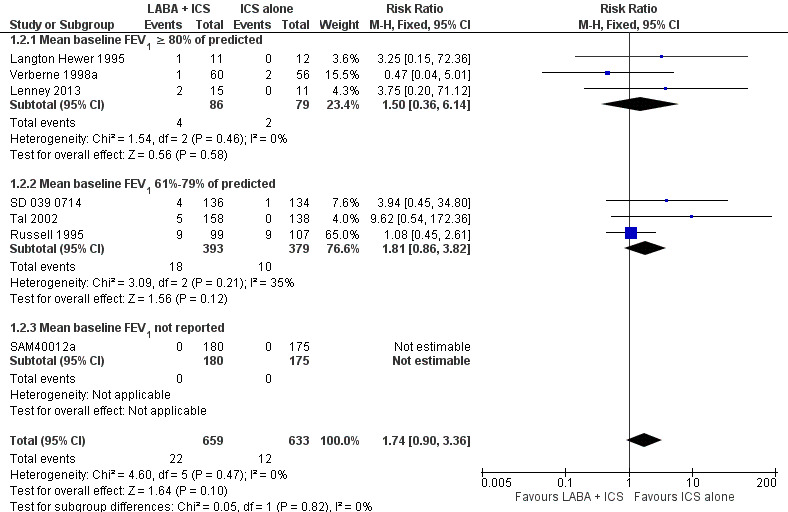
Forest plot of comparison: 1 LABA versus placebo: both groups receiving similar dose ICS, outcome: 1.2 # participants with exacerbations requiring hospitalisation.
1.3. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 3 # participants with exacerbations requiring urgent care visit.
1.6. Analysis.
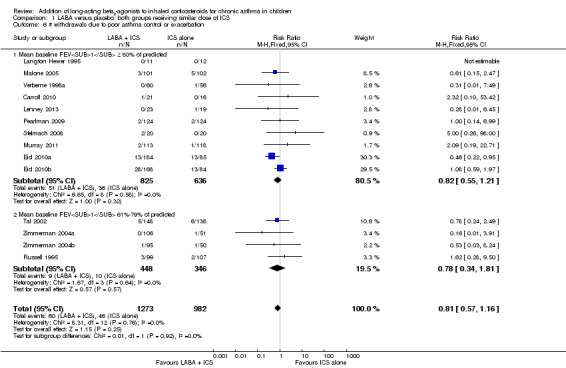
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 6 # withdrawals due to poor asthma control or exacerbation.
1.7. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 7 # withdrawals due to adverse events.
1.8. Analysis.
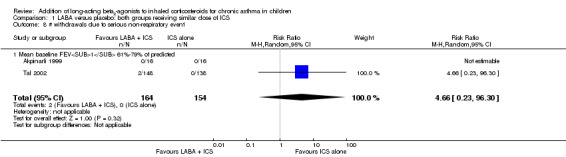
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 8 # withdrawals due to serious non‐respiratory event.
1.5. Analysis.
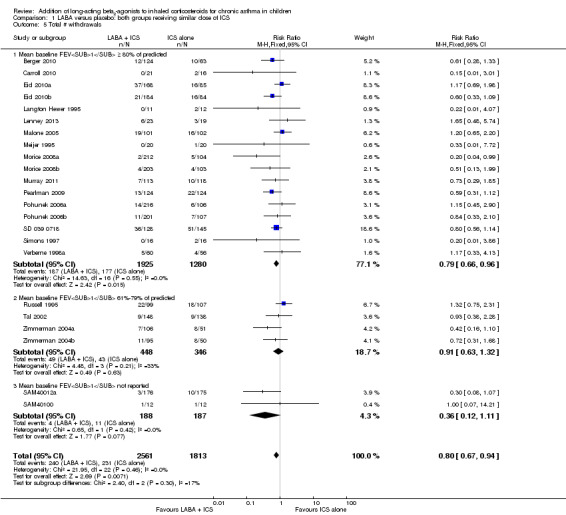
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 5 Total # withdrawals.
Lung function
LABA added to ICS provided significantly greater improvement in lung function from baseline compared with the same dose of ICS. This was true, irrespective of whether group differences were reported for FEV1 as change in litres (inverse variance (IV) 0.08 L, 95% CI 0.06 to 0.10, nine studies, N = 1942; Analysis 1.9), change in % predicted (MD 2.99%, 95% CI 0.86 to 5.11; seven studies, N = 534; Analysis 1.10) or change in morning PEF (MD 10.20 L/min, 95% CI 8.14 to 12.26, 16 studies, N = 3934; Analysis 1.12; and one study, MD 3.77%, 95% CI 1.84 to 5.70, N = 286; Analysis 1.13) or evening PEF (MD 9.30 L/min, 95% CI 6.96 to 11.65, 12 studies, N = 3140; Analysis 1.14; and MD 3.40%, 95% CI 1.54 to 5.26, one study, N = 286; Analysis 1.15). The change in clinic PEF (Analysis 1.16) and the variability in PEF (Analysis 1.17) could not be aggregated, as they were reported by a single trial. Studies contributing data to lung function endpoints recruited children with mild to moderate airway obstruction, with a range of lung function at baseline; they examined the effects of both salmeterol and formoterol, given in conjunction with a range of doses of ICS. The % fall in FEV1 % predicted due to exercise showed no significant group difference (three studies, MD 0.46%, 95% CI ‐1.00 to 1.93, N = 517; Analysis 1.11).
1.9. Analysis.
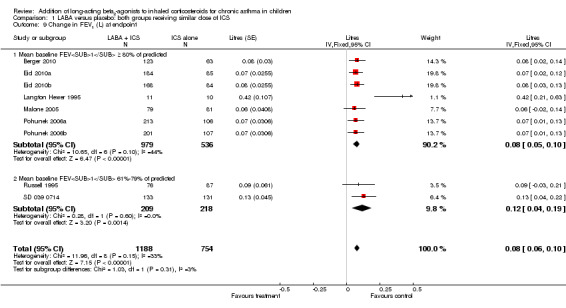
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 9 Change in FEV1 (L) at endpoint.
1.10. Analysis.
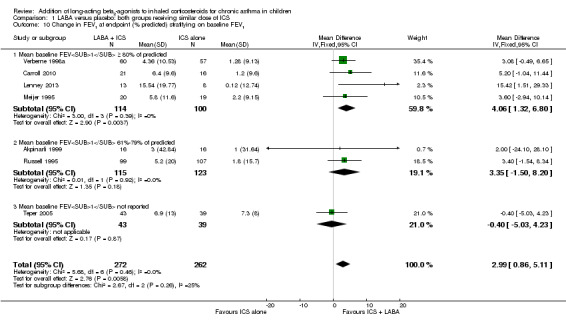
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 10 Change in FEV1 at endpoint (% predicted) stratifying on baseline FEV1.
1.12. Analysis.
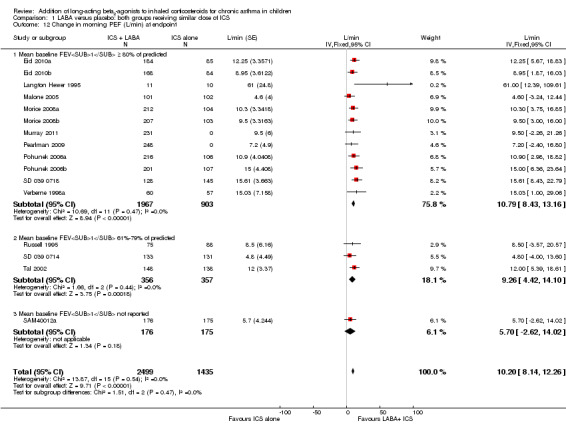
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 12 Change in morning PEF (L/min) at endpoint.
1.13. Analysis.
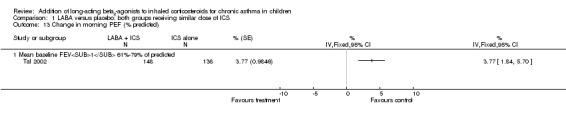
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 13 Change in morning PEF (% predicted).
1.14. Analysis.
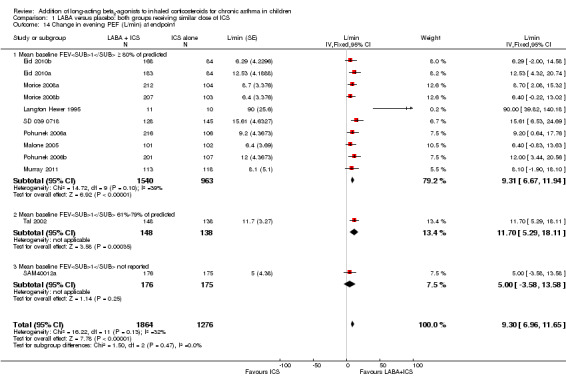
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 14 Change in evening PEF (L/min) at endpoint.
1.15. Analysis.
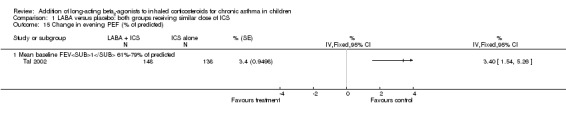
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 15 Change in evening PEF (% of predicted).
1.16. Analysis.
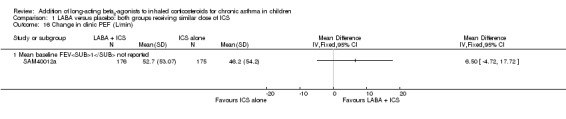
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 16 Change in clinic PEF (L/min).
1.17. Analysis.
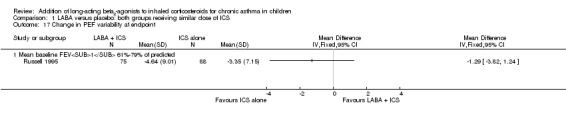
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 17 Change in PEF variability at endpoint.
1.11. Analysis.
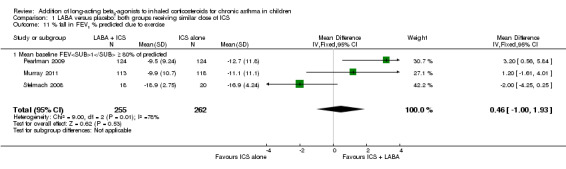
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 11 % fall in FEV1 % predicted due to exercise.
Symptoms, rescue SABA use and quality of life
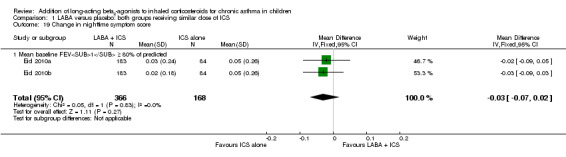
LABA added to ICS resulted in significant group differences for the following outcomes: change in daytime use of rescue SABA (MD ‐0.07 puffs/d, 95% CI ‐0.11 to ‐0.02, seven studies, N = 1798; Analysis 1.23) and change in nighttime use of rescue SABA (MD ‐0.08 puffs/d, 95% CI ‐0.13 to ‐0.03, three studies, N = 672; Analysis 1.24).
1.23. Analysis.
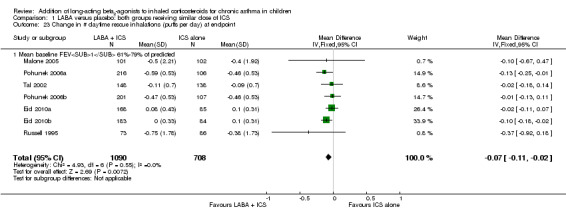
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 23 Change in # daytime rescue inhalations (puffs per day) at endpoint.
1.24. Analysis.
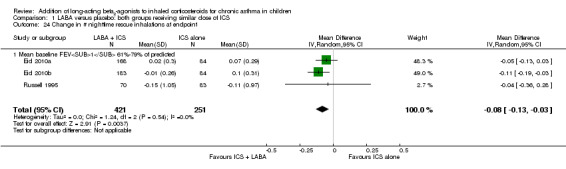
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 24 Change in # nighttime rescue inhalations at endpoint.
The addition of LABA did not result in significant group differences for the following outcomes: change in mean symptom scores (SMD ‐0.07, 95% CI ‐0.17 to 0.04, six studies, N = 1653; Analysis 1.18), change in nighttime symptom scores (two studies, MD ‐0.03, 95% CI ‐0.07 to 0.02, N = 534; Analysis 1.19), change in % symptom‐free days at endpoint (MD 0.96, 95% CI ‐1.91 to 3.84, seven studies, N = 1831; Analysis 1.20 ), % symptom‐free days (MD ‐0.04, 95% CI ‐0.20 to 0.12, four studies, N = 623; Analysis 1.21), % symptom‐free nights (MD 0.00, 95% CI ‐2.38 to 2.38, one study, N = 82; Analysis 1.22 ), % days without bronchodilator use (MD 2.07, 95% CI ‐1.03 to 5.16, seven studies, N = 1710, random‐effects model; Analysis 1.25), change in nighttime awakening (number of nights) (MD 0.20, 95% CI ‐2.21 to 2.61, one study, N = 286; Analysis 1.26), % nights with awakening (MD ‐1.10, 95% CI ‐3.51 to 1.31, one study, N = 286; Analysis 1.27), % change in awakening‐free nights (MD 0.60, 95% CI ‐1.05 to 2.26, N = 519; Analysis 1.28), change in rescue medication‐free days (two studies, MD ‐2.20, 95% CI ‐12.15 to 7.75, two studies, N = 231; Analysis 1.29), % change in asthma control days (MD 4.30, 95% CI ‐5.56 to 9.16, two studies, N = 519; Analysis 1.30), change in paediatric asthma quality of life (MD ‐0.02, 95% CI ‐0.14 to 0.10, four studies, N = 668; Analysis 1.31), absolute paediatric asthma quality of life (MD 0.03, 95% CI ‐0.04 to 0.11, 10 studies, N = 2333; Analysis 1.32) and change in paediatric asthma caregiver quality of life (MD 0.07, 95% CI ‐0.05 to 0.18; four studies, N = 669; Analysis 1.33).
1.18. Analysis.
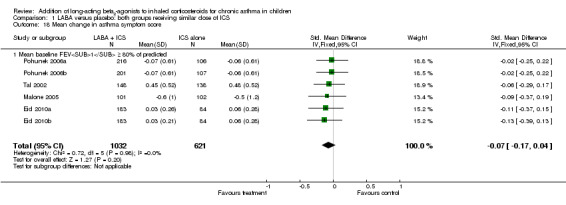
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 18 Mean change in asthma symptom score.
1.19. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 19 Change in nighttime symptom score.
1.20. Analysis.
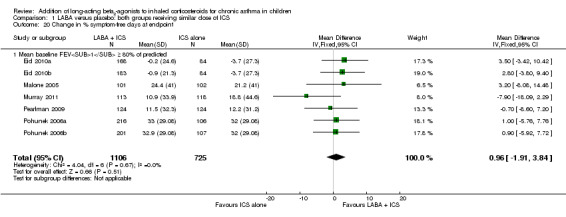
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 20 Change in % symptom‐free days at endpoint.
1.21. Analysis.
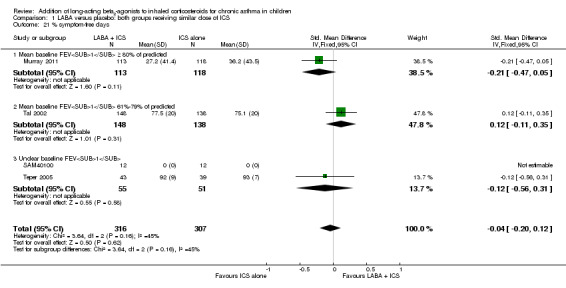
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 21 % symptom‐free days.
1.22. Analysis.
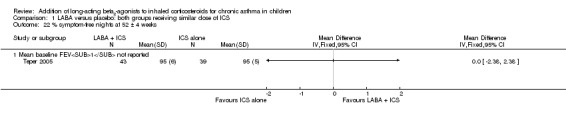
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 22 % symptom‐free nights at 52 ± 4 weeks.
1.25. Analysis.
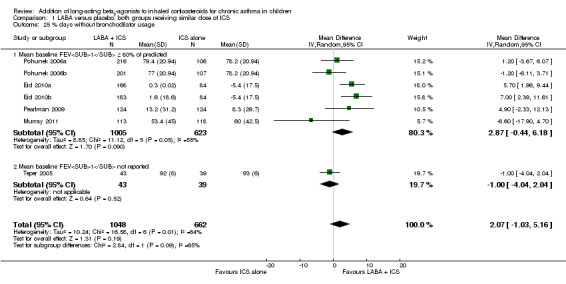
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 25 % days without bronchodilator usage.
1.26. Analysis.
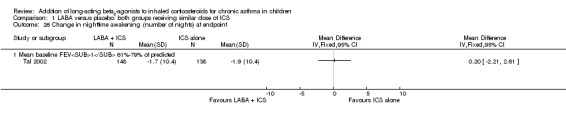
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 26 Change in nighttime awakening (number of nights) at endpoint.
1.27. Analysis.
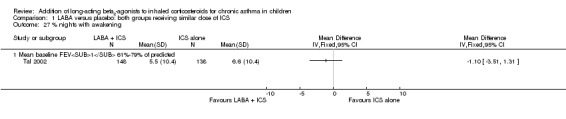
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 27 % nights with awakening.
1.28. Analysis.
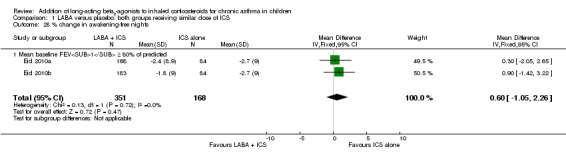
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 28 % change in awakening‐free nights.
1.29. Analysis.
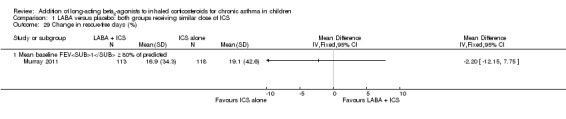
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 29 Change in rescue‐free days (%).
1.30. Analysis.
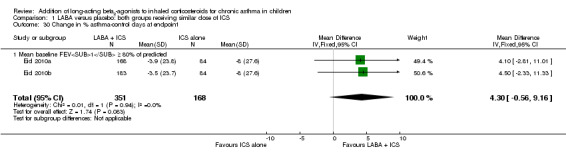
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 30 Change in % asthma‐control days at endpoint.
1.31. Analysis.
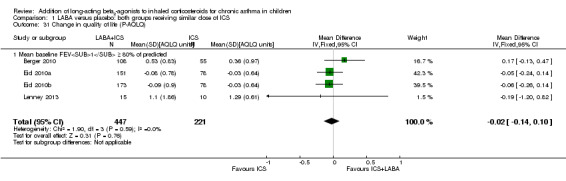
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 31 Change in quality of life (P‐AQLQ).
1.32. Analysis.
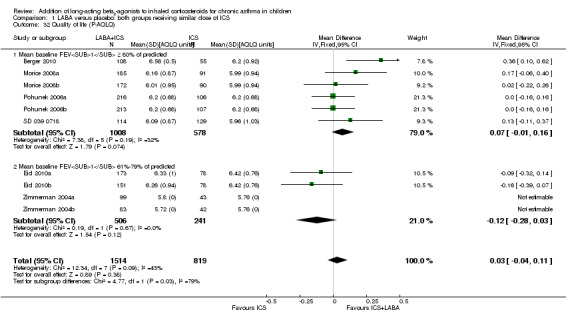
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 32 Quality of life (P‐AQLQ).
1.33. Analysis.
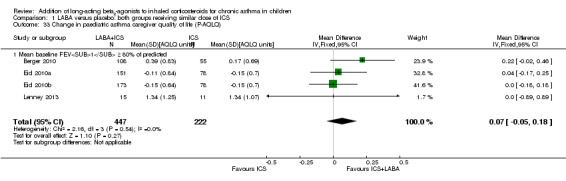
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 33 Change in paediatric asthma caregiver quality of life (P‐AQLQ).
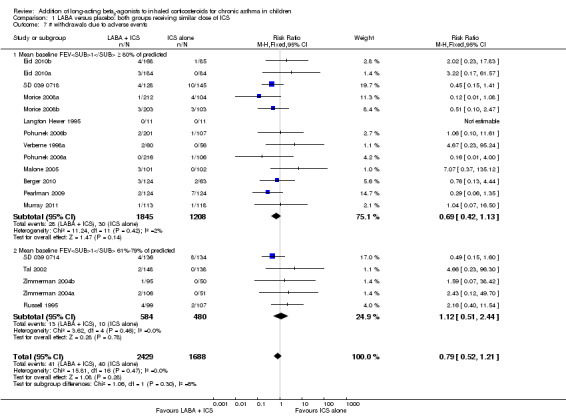
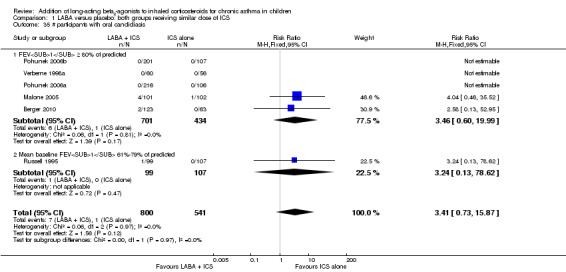
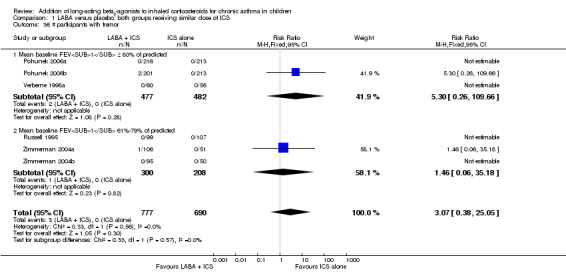
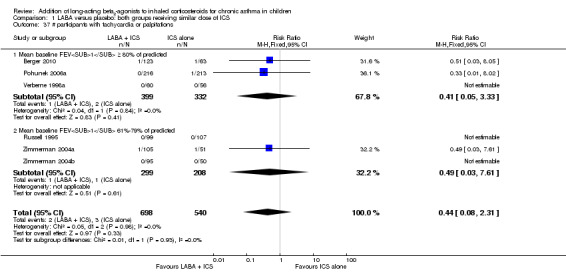
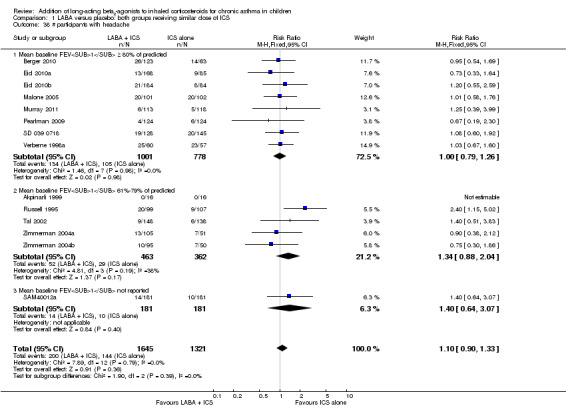
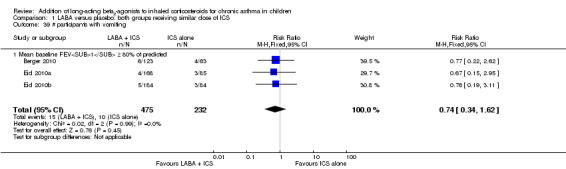
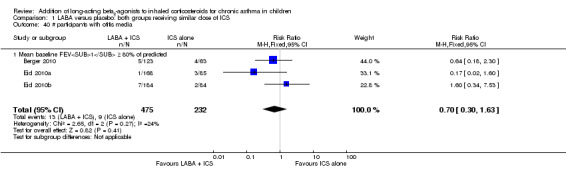
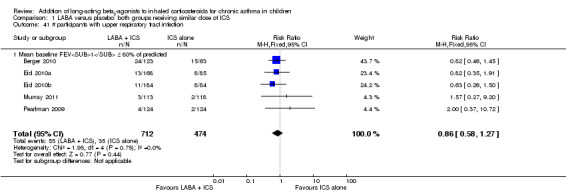
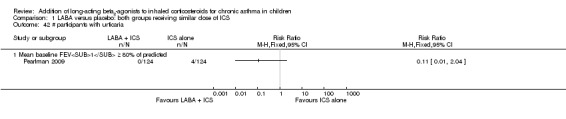
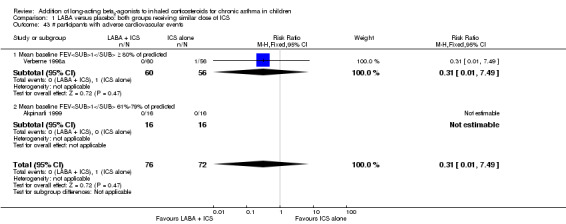
Adverse events
There was no statistically significant differences in risk of overall adverse effects (RR 1.04, 95% 0.98 to 1.10, 15 studies, N = 3284; Analysis 1.34), reaching our a priori defined criterion for equivalence. However, for specific adverse effects, confidence intervals are wide, so we cannot rule out differences in any of these specific events. Specifically, there was no significant group differences in risk of oral candidiasis (RR 3.41, 95% CI 0.73 to 15.87, six studies, N = 1341; Analysis 1.35), tremor (RR 3.07, 95% CI 0.38 to 25.05, six studies, N = 1467; Analysis 1.36), palpitations (RR 0.44, 95% CI 0.08 to 2.31, six studies, N = 1238; Analysis 1.37), headache (RR 1.10, 95% CI 0.90 to 1.33, 14 studies, N = 2966; Analysis 1.38), vomiting (RR 0.74, 95% CI 0.34 to 1.62, three studies, N = 707; Analysis 1.39), otitis media (RR 0.70, 95% CI 0.30 to 1.63, three studies, N = 707; Analysis 1.40), upper respiratory tract infection (RR 0.86, 95% CI 0.58 to 1.27, five studies, N = 1186; Analysis 1.41), urticaria (RR 0.11, 95% CI 0.01 to 2.04, one study, N = 248; Analysis 1.42), cardiovascular adverse events (RR 0.31, 95% CI 0.01 to 7.49, two studies, N = 148; Analysis 1.43) and serious adverse events (RR 1.17, 95% CI 0.75 to 1.85, 17 studies, N = 4021; Analysis 1.4), Although effects on growth could not be aggregated because only one study documented this outcome (Verberne 1998a), data show no statistically significant group differences in growth velocity over 52 weeks among prepubertal children (mean age 10 to 11 years) when beclomethasone 400 μg with salmeterol was compared with beclomethasone 400 μg alone (5.1 cm vs 4.5 cm, respectively; Analysis 1.47). In three studies that recorded mortality, no deaths were mentioned (Analysis 1.44).
1.34. Analysis.
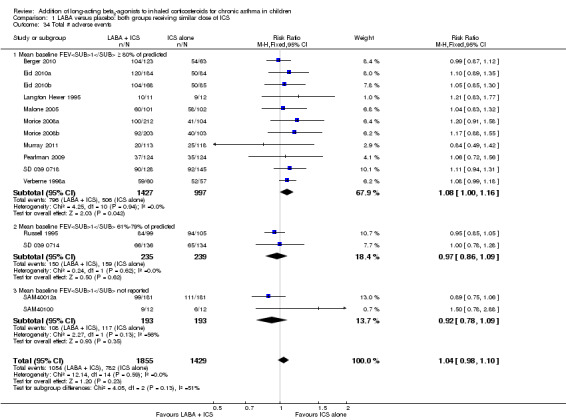
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 34 Total # adverse events.
1.35. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 35 # participants with oral candidiasis.
1.36. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 36 # participants with tremor.
1.37. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 37 # participants with tachycardia or palpitations.
1.38. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 38 # participants with headache.
1.39. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 39 # participants with vomiting.
1.40. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 40 # participants with otitis media.
1.41. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 41 # participants with upper respiratory tract infection.
1.42. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 42 # participants with urticaria.
1.43. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 43 # participants with adverse cardiovascular events.
1.4. Analysis.
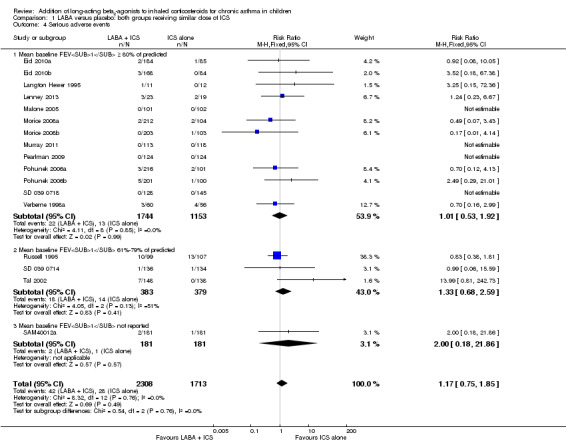
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 4 Serious adverse events.
1.47. Analysis.
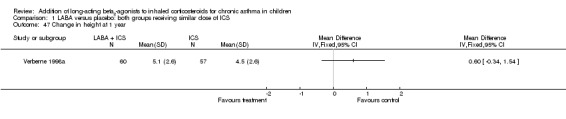
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 47 Change in height at 1 year.
1.44. Analysis.
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 44 Deaths.
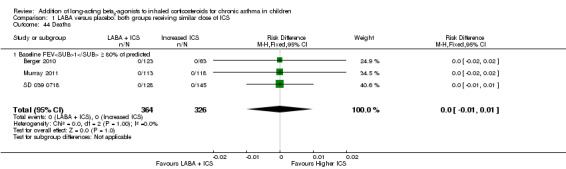
LABA and ICS versus increased dose of ICS (step 3 vs step 3)
Eight studies on 1520 participants contributed data to outcomes under this comparison (Verberne 1998b; Bisgaard 2006; De Blic 2009; Gappa 2009; Vaessen‐Verberne 2010; Murray 2010; SAM40100; SAM40012b).
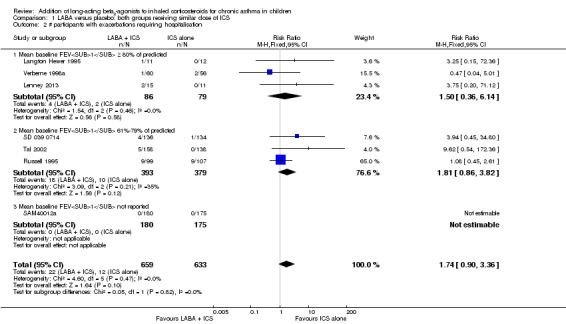
Primary outcome: participants with at least one exacerbation requiring systemic steroids
Despite correspondence with study sponsors to obtain data on exacerbations requiring rescue oral steroids, we obtained data from only three studies (Verberne 1998b; De Blic 2009; Vaessen‐Verberne 2010). There was no significant group differences in the number of participants with exacerbations requiring OCS (RR 1.69, 95% CI 0.85 to 3.32, three studies, N = 581; Analysis 2.1; Figure 5). All trials contributing data to the primary outcome recruited participants with mild airway obstruction (FEV1 % predicted ≥ 80%).
2.1. Analysis.
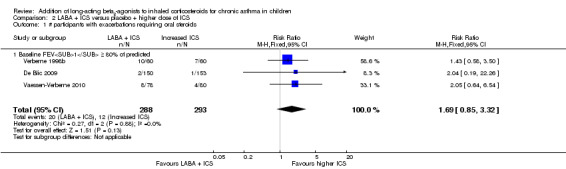
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 1 # participants with exacerbations requiring oral steroids.
5.
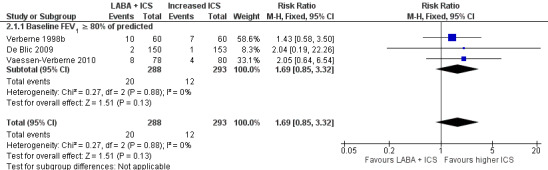
Forest plot of comparison: 2 LABA + ICS versus placebo + higher dose of ICS, outcome: 2.1 # participants with exacerbations requiring oral steroids.
Subgroup analysis
We performed subgroup analysis to evaluate the potential influence of characteristics of participants and interventions on the magnitude of the primary outcome. Dose of ICS (Analysis 4.1), dose of LABA (Analysis 4.2), type of LABA (Analysis 4.3), use of single versus separate inhaler(s) to deliver LABA and ICS (Analysis 4.4) and trial duration (Analysis 4.5) did not influence the magnitude of response.
4.1. Analysis.
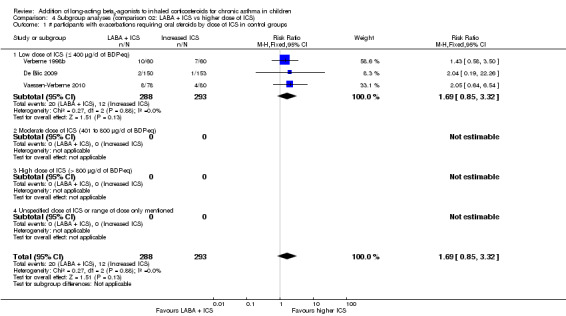
Comparison 4 Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS), Outcome 1 # participants with exacerbations requiring oral steroids by dose of ICS in control groups.
4.2. Analysis.
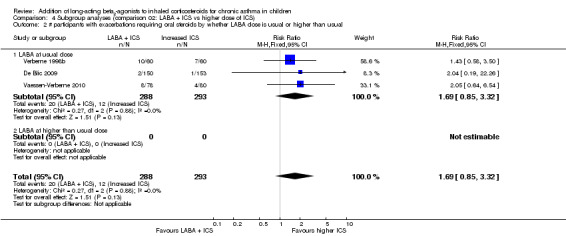
Comparison 4 Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS), Outcome 2 # participants with exacerbations requiring oral steroids by whether LABA dose is usual or higher than usual.
4.3. Analysis.
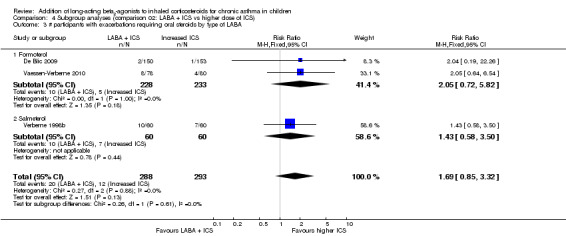
Comparison 4 Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS), Outcome 3 # participants with exacerbations requiring oral steroids by type of LABA.
4.4. Analysis.
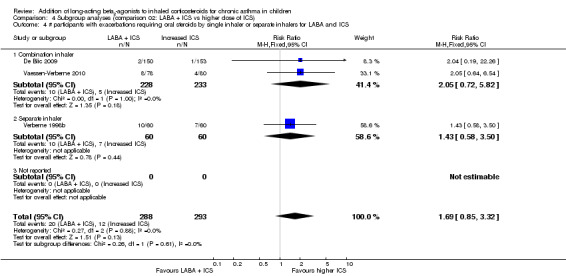
Comparison 4 Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS), Outcome 4 # participants with exacerbations requiring oral steroids by single inhaler or separate inhalers for LABA and ICS.
4.5. Analysis.
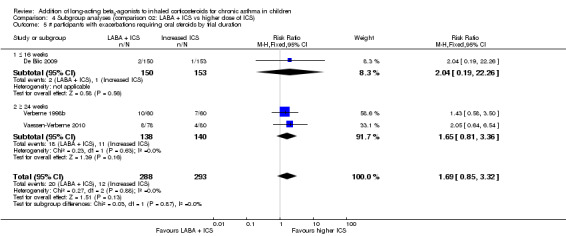
Comparison 4 Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS), Outcome 5 # participants with exacerbations requiring oral steroids by trial duration.
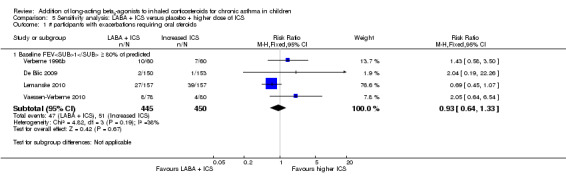
Sensitivity analysis
We performed sensitivity analysis by including data from Lemanske 2010, which was a cross‐over study that reported data on the number of participants with exacerbations requiring oral corticosteroids and contributed the greatest weight by including the largest number of participants. There was no significant group difference in numbers of participants with exacerbations requiring OCS (RR 0.93, 95% CI 0.64 to 1.33, four studies, N = 895; Analysis 5.1). We were not able to perform the other sensitivity analysis, as all trials contributing data on the primary outcome were funded by producers of LABA and ICS, were published as full‐text articles and were double‐blinded.
5.1. Analysis.
Comparison 5 Sensitivity analysis: LABA + ICS versus placebo + higher dose of ICS, Outcome 1 # participants with exacerbations requiring oral steroids.
Secondary outcomes
Hospital admission, urgent care visit, withdrawal
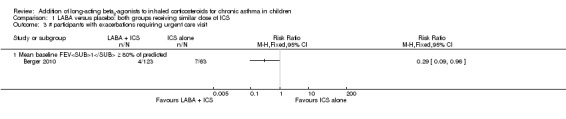
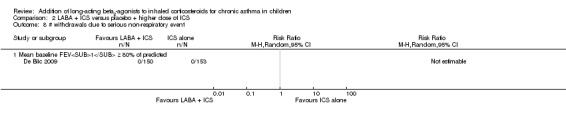
There was no significant group difference in the number of participants with exacerbations requiring hospital admission (RR 1.90, 95% CI 0.65 to 5.54, four studies, N = 1008; Analysis 2.2; Figure 6) or an urgent care visit (RR 5.13, 95% CI 0.25 to 105.10, one study, N = 158; Analysis 2.3). Data also showed no statistically significant group differences in overall risk of all‐cause withdrawals (RR 0.96, 95% CI 0.67 to 1.37, eight studies, N = 1491; Analysis 2.5), withdrawals due to poor asthma control (RR 0.34, 95% CI 0.05 to 2.13, four studies, N = 862; Analysis 2.6) and withdrawals due to adverse events (RR 0.76, 95% CI 0.19 to 3.07, five studies, N = 951; Analysis 2.7). Only one trial reported withdrawals due to a serious non‐respiratory event, none of which occurred (Analysis 2.8), thus preventing aggregation.
2.2. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 2 # participants with exacerbations requiring hospitalisation.
6.
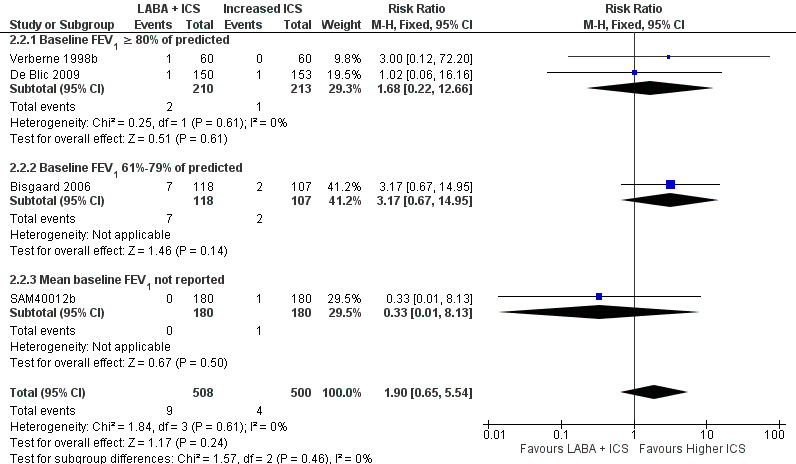
Forest plot of comparison: 2 LABA + ICS versus placebo + higher dose of ICS, outcome: 2.2 # participants with exacerbations requiring hospitalisation.
2.3. Analysis.
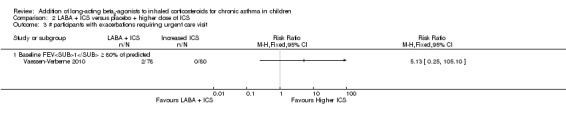
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 3 # participants with exacerbations requiring urgent care visit.
2.5. Analysis.
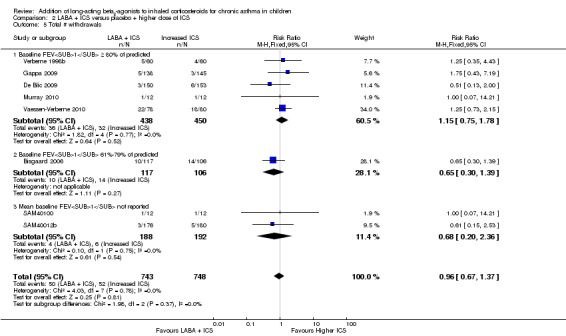
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 5 Total # withdrawals.
2.6. Analysis.
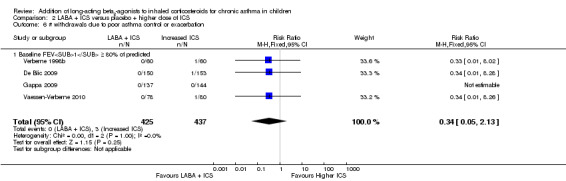
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 6 # withdrawals due to poor asthma control or exacerbation.
2.7. Analysis.
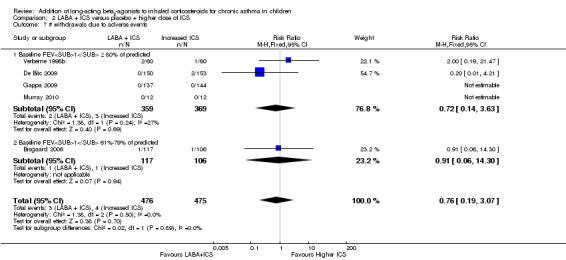
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 7 # withdrawals due to adverse events.
2.8. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 8 # withdrawals due to serious non‐respiratory event.
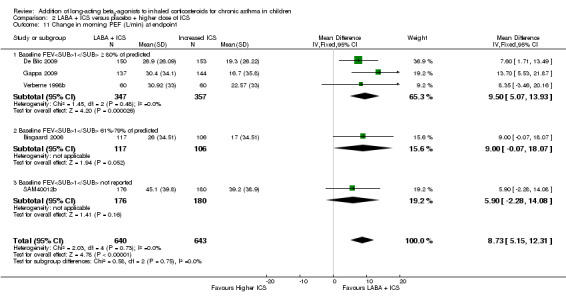
Lung function
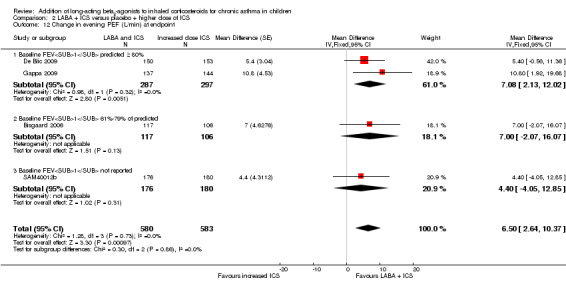
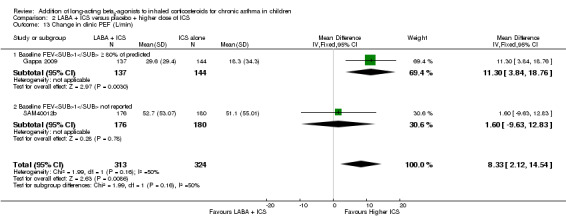
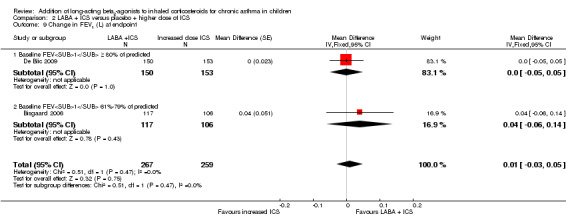
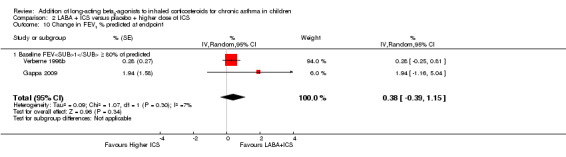
LABA added to ICS led to greater improvement from baseline in the change in morning PEF (MD 8.73 L/min, 95% CI 5.15 to 12.31, five studies, N = 1283; Analysis 2.11) and evening PEF (MD 6.5 L/min, 95% CI 2.64 to 10.37, four studies, N = 1163; Analysis 2.12). Similarly, data showed a significant group difference in change in PEF recorded at clinic visit at the end point (MD 8.33 L/min, 95% CI 2.12 to 14.54, two studies, N = 637; Analysis 2.13). Changes from baseline in FEV1 between treatment options were not statistically significant (MD 0.01 L, 95% CI ‐0.03 to 0.05, two trials, N = 526; Analysis 2.9; and MD 0.38%, 95% CI ‐0.39 to 1.15, two trials, N = 682; Analysis 2.10). Data were insufficient for pooling of other lung function data.
2.11. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 11 Change in morning PEF (L/min) at endpoint.
2.12. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 12 Change in evening PEF (L/min) at endpoint.
2.13. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 13 Change in clinic PEF (L/min).
2.9. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 9 Change in FEV1 (L) at endpoint.
2.10. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 10 Change in FEV1 % predicted at endpoint.
Symptoms and SABA
There was no statistically significant group difference in change in daytime asthma symptom score (MD 0.01 L, 95% CI ‐0.20 to 0.23, three studies, N = 329; Analysis 2.17) and change in nighttime asthma symptom score (MD 0.01 L, 95% CI ‐0.20 to 0.23, three studies, N = 329; Analysis 2.18). Studies were insufficient for aggregation of other data related to markers of symptoms and use of rescue SABA.
2.17. Analysis.
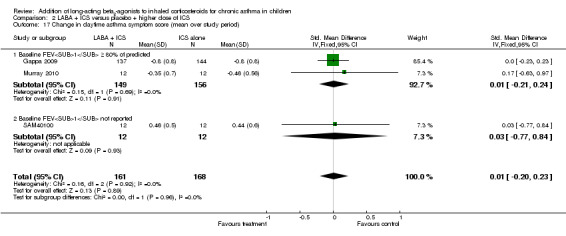
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 17 Change in daytime asthma symptom score (mean over study period).
2.18. Analysis.
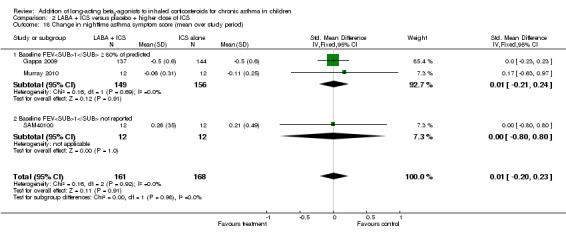
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 18 Change in nighttime asthma symptom score (mean over study period).
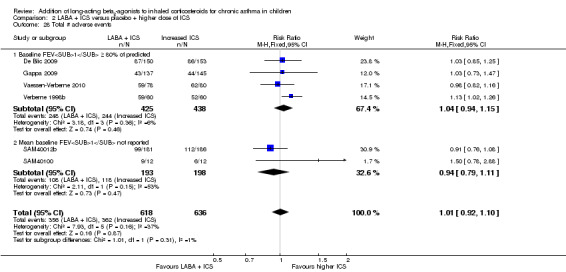
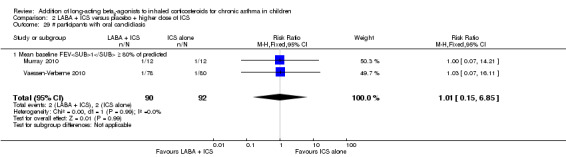
Adverse events
There was no statistically significant difference in risk of overall adverse effects (RR 1.01, 95% CI 0.92 to 1.10, seven studies, N = 1254; Analysis 2.28), meeting our a priori criteria for equivalence. However, the specific adverse events have wide confidence intervals, so we cannot rule out a difference in any of these specific events. Data show no significant group difference in risk of oral candidiasis (RR 0.76, 95% CI 0.17 to 3.30, three studies, N = 182; Analysis 2.29), headache (RR 1.13, 95% CI 0.85 to 1.50, five studies, N = 1230; Analysis 2.30) and serious adverse events (RR 1.54, 95% CI 0.81 to 2.94, seven studies, N = 1343; Analysis 2.4). Other adverse events including vomiting, cold, upper respiratory tract infection and death could not be aggregated because trials reporting data are lacking. Two studies measured linear growth over one year (Verberne 1998b; Bisgaard 2006); findings favoured LABA treatment for children by an average of 1.21 cm/y (95% CI 0.72 to 1.7; Analysis 2.34).
2.28. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 28 Total # adverse events.
2.29. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 29 # participants with oral candidiasis.
2.30. Analysis.
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 30 # participants with headache.
2.4. Analysis.
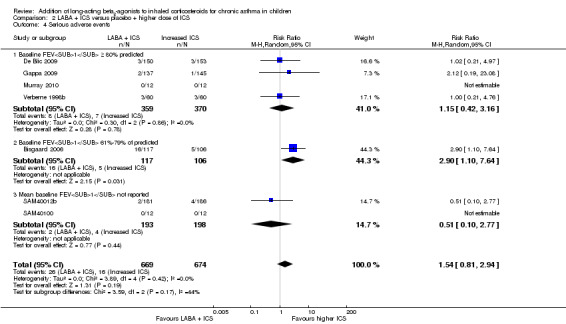
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 4 Serious adverse events.
2.34. Analysis.
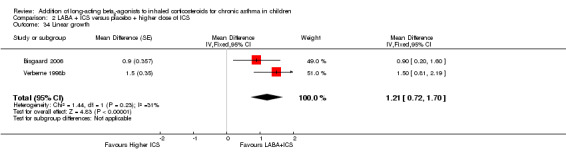
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 34 Linear growth.
Discussion
Summary of main results
Exacerbations requiring systemic steroids in school‐aged children with inadequately controlled asthma despite the use of daily low‐dose ICS were not significantly reduced by adding LABA to ICS compared with using the same, or an increased, dose of ICS. A priori defined subgroup analysis indicates that characteristics of participants or of the intervention did not influence outcomes.
Although not statistically significant, a trend towards increased risk of exacerbations requiring hospital admissions was noted in children treated with combination therapy. This trend towards increased risk of hospital admission with the addition of LABA compared with the same dose of ICS (step 2) or an increased dose of ICS (step 3) is a matter of concern, particularly as combination therapy failed to show any benefit in reducing severity markers including the primary outcome, that is, exacerbation requiring systemic steroids.
With regard to secondary outcomes, lung function endpoints consistently favoured the addition of LABA to ICS therapy, whether compared with the same or an increased dose of ICS. A modest reduction in the use of rescue SABA was evident with the addition of LABA to ICS when compared with the same dose of ICS; however, data were insufficient to pool for comparison with an increased ICS dose. In contrast, LABA added to ICS did not result in significantly greater improvement in asthma symptoms compared with the same or an increased dose of ICS. With the exception of growth, data show no statistically significant group differences in reported adverse events; overall adverse events met our definition of equivalence. The combination of LABA and ICS led to greater gain in linear growth than was seen with an increased dose of ICS; this is consistent with recent findings of a dose‐response effect of ICS on growth in children (Pruteanu 2014).
In this paediatric review, LABA added to ICS did not result in improvement in most other clinical indicators of asthma control and future risk of exacerbations. We recognised that absence of a significant group difference in other clinical indicators of asthma control may be due to mild asthma severity among most participants. Yet, aggregation of the best available evidence to date provides little data to support the addition of LABA to ICS in children insufficiently controlled by ICS monotherapy.
Overall completeness and applicability of evidence
Although we identified several unpublished studies, we had only limited success in obtaining useable data for our primary outcome. We successfully obtained data for exacerbations requiring rescue systemic steroids and for hospital admissions for a small number of trials from a recent meta‐analysis of GSK‐sponsored trials (Bateman 2008). Few data in study reports are available as downloads from pharmaceutical company trial results registries.
Quality of the evidence
Overall we judged the quality of evidence to be moderate. Most outcomes showed wide confidence intervals, which led to downgrading of evidence quality to moderate. In a few outcomes for which open‐label studies contributed data, we further downgraded evidence quality to low.
Potential biases in the review process
These findings are consistent with findings of Bisgaard 2003. Of note, about half of the trials in our review were conducted in school‐aged children treated predominantly with ICS and LABA delivered in separate (rather than single) devices. Although adherence to ICS may have been suboptimal, we cannot speculate whether different results would have been obtained if most trials had used a single device to deliver LABA and ICS. Is it possible that ongoing inflammation associated with use of a lower dose of ICS or tachyphylaxis associated with prolonged use of LABA may be associated with more severe exacerbations with combination therapy. In light of the prevailing uncertainty and an FDA mandate, a large six‐month study, to evaluate safety and benefit of LABA and ICS (salmeterol and fluticasone), is ongoing in children of four to 11 years of age. Outcomes of the study will shed more light on the safety and benefits of this combination (NCT01462344).
Agreements and disagreements with other studies or reviews
Our findings contrast with some of the estimates derived from the systematic review of adult trials performing the same comparisons (Ducharme 2010). Indeed, when compared with a similar dose of ICS, LABA added to ICS reduces by 20% the risk for adults with exacerbations requiring systemic steroids (RR 0.77, 95% CI 0.68 to 0.88; Ducharme 2010). This was accompanied by notably greater improvement in lung function (170 mL in FEV1) and symptom‐free days (+ 17%) and a modest reduction in use of rescue SABA (‐0.7 puffs/d). Given the smaller lung volumes in children, the observed 80 mL greater improvement in FEV1 associated with LABA added to ICS in children may be of clinical importance. However, observed improvement in lung function was expected, given that LABA is a bronchodilator, and children were selected primarily on the basis of significant reversibility with SABA to confirm the diagnosis of asthma. This apparent discordance between outcomes may be due to a more rapid effect of LABA on lung function, which is more easily detectable in studies of short duration, whereas a longer period of follow‐up may be required to detect an effect on exacerbations, particularly among children with normal or near normal lung function.
With regard to the second comparison ‐ LABA and ICS versus a higher dose of ICS ‐ findings also differ from a Cochrane Review of studies in adults (Ducharme 2010a), which demonstrates a significant reduction associated with LABA in the risk of patients with exacerbations requiring rescue systemic steroids (RR 0.88, 95% CI 0.78 to 0.98). Despite identification of 11 studies, only four provided data for the primary outcome. A modest improvement (< 9 L/min) in morning and evening PEF, but not in FEV1, was associated with use of LABA compared with a higher ICS dose. Insufficient reporting prevented aggregation of most outcomes. However, the trend towards a higher proportion of exacerbations requiring hospital admission and serious adverse events in children using LABA in combination with ICS, compared with a high dose of ICS, is a matter of concern. Findings are consistent with an overview of Cochrane Reviews evaluating the safety of formoterol or salmeterol in children with asthma (Cates 2012), in which review authors reported an additional three children per 1000 who suffered a non‐fatal serious adverse event with combination therapy in comparison with ICS over three months. Meanwhile, available data are also insufficient to allow firm recommendations regarding the preference of increasing the ICS dose versus adding LABA to ICS as a step 3 strategy. One must weigh the greater linear growth (reported in only two trials with beclomethasone and budesonide ‐ molecules known to be associated with growth suppression) (Skoner 2000; CAMP Research Group 2012) and the improvement in PEF against the possible, but unproven, increased risk of greater severity of exacerbations associated with combination therapy.
Data show no group differences in adverse effects or withdrawals due to adverse effects when the combination of LABA and ICS was compared with the step 2 or step 3 strategy. Of note, side effects were scarcely reported in short‐term trials, and long‐term studies were lacking. Moreover, although an increased dose of ICS calls for assessment of growth, adrenal function and bone mineralisation in children, no trial reported data on adrenal function and bone mineralisation that could be aggregated. Only two studies reporting the addition of LABA to 400 versus 800 μg of beclomethasone (Verberne 1998b) and to 100 versus 400 μg of budesonide (Bisgaard 2006) examined growth, for a differential of 300 to 400 μg of BDP‐equivalent. The observed reduction in growth averaging 1.2 cm/y is consistent with the documented decrease in linear growth associated with 400 μg/d of BDP (Sharek 1999; Pruteanu 2014) and the documented dose‐response relationship between growth impairment and ICS dose (Pruteanu 2014). Any apparent benefit of doubling the dose of ICS should be weighed against the possible impact on growth compared with other therapeutic regimens; it deserves careful evaluation (Pruteanu 2014).
Authors' conclusions
Implications for practice.
Evidence is insufficient at present to firmly support use of LABA as an adjunct therapy to ICS as a step 3 strategy to reduce risk of asthma exacerbations requiring steroids, as compared with using the usual dose of ICS (step 2) or an increased dose of ICS (step 3). The wide confidence intervals do not rule out a superior effect of either treatment. Stepping up therapy with the addition of LABA to the usual dose of ICS improves lung function beyond that observed when remaining on ICS as step 2 strategy, but with no apparent benefits of asthma symptom control and use of rescue SABA. Similarly, significant improvements in morning PEF observed with the combination of LABA and usual ICS dose versus an increased dose of ICS have not been associated with improvement in other indicators of lung function and asthma control. The apparent reduction in growth associated with use of 400 to 800 μg/d of BDP‐equivalent raises concern when high‐dose beclomethasone or budesonide is considered as increased ICS (step 3 therapy). Of note, the trend towards increased hospital admission with LABA, irrespective of the dose of ICS, and toward serious adverse health events compared with an increased dose of ICS is a matter of some concern and calls for larger, longer‐term trials in children with substantial morbidity, to clarify this issue.
Implications for research.
Future trials should have the following characteristics.
Population
A large study is urgently needed in children with moderate and severe airway obstruction and with higher asthma morbidity (e.g. prior hospital admission, requirement for OCS) at baseline than those recruited to trials aggregated in this review. Stratification according to degree of airway obstruction (i.e. baseline FEV1) and inclusion of younger, preschool‐aged children should feature in the design of such trials. Use of diagnostic criteria for asthma that do not require a positive bronchodilator response for enrolment would allow the study to be more generalisable to the general paediatric asthma population and would reduce the potential overestimation of effect on lung function (by preselecting responders to SABA).
Interventions
Future interventions should test the combination therapy delivered by a single inhaler (combining LABA and ICS) to ensure no use of LABA as monotherapy. Interventions may include head‐to‐head comparisons of salmeterol versus formoterol, combined with low or moderate doses of ICS. The control intervention should focus on increased doses of ICS (step 3), so that two step 3 treatment strategies are compared.
Design
Double‐blinding, adequate randomisation and complete reporting of withdrawals and dropouts with an explicit definition of the intention‐to‐treat population analysed.
Intervention period of 24 to 52 weeks or longer, to properly assess the impact on exacerbations requiring systemic corticosteroids and those resulting in hospital admission, as well as adverse health events (growth, adrenal function, bone mineralisation, serious adverse health events).
Clear reporting of the percentage of (and reasons for) non‐eligibility of approached participants and of those enrolled in the run‐in period is required, as inadequate reporting of the selected population results in difficulty identifying to whom the results can be generalised.
Complete reporting of continuous (denominators, mean change and mean standard deviation of change) and dichotomous (denominators and rate) data in the units used in this systematic review would allow aggregation of data.
Outcomes of particular importance to assess include the following.
Exacerbations requiring rescue systemic corticosteroids.
Asthma‐related hospital admission or acute care visit.
Compliance with either intervention both before (for ICS) and after randomisation (for both ICS and combination therapy). The impact of compliance with combination therapy versus placebo and ICS on the magnitude of the effect size should be examined.
Cost‐effectiveness of use of combination inhalers as compared with ICS alone.
Serious or overall adverse events associated with LABA or ICS especially growth, adrenal function, bone mineralisation.
Functional measures including quality of life.
An ongoing large six‐month study on safety and benefit of LABA and ICS (salmeterol and fluticasone) in children four to 11 years of age may provide further evidence to support our preliminary outcomes (NCT01462344).
What's new
| Date | Event | Description |
|---|---|---|
| 23 January 2015 | New citation required but conclusions have not changed | 8 studies added ‐ conclusions similar Few new outcomes added ‐ urgent care visits, nighttime awakenings ‐ new lead author added Results and discussion redrafted. Summary of findings tables added |
| 23 January 2015 | New search has been performed | New literature search run |
History
Review first published: Issue 3, 2009
| Date | Event | Description |
|---|---|---|
| 8 December 2009 | Amended | We have revised the reporting of correspondence in relation to missing data Correspondence regarding data from Bisgaard 2006 was made directly with study sponsors, not with Hans Bisgaard. Sponsors were not able to provide data on children in this study with exacerbations requiring oral corticosteroids |
| 21 April 2008 | Amended | Converted to new review format |
Acknowledgements
We thank Toby Lasserson and Ilana Greenstone for their contributions to protocol development, data extraction, analysis and drafting of the original version of this review. We thank the Cross Canada Respiratory Rounds Review Group for their valuable comments on the first version of the review. We are indebted to the Cochrane Airways Review Group, namely, Stephen Milan, Elizabeth Stovold, Veronica Stewart, Karen Blackhall and Bettina Reuben, for assistance with the literature search and ongoing support, as well as to Peter Gibson and Christopher Cates for their constructive comments. We are indebted to the trialists who provided us with data and information regarding their studies, namely, A. Tal, E. Simons, G. Russell, F. Meijer, P. Pohunek, C. Sorkne and A.A.P.H. Verberne. We thank Richard Follows, Tracey Armstrong and Maggie Hemedah from GlaxoSmithKline; and Robyn von Maltzahn, Nils Grundstrom and Roger Metcalf from AstraZeneca; who cooperated with our requests for information. We obtained data from only four studies Verberne 1998b, De Blic 2009, Lemanske 2010 and Vaessen‐Verberne 2010.
The Background and Methods sections of this review are based on a standard template used by the Cochrane Airways Group.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Group Specialised Register (CAGR)
Electronic searches: core databases
| Database | Frequency of search |
| CENTRAL (The Cochrane Library) | Monthly |
| MEDLINE (Ovid) | Weekly |
| EMBASE (Ovid) | Weekly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify trials for the CAGR
Asthma search
1. exp Asthma/
2. asthma$.mp.
3. (antiasthma$ or anti‐asthma$).mp.
4. Respiratory Sounds/
5. wheez$.mp.
6. Bronchial Spasm/
7. bronchospas$.mp.
8. (bronch$ adj3 spasm$).mp.
9. bronchoconstrict$.mp.
10. exp Bronchoconstriction/
11. (bronch$ adj3 constrict$).mp.
12. Bronchial Hyperreactivity/
13. Respiratory Hypersensitivity/
14. ((bronchial$ or respiratory or airway$ or lung$) adj3 (hypersensitiv$ or hyperreactiv$ or allerg$ or insufficiency)).mp.
15. ((dust or mite$) adj3 (allerg$ or hypersensitiv$)).mp.
16. or/1‐15
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomized or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter are adapted to identify trials in other electronic databases.
Appendix 2. Search methods up to May 2008
Electronic searches
An electronic literature search was carried out in the Cochrane Airways Group Specialised Register of asthma trials which is derived from systematic searches of bibliographic databases including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and CINAHL and handsearching of respiratory journals and meeting abstracts. This Register also contains a variety of studies published in foreign languages. We did not exclude trials on the basis of language. The Register was searched using the following terms:
(((beta* and agonist*) and long‐acting or "long‐acting") or ((beta* and adrenergic*) and long‐acting or "long‐acting") or (bronchodilat* and long‐acting or "long‐acting") or (salmeterol or formoterol or advair or symbicort)) and (((steroid* or glucocorticoid* or corticosteroid*) and inhal*) or (budesonide or beclomethasone or fluticasone or triamcinolone or flunisolide)).
This search was then limited with the text word terms (child* or paediat* or pediat* or adolesc* or infan* or toddler* or bab* or young* or preschool* or "pre school*" or pre‐school* or newborn* or "new born*" or new‐born* or neo‐nat* or neonat*)
Appendix 3. Search strategy to identify relevant trials from the CAGR
#1 AST:MISC1
#2 MeSH DESCRIPTOR Asthma Explode All
#3 asthma*:ti,ab
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Adrenergic beta‐2 Receptor Antagonists
#6 (beta* and agonist*) and (long‐acting or "long acting")
#7 (beta* and adrenergic*) and (long‐acting or "long acting")
#8 bronchodilat* and (long‐acting or "long acting")
#9 salmeterol
#10 *formoterol
#11 #5 or #6 or #7 or #8 or #9 or #10
#12 MeSH DESCRIPTOR Glucocorticoids Explode All
#13 budesonide
#14 beclomethasone
#15 beclometasone
#16 fluticasone
#17 triamcinolone
#18 flunisolide
#19 ciclesonide
#20 #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19
#21 #11 and #20
#22 Advair or symbicort or Viani or Seretide or Flutiform
#23 #21 or #22
#24 #4 and #23
#25 child* or paediat* or pediat* or adolesc* or infan* or toddler* or bab* or young* or preschool* or "pre school*" or pre‐school* or newborn* or "new born*" or new‐born* or neo‐nat* or neonat*
#26 #24 and #25
[In search line #1, MISC1 denotes the field in which the reference has been coded for condition, in this case, asthma]
Appendix 4. Randomisation procedures for GSK‐sponsored studies
The procedures for randomising GSK‐sponsored studies has been detailed in correspondence between Richard Follows and TL, the details of which are given below:
The randomisation software is a computer‐generated, centralised programme (RandAll). After verification that the randomisation sequence is suitable for the study design (crossover, block or stratification), Clinical Supplies then package the treatments according the randomisation list generated. Concealment of allocation is maintained by a third party, since the sites phone in and are allocated treatments on that basis. Alternatively a third party may dispense the drug at the sites. Unblinding of data for interim analyses can only be done through RandAll, and are restricted so that only those reviewing the data are unblinded to treatment group allocation.
Data and analyses
Comparison 1. LABA versus placebo: both groups receiving similar dose of ICS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # participants with exacerbations requiring systemic steroids | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 1.1 Mean baseline FEV1 ≥ 80% of predicted | 9 | 1399 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.69, 1.37] |
| 1.2 Mean baseline FEV1 61%‐79% of predicted | 2 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.48, 1.64] |
| 1.3 Mean baseline FEV1 not reported | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 # participants with exacerbations requiring hospitalisation | 7 | 1292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.90, 3.36] |
| 2.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.36, 6.14] |
| 2.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [0.86, 3.82] |
| 2.3 Mean baseline FEV1 not reported | 1 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 # participants with exacerbations requiring urgent care visit | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Serious adverse events | 17 | 4021 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.75, 1.85] |
| 4.1 Mean baseline FEV1 ≥ 80% of predicted | 13 | 2897 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.53, 1.92] |
| 4.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 762 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.68, 2.59] |
| 4.3 Mean baseline FEV1 not reported | 1 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.18, 21.86] |
| 5 Total # withdrawals | 23 | 4374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.67, 0.94] |
| 5.1 Mean baseline FEV1 ≥ 80% of predicted | 17 | 3205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.66, 0.96] |
| 5.2 Mean baseline FEV1 61%‐79% of predicted | 4 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.63, 1.32] |
| 5.3 Mean baseline FEV1 not reported | 2 | 375 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.12, 1.11] |
| 6 # withdrawals due to poor asthma control or exacerbation | 14 | 2255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.57, 1.16] |
| 6.1 Mean baseline FEV1 ≥ 80% of predicted | 10 | 1461 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.55, 1.21] |
| 6.2 Mean baseline FEV1 61%‐79% of predicted | 4 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.34, 1.81] |
| 7 # withdrawals due to adverse events | 18 | 4117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.52, 1.21] |
| 7.1 Mean baseline FEV1 ≥ 80% of predicted | 13 | 3053 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.42, 1.13] |
| 7.2 Mean baseline FEV1 61%‐79% of predicted | 5 | 1064 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.51, 2.44] |
| 8 # withdrawals due to serious non‐respiratory event | 2 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 4.66 [0.23, 96.30] |
| 8.1 Mean baseline FEV1 61%‐79% of predicted | 2 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 4.66 [0.23, 96.30] |
| 9 Change in FEV1 (L) at endpoint | 9 | 1942 | Litres (Fixed, 95% CI) | 0.08 [0.06, 0.10] |
| 9.1 Mean baseline FEV1 ≥ 80% of predicted | 7 | 1515 | Litres (Fixed, 95% CI) | 0.08 [0.05, 0.10] |
| 9.2 Mean baseline FEV1 61%‐79% of predicted | 2 | 427 | Litres (Fixed, 95% CI) | 0.12 [0.04, 0.19] |
| 10 Change in FEV1 at endpoint (% predicted) stratifying on baseline FEV1 | 7 | 534 | Mean Difference (IV, Fixed, 95% CI) | 2.99 [0.86, 5.11] |
| 10.1 Mean baseline FEV1 ≥ 80% of predicted | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | 4.06 [1.32, 6.80] |
| 10.2 Mean baseline FEV1 61%‐79% of predicted | 2 | 238 | Mean Difference (IV, Fixed, 95% CI) | 3.35 [‐1.50, 8.20] |
| 10.3 Mean baseline FEV1 not reported | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐5.03, 4.23] |
| 11 % fall in FEV1 % predicted due to exercise | 3 | 517 | Mean Difference (IV, Fixed, 95% CI) | 0.46 [1.00, 1.93] |
| 11.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 517 | Mean Difference (IV, Fixed, 95% CI) | 0.46 [1.00, 1.93] |
| 12 Change in morning PEF (L/min) at endpoint | 16 | 3934 | L/min (Fixed, 95% CI) | 10.20 [8.14, 12.26] |
| 12.1 Mean baseline FEV1 ≥ 80% of predicted | 12 | 2870 | L/min (Fixed, 95% CI) | 10.79 [8.43, 13.16] |
| 12.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 713 | L/min (Fixed, 95% CI) | 9.26 [4.42, 14.10] |
| 12.3 Mean baseline FEV1 not reported | 1 | 351 | L/min (Fixed, 95% CI) | 5.7 [‐2.62, 14.02] |
| 13 Change in morning PEF (% predicted) | 1 | % (Fixed, 95% CI) | Totals not selected | |
| 13.1 Mean baseline FEV1 61%‐79% of predicted | 1 | % (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Change in evening PEF (L/min) at endpoint | 12 | 3140 | L/min (Fixed, 95% CI) | 9.30 [6.96, 11.65] |
| 14.1 Mean baseline FEV1 ≥ 80% of predicted | 10 | 2503 | L/min (Fixed, 95% CI) | 9.31 [6.67, 11.94] |
| 14.2 Mean baseline FEV1 61%‐79% of predicted | 1 | 286 | L/min (Fixed, 95% CI) | 11.7 [5.29, 18.11] |
| 14.3 Mean baseline FEV1 not reported | 1 | 351 | L/min (Fixed, 95% CI) | 5.0 [‐3.58, 13.58] |
| 15 Change in evening PEF (% of predicted) | 1 | % (Fixed, 95% CI) | Totals not selected | |
| 15.1 Mean baseline FEV1 61%‐79% of predicted | 1 | % (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Change in clinic PEF (L/min) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Mean baseline FEV1 not reported | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Change in PEF variability at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Mean baseline FEV1 61%‐79% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Mean change in asthma symptom score | 6 | 1653 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.17, 0.04] |
| 18.1 Mean baseline FEV1 ≥ 80% of predicted | 6 | 1653 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.17, 0.04] |
| 19 Change in nighttime symptom score | 2 | 534 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.07, 0.02] |
| 19.1 Mean baseline FEV1 ≥ 80% of predicted | 2 | 534 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.07, 0.02] |
| 20 Change in % symptom‐free days at endpoint | 7 | 1831 | Mean Difference (IV, Fixed, 95% CI) | 0.96 [‐1.91, 3.84] |
| 20.1 Mean baseline FEV1 ≥ 80% of predicted | 7 | 1831 | Mean Difference (IV, Fixed, 95% CI) | 0.96 [‐1.91, 3.84] |
| 21 % symptom‐free days | 4 | 623 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.20, 0.12] |
| 21.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | 231 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.47, 0.05] |
| 21.2 Mean baseline FEV1 61%‐79% of predicted | 1 | 286 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.11, 0.35] |
| 21.3 Unclear baseline FEV1 | 2 | 106 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.56, 0.31] |
| 22 % symptom‐free nights at 52 ± 4 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 Mean baseline FEV1 not reported | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Change in # daytime rescue inhalations (puffs per day) at endpoint | 7 | 1798 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.11, ‐0.02] |
| 23.1 Mean baseline FEV1 61%‐79% of predicted | 7 | 1798 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.11, ‐0.02] |
| 24 Change in # nighttime rescue inhalations at endpoint | 3 | 672 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.13, ‐0.03] |
| 24.1 Mean baseline FEV1 61%‐79% of predicted | 3 | 672 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.13, ‐0.03] |
| 25 % days without bronchodilator usage | 7 | 1710 | Mean Difference (IV, Random, 95% CI) | 2.07 [‐1.03, 5.16] |
| 25.1 Mean baseline FEV1 ≥ 80% of predicted | 6 | 1628 | Mean Difference (IV, Random, 95% CI) | 2.87 [‐0.44, 6.18] |
| 25.2 Mean baseline FEV1 not reported | 1 | 82 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐4.04, 2.04] |
| 26 Change in nighttime awakening (number of nights) at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Mean baseline FEV1 61%‐79% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 % nights with awakening | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 27.1 Mean baseline FEV1 61%‐79% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 % change in awakening‐free nights | 2 | 519 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐1.05, 2.26] |
| 28.1 Mean baseline FEV1 ≥ 80% of predicted | 2 | 519 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐1.05, 2.26] |
| 29 Change in rescue‐free days (%) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Change in % asthma‐control days at endpoint | 2 | 519 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐0.56, 9.16] |
| 30.1 Mean baseline FEV1 ≥ 80% of predicted | 2 | 519 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐0.56, 9.16] |
| 31 Change in quality of life (P‐AQLQ) | 4 | 668 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.14, 0.10] |
| 31.1 Mean baseline FEV1 ≥ 80% of predicted | 4 | 668 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.14, 0.10] |
| 32 Quality of life (P‐AQLQ) | 10 | 2333 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.04, 0.11] |
| 32.1 Mean baseline FEV1 ≥ 80% of predicted | 6 | 1586 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.01, 0.16] |
| 32.2 Mean baseline FEV1 61%‐79% of predicted | 4 | 747 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.28, 0.03] |
| 33 Change in paediatric asthma caregiver quality of life (P‐AQLQ) | 4 | 669 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.18] |
| 33.1 Mean baseline FEV1 ≥ 80% of predicted | 4 | 669 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.05, 0.18] |
| 34 Total # adverse events | 15 | 3284 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.98, 1.10] |
| 34.1 Mean baseline FEV1 ≥ 80% of predicted | 11 | 2424 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.00, 1.16] |
| 34.2 Mean baseline FEV1 61%‐79% of predicted | 2 | 474 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.86, 1.09] |
| 34.3 Mean baseline FEV1 not reported | 2 | 386 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 35 # participants with oral candidiasis | 6 | 1341 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.41 [0.73, 15.87] |
| 35.1 FEV1 ≥ 80% of predicted | 5 | 1135 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.46 [0.60, 19.99] |
| 35.2 Mean baseline FEV1 61%‐79% of predicted | 1 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.13, 78.62] |
| 36 # participants with tremor | 6 | 1467 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.38, 25.05] |
| 36.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 959 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.30 [0.26, 109.66] |
| 36.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 508 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.06, 35.18] |
| 37 # participants with tachycardia or palpitations | 6 | 1238 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.08, 2.31] |
| 37.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 731 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.05, 3.33] |
| 37.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.03, 7.61] |
| 38 # participants with headache | 14 | 2966 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.90, 1.33] |
| 38.1 Mean baseline FEV1 ≥ 80% of predicted | 8 | 1779 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.79, 1.26] |
| 38.2 Mean baseline FEV1 61%‐79% of predicted | 5 | 825 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.88, 2.04] |
| 38.3 Mean baseline FEV1 not reported | 1 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.4 [0.64, 3.07] |
| 39 # participants with vomiting | 3 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.34, 1.62] |
| 39.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.34, 1.62] |
| 40 # participants with otitis media | 3 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.30, 1.63] |
| 40.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.30, 1.63] |
| 41 # participants with upper respiratory tract infection | 5 | 1186 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.58, 1.27] |
| 41.1 Mean baseline FEV1 ≥ 80% of predicted | 5 | 1186 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.58, 1.27] |
| 42 # participants with urticaria | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 42.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 43 # participants with adverse cardiovascular events | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.49] |
| 43.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.49] |
| 43.2 Mean baseline FEV1 61%‐79% of predicted | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 44 Deaths | 3 | 690 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.01, 0.01] |
| 44.1 Baseline FEV1 ≥ 80% of predicted | 3 | 690 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.01, 0.01] |
| 45 # participants with exacerbations requiring hospitalisation | 7 | 1292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.90, 3.36] |
| 45.1 Mean baseline FEV1 ≥ 80% of predicted | 3 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.36, 6.14] |
| 45.2 Mean baseline FEV1 61%‐79% of predicted | 3 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [0.86, 3.82] |
| 45.3 Mean baseline FEV1 not reported | 1 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 46 Change in height (cm) as SD scores at 24 ± 4 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 46.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 47 Change in height at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.45. Analysis.
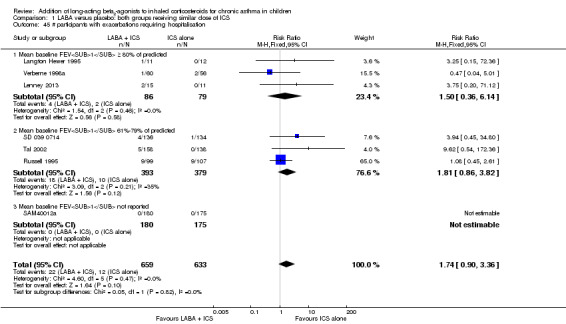
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 45 # participants with exacerbations requiring hospitalisation.
1.46. Analysis.
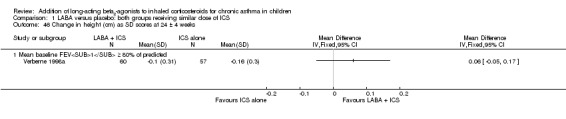
Comparison 1 LABA versus placebo: both groups receiving similar dose of ICS, Outcome 46 Change in height (cm) as SD scores at 24 ± 4 weeks.
Comparison 2. LABA + ICS versus placebo + higher dose of ICS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # participants with exacerbations requiring oral steroids | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 1.1 Baseline FEV1 ≥ 80% of predicted | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 2 # participants with exacerbations requiring hospitalisation | 4 | 1008 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.65, 5.54] |
| 2.1 Baseline FEV1 ≥ 80% of predicted | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.22, 12.66] |
| 2.2 Baseline FEV1 61%‐79% of predicted | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.17 [0.67, 14.95] |
| 2.3 Mean baseline FEV1 not reported | 1 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.13] |
| 3 # participants with exacerbations requiring urgent care visit | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Serious adverse events | 7 | 1343 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [0.81, 2.94] |
| 4.1 Baseline FEV1 ≥ 80% predicted | 4 | 729 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.42, 3.16] |
| 4.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 2.90 [1.10, 7.64] |
| 4.3 Mean baseline FEV1 not reported | 2 | 391 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.10, 2.77] |
| 5 Total # withdrawals | 8 | 1491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.67, 1.37] |
| 5.1 Baseline FEV1 ≥ 80% of predicted | 5 | 888 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.75, 1.78] |
| 5.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.30, 1.39] |
| 5.3 Mean baseline FEV1 not reported | 2 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.20, 2.36] |
| 6 # withdrawals due to poor asthma control or exacerbation | 4 | 862 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.05, 2.13] |
| 6.1 Baseline FEV1 ≥ 80% of predicted | 4 | 862 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.05, 2.13] |
| 7 # withdrawals due to adverse events | 5 | 951 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.19, 3.07] |
| 7.1 Baseline FEV1 ≥ 80% of predicted | 4 | 728 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.14, 3.63] |
| 7.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.06, 14.30] |
| 8 # withdrawals due to serious non‐respiratory event | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Change in FEV1 (L) at endpoint | 2 | 526 | Mean Difference (Fixed, 95% CI) | 0.01 [‐0.03, 0.05] |
| 9.1 Baseline FEV1 ≥ 80% of predicted | 1 | 303 | Mean Difference (Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 9.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Mean Difference (Fixed, 95% CI) | 0.04 [‐0.06, 0.14] |
| 10 Change in FEV1 % predicted at endpoint | 2 | % (Random, 95% CI) | 0.38 [‐0.39, 1.15] | |
| 10.1 Baseline FEV1 ≥ 80% of predicted | 2 | % (Random, 95% CI) | 0.38 [‐0.39, 1.15] | |
| 11 Change in morning PEF (L/min) at endpoint | 5 | 1283 | Mean Difference (IV, Fixed, 95% CI) | 8.73 [5.15, 12.31] |
| 11.1 Baseline FEV1 ≥ 80% of predicted | 3 | 704 | Mean Difference (IV, Fixed, 95% CI) | 9.50 [5.07, 13.93] |
| 11.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Mean Difference (IV, Fixed, 95% CI) | 9.0 [‐0.07, 18.07] |
| 11.3 Baseline FEV1 not reported | 1 | 356 | Mean Difference (IV, Fixed, 95% CI) | 5.90 [‐2.28, 14.08] |
| 12 Change in evening PEF (L/min) at endpoint | 4 | 1163 | Mean Difference (Fixed, 95% CI) | 6.50 [2.64, 10.37] |
| 12.1 Baseline FEV1 predicted ≥ 80% | 2 | 584 | Mean Difference (Fixed, 95% CI) | 7.08 [2.13, 12.02] |
| 12.2 Baseline FEV1 61%‐79% of predicted | 1 | 223 | Mean Difference (Fixed, 95% CI) | 7.0 [‐2.07, 16.07] |
| 12.3 Baseline FEV1 not reported | 1 | 356 | Mean Difference (Fixed, 95% CI) | 4.4 [‐4.05, 12.85] |
| 13 Change in clinic PEF (L/min) | 2 | 637 | Mean Difference (IV, Fixed, 95% CI) | 8.33 [2.12, 14.54] |
| 13.1 Baseline FEV1 ≥ 80% of predicted | 1 | 281 | Mean Difference (IV, Fixed, 95% CI) | 11.3 [3.84, 18.76] |
| 13.2 Baseline FEV1 not reported | 1 | 356 | Mean Difference (IV, Fixed, 95% CI) | 1.60 [‐9.63, 12.83] |
| 14 Change in morning PEF (% predicted) at endpoint | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Change in evening PEF (% predicted) at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Change in % of days with a peak flow variability ≥ 20% | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Change in daytime asthma symptom score (mean over study period) | 3 | 329 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.20, 0.23] |
| 17.1 Baseline FEV1 ≥ 80% of predicted | 2 | 305 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.21, 0.24] |
| 17.2 Baseline FEV1 not reported | 1 | 24 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.77, 0.84] |
| 18 Change in nighttime asthma symptom score (mean over study period) | 3 | 329 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.20, 0.23] |
| 18.1 Baseline FEV1 ≥ 80% of predicted | 2 | 305 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.21, 0.24] |
| 18.2 Baseline FEV1 not reported | 1 | 24 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.80, 0.80] |
| 19 Change in % of days without asthma symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 # daytime rescue inhalations (puffs per day; mean over study period) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20.1 Baseline FEV1 not reported | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 # nighttime rescue inhalations (puffs per day; mean over study period) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 21.1 Baseline FEV1 not reported | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 # daytime rescue inhalations at endpoint | 1 | puffs/d (Fixed, 95% CI) | Totals not selected | |
| 22.1 Baseline FEV1 61%‐79% of predicted | 1 | puffs/d (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Change in daytime rescue inhalations (puffs per day) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Change in nighttime rescue inhalations (puffs per day) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Change in number of weeks with successful asthma control | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Change in % of days without salbutamol | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Baseline FEV1 ≥ 80% of predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Number of nighttime awakenings | 1 | Awakenings/yr (Fixed, 95% CI) | Totals not selected | |
| 27.1 Baseline FEV1 61%‐79% of predicted | 1 | Awakenings/yr (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 Total # adverse events | 6 | 1254 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.92, 1.10] |
| 28.1 Baseline FEV1 ≥ 80% of predicted | 4 | 863 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.94, 1.15] |
| 28.2 Mean baseline FEV1 not reported | 2 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.79, 1.11] |
| 29 # participants with oral candidiasis | 2 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.15, 6.85] |
| 29.1 Mean baseline FEV1 ≥ 80% of predicted | 2 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.15, 6.85] |
| 30 # participants with headache | 5 | 1230 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.85, 1.50] |
| 30.1 Baseline FEV1 ≥ 80% of predicted | 4 | 863 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.80, 1.46] |
| 30.2 Mean baseline FEV1 not reported | 1 | 367 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.66, 3.16] |
| 31 # participants with vomiting | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 31.1 Baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 # participants with cold | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 32.1 Mean baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33 # participants with upper respiratory tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 33.1 Baseline FEV1 ≥ 80% of predicted | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 34 Linear growth | 2 | Mean Difference (Fixed, 95% CI) | 1.21 [0.72, 1.70] | |
| 35 Deaths | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 35.1 Baseline FEV1 ≥ 80% of predicted | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.14. Analysis.
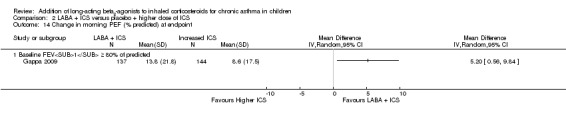
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 14 Change in morning PEF (% predicted) at endpoint.
2.15. Analysis.
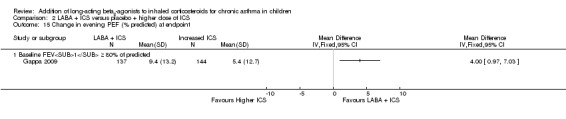
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 15 Change in evening PEF (% predicted) at endpoint.
2.16. Analysis.
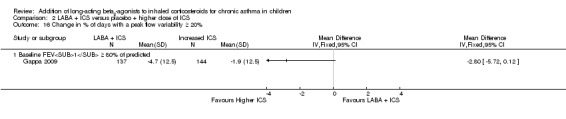
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 16 Change in % of days with a peak flow variability ≥ 20%.
2.19. Analysis.
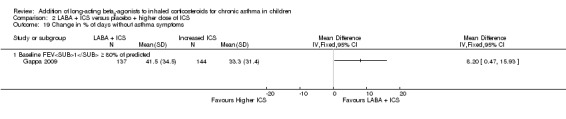
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 19 Change in % of days without asthma symptoms.
2.20. Analysis.
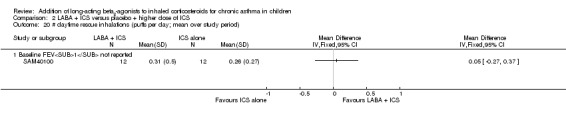
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 20 # daytime rescue inhalations (puffs per day; mean over study period).
2.21. Analysis.
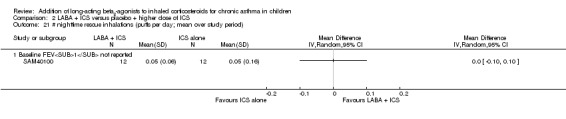
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 21 # nighttime rescue inhalations (puffs per day; mean over study period).
2.22. Analysis.
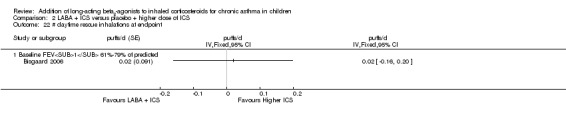
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 22 # daytime rescue inhalations at endpoint.
2.23. Analysis.
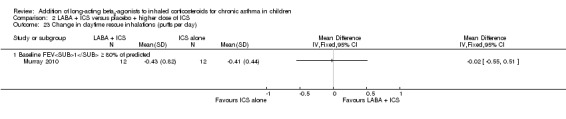
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 23 Change in daytime rescue inhalations (puffs per day).
2.24. Analysis.
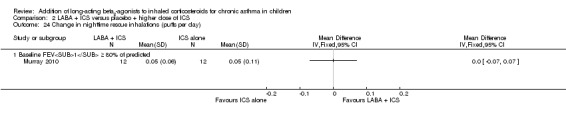
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 24 Change in nighttime rescue inhalations (puffs per day).
2.25. Analysis.
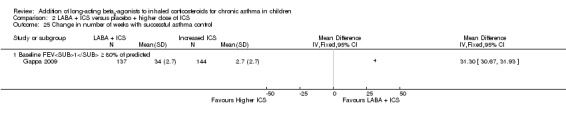
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 25 Change in number of weeks with successful asthma control.
2.26. Analysis.
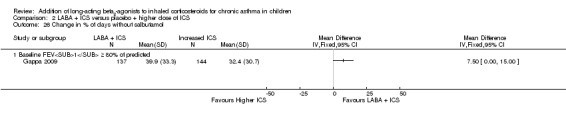
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 26 Change in % of days without salbutamol.
2.27. Analysis.
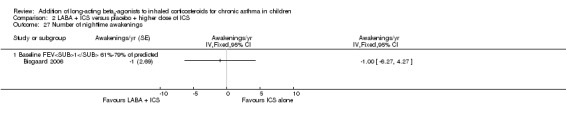
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 27 Number of nighttime awakenings.
2.31. Analysis.
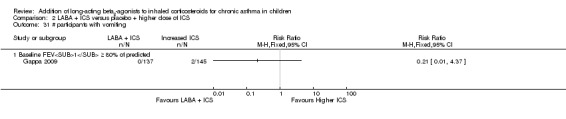
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 31 # participants with vomiting.
2.32. Analysis.
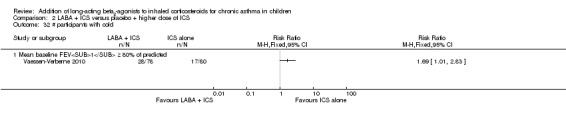
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 32 # participants with cold.
2.33. Analysis.
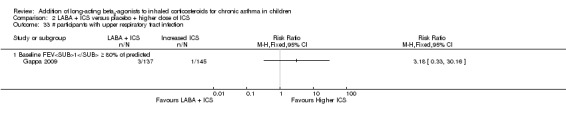
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 33 # participants with upper respiratory tract infection.
2.35. Analysis.
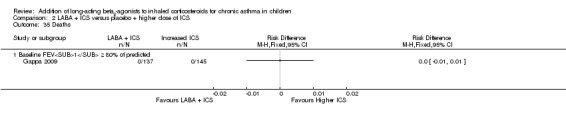
Comparison 2 LABA + ICS versus placebo + higher dose of ICS, Outcome 35 Deaths.
Comparison 3. Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # participants with exacerbations requiring oral steroids by dose of ICS in both groups | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 1.1 Low dose of ICS (≤ 400 μg/d of BDP‐eq) | 8 | 1376 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.67, 1.37] |
| 1.2 Moderate dose of ICS (401 to 800 μg/d of BDP‐eq) | 3 | 270 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.48, 1.64] |
| 1.3 High dose of ICS (> 800 μg/d of BDP‐eq) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Unspecified dose of ICS or range of dose only mentioned | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.28, 4.32] |
| 2 # participants with exacerbations requiring oral steroids by whether LABA dose is usual or higher than usual | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 2.1 LABA at usual dose | 11 | 1646 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.69, 1.28] |
| 2.2 LABA at higher than usual dose | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.28, 4.32] |
| 3 # participants with exacerbations requiring oral steroids by type of LABA | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 3.1 Formoterol | 4 | 591 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.58, 1.39] |
| 3.2 Salmeterol | 8 | 1078 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.66, 1.51] |
| 4 # participants with exacerbations requiring oral steroids by single inhaler or separate inhalers for LABA and ICS | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 4.1 Single inhaler | 6 | 1227 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.66, 1.47] |
| 4.2 Separate inhaler | 6 | 442 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.57, 1.42] |
| 5 # participants with exacerbations requiring oral steroids by trial duration | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 5.1 ≤ 16 weeks | 10 | 1526 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.65, 1.25] |
| 5.2 ≥ 24 weeks | 2 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.59, 2.52] |
| 6 # participants with exacerbations requiring oral steroids by whether funded by producers of LABA | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 6.1 Charity/grant agency funded | 2 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.60, 5.56] |
| 6.2 Funded by manufacturers of LABA | 9 | 1580 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.66, 1.23] |
| 6.3 Unknown funding source | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 # participants with exacerbations requiring systemic steroids by publication status | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 7.1 Published as full‐text papers | 10 | 1439 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.69, 1.37] |
| 7.2 Not published as full‐text papers | 2 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.48, 1.64] |
| 8 # participants with exacerbations requiring systemic steroids by blinding of study | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 8.1 Double‐blinded studies | 12 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.70, 1.28] |
| 8.2 Open‐label studies | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.8. Analysis.
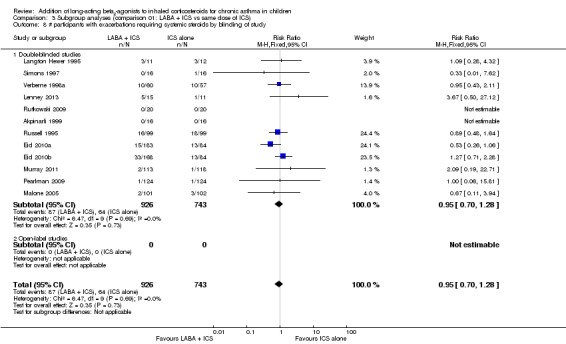
Comparison 3 Subgroup analyses (comparison 01: LABA + ICS vs same dose of ICS), Outcome 8 # participants with exacerbations requiring systemic steroids by blinding of study.
Comparison 4. Subgroup analyses (comparison 02: LABA + ICS vs higher dose of ICS).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # participants with exacerbations requiring oral steroids by dose of ICS in control groups | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 1.1 Low dose of ICS (≤ 400 μg/d of BDP‐eq) | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 1.2 Moderate dose of ICS (401 to 800 μg/d of BDP‐eq) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 High dose of ICS (> 800 μg/d of BDP‐eq) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Unspecified dose of ICS or range of dose only mentioned | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 # participants with exacerbations requiring oral steroids by whether LABA dose is usual or higher than usual | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 2.1 LABA at usual dose | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 2.2 LABA at higher than usual dose | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 # participants with exacerbations requiring oral steroids by type of LABA | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 3.1 Formoterol | 2 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.72, 5.82] |
| 3.2 Salmeterol | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.58, 3.50] |
| 4 # participants with exacerbations requiring oral steroids by single inhaler or separate inhalers for LABA and ICS | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 4.1 Combination inhaler | 2 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.72, 5.82] |
| 4.2 Separate inhaler | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.58, 3.50] |
| 4.3 Not reported | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 # participants with exacerbations requiring oral steroids by trial duration | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.85, 3.32] |
| 5.1 ≤ 16 weeks | 1 | 303 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.19, 22.26] |
| 5.2 ≥ 24 weeks | 2 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.65 [0.81, 3.36] |
Comparison 5. Sensitivity analysis: LABA + ICS versus placebo + higher dose of ICS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # participants with exacerbations requiring oral steroids | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Baseline FEV1 ≥ 80% of predicted | 4 | 895 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.64, 1.33] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akpinarli 1999.
| Methods | Parallel‐group multi‐centre study | |
| Participants | Symptomatic asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 32 (ICS + F12 (twice daily): 16; ICS: 16) WITHDRAWALS: not described AGE, mean (range) or mean (SD): 6 to 14 years GENDER (% male): 47 SEVERITY: not reported BASELINE % PRED FEV1: not described BASELINE DOSE OF ICS: 400 to 800 μg ASTHMA DURATION: not described ATOPY (%): 68 ELIGIBILITY CRITERIA: met ATS criteria for asthma; ≥ 15% increase in FEV1 within previous year EXCLUSION CRITERIA: asthma exacerbation or respiratory infection within last month ELIGIBILITY CRITERIA DURING RUN‐IN: Only participants requiring salbutamol more than once a week were randomly assigned |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES reported at 6 weeks RUN‐IN PERIOD: 2 weeks with ICS 400 to 800 μg/d to document symptoms and beta2‐use DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 6 weeks TEST GROUP: (ICS + F12) ICS 400 to 800 μg/d + F 12 μg twice daily CONTROL GROUP: (ICS) ICS (400 to 800 μg/d) + placebo twice daily DEVICE: MDI + large volume spacer (Volumatic) NUMBER OF DEVICES: 2 COMPLIANCE: assessed by weighing canisters CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; am PEF; pm PEF; PEF variability (%); PC 20 SYMPTOM SCORES: score of 0 to 3 (max 9); nighttime symptom score; symptom‐free days or nights FUNCTIONAL STATUS: rescue medication use; exacerbations requiring systemic steroids; exacerbations requiring admission INFLAMMATORY MARKERS: not described ADVERSE EFFECTS: described WITHDRAWALS: not described PRIMARY OUTCOME MEASURE; not reported |
|
| Notes | Full‐text publication Funded by AstraZeneca Study author contacted and unable to confirm methods or data User‐defined number: 600 (mean ICS dose in LAB2 group in μg/d of BDP‐equivalent: 400 to 800) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical placebo used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information available on statistical handling of missing data |
| Selective reporting (reporting bias) | Low risk | Data on OCS‐treated exacerbations available |
| Other bias | Unclear risk | No data provided on % participants meeting eligibility criteria from screening nor on run‐in populations |
Berger 2010.
| Methods | Randomised open‐label tolerability study (SD‐039‐0719) | |
| Participants | Inadequately controlled on other asthma controller medication % ELIGIBLE OF SCREENED POPULATION: 74 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 187 (ICS + F (twice daily): 124; ICS: 63) WITHDRAWALS: ICS + F: 13 ICS: 10 AGE, mean (SD): 9 (1.6) years GENDER (% male): 64 SEVERITY: not reported BASELINE % PRED FEV1: 83.5 BASELINE DOSE OF ICS, mean (SD) μg/d: ICS + F: 306 (214.1) ICS: 309 (212.6) ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA
EXCLUSION CRITERIA
ELIGIBILITY CRITERIA DURING RUN‐IN
on other asthma controller medication |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES reported at 12 weeks RUN‐IN PERIOD: 1 week with existing ICS to document inadequate asthma control DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 12 weeks TEST GROUP: BUD 320 μg/d + F 9 μg twice daily CONTROL GROUP: budesonide 400 μg/d DEVICE: single device
COMPLIANCE: not reported. CO‐TREATMENT: Albuterol pMDI was permitted as rescue medication throughout the study but was to be withheld for 6 hours before scheduled spirometry. If the participant experienced uncontrolled asthma or increased symptoms after 2 weeks of randomly assigned treatment, leukotriene receptor antagonists, inhaled non‐steroidal anti‐inflammatory agents, methylxanthines and alternative SABA were permitted as needed. OCS bursts were allowed for treatment of asthma exacerbations |
|
| Outcomes | PULMONARY FUNCTION TEST: morning predose forced vital capacity (FVC [L]), FEV1 (L) and forced expiratory flow expired during middle half of exhalation (FEF25–75% [L/s]) SYMPTOM SCORES: FUNCTIONAL STATUS: physician and caregiver global assessments, Quality of Life Questionnaire (PAQLQ[S]) and caregiver quality of life INFLAMMATORY MARKERS: not described ADVERSE EFFECTS: adverse effects, clinical laboratory data (including serum glucose, serum potassium and 24‐hour urinary cortisol), vital signs, 12‐lead ECGs and physical examinations WITHDRAWALS: described Blood chemistry, haematology tests and urinary free cortisol were evaluated Validated standardised paediatric asthma PRIMARY OUTCOME MEASURE: Safety evaluation was the primary aim of the study. However, specific primary outcome was not specified |
|
| Notes | Full‐text publication Funded by AstraZeneca Dose of ICS: Intervention: 800 μg/d of BDP‐equivalent; control: 800 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated allocation schedule was used |
| Allocation concealment (selection bias) | Low risk | Interactive voice response system was used to assign randomisation numbers and treatment assignments to eligible participants to avoid selection bias |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawal rate is imbalance. Reasons for withdrawals were reported |
| Selective reporting (reporting bias) | Unclear risk | Primary or secondary outcomes were not distinguished. Not clear |
| Other bias | Unclear risk | Inadequate information was reported |
Bisgaard 2006.
| Methods | Parallel‐group multi‐centre study | |
| Participants | Steroid‐using asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 223 (Bud/F: 117; Bud: 106) WITHDRAWALS: not reported AGE, mean (range): 8 (4 to 11) years GENDER (% male): 68 ASTHMA SEVERITY: moderate BASELINE % PRED FEV1 mean: 76 BASELINE DOSE OF ICS (start of run‐in): 200 to 500 μg/d ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: ICS 200 to 500 μg BDP‐equivalent (≥ 3 months before run‐in); FEV1 60% to 100% of predicted normal; ≥ 1 severe exacerbation ≤ 12 months before run‐in EXCLUSION CRITERIA: not reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: 8 puffs over last 10 days of run‐in |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: reported at 12 months RUN‐IN PERIOD: 2 weeks to document stability DOSE OF ICS DURING RUN‐IN: not clear DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 12 months TEST GROUP: combination F 4.5/BUD 80 μg qd CONTROL GROUP: BUD 320 μg qd DEVICE: Turbuhaler NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: recorded but not reported SYMPTOM SCORES: recorded but not reported FUNCTIONAL STATUS: night awakenings; rescue medication use; exacerbations* (hospitalisation/need for OCS or other medication, increase in ICS, PEF ≤ 70% baseline on 2 consecutive days) INFLAMMATORY MARKERS: not reported ADVERSE EFFFECTS: reported WITHDRAWALS: not reported *Primary outcome |
|
| Notes | Full‐text article Additional data downloaded from AZ website (www.astrazenecaclinicaltrials.com) Funded by AstraZeneca User‐defined number: 320 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation scheme |
| Allocation concealment (selection bias) | Unclear risk | Eligible patients were randomised in balanced blocks by allocating patient numbers in consecutive order |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical inhaler devices used. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 'All analyses were performed on an intention‐to‐treat basis.' Additional information on the composition of the ITT population was not provided. |
| Selective reporting (reporting bias) | Low risk | Data on OCS‐treated exacerbations reported as composite with ED visits/hospitalisations, PEF falls and requirement for medical intervention. Request for separate data on OCS‐treated exacerbations from study sponsors has not been successful |
| Other bias | Unclear risk | No data provided on % participants meeting eligibility criteria from screening or run‐in populations |
Carroll 2010.
| Methods | Randomised double‐blind placebo‐controlled | |
| Participants | Children with persistent asthma symptoms despite treatment with low‐dose ICS % ELIGIBLE OF SCREENED POPULATION: 84 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 93 RANDOMLY ASSIGNED: 39 Fluticasone/salmeterol: not reported. Fluticasone: not reported. WITHDRAWALS: 2
AGE, mean (range): 10.6 (7 to 18) years GENDER (% male): 59 ASTHMA SEVERITY: not reported BASELINE % PRED FEV1 mean: 95.8% BASELINE DOSE OF ICS (start of run‐in): 400 μg/d of BDP, BUD or 200 μg/d of fluticasone propionate ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: not adequately reported |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 4 and 8 weeks RUN‐IN PERIOD: 4 weeks DOSE OF ICS DURING RUN‐IN: FP 100 μg twice daily DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 8 weeks TEST GROUP: combination fluticasone and salmeterol 100/50 twice daily CONTROL GROUP: fluticasone 100 μg twice daily DEVICE: Diskus inhaler NUMBER OF DEVICES: 1 COMPLIANCE: estimated at each visit by reading the number of doses left in each inhaler device CO‐TREATMENT: not reported |
|
| Outcomes | PULMONARY FUNCTION TEST: changes in mean basal FEV1 (% predicted), fall in mean basal FEV1 (% predicted) due to cold air*, salbutamol reversibility SYMPTOM SCORES: reported FUNCTIONAL STATUS: not reported INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full‐text article Funded by GlaxoSmithKline Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 400 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trail was randomised but no information was provided on how the randomisation was generated. |
| Allocation concealment (selection bias) | Low risk | Devices were masked to make them identical in external physical appearance. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Dobule‐blind study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12% withdrawal from control vs no withdrawal in the treatment group. Reasons for withdrawals were mentioned. |
| Selective reporting (reporting bias) | Low risk | Study protocol was not available. All outcomes were presented. |
| Other bias | Low risk | No apparent source of bias was noted. |
De Blic 2009.
| Methods | Randomised double‐blind double‐dummy parallel‐group non‐inferiority study (SAM104926) | |
| Participants | Not controlled asthmatic children % ELIGIBLE OF SCREENED POPULATION: 55 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 321 Fluticasone/salmeterol: 160 Fluticasone: 161 WITHDRAWALS:
AGE, mean (range): 8.1 (4 to 11) years GENDER (% male): 65 ASTHMA SEVERITY: not reported BASELINE % PRED FEV1 mean: not reported BASELINE DOSE OF ICS (start of run‐in): BDP 400 μg/d or equivalent ASTHMA DURATION: not reported ATOPY (%): 88 ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: Asthma had been assessed as 'Not controlled' for ≥ 2 of the 4 weeks of the run‐in period |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: reported at 12 months RUN‐IN PERIOD: 4 weeks to document asthma control DOSE OF ICS DURING RUN‐IN: FP 100 μg twice daily DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 12 weeks TEST GROUP: combination fluticasone and salmeterol 100/50 twice daily CONTROL GROUP: fluticasone 200 μg twice daily DEVICE: Diskus inhaler NUMBER OF DEVICES: 1 COMPLIANCE: checked by counting the number of remaining doses in the Diskus inhalers CO‐TREATMENT: not reported |
|
| Outcomes | PULMONARY FUNCTION TEST: clinic morning PEF, home morning and evening, before taking any study medication, FEV1, MEF50, reversibility in PEF/FEV1 SYMPTOM SCORES: symptoms, exacerbations* (deterioration in asthma requiring administration of OCS and/or deterioration in asthma requiring emergency room visit and/or admission to hospital); exacerbation requiring OCS FUNCTIONAL STATUS: number of night‐time awakenings, amount of rescue use, asthma control INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full‐text article Funded by GlaxoSmithKline Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 800 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was generated by centralised RANDALL system |
| Allocation concealment (selection bias) | Low risk | All study inhalers were identical in appearance, and use of dummy inhalers ensured that both participants and site personnel remained blinded to an individual's treatment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Well‐balanced withdrawal in both groups; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol is available, and primary and secondary outcomes are predefined |
| Other bias | Low risk | No apparent source of bias was noted |
Eid 2010a.
| Methods | Parallel‐group multi‐centre study | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 35 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 79 RANDOMLY ASSIGNED: 521 (BUD/F twice daily: 184; BUD/F QD: 168; BUD: 169) WITHDRAWALS: BUD/F twice daily: 21; BUD/F QD: 37; BUD: 33 AGE, mean (range) or mean (SD): 10.3 (2.5) years SEVERITY: not stated BASELINE % PRED FEV1: 78.3 (8.56) BASELINE DOSE OF ICS: 245.3 ASTHMA DURATION: 6.8 ATOPY (%): not reported ELIGIBILITY CRITERIA: 6 to 15 years; diagnosis of asthma for ≥ 6 months; maintenance ICS treatment for ≥ 4 weeks before screening; FEV1 predicted 60%‐90% predicted; reversibility of FEV1 ≥ 12% and > 0.20 L from baseline; children > 11 years were required to demonstrate reversibility > 12% only EXCLUSION CRITERIA: not stated ELIGIBILITY CRITERIA DURING RUN‐IN: stable asthma symptoms |
|
| Interventions | LABA and ICS vs SAME DOSE ICS OUTCOMES: 12 weeks RUN‐IN PERIOD: 4 to 5 weeks DOSE OPTIMISATION PERIOD: not reported INTERVENTION PERIOD: 12 weeks TEST GROUP: combination BUD and F 80/9 μg twice daily via MDI CONTROL GROUP: BUD 160 μg QD via MDI NUMBER OF DEVICES: 1 COMPLIANCE: not assessed CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF* SYMPTOM SCORES: day and nocturnal symptoms FUNCTIONAL STATUS: AQLQ INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported by treatment group |
|
| Notes | Full‐text article Funding source: AZ Confirmation of methods and data obtained from AZ in April 2008 Unpublished data downloaded from http://www.astrazenecaclinicaltrials.com Dose of ICS: intervention: 200 μg/d of BDP‐equivalent; control: 200 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented. Age‐based strata to ensure balance in ages between groups (6‐11 years & 12‐15 years) |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Efficacy analysis does not explicitly describe whether missing data imputed or drawn from follow‐up: 'all randomised subjects who took at least 1 dose of double‐blind treatment, and who contributed at least 1 evening PEF diary entry after receiving double‐blind medication, was used in the primary analysis.' |
| Selective reporting (reporting bias) | High risk | OCS‐treated exacerbations were not reported in the study publication. Data request has been made to study sponsors for this information. |
| Other bias | Low risk | 37% screening population eligible for randomisation |
Eid 2010b.
| Methods | See Eid 2010b | |
| Participants | See Eid 2010b | |
| Interventions | See Eid 2010b TEST GROUP:
|
|
| Outcomes | See Eid 2010b | |
| Notes | See Eid 2010b | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information not available |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Efficacy analysis does not explicitly describe whether missing data imputed or drawn from follow‐up: 'all randomised subjects who took at least 1 dose of double‐blind treatment, and who contributed at least 1 evening PEF diary entry after receiving double‐blind medication, were used in the primary analysis' |
| Selective reporting (reporting bias) | High risk | OCS‐treated exacerbations were not reported in the study publication. Data request has been made to study sponsors for this information. |
| Other bias | Low risk | 37% screening population eligible for randomisation |
Gappa 2009.
| Methods | Multi‐center prospective randomised double‐blind double‐dummy parallel‐group study | |
| Participants | Children with uncontrolled asthma % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 64.2 RANDOMLY ASSIGNED: 283
WITHDRAWALS: 8
MEAN AGE, mean age (range): 9.5 (4 to 16) years GENDER (% male): 81 SEVERITY: not reported. BASELINE FEV1 % predicted: 91.6 BASELINE DOSE OF ICS: mean: (200 to 400 μg/d BDP‐equivalent) ASTHMA DURATION (range in years): not reported. ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA: Participants were excluded if they had experienced 1 of the following events during the 4 weeks preceding the study: pneumonia, bronchitis, respiratory infection requiring antibiotic treatment or an asthma‐related hospitalisation. Asthma medications during the 4 weeks before visit 1, which precluded the child from being admitted to the trial, were oral or parenteral corticosteroids, and included oral or inhaled LABA |
|
| Interventions | LABA + ICS vs increased dose of ICS OUTCOMES: reported weekly RUN‐IN: none DOSE OF ICS DURING RUN‐IN: N/A INTERVENTION PERIOD: 12 weeks TEST GROUP: F 12 μg twice daily + BUD 100 twice daily CONTROL GROUP: placebo + ICS BUD 200 twice daily DEVICE: Diskus inhalers NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: Participants were not allowed to take any other drugs for the long‐term treatment of asthma. Medications for concomitant illnesses could be continued during the study, if the dose was kept constant and the drug had no influence on asthma |
|
| Outcomes | PULMONARY FUNCTION TEST: FVC, FEV1 and morning and evening PEF SYMPTOM SCORE: asthma Symptom Score (ASS) on a scale of 0 to 4 FUNCTIONAL STATUS: number of days (24 hours) without asthma symptoms, use of salbutamol as rescue medication, number of weeks with successful asthma control INFLAMMATORY MARKERS: ADVERSE EFFECTS: reported WITHDRAWALS: reported PRIMARY OUTCOME MEASURE: change in mean morning expiratory PEF (L/min) |
|
| Notes | Full‐text publication Source of funding: GlaxoSmithKline Confirmation of methods and data not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 800 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated code produced in the centralised facility |
| Allocation concealment (selection bias) | Unclear risk | Inadequate details were reported on allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Well‐balanced withdrawals in groups compared; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol is available. Primary and secondary outcomes were prespecified |
| Other bias | Low risk | No apparent source of bias was noted |
Heuck 2000.
| Methods | Cross‐over study; single centre (outpatient referral centre) | |
| Participants | Asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 27 WITHDRAWALS: 2 participants were withdrawn during treatment with BUD alone; 1 withdrawal ‐ unclear which period AGE, mean (range): 9.6 (6.1 to 13.5) years GENDER (% male): 52 SEVERITY: mild to moderate BASELINE FEV1: not reported BASELINE PEF L/min: 280 L/min BASELINE DOSE OF ICS: mean ‐ BUD 200 twice daily or equivalent ASTHMA DURATION (range in years): 4.5 (1.4 to 9.5) ATOPY (%): not reported ELIGIBILITY CRITERIA: treatment with inhaled BUD 200 μg twice daily (or equipotent doses of other ICS) for 1 month before study entry; children were prepubertal EXCLUSION CRITERIA: not described |
|
| Interventions | LABA + ICS vs INCREASED DOSE ICS OUTCOMES: reported weekly RUN‐IN: none DOSE OF ICS DURING RUN‐IN: N/A INTERVENTION PERIOD: 12 weeks TEST GROUP: F 12 μg twice daily + BUD 100 μg twice daily CONTROL GROUP: placebo + ICS BUD 200 μg twice daily DEVICE: Turbuhaler (ICS) and Aerolizer (F) NUMBER OF DEVICES: 2 COMPLIANCE: Turbuhalers weighed and number of F capsules counted CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOM SCORE: daytime and nighttime score (score of 0 to 4) FUNCTIONAL STATUS: exacerbations; rescue medication use; lower leg growth; serum and urinary markers of type I and III collagen turnover INFLAMMATORY MARKERS: inflammatory markers in serum ADVERSE EFFECTS: reported WITHDRAWALS: reported PRIMARY OUTCOME MEASURES: not reported |
|
| Notes | Full‐text publication Source of funding not stated Confirmation of methods and data not obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Treatment order was allocated by a computerised randomisation scheme prepared in balanced blocks' |
| Allocation concealment (selection bias) | Unclear risk | Information on concealment of allocation not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information available |
| Selective reporting (reporting bias) | Low risk | Data on OCS‐treated exacerbations available |
| Other bias | Unclear risk | No data provided on % participants meeting eligibility criteria from screening or run‐in populations |
Langton Hewer 1995.
| Methods | Parallel‐group single‐centre double‐blind placebo‐controlled study | |
| Participants | Symptomatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported NUMBER RECRUITED NOT RANDOMLY ASSIGNED: not stated RANDOMLY ASSIGNED: 23 (usual ICS + salmeterol 100 twice daily: 11; usual ICS: 12) WITHDRAWALS: usual ICS + salmeterol: 0; usual ICS: 2 AGE, median (range): 15 (12 to 17) years GENDER (% male): 70 SEVERITY: severe BASELINE % PRED FEV1: 82 BASELINE DOSE OF ICS (start of run‐in): 400 ASTHMA DURATION: 13 years ATOPY (%): 100 ELIGIBILITY CRITERIA: severe asthma (not defined but severe enough to be attending residential school for asthma and persistent symptoms) EXCLUSION CRITERIA: already taking LABA CRITERIA FOR RANDOMISATION DURING RUN‐IN: none specified |
|
| Interventions | LABA + ICS vs SAME DOSE (usual dose) of ICS OUTCOMES reported at 8 and 10 weeks RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: same as during study DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 8 weeks TEST GROUP: (usual ICS + salmeterol): salmeterol 100 μg twice daily CONTROL GROUP: usual ICS and placebo twice daily DEVICE: Diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: supervised in school taking medication by investigators CO‐TREATMENT OCS: methylxanthines and anticholinergics taken by 20% of participants |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOM SCORES: morning and evening symptom scores FUNCTIONAL STATUS: SABA; symptom‐free days/nights; exacerbation (requiring systemic steroids); quality of life score INFLAMMATORY MARKERS: none ADVERSE EFFECTS: described WITHDRAWALS: described PRIMARY OUTCOME MEASURES: not reported |
|
| Notes | Full‐text publication Funded by Charity Confirmation of methods and data pending User‐defined number: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Identical placebo |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data analysis described as intention to treat; methods applied not elaborated |
| Selective reporting (reporting bias) | Low risk | Data on OCS‐treated exacerbations available |
| Other bias | Unclear risk | No data provided on % participants meeting eligibility criteria from screening or run‐in populations (niche population sampled for residential school for children with particularly difficult to treat asthma) |
Lemanske 2010.
| Methods | Randomised double‐blind 3‐treatment 3‐period cross‐over trial | |
| Participants | Symptomatic asthmatic children despite low‐dose ICS therapy % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 38 RANDOMLY ASSIGNED: 182 WITHDRAWALS: 25 AGE, median ± SD years: 2 age strata 6 to 11 years (N = 126): 9.1 ± 1.5 12 to 17 years (N = 56): 14.7 ± 1.7 GENDER (% male): 65 SEVERITY: mild to moderate BASELINE % PRED FEV1: 97 BASELINE DOSE OF ICS (start of run‐in): 100 μg of fluticasone twice daily ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: children 6 to 17 years of age with mild to moderate asthma diagnosed by a physician on the basis of criteria recommended by the National Asthma Education and Prevention Program; ability to perform reproducible spirometry; FEV1 ≥ 60% before bronchodilation; increase in FEV1 ≥ 12% (bronchodilator reversibility) or methacholine PC20 in FEV1 ≤ 12.5 mg/mL EXCLUSION CRITERIA: not reported. CRITERIA FOR RANDOMISATION DURING RUN‐IN: after use of 100 μg of fluticasone twice daily during run‐in period, documentation of uncontrolled asthma, which was defined as occurrence of ≥ 1 of the following more than 2 days per week on average during a 2‐week period: diary‐reported symptoms (coughing rated as moderate or severe, or wheezing rated as mild, moderate or severe); rescue use of an inhaled bronchodilator with ≥ 2 puffs per day; or PEF < 80% of predetermined reference value |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: reported at 16 weeks RUN‐IN PERIOD: 2 to 8 weeks DOSE OF ICS DURING RUN‐IN: 100 μg of fluticasone twice daily INTERVENTION PERIOD: 16‐weeks TEST GROUP: 100 μg of fluticasone + 50 μg of long‐acting beta‐agonist salmeterol (Advair Diskus, GlaxoSmithKline) twice daily CONTROL GROUP: 250 μg of fluticasone (Flovent Diskus, GlaxoSmithKline) twice daily DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: recorded CO‐TREATMENT: Participants received open‐label metered‐dose inhaler of albuterol (Ventolin HFA, GlaxoSmithKline). Standardised course of prednisone treatment was initiated for an asthma exacerbation if predetermined clinical criteria were met |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1, PC20 SYMPTOM SCORES: symptom scores; symptom‐free days FUNCTIONAL STATUS: An asthma‐control day, as documented in each participant's diary, was a day with no use of albuterol rescue (excluding use of albuterol as pre‐exercise treatment), no use of a non‐study asthma medication, no daytime or nighttime asthma symptoms, no unscheduled visit to a healthcare provider for asthma and no PEF < 80% of predetermined reference value EXACERBATION: OCS‐treated exacerbations; hospitalisations. INFLAMMATORY MARKERS: FeNO ADVERSE EFFECTS: reported WITHDRAWALS: stated PRIMARY OUTCOME MEASURES: differential response to each of the 3 step‐up therapies on the basis of fixed threshold criteria for the following 3 asthma‐control measures: need for treatment with oral prednisone for acute asthma exacerbations, number of asthma‐control days and FEV1 |
|
| Notes | Full‐text publication Funded by grant agencies but not by pharmaceutical companies Confirmation of data and methods not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 1000 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 3 × 3 cross‐over design based on complete set of orthogonal Latin squares; stratification based on clinical sites |
| Allocation concealment (selection bias) | Low risk | Drug assignments were masked with use of placebo tablets and dummy disk devices that discharged powder without active drug |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Triple‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few withdrawals; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol is available; primary and secondary outcomes were prespecified |
| Other bias | Low risk | No apparent source of bias was noted |
Lenney 2013.
| Methods | Randomised double‐blind placebo‐controlled trial | |
| Participants | Children with uncontrolled asthma % ELIGIBLE OF SCREENED POPULATION: 7 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 42
WITHDRAWALS: 9
AGE, mean (range): 10.5 (6 to 14) years GENDER (male%): 73 ASTHMA SEVERITY: not reported BASELINE % PRED FEV1 mean: 88.5 BASELINE DOSE OF ICS (start of run‐in): not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: The following eligibility criteria were considered before randomisation INCLUSION CRITERIA:
EXCLUSION CRITERIA:
|
|
| Interventions | LABA + ICS vs same dose of ICS OUTCOMES: reported at 48 weeks RUN‐IN PERIOD: 4 weeks DOSE OF ICS DURING RUN‐IN: usual maintenance dose INTERVENTION PERIOD: 48 weeks TEST GROUP: combination fluticasone propionate 100 μg and salmeterol 50 μg twice daily CONTROL GROUP: fluticasone propionate 100 μg twice daily DEVICE: Accuhaler NUMBER OF DEVICES: 1 COMPLIANCE: reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1, FVC SYMPTOM SCORES: not reported FUNCTIONAL STATUS: quality of life of children as measured by the Paediatric Asthma Quality of Life Questionnaire, quality of life of caregivers as measured by the Paediatric Asthma Caregiver’s Quality of Life Questionnaire, number of schooldays missed because of respiratory problems, amount of rescue SABA therapy prescribed for asthma symptoms, time from randomisation to treatment withdrawal (because of lack of efficacy or side effects) EXACERBATIONS: number of asthma exacerbations requiring treatment with OCS*; time from randomisation to first exacerbation requiring treatment with a short course of OCS; number of hospital admissions due to respiratory problems INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: stated *Primary outcome |
|
| Notes | Full‐text publication Funded by the Health Technology Assessment programme (HTA) of the Department of Health Confirmation of data and methods not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 400 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation with variable block length, stratified by secondary care centre, with allocation to 3 treatment arms in the ratio of 1 : 1 : 1 |
| Allocation concealment (selection bias) | Low risk | Study drugs were identical in appearance and were identically packaged, with all participants, clinicians and trial personnel blinded to treatment allocation throughout |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for withdrawals reported |
| Selective reporting (reporting bias) | Low risk | Full protocol is available. Primary and secondary outcomes were prespecified. |
| Other bias | Low risk | Study was prematurely terminated due to lack of funds. However, no apparent source of bias was noticed. |
Malone 2005.
| Methods | Parallel‐group multi‐centre (66 centres in North America) | |
| Participants | Steroid‐using asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 48 RANDOMLY ASSIGNED: 203 (fluticasone/salmeterol: 101; fluticasone: 102) WITHDRAWALS: fluticasone/salmeterol: 19; fluticasone: 16 AGE, mean: 8 years GENDER (male %): 64 ASTHMA SEVERITY: mild to moderate BASELINE % PRED FEV1 mean: 80% BASELINE DOSE OF ICS (start of run‐in): 166 μg fluticasone ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: 4 to 11 years of age; ATS defined asthma ≥ 2 months; ICS therapy (BDP‐equivalent 252 to 336 μg/d) for 1 month before entry; participants 6 to 11 years of age required to have FEV1% predicted; participants 4 to 5 years of age required to have am PEF 50% to 95% of predicted; ≥ 12% response to beta2‐agonist at screening visit or within 1 year of screening visit EXCLUSION CRITERIA: history of life‐threatening asthma; hospitalisation with asthma twice or more in previous year; significant concurrent disease; oral or parenteral use of steroids during month before study entry CRITERIA FOR RANDOMISATION DURING RUN‐IN: am FEV1 50% to 95% of predicted; daytime asthma (score ≥ 1); use of SABA on 3+ days of last 7 days of run‐in; ≥ 70% diary card entry |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 3 months RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: usual maintenance dose INTERVENTION PERIOD: 3 months TEST GROUP: combination salmeterol 50/fluticasone 100 μg twice daily CONTROL GROUP: fluticasone 100 μg twice daily DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; clinic PEF; am PEF; pm PEF SYMPTOM SCORES: symptom scores; symptom‐free days FUNCTIONAL STATUS: OCS‐treated exacerbations; hospitalisations; use of reliever medication; SABA‐free days INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: stated *Primary outcome: not identified (safety study) |
|
| Notes | Full‐text publication Funded by GSK User‐defined number: 400 Confirmation of data and methods obtained |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Appendix 4 |
| Allocation concealment (selection bias) | Low risk | See Appendix 4 |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical inhaler devices |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 'For patients who withdrew from the study prematurely, all available data up to the time of discontinuation were included in the intent‐to‐treat population' |
| Selective reporting (reporting bias) | Low risk | Full protocol is available. Primary and secondary outcomes were prespecified. |
| Other bias | Low risk | Study was prematurely terminated due to lack of funds. However, no apparent source of bias was noticed. |
Meijer 1995.
| Methods | Parallel‐group single‐centre study | |
| Participants | Asymptomatic asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 40 (salmeterol 50 μg twice daily + ICS: 20; ICS + placebo: 20) WITHDRAWALS: salmeterol 50 μg twice daily + ICS: 0; ICS + placebo: 1 (5%) AGE, mean (SD): 11.4 (2.6) years GENDER (% male): 58 SEVERITY: mild BASELINE % PRED FEV1: 94 BASELINE DOSE OF ICS: twice‐daily 200 or 400 μg BDP rotadisk ASTHMA DURATION: 8.4 years ATOPY (%): 100 ELIGIBILITY CRITERIA: none reported EXCLUSION CRITERIA: none reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: N/A |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 1, 8, 16 weeks RUN‐IN PERIOD: none DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 16 weeks TEST GROUP: salmeterol 50 μg twice daily + BDP 250 μg twice daily CONTROL GROUP: BDP 250 μg twice daily + placebo DEVICE: dry powder inhaler (Diskhaler) NUMBER OF DEVICES: 2 COMPLIANCE: returned powder disks counted CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; PC20 doubling doses (DD); circadian variation (day‐night differences in FEV1) SYMPTOM SCORES: only individual symptoms reported (yes/no) FUNCTIONAL STATUS: rescue medication use INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: not reported WITHDRAWALS: reported PRIMARY OUTCOME MEASURE: not specified |
|
| Notes | Full‐text publication Funded by Glaxo User‐defined number: 500 Confirmation of data and methods not obtained |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not enough information presented to determine this |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected in the study |
| Other bias | Unclear risk | No data presented on % screening population eligible for randomisation |
Morice 2008a.
| Methods | Parallel‐group multi‐centre study (53 centres in South America, Europe, Hong Kong and Taiwan) | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 77 RANDOMLY ASSIGNED: 622 (BUD: 207; BUD/F (DPI): 203; BUD/F (MDI): 212) WITHDRAWALS: BUD: 14 BUD/F (DPI): 11; BUD/F (MDI): 14 AGE, mean (range): 9 (6 to 11) years GENDER (% male): 66 SEVERITY: not specified BASELINE % PRED FEV1: 89 BASELINE DOSE OF ICS: (start of run‐in): 470 μg ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: age 6 to 11 years; diagnosis of asthma for ≥ 6 months; PEF > 50% of predicted normal; history daily ICS use (stable dose of 375 to 1000 μg 30 days before enrolment); clinically important exercise‐induced bronchoconstriction for 3 months before enrolment; ability to use DPI, pMDI and peak flow meter EXCLUSION CRITERIA: not reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: symptom score 1 to 4; mean morning PEF 50% to 85% post SABA |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: 12 weeks RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: 470 DOSE OPTIMISATION PERIOD: not reported INTERVENTION PERIOD: 12 weeks TEST GROUP: combination BUD and F (160/9 μg) twice daily via dry powder inhaler + placebo metered‐dose inhaler CONTROL GROUP: BUD 200 μg twice daily DEVICE: MDI and DPI NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: day/night scores FUNCTIONAL STATUS: paediatric AQLQ INFLAMMATORY MARKERS: NA ADVERSE EFFECTS: stated WITHDRAWALS: stated *Primary outcome |
|
| Notes | Full‐text publication AZ funded User‐defined number: 200 Confirmation of data and methods not obtained |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated schedule |
| Allocation concealment (selection bias) | Unclear risk | Information not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | '...all randomised patients with post‐randomisation data' |
| Selective reporting (reporting bias) | High risk | Data on OCS‐treated exacerbations were not reported in the trial publication. Study sponsors have indicated that the data from this study are not available |
| Other bias | Low risk | 77% of screening population eligible for randomisation |
Morice 2008b.
| Methods | See Morice 2008a | |
| Participants | See Morice 2008a | |
| Interventions | See Morice 2008a, except for: TEST GROUP:
|
|
| Outcomes | See Morice 2008a | |
| Notes | See Morice 2008a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Morice 2008a |
| Allocation concealment (selection bias) | Unclear risk | See Morice 2008a |
| Blinding (performance bias and detection bias) All outcomes | Low risk | See Morice 2008a |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Morice 2008a |
| Selective reporting (reporting bias) | High risk | See Morice 2008a |
| Other bias | Low risk | See Morice 2008a |
Murray 2010.
| Methods | Two‐centre randomised double‐blind double‐dummy study (SAM40100) | |
| Participants | Children with moderate/severe persistent asthma % ELIGIBLE OF SCREENED POPULATION: 40 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 69 RANDOMLY ASSIGNED: 24
WITHDRAWALS: 2
AGE, mean (SD): 7.3 (2.2) years GENDER (% male): 50 SEVERITY: moderate to severe BASELINE % PRED FEV1 mean (SD): 84.5 ASTHMA DURATION: reported as strata of 1 to 5 years and > 5 years ATOPY (%): not reported ELIGIBILITY CRITERIA: children 4 to 11 years of age, physician‐diagnosed asthma, daily 200 to 800 μg BDP‐equivalent ICS use EXCLUSION CRITERIA: participants with oral, parenteral or nebulized corticosteroids 4 weeks before run‐in; ≥ 3 courses of oral prednisolone in previous year; intensive care admission in previous 3 months; regular use of SABA; use of LTRA; cromoglycates and/or theophyllines; known serious, uncontrolled systemic disease and asthma exacerbation requiring change of asthma medication during run‐in CRITERIA FOR RANDOMISATION DURING RUN‐IN: Randomisation included sRaw ≥ 1.3 kPa.s; correct completion of diary; symptom score ≥ 2 or required use of salbutamol on ≥ 2 occasions per day for ≥ 3 days of previous 7 days of run‐in period |
|
| Interventions | LABA + ICS vs HIGH HIGH dose ICS RUN‐IN PERIOD: 2 weeks OUTCOMES: reported at 6 weeks DOSE OF ICS DURING RUN‐IN: FP 100 μg twice daily DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 6 weeks TEST GROUP: fluticasone 100 μg and salmeterol 50 μg twice daily CONTROL GROUP: fluticasone 200 μg twice daily DEVICE: Accuhaler/Diskus NUMBER OF DEVICES: 1 COMPLIANCE: reported CO‐TREATMENT: albuterol as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: predose sRaw at end of 6 weeks of treatment*, FEV1 SYMPTOM SCORES: symptom score recorded FUNCTIONAL STATUS: salbutamol rescue use, percent of rescue‐free days and nights, percent of symptom‐free days INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full‐text publication Funded by GlaxoSmithKline Confirmation of methods and data not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 800 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on sequence generation reported |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information on allocation concealment reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low and balanced withdrawals. Intention to treat analysis. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes prespecified. All outcomes were reported. |
| Other bias | Low risk | No apparent source of bias was noticed. |
Murray 2011.
| Methods | Stratified multi‐centre randomised double‐blind parallel‐group study (SFA100316) | |
| Participants | Children with persistent asthma treated with daily ICS for ≥ 4 weeks % ELIGIBLE OF SCREENED POPULATION: 33 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 231
WITHDRAWALS: 17
AGE, mean (range): 11.6 (4 to 17) years GENDER (% male): 57 SEVERITY: not reported BASELINE % PRED FEV1 mean (SD): 83.5 ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN:
|
|
| Interventions | LABA + ICS vs SAME dose ICS RUN‐IN PERIOD: 2 to 5 weeks OUTCOMES: reported at 4 weeks DOSE OF ICS DURING RUN‐IN: FP 100 μg twice daily (Flovent DISKUS, GlaxoSmithKline, Research Triangle Park, North Carolina) DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 4 weeks TEST GROUP: fluticasone 100 μg and salmeterol 50 μg twice daily CONTROL GROUP: fluticasone 100 μg twice daily DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: reported CO‐TREATMENT: albuterol as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: maximal percent fall in FEV1 following exercise challenge*, 4‐hour serial post‐dose FEV1 AUC
on Treatment Day 1, morning PEF, evening PEF FUNCTIONAL STATUS: percent of rescue‐free days, percent of symptom free days INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full‐text publication Funded by GlaxoSmithKline Confirmation of methods and data not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 400 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on sequence generation reported. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information on allocation concealment reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low and balanced withdrawals. Intention to treat analysis. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes prespecified. All outcomes were reported. |
| Other bias | Low risk | No apparent source of bias was noticed. |
Ortega‐Cisneros 1998.
| Methods | Parallel‐group single‐centre | |
| Participants | Symptomatic asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICAPNTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 20
WITHDRAWALS: not described AGE (range): 6 to 19 years GENDER (% male): not described SEVERITY: moderate BASELINE % PRED FEV1 mean (SD): not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: still symptomatic despite maintenance treatment with 200 μg twice daily of BDP EXCLUSION CRITERIA: not described |
|
| Interventions | LABA + ICS vs INCREASED dose ICS RUN‐IN PERIOD: 2 weeks OUTCOMES: reported at 8, 12 weeks DOSE OF ICS DURING RUN‐IN: BDP 200 μg twice daily DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 12 weeks TEST GROUP: salmeterol 50 μg twice daily + BDP 200 μg twice daily CONTROL GROUP: BDP 400 μg twice daily DEVICE: not specified NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: not specified |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; PEF; FEF 25% to 75% SYMPTOM SCORES: symptoms FUNCTIONAL STATUS: not reported INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: not reported WITHDRAWALS: not reported |
|
| Notes | Abstract Funding not reported Confirmation of methods and data not obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not provided |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected in the study |
| Other bias | Unclear risk | No information provided |
Pearlman 2009.
| Methods | Multi‐centre stratified randomised double‐blind parallel‐group study (Protocol SFA100314) | |
| Participants | Children with persistent asthma with a minimum decrease in FEV1 of 15% after exercise challenge % ELIGIBLE OF SCREENED POPULATION: 31 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 248
WITHDRAWALS: 35
AGE, mean (range) 11.1 (4 to 17) years GENDER (male %): 60 ASTHMA SEVERITY: not reported BASELINE % PRED FEV1 mean: 83.6 BASELINE DOSE OF ICS (start of run‐in): 237 μg/d ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA:
first visit, approximately 8 hours after taking their prestudy ICS EXCLUSION CRITERIA: POST‐RUN‐IN: Participants were required to have documented use of albuterol and/or asthma symptoms in the 7 days immediately before randomisation. In addition, at the end of the run‐in period, each participant was required to demonstrate a ≥ 20% decrease from baseline in FEV1 following the exercise challenge |
|
| Interventions | LABA + ICS vs SAME dose ICS OUTCOMES: 4 weeks RUN‐IN PERIOD: 1 to 2 weeks DOSE OF ICS DURING RUN‐IN: fluticasone 100 μg twice daily INTERVENTION PERIOD: 4 weeks TEST GROUP: combination fluticasone/salmeterol 100/50 μg twice daily CONTROL GROUP: fluticasone 100 μg twice daily DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: reported CO‐TREATMENT: albuterol as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: maximal % fall in FEV1 following exercise challenge*, 4‐hour serial post‐dose FEV1 AUC on Treatment Day 1, FEV1 (L), am PEF (L/min), pm PEF (L/min) SYMPTOM SCORES: not reported FUNCTIONAL STATUS: % symptom‐free days, % albuterol‐free days INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome: defined |
|
| Notes | Full‐text publication Funded by GlaxoSmithKline Confirmation of methods and data not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 400 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Assignment to blinded study drug was stratified on the basis of age |
| Allocation concealment (selection bias) | Unclear risk | Inadequate information was reported on allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Well‐balanced withdrawals in comparison groups; reasons for withdrawals were reported; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol is available; primary and secondary outcomes were prespecified |
| Other bias | Low risk | No apparent source of bias was noted |
Pohunek 2006a.
| Methods | Parallel‐group multi‐centre study (80 centres in Europe); 3 treatment groups | |
| Participants | Steroid‐using asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 77 RANDOMLY ASSIGNED: 429 (BUD/F: 216; BUD: 213) WITHDRAWALS: BUD/F: 14 BUD: 13 AGE, mean (range): 8 (4 to 11) years GENDER (male %): 67 ASTHMA SEVERITY: mild to moderate BASELINE % PRED FEV1 mean: 92 BASELINE DOSE OF ICS (start of run‐in): 454 μg/d ASTHMA DURATION: 3 ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
POST‐RUN‐IN: total asthma symptom score ≥ 1 on ≥ 4 of last 7 days of run‐in period; during last 7 days of run‐in, participants had to have a mean morning PEF of 50% to 85% of post‐SABA PEF |
|
| Interventions | LABA + ICS vs SAME dose ICS OUTCOMES: 12 weeks RUN‐IN PERIOD: 10 to 14 days DOSE OF ICS DURING RUN‐IN: usual dose of ICS INTERVENTION PERIOD: 12 weeks TEST GROUP: combination BUD/F 200/6 μg twice daily CONTROL GROUP: BUD 200 μg twice daily DEVICE: Turbuhaler NUMBER OF DEVICES: 1 (Symbicort; double‐dummy) COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: not reported FUNCTIONAL STATUS: not reported INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: not reported PRIMARY OUTCOME MEASURE: not reported |
|
| Notes | Full‐text publication Funded by AstraZeneca Confirmation of methods and data not obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schedule generated using a computer programme (AstraZeneca, UK) |
| Allocation concealment (selection bias) | Low risk | Person not involved in the study team generated the randomisation schedule |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 'Intent to treat analysis was performed using data from all randomised patients' No additional data were provided on the composition of the ITT population |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether OCS‐treated exacerbations were collected in the study; correspondence with trialist has failed to clarify this |
| Other bias | Low risk | 78% screening population eligible for randomisation |
Pohunek 2006b.
| Methods | See Pohunek 2006a | |
| Participants | See Pohunek 2006a, except for RANDOMLY ASSIGNED: 414 (F + BUD: 201; BUD: 213) |
|
| Interventions | See Pohunek 2006a, except for TEST GROUP: separate F 6 and BUD 200 μg twice daily NUMBER OF DEVICES: 2 |
|
| Outcomes | See Pohunek 2006a | |
| Notes | See Pohunek 2006a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Pohunek 2006a |
| Allocation concealment (selection bias) | Low risk | See Pohunek 2006a |
| Blinding (performance bias and detection bias) All outcomes | Low risk | See Pohunek 2006a |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Pohunek 2006a |
| Selective reporting (reporting bias) | Unclear risk | See Pohunek 2006a |
| Other bias | Low risk | See Pohunek 2006a |
Russell 1995.
| Methods | Parallel‐group multi‐centre study (78 centres) | |
| Participants | Symptomatic asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 208 (salmeterol 50 + ICS: 99; placebo + ICS: 109) WITHDRAWALS: salmeterol 50 + ICS: 22%; placebo + ICS: 16.8% AGE, mean (SD): 10.2 (2.7) years GENDER (% male): 60 SEVERITY: moderate BASELINE MEAN % PRED FEV1: 78 BASELINE DOSE OF ICS: 750 μg ASTHMA DURATION (%): < 1 year: 3; 1 to 5 years: 20; > 5 years: 77 ATOPY (%): 77 ELIGIBILITY CRITERIA DURING RUN‐IN:
EXCLUSION CRITERIA: received a course of OCS; change in prophylactic therapy during previous 2 weeks |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 4, 8 and 12 weeks RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: continued on usual ICS of ≥ 400 μg/d BDP DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 12 weeks TEST GROUP: (salmeterol 50 + ICS) salmeterol 50 μg twice daily + ICS 400 to 2400 μg/d (average: 750 μg/d) CONTROL GROUP: (placebo + ICS) placebo + ICS 400 to 2400 μg/d (average 750 μg/d) DEVICE: Diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: evaluated using participant‐kept record booklets CO‐TREATMENT: salbutamol as needed and any other prophylactic asthma medication via Diskhaler |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF percent predicted*; pm PEF percent predicted SYMTPOM SCORES: Symptoms were recorded daily as present or absent wheeze or cough during day or night FUNCTIONAL STATUS: proportion symptom‐free days; proportion symptom‐free nights; rescue medication use INFLAMMATORY MARKERS: not described ADVERSE EFFECTS: described WITHDRAWALS: described *Primary outcome |
|
| Notes | Full‐text publication Funded by Allen & Hanburys Confirmation of methods and data obtained User‐defined number: 750 (750 μg/d) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Numbered coded envelopes supplied by pharmacy |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical placebo |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 'Total population used, this comprised all subjects who received at least one puff of medication and recorded at least one day of valid diary or clinic data during the treatment period. Where a subject withdrew before completion of the study, data recorded after this withdrawal data was excluded' |
| Selective reporting (reporting bias) | Low risk | OCS‐treated exacerbation data available |
| Other bias | Unclear risk | Information on % screening population eligible not available |
Rutkowski 2009.
| Methods | Randomised double‐blind placebo‐controlled study | |
| Participants | Children with mild to moderate asthma % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 40
WITHDRAWALS: 0
AGE (range): 10 to 18 years GENDER (male %): 45 ASTHMA SEVERITY: mild to moderate asthma BASELINE % PRED FEV1 mean: not reported BASELINE DOSE OF ICS (start of run‐in): not reported ASTHMA DURATION: 4.8 years ATOPY (%): not reported ELIGIBILITY CRITERIA: children with diagnosed mild to moderate asthma as per GINA 2008, with FEV1 > 60% of predicted values, positive reversibility test to salbutamol and no symptoms of respiratory tract infection EXCLUSION CRITERIA: children with positive skin prick tests with common airborne allergens (house dust mites, trees, grasses, weeds, cat, Alternaria, Cladosporium) ELIGIBILITY CRITERIA DURING RUN‐IN: not reported |
|
| Interventions | ICS and LABA vs SAME dose ICS OUTCOMES: 6 weeks RUN‐IN PERIOD: 1 week DOSE OPTIMISATION PERIOD: NA INTERVENTION PERIOD: 6 weeks TEST GROUP: 400 μg BUD with 12 μg F fumarate twice daily CONTROL GROUP: 400 μg BUD twice daily NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: not reported |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 and FEF25% to 75%, adenosine provocative test SYMPTOM SCORES: dyspnoea severity score FUNCTIONAL STATUS: asthma exacerbation INFLAMMATORY MARKERS: NA ADVERSE EFFECTS: not reported WITHDRAWALS: reported |
|
| Notes | Full‐text publication Funded by: not reported Confirmation of methods and data not obtained Dose of ICS: intervention: 800 μg/d of BDP‐equivalent; control: 800 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Inadequate information on randomisation technique is reported. |
| Allocation concealment (selection bias) | Low risk | Placebo capsules were identical in appearance, coded and inhaled via identical aerosoliser. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data presented. No withdrawals in the study. |
| Selective reporting (reporting bias) | Unclear risk | Primary and secondary outcomes were not clearly defined. Study protocol is not available. |
| Other bias | Low risk | No apparent source of bias was noticed. |
SAM40012a.
| Methods | Parallel‐group multi‐centre study in Europe and Middle East | |
| Participants | Steroid‐using asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 362 (fluticasone/salmeterol: 181; fluticasone: 181) WITHDRAWALS: fluticasone/salmeterol: 3; fluticasone: 10 AGE, mean: 8 years GENDER (male %): 68 ASTHMA SEVERITY: moderate BASELINE % PRED FEV1 mean: not reported BASELINE DOSE OF ICS (start of run‐in): not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: 4 to 500 μg BDP‐equivalent; documented history of asthma EXCLUSION CRITERIA: not reported ELIGIBILITY CRITERIA DURING RUN‐IN: symptom score ≥ 2 on 3 of last 7 days of run‐in |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 6 months RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: not clear DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 6 months TEST GROUP: combination salmeterol 50/fluticasone 100 μg twice daily CONTROL GROUP: fluticasone 100 μg twice daily DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | OUTCOMES: reported at 6 months PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: symptom‐free days FUNCTIONAL STATUS: use of reliever medication; exacerbations (undefined) INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full unpublished data set available from http://www.ctr.gsk.co.uk Source of funding: GSK Confirmation of methods and data not obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Appendix 4 |
| Allocation concealment (selection bias) | Low risk | See Appendix 4 |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Identical inhaler devices |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 'To be evaluable, subjects had to meet the entry and randomisation criteria, receive at least one dose of study medication and have completed at least one day's post‐randomisation diary information.' |
| Selective reporting (reporting bias) | Unclear risk | Exacerbations described in trial report available; OCS‐treated exacerbations could not be identified from the data available |
| Other bias | Unclear risk | Information not available |
SAM40012b.
| Methods | See SAM40012a | |
| Participants | See SAM40012a, except for RANDOMLY ASSIGNED: fluticasone/salmeterol: 181; FP: 186 WITHDRAWALS: fluticasone/salmeterol: 3; FP: 5 |
|
| Interventions | LABA + ICS vs HIGH dose of ICS See SAM40012a |
|
| Outcomes | See SAM40012a | |
| Notes | See SAM40012a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Appendix 4 |
| Allocation concealment (selection bias) | Low risk | See Appendix 4 |
| Blinding (performance bias and detection bias) All outcomes | Low risk | See SAM40012a |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See SAM40012a |
| Selective reporting (reporting bias) | Unclear risk | See SAM40012a |
| Other bias | Unclear risk | See SAM40012a |
SAM40100.
| Methods | Parallel‐group multi‐centre study | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 24 (fluticasone/salmeterol: 12; FP: 12) WITHDRAWALS: fluticasone/salmeterol: 1; FP: 1 AGE, mean: 7.3 years SEVERITY: not stated. BASELINE % PRED FEV1: not reported BASELINE DOSE OF ICS: not stated ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
ELIGIBILITY CRITERIA DURING RUN‐IN: Participants who had a change in medication following an exacerbation during run‐in were excluded |
|
| Interventions | LABA + ICS vs INCREASED DOSE ICS OUTCOMES: 6 weeks RUN‐IN PERIOD: 2 weeks DOSE OPTIMISATION PERIOD: 2 weeks INTERVENTION PERIOD: 6 weeks TEST GROUP: combination fluticasone and salmeterol 100/50 μg twice daily via DPI CONTROL GROUP: fluticasone 200 μg twice daily via DPI NUMBER OF DEVICES: 1 COMPLIANCE: not assessed CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 SYMPTOM SCORES: day and nocturnal scores FUNCTIONAL STATUS: rescue medication use INFLAMMATORY MARKERS: sRAW* ADVERSE EFFECTS: reported WITHDRAWALS: reported |
|
| Notes | Unpublished data source from http://ctr.gsk.co.uk Funding source: GSK Confirmation of methods and data not obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Appendix 4 |
| Allocation concealment (selection bias) | Low risk | See Appendix 4 |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical devices used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No detailed information on how intention‐to‐treat population was composed |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected; request for data from study sponsors has not been successful |
| Other bias | Unclear risk | Information on % screening/run‐in population eligible not reported |
SD 039 0714.
| Methods | Parallel‐group multi‐centre study | |
| Participants | Steroid‐using symptomatic asthmatic adolescents % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 60 RANDOMLY ASSIGNED: 271 (F6/Bud 200 μg twice daily: 136; Bud 200 μg twice daily: 135) WITHDRAWALS: F/BUD 200 μg twice daily: 25; BUD 200 μg twice daily: 27 AGE, mean (range): 14 (11 to 17) years GENDER (male %): 42 ASTHMA SEVERITY: moderate BASELINE % PRED FEV1 mean: 75 BASELINE DOSE OF ICS (start of run‐in): not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: ICS 375 to 1000 μg BDP equivalent; FEV1 40% to 90% of predicted normal; ≥ 12% improvement following inhalation of 1 mg of terbutaline EXCLUSION CRITERIA: not reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: symptomatic |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES: reported at 1, 2 and 3 months RUN‐IN PERIOD: 2 weeks to document stability DOSE OF ICS DURING RUN‐IN: not clear DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 3 months TEST GROUP: combination BUD and F 200/6 μg twice daily CONTROL GROUP: BUD 200 μg twice daily DEVICE: Turbuhaler NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF*; pm PEF SYMPTOM SCORES: recorded but not reported FUNCTIONAL STATUS: rescue medication use (recorded but not reported); nocturnal awakening (recorded but not reported); episode‐free days (recorded but not reported) INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Unpublished data downloaded from AZ website (www.astrazenecaclinicaltrials.com) Funded by AstraZeneca Confirmation of data and methods obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information not available |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No detailed information on how intention‐to‐treat population was composed |
| Selective reporting (reporting bias) | Unclear risk | OCS‐treated exacerbations were not reported in the study publication; data request was made to study sponsors to ask for this information |
| Other bias | Low risk | 59% run‐in population eligible |
SD 039 0718.
| Methods | Parallel‐group multi‐centre study (52 centres in USA) | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 60 RANDOMLY ASSIGNED: 273 (BUD/F: 128; BUD: 145) WITHDRAWALS: BUD/F: 36; BUD: 51 AGE, mean (range) or mean (SD): 10.4 (2.6) years SEVERITY: not stated BASELINE % PRED FEV1: 82 BASELINE DOSE OF ICS: 235 μg/d ASTHMA DURATION: 7 years ATOPY (%): not stated ELIGIBILITY CRITERIA: 6 to 15 years; low to medium dose of ICS; FEV1 predicted > 50%; reversibility criteria age dependent: > 12 years 14% and 0.2 L; < 12 years: 12% EXCLUSION CRITERIA: not reported ELIGIBILITY CRITERIA DURING RUN‐IN: symptoms and lung function not otherwise described |
|
| Interventions | LABA + ICS vs SAME DOSE ICS OUTCOMES: 12 weeks RUN‐IN PERIOD: 1 to 2 weeks DOSE OPTIMISATION PERIOD: not applicable INTERVENTION PERIOD: 12 weeks TEST GROUP: combination BUD/F (100/9 μg) twice daily via metered‐dose inhaler CONTROL GROUP: BUD 100 μg twice daily via metered‐dose inhaler NUMBER OF DEVICES: 1 COMPLIANCE: not assessed CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: NA FUNCTIONAL STATUS: NA INFLAMMATORY MARKERS: NA ADVERSE EFFECTS: stated WITHDRAWALS: stated |
|
| Notes | Unpublished data from AZ clinical trials website Funded by AstraZeneca Confirmation of data and methods obtained User‐defined number: 200 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 'The efficacy analysis set (EAS) was defined as all randomised subjects who took at least 1 dose of study medication and contributed at least 1 PEF value to the primary endpoint' No information given on whether EAS population included last observation |
| Selective reporting (reporting bias) | Unclear risk | OCS‐treated exacerbations were not reported in the study publication. Data request has been made to study sponsors for this information. |
| Other bias | Low risk | 59% screening population eligible |
Simons 1997.
| Methods | Randomised double‐blind cross‐over single‐centre study | |
| Participants | Asymptomatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 16 WITHDRAWALS: 2 (13%) AGE, mean (range): 13.1 (12 to 16) years GENDER (% male): 44 SEVERITY: not described BASELINE % PRED FEV1: 93.4 BASELINE DOSE OF ICS: 100 to 200 μg BDP twice daily ASTHMA DURATION: 5.9 ± 3.4 years ATOPY (%): 100 ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: N/A |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES measured at: days 1 and 28 RUN‐IN PERIOD: not specified DOSE OF ICS DURING RUN‐IN: not reported DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 28 days WASHOUT PERIOD: 14 days TEST GROUP: salmeterol 50 μg once daily + BDP 100 to 200 μg twice daily CONTROL GROUP: BDP 100 to 200 μg twice daily + placebo DEVICE: metered‐dose inhaler and Nebulizer Chronolog device NUMBER OF DEVICES: 2 COMPLIANCE: medication usage recorded in participant diary. Device inserted into MDI recorded date, hour and minute of each inhalation CO‐TREATMENT: SABA as needed (200 μg up to 3 times daily), except that albuterol was not permitted 8 hours before each exercise test. If participants had allergic rhinitis, they were permitted to use pseudoephedrine (Sudafed) 1 to 3 times daily as needed, except on the days when exercise tests were scheduled |
|
| Outcomes | PULMONARY FUNCTION TEST: exercise challenge (max % fall in FEV1 from pre‐exercise baseline) SYMPTOM SCORES: symptoms FUNCTIONAL STATUS: rescue medication use; exacerbations requiring systemic steroids INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: described PRIMARY OUTCOME MEASURE: not specified |
|
| Notes | Full‐text publication Funded by GSK Confirmation of data and methods obtained User‐defined number: 300 (1/2 with BDP 100 twice daily; 1/2 with BDP 200 twice daily) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the study |
| Selective reporting (reporting bias) | Low risk | Data on OCS‐treated exacerbations available |
| Other bias | Unclear risk | Information on % screening population eligible not available |
Stelmach 2007.
| Methods | Parallel‐group single‐centre study in Poland | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 97 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 58 (BUD/F: 29; BUD: 29) WITHDRAWALS: 0 AGE, mean (range) or mean (SD): 10 years SEVERITY: moderate BASELINE % PRED FEV1: 94 BASELINE DOSE OF ICS: 400 μg/d BDP‐equivalent ASTHMA DURATION: 4 years ATOPY (%): 100 ELIGIBILITY CRITERIA: 6 to 18 years; history of asthma requiring treatment with ICS EXCLUSION CRITERIA: upper RTI in previous 3 weeks; sinus disease requiring antibiotics within 4 weeks; oral steroids within 4 weeks of study entry; immunotherapy ELIGIBILITY CRITERIA DURING RUN‐IN: not reported |
|
| Interventions | ICS and LABA vs SAME DOSE ICS OUTCOMES: 8 weeks RUN‐IN PERIOD: 4 weeks DOSE OPTIMISATION PERIOD: INTERVENTION PERIOD: 8 weeks TEST GROUP: BUD 200 μg + F 9 μg via Turbuhaler CONTROL GROUP: BUD 200 μg/d via Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: not assessed CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; FEF25% to 75%; SRaw SYMPTOM SCORES: not reported FUNCTIONAL STATUS: not reported INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: not reported WITHDRAWALS: reported |
|
| Notes | Full‐text article Funded by grant from Lodz University, Poland Confirmation of data and methods not obtained User‐defined number: 200 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All completed |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected. Request for this information from study investigator has not been successful. |
| Other bias | Low risk | 97% screening population eligible for study |
Stelmach 2008.
| Methods | Randomised double‐blind placebo‐controlled study | |
| Participants | Children with atopic asthma with confirmed fall ≥ 20% in FEV1 post exercise % ELIGIBLE OF SCREENED POPULATION: 67 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not applicable RANDOMLY ASSIGNED: 40
WITHDRAWALS: 2
AGE, mean: 11.6 years GENDER (% male): not reported SEVERITY: not reported BASELINE % PRED FEV1: 91.7 BASELINE DOSE OF ICS: not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: Male and female outpatients 6 to 18 years of age with a clinical diagnosis of bronchial asthma lasting ≥ 6 months before the first visit were enrolled. To be included in the study, participants had to have a resting FEV1 ≥ 70% and a documented decrease in FEV1 ≥ 20% after a standard exercise challenge test EXCLUSION CRITERIA: Participants were excluded if they had an active upper respiratory tract infection within 3 weeks before the study and acute sinus disease requiring antibiotic treatment within 1 month before the study, previous intubation or asthma hospitalisation during the 3 months before the prestudy visit. Additional criteria were other clinically significant pulmonary, haematological, hepatic, gastrointestinal, renal, endocrine, neurological, cardiovascular and/or psychiatric disease or malignancy that put the patient at risk when participating in the study or could influence study results or the patient’s ability to participate in the study as judged by the investigator. Medications that resulted in patient exclusion included beta‐blockers (eye drops included) or OCS within 1 month before the first visit. Participants receiving immunotherapy were also excluded CRITERIA FOR RANDOMISATION DURING RUN‐IN: ICS (BUD; average dose, 400 μg/d) and montelukast sodium (5 mg or 10 mg, according to age) or LABA |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES measured at: 4 weeks RUN‐IN PERIOD: 4 weeks DOSE OF ICS DURING RUN‐IN: not applicable. DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 4 weeks TEST GROUP: F 4.5 μg + BUD 100 μg twice daily CONTROL GROUP: BDP 100 μg twice daily and placebo DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: inhaled SABA as needed. |
|
| Outcomes | PULMONARY FUNCTION TEST: exercise‐induced bronchoconstriction (AUC0‐20min (% of predicted 3 minutes); maximum % fall in FEV1) SYMPTOM SCORES: not reported FUNCTIONAL STATUS: not reported INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: Standing height and weight were recorded WITHDRAWALS: described |
|
| Notes | Full‐text publication Source of funding: not reported Confirmation of data and methods not obtained Dose of ICS: intervention: 200 μg/d of BDP‐equivalent; control: 200 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated allocation schedule was used. |
| Allocation concealment (selection bias) | Low risk | Centralized hospital pharmacy prepared the drugs and placebos by breaking formulations open. The part of the turbuhaler containing a reservoir of powder with active ingredient was replaced with inert placebo powder. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawals were reported with reasons. All data presented. |
| Selective reporting (reporting bias) | Low risk | Although, the study protocol was not available, no selective reporting was noted. |
| Other bias | Low risk | No apparent source of bias was noticed. |
Tal 2002.
| Methods | Parallel‐group multi‐centre study (48 centres in 7 countries) | |
| Participants | Asymptomatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 286 (F + BDP: 148; BDP: 138) WITHDRAWALS: F/BDP: 9; BDP: 9 AGE, mean (range): 11 (4 to 17) years GENDER (% male): 62 SEVERITY: mild BASELINE % PRED FEV1: 75 BASELINE DOSE OF ICS: 548 ASTHMA DURATION: 6.8 years ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: no other additional criteria |
|
| Interventions | LABA + ICS vs SAME dose of ICS OUTCOMES measured at: 4, 8 and 12 weeks RUN‐IN PERIOD: 2 to 4 weeks DOSE OF ICS DURING RUN‐IN: BUD 200 twice daily DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 12 weeks TEST GROUP: F 12 µg twice daily + BDP 200 µg twice daily CONTROL GROUP: BDP 200 µg twice daily and placebo DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed. If participants had allergic rhinitis, they were permitted to use nasal corticosteroids; treatment with other asthma medication not permitted |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 predicted SYMPTOM SCORES: daily and nocturnal on 4‐point scale FUNCTIONAL STATUS: rescue medication use; nighttime awakening; symptom‐free days INFLAMMATORY MARKERS: not reported ADVERSE EFFECTS: reported WITHDRAWALS: described *Primary outcome |
|
| Notes | Full‐text publication Source of funding: AstraZeneca Confirmation of data and methods obtained |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | 'Individual treatment code envelopes were provided for each subject' |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Explicit description of how ITT population was composed was not presented: 'An intention‐to‐treat analysis was used with all available data' |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected in the study; correspondence with study investigators has not clarified this |
| Other bias | Unclear risk | No information available on % screening/run‐in populations eligible for the study |
Teper 2005.
| Methods | Parallel‐group single‐centre study | |
| Participants | Children with mild to moderate asthma % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 82 (fluticasone/salmeterol: 43; FP: 39) WITHDRAWALS: not reported AGE, mean: 10 years GENDER (male %): 59 ASTHMA SEVERITY: mild to moderate BASELINE % PRED FEV1: 95 BASELINE DOSE OF ICS (start of run‐in): not reported ASTHMA DURATION: not reported ATOPY (%): not reported ELIGIBILITY CRITERIA: ATS diagnosed mild or moderate asthma; age 6 to 14 years of participants; FEV1 > 70% of predicted; methacholine PC20 < 2 μg/mL EXCLUSION CRITERIA: not reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: not reported |
|
| Interventions | LABA + ICS vs SAME dose ICS OUTCOMES: 12 months RUN‐IN PERIOD: unclear DOSE OF ICS DURING RUN‐IN: not reported DOSE OPTIMISATION PERIOD: none reported INTERVENTION PERIOD: 12 months TEST GROUP: combination fluticasone and salmeterol 125/25 twice daily CONTROL GROUP: fluticasone 125 μg twice daily DEVICE: MDI (with aerochamber) NUMBER OF DEVICES: 1 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 % predicted SYMPTOM SCORES: % symptom‐free days; % symptom‐free nights FUNCTIONAL STATUS: % SABA‐free days INFLAMMATORY MARKERS: PC20 ADVERSE EFFECTS: reported WITHDRAWALS: not reported PRIMARY OUTCOME MEASURES: not clear |
|
| Notes | Unpublished conference abstract Source of funding: not reported Confirmation of data and methods not obtained User‐defined number: 500 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information available |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; means by which assignment to treatment group is masked is not available |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided on ITT population |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether data on OCS‐treated exacerbations were collected |
| Other bias | Unclear risk | No information available on % screening/run‐in populations eligible for the study |
Vaessen‐Verberne 2010.
| Methods | Multi‐centre randomised parallel‐group double‐blind study | |
| Participants | Children with moderate asthma % ELIGIBLE OF SCREENED POPULATION: 62 % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 158
WITHDRAWALS: 7
AGE, mean: 9.4 years GENDER (male %): 58 ASTHMA SEVERITY: moderate BASELINE % PRED FEV1: 100 BASELINE DOSE OF ICS (start of run‐in): maximum 250 μg fluticasone or equivalent ASTHMA DURATION: 5.6 years ATOPY (%): 59 ELIGIBILITY CRITERIA: all children with moderate asthma; history of bronchial hyperresponsiveness; used ICS (maximum 250 μg fluticasone or equivalent) EXCLUSION CRITERIA: not reported CRITERIA FOR RANDOMISATION DURING RUN‐IN: children still symptomatic despite regular use of FP, 100 μg twice a day |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES: evaluated at 1, 6, 16 and 26 weeks RUN‐IN PERIOD: 4 weeks DOSE OF ICS DURING RUN‐IN: INTERVENTION PERIOD: 26 weeks DOSE OPTIMISATION PERIOD: none Test group: salmeterol/fluticasone 50/100 μg twice a day Control group: fluticasone 200 μg twice a day DEVICE: Diskhaler NUMBER OF DEVICES: 1 COMPLIANCE: reported CO‐TREATMENT: salbutamol 200 μg Diskus |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1, FVC, FEV1/FVC, MEF50 and PEF rate, PD20 methacholine test SYMPTOM SCORES: symptom‐free days after 26 weeks* FUNCTIONAL STATUS: oropharyngeal examination, height by stadiometry (including height history), 12‐hour urine cortisol, weekly % of participants with ‘good controlled weeks’, ‘maximal controlled weeks’, cumulative number of symptom‐free weeks until end of treatment, time to asthma control defined as time to first ‘good controlled week’ or ‘maximum controlled week' INFLAMMATORY MARKERS: exhaled nitric oxide (in selected centres) ADVERSE EFFECTS: adverse events and serious adverse events reported WITHDRAWALS: reported *Primary outcome |
|
| Notes | Full‐text publication Funded by GSK Confirmation of methods and data not obtained Dose of ICS: intervention: 400 μg/d of BDP‐equivalent; control: 400 μg/d of BDP‐equivalent |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported the technique of randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Not reported the allocation technique. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention to treat analysis. All outcomes were reported. Imbalanced withdrawals but reasons for withdrawals clearly reported. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes were reported. |
| Other bias | Low risk | No apparent bias was noticed. |
Verberne 1998a.
| Methods | Parallel‐group multi‐centre study (9 centres); 3 groups, of which 2 are considered in this review | |
| Participants | Asthmatic children % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: not reported RANDOMLY ASSIGNED: 117 (BDP 400 + salmeterol: 60; BDP 400: 57) WITHDRAWALS: BDP 400 + salmeterol: 5; BDP 400: 4 AGE, mean (SD): 11 (2.6) years GENDER (% male): 65 SEVERITY: mild BASELINE % PRED FEV1: 88 BASELINE DOSE OF ICS (SD): 489 (153) ASTHMA DURATION mean (SD): 8.1 (3.2) ATOPY (%): 88 ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
CRITERIA FOR RANDOMISATION DURING RUN‐IN: no additional criteria |
|
| Interventions | LABA + ICS vs SAME dose ICS OUTCOMES: reported at 6, 12, 18, 24, 30, 36, 42, 48 and 54 weeks RUN‐IN PERIOD: 6 weeks DOSE OF ICS DURING RUN‐IN: BDP 200 μg twice daily INTERVENTION PERIOD: 54 weeks DOSE OPTIMISATION PERIOD: none TEST GROUP: (salmeterol 50 μg + BDP 200 μg) salmeterol 50 μg twice daily and BDP 200 μg twice daily CONTROL GROUP: (BDP 200 + placebo) BDP 200 μg twice daily + placebo DEVICE: Rotadisks in combination with a Diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF; FVC SYMPTOM SCORES: Asthma symptoms like wheezing, dyspnoea, exercise‐induced asthma and cough were scored in the morning and evening on a scale from 1 to 3 FUNCTIONAL STATUS: Rescue medication use; exacerbation (requiring systemic steroids); height, body weight, heart rate and systolic and diastolic blood pressures were measured INFLAMMATORY MARKERS: total IgE ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome: airway calibre measured as FEV1 and airway responsiveness to methacholine |
|
| Notes | Full‐text publication Funded by GSK Confirmation of methods and data obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Telephone notification of assignment by coordinating centre |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; identical placebo used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear how population was identified for primary outcome Incomplete diary card data not included in analysis: 'Where patients failed to complete their daily record cards for more than 7 d in any 14‐d period such assessments were not included in the analysis. Otherwise, when there were missing days in the record, pro rata adjustment was made to give a 2‐wk assessment' |
| Selective reporting (reporting bias) | Low risk | OCS‐treated exacerbation data available |
| Other bias | Unclear risk | No information available on % screening/run‐in populations eligible for the study |
Verberne 1998b.
| Methods | See Verberne 1998a | |
| Participants | As for Verberne 1998a, except for RANDOMLY ASSIGNED: 120 WITHDRAWALS: BDP 400 + salmeterol: 5; BDP 800: 6 |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES: reported at 6, 12, 18, 24, 30, 36, 42, 48 and 54 RUN‐IN PERIOD: 6 weeks DOSE OF ICS DURING RUN‐IN: BDP 200 twice daily DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 54 weeks TEST GROUP: (salmeterol 50 + BDP200): salmeterol 50 μg twice daily + BDP 200 μg twice daily CONTROL GROUP: (BDP 400 + placebo): BDP 400 μg/d + placebo DEVICE: Rotadisks in combination with a Diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: not reported CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF; FVC SYMPTOM SCORES: Asthma symptoms like wheezing, dyspnoea, exercise‐induced asthma and cough were scored in the morning and evening on a scale from 1 to 3 FUNCTIONAL STATUS: Rescue medication use; exacerbation (requiring systemic steroids); height, body weight, heart rate and systolic and diastolic blood pressures were measured INFLAMMATORY MARKERS: total IgE ADVERSE EFFECTS: reported WITHDRAWALS: reported *Primary outcome: airway calibre measured as FEV1 and airway responsiveness to methacholine |
|
| Notes | Full‐text publication Funded by GSK Confirmation of methods and data obtained User‐defined number: 400 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | See Verberne 1998a |
| Allocation concealment (selection bias) | Low risk | See Verberne 1998a |
| Blinding (performance bias and detection bias) All outcomes | Low risk | See Verberne 1998a |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Verberne 1998a |
| Selective reporting (reporting bias) | Low risk | See Verberne 1998a |
| Other bias | Unclear risk | See Verberne 1998a |
Zimmerman 2004a.
| Methods | Parallel‐group multi‐centre study (27 centres in Canada). Three treatment arms comparing LABA/ICS with 2 doses of LABA and ICS alone. Two groups will be considered here, and as the same control group is used for both comparisons, half the control group will be applied to each | |
| Participants | Children ≥ 6 to 11 years of age % ELIGIBLE OF SCREENED POPULATION: not reported % RUN‐IN PARTICIPANTS RANDOMLY ASSIGNED: 68 RANDOMLY ASSIGNED: 196 (F + usual ICS twice daily: 95; usual ICS: 101) WITHDRAWALS: F + usual ICS: 7; usual ICS: 16 AGE, mean (range): 9 (6 to 11) years GENDER (% male): 63 SEVERITY: moderate BASELINE FEV1 % Pred: 77.4 BASELINE DOSE OF ICS: 445 ASTHMA DURATION (years): 5.7 ATOPY (%): not reported ELIGIBILITY CRITERIA:
EXCLUSION CRITERIA:
RANDOMISATION CRITERIA FOLLOWING RUN‐IN:
|
|
| Interventions | LABA + ICS vs usual dose of ICS OUTCOMES: measured at trial entry and after 4, 8 and 12 weeks RUN‐IN PERIOD: 2 weeks DOSE OF ICS DURING RUN‐IN: usual ICS DOSE OPTIMISATION PERIOD: none INTERVENTION PERIOD: 12 weeks TEST GROUP: usual dose ICS + F 4.5 μg twice daily CONTROL GROUP: usual dose ICS + placebo twice daily DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: measured during run‐in CO‐TREATMENT: SABA as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 (Note: Mean value during treatment for 12 weeks reported rather than value at endpoint) SYMPTOM SCORES: total asthma symptom score FUNCTIONAL STATUS: rescue medication use; paediatric asthma quality of life score INFLAMMATORY MARKERS: not described ADVERSE EFFECTS: described WITHDRAWALS: described *Primary outcome measure |
|
| Notes | Full‐text publication Supported by: not stated Confirmation of methods and data not obtained User‐defined number (mean ICS dose in LABA group in μg/d of BDP‐equivalent): 444 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised; no other information presented |
| Allocation concealment (selection bias) | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind; double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention‐to‐treat population presented in study publication, but handling of missing data not described |
| Selective reporting (reporting bias) | Low risk | Exacerbations described as those requiring OCS‐treatment and those requiring increased ICS. Separate OCS‐treated exacerbation data could not be extracted |
| Other bias | Low risk | 68% of screening population randomised |
Zimmerman 2004b.
| Methods | See Zimmerman 2004a | |
| Participants | See Zimmerman 2004a, except for TEST GROUP: usual dose ICS + F 9 μg twice daily CONTROL GROUP: usual dose ICS + placebo twice daily RANDOMLY ASSIGNED: 196 (F + usual ICS: 95; usual ICS: 101) WITHDRAWALS: F + usual ICS: 7; usual ICS: 16 |
|
| Interventions | As for Zimmerman 2004a, except for: TEST GROUP: usual dose ICS + F 6 μg twice daily |
|
| Outcomes | See Zimmerman 2004a | |
| Notes | See Zimmerman 2004a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | See Zimmerman 2004a |
| Allocation concealment (selection bias) | Unclear risk | See Zimmerman 2004a |
| Blinding (performance bias and detection bias) All outcomes | Low risk | See Zimmerman 2004a |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Zimmerman 2004a |
| Selective reporting (reporting bias) | Low risk | See Zimmerman 2004a |
| Other bias | Low risk | See Zimmerman 2004a |
AQLQ: Asthma Quality of Life Questionnaire; AUC: Area under the curve; BDP: Beclomethasone dipropionate; BUD: Budesonide; BUD/F: Budesonide and formoterol; DPI: Dry powder inhaler; F: Formoterol; FEF: Forced expiratory flow; FeNO: Exhaled nitric oxide; FEV1: Forced expiratory volume in one second; FP: Fluticasone; FVC: Forced vital capacity; GINA: Global Initiative for Asthma; ICS: Inhaled corticosteroid; IgE: Immunoglobulin E; ITT: Intention‐to‐treat; LABA: Long‐acting beta2‐agonist (salmeterol or formoterol); LTRA: Leukotriene receptor antagonist; MDI: Metered‐dose inhaler; MEF50: Maximal expiratory flow at 50% vital capacity; OCS: Oral corticosteroids; PAQLQ: Paediatric Quality of Life Questionnaire; PC20: Provocative concentrations that caused a 20% fall in FEV1; PEF: Peak expiratory flow; QD: Once per day; RTI: Respiratory tract infection; SABA: Short‐acting beta2‐agonist; sRAW: Specific airway resistance; SD: Standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aldington 2006 | Inadequate duration |
| Aubier 1999 | Study conducted in adults |
| Bateman 2008 Jul | Dose of ICS was not stable (dose tapering study) |
| Bergmann 2004 | Not exclusively children |
| Bernstein 2011 | Control was not ICS |
| Borker 2005 | No LABA alone |
| Boulet 2003 | Adult study |
| Bousquet 2005 | No LABA alone |
| Bracamonte 2005 | Comparison of devices |
| Bruce 2005 | Review article |
| Bruggenjurgen 2005 | Not exclusively paediatric |
| Buchvald 2002 | No ICS alone |
| Buhl 2004 | Adjustable dosing in adults |
| Caffey 2005 | No LABA alone |
| Chen 2010 | Not an RCT |
| Chopra 2005 | No ICS alone |
| Chuchalin 2005 | No ICS alone |
| Corren 2013 | Adult study |
| Covar 2008 Oct | Duplication of Sorkness 2007 |
| Cowan 2004 | Not an RCT |
| Daviskas 2005 | No ICS alone |
| Delaronde 2005 | No assessment of asthma control |
| Drummond 2011 | Duplication of LOCCS study |
| Dubus 2003 | No LABA |
| Emeryk 2003 | Comparison of devices |
| Everden 2004 | Not placebo‐controlled |
| Fardon 2005 | No LABA |
| Grady 1995 | Not exclusively children |
| Holgate 2004 | Study of Xolair |
| Holt 2005 | Not exclusively children |
| Ilowite 2004 | Adult study |
| Jenkins 2005 | Adult study |
| Karaman 2007 | No prior ICS exposure |
| Katial 2011 Mar | Adult study |
| Kerwin 2008 Apr | Adult study |
| Lara‐Perez 2005 | No ICS alone |
| Levy 2005 | Co‐treatment with ICS in only 3/4 participants. Study primarily interested in efficacy of formoterol on top of usual therapy. ICS dosing not standardised |
| Li 2010 | No asthma control |
| Lipworth 2013 | Control group was not given ICS |
| LOCCS | Adult study |
| Lundbäck 2009 Mar | Adult study |
| Makela 2012 | Steroid‐naive patients enrolled in the study |
| Matthys 2004 | Open study |
| Miraglia 2007 | No prior exposure to ICS |
| Mitchell 2005 | No LABA |
| Mitra 2003 | No concurrent ICS |
| Morice 2005 | Not exclusively children |
| Morice 2005a | Not exclusively children |
| Morice 2008 | Compared the same medication |
| Murray 2004 | Not exclusively children |
| Nathan 2005 | Not exclusively children |
| Nelson 2006 | Not exclusively children |
| Nguyen 2005 | Not an RCT |
| Noyes 2013 | Not an RCT |
| O'Byrne 2001 | Adolescents and adults |
| Pearlman 2004 | Study in adults |
| Peroni 2005 | No ICS alone |
| Peters 2008 Sep‐Oct | Adult study |
| Pijnenburg 2005 | No LABA |
| Prates 2009 | Not an RCT |
| Price 2011 May | Adult study |
| Prieto 2005 | Not exclusively children |
| Quirce 2011 Oct | Adult study |
| Reddel 2010 Aug | Adult study |
| Renzi 2005 | Not exclusively children |
| Renzi 2010 Apr | Steroid‐naive patients enrolled in the study |
| SAM30002 | Not exclusively children |
| SAM40101 | Inadequate duration |
| SAS30021 | Steroid‐naive children |
| Schauer 2003 | No ICS alone |
| Scicchitano 2004a | Study in adults |
| Selroos 2004 | No LABA |
| SFCF3001 | Different devices used |
| SFCF3002 | Different devices used |
| Sienra‐Monge 2004 | Not an RCT |
| Soes‐Petersen 2011 Jul | Adult study |
| Sorkness 2007 | Mixed population at baseline |
| Spector 2012 | Adult study |
| Stelmach 2008a | Steroids were stopped for 4 weeks before study visit |
| Storms 2004 | Study in adults |
| van den Toorn 2005 | No ICS alone |
| Vogelmeier 2005 | No ICS alone |
| Von Berg 2003 | No concurrent ICS |
| Weiler 2005 | Study in adults |
| You‐Ning 2005 | Study in adults; no ICS alone |
EIB: Exercise‐induced bronchoconstriction; ICS: Inhaled corticosteroid; LABA: Long‐acting beta2‐agonist; RCT: Randomised controlled trial.
Differences between protocol and review
The principal difference between the protocol for the set of reviews related to long‐acting beta‐agonists and ICS and this review is the risk of bias assessment. This has been developed by methodologists and statisticians and aims to provide a transparent mechanism for reporting the design of clinical trials, and the extent to which review authors judge them to be at risk of bias.
In the current update, we have added two new secondary outcomes, numbers of participants with exacerbations requiring an urgent care visit and % nights with awakening. We have added a 'Summary of findings' table.
Contributions of authors
BC: update of the review, screening of citations, data extraction, method assessment, write‐up and correspondence with the editorial board of the Cochrane Airways Group.
CC: data extraction and method assessment.
MNC: protocol initiation and write‐up, study assessment, characterisation extraction of data and write‐up.
SJM: data extraction and proofreading of the manuscript.
FD: protocol development, review development, interpretation of results and review of final manuscript.
Sources of support
Internal sources
The authors declare that no such funding was received for this systematic review, Other.
External sources
The authors declare that no such funding was received for this systematic review, Other.
Declarations of interest
In the past five years, Francine Ducharme received some research funding from GSK, Merck and AstraZeneca, and gave CME conferences supported by Merck Frost, GSK and Takeda. Over the past five years, M Ni Chroinin has given CME lectures sponsored by AstraZeneca. Bhupendrasinh Chauhan, Caroline Chartrand and Stephen J Milan, as well as previous authors, namely, A. Danish, H. Magalinos, V. Masse, X. Zhang, Toby Lasserson and Ilana Greenstone, report no conflicts of interest.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Akpinarli 1999 {published data only}
- Akpinarli A, Tuncer A, Saraclar Y, Sekerel BE, Kalayci O. Effect of formoterol on clinical parameters and lung functions in patients with bronchial asthma: a randomised controlled trial. Archives of Disease in Childhood 1999;81(1):45‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berger 2010 {published data only}
- AstraZeneca Pharmaceuticals (SD 039 0719). A six‐month, randomized, open‐label safety study of Symbicort® (160/4.5 mcg) compared to Pulmicort Turbuhaler® in asthmatic children aged 6 to 11 years. http://www.astrazenecaclinicaltrials.com (accessed 4 January 2008).
- Berger WE, Leflein JG, Geller DE, Parasuraman B, Miller CJ, O'Brien CD, et al. The safety and clinical benefit of budesonide/formoterol pressurized metered‐dose inhaler versus budesonide alone in children. Allergy Asthma Proceedings 2010;31(1):26‐39. [DOI] [PubMed] [Google Scholar]
Bisgaard 2006 {published data only}
- Barnes PJ, O'Byrne PM, Rodriguez‐Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Oxis and Pulmicort turbuhaler in the management of asthma OPTIMA international study group. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. Thorax 2000;55(Suppl 3):A4. [Google Scholar]
- Barnes PJ, O'Byrne PM, Rodriguez‐Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. For the Oxis and Pulmicort Turbuhaler in the Management of Asthma (OPTIMA) international study group. Thorax 2000; Vol. 55, issue Suppl 3:s5.
- Bisgaard H, Hultquist C. Budesonide/formoterol for maintenance and as needed ‐ a new approach to asthma management in children [Abstract]. European Respiratory Journal 2005;26(Suppl 49):1060. [Google Scholar]
- Bisgaard H, Roux P, Bjamer D, Dymek A, Vermeulen JH, Hultquist C. Budesonide/formoterol maintenance plus reliever therapy ‐ a new strategy in pediatric asthma. Chest 2006;130(6):1733‐43. [DOI] [PubMed] [Google Scholar]
- Jönsson BG, Berggren FE, Svensson K, O'Byrne PM. Budesonide and formoterol in mild persistent asthma compared with doubling the dose of budesonide ‐ a cost‐effectiveness analysis. European Respiratory Journal. 2001;18(Suppl 33):517s. [Google Scholar]
- Jönsson BG, Berggren FE, Svensson K, O'Byrne PM. Economic results of adding formoterol to budesonide in mild persistent asthma. European Respiratory Journal 2001;18(Suppl 33):331s. [Google Scholar]
- O'Byrne PM. Acute asthma intervention: Insights from the STAY study. Journal of Allergy and Clinical Immunology 2007;119(6):1332‐6. [DOI] [PubMed] [Google Scholar]
- O'Byrne PM, Barnes PJ, Rodriguez‐Roisin R, Sandtröm T, Tattersfield AE, Runnerström EM, et al. Addition of formoterol Turbuhaler® to budesonide Tubuhaler® is safe and well tolerated in the long‐term treatment of mild asthma: results from the OPTIMA trial. European Respiratory Journal 2001;18(Suppl 33):330s. [Google Scholar]
- O'Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma [see comment]. American Journal of Respiratory and Critical Care Medicine 2005;171(2):129‐36. [DOI] [PubMed] [Google Scholar]
- SD‐039‐0673. Efficacy and safety of budesonide/formoterol (Symbicort) Turbuhaler® as Single Therapy in patients with mild‐moderate asthma. Comparison with Symbicort Turbuhaler and Pulmicort® Turbuhaler as maintenance therapy, both complemented with Bricanyl® Turbuhaler (STAY). http://www.astrazenecaclinicaltrials.com/Submission/View?id=1007 (accessed 8 May 2015).
Carroll 2010 {published data only}
- Carroll WD, Jones PW, Boit P, Clayton S, Cliff I, Lenney W. Childhood evaluation of salmeterol tolerance ‐ A double‐blind randomized controlled trial. Pediatric Allergy and Immunology 2010 Mar;21(2 PART 1):336‐44. [DOI] [PubMed] [Google Scholar]
De Blic 2009 {published data only}
- Blic J, Ogorodova L, Klink R, Sidorenko I, Valiulis A, Hofman J, et al. Salmeterol/fluticasone propionate vs. double dose fluticasone propionate on lung function and asthma control in children. Pediatric Allergy and Immunology 2009; Vol. 20, issue 8:763‐71. [DOI] [PubMed]
- Glaxo Smith Kline (SAM104926). A multicentre, randomised, double‐blind, double dummy, parallel group study to compare the salmeterol/fluticasone propionate combination (SERETIDE™) at a dose of 50/100mcg twice daily and fluticasone propionate (FLIXOTIDE™) at a dose of 200mcg twice daily, both delivered via a dry powder inhaler (DISKUS™) for 12 weeks in asthma in children aged 4‐11 years not controlled by inhaled corticosteroids alone at medium dose. http://ctr.gsk.co.uk (accessed 14 January 2008).
Eid 2010a {published data only}
- AstraZeneca Pharmaceuticals (SD 039 0725). A twelve‐week, randomized, double‐blind, double‐dummy, active‐controlled study of Symbicort® pMDI administered once daily in children and adolescents 6 to 15 years of age with asthma. http://astrazenecagrouptrials.pharmacm.com/Submission/View?id=966 (accessed 8 May 2015).
Eid 2010b {unpublished data only}
- AstraZeneca Pharmaceuticals (SD 039 0725). A twelve‐week, randomized, double‐blind, double‐dummy, active‐controlled study of Symbicort® pMDI administered once daily in children and adolescents 6 to 15 years of age with asthma. http://www.astrazenecaclinicaltrials.com (accessed 4 January 2008).
Gappa 2009 {published data only}
- Gappa M, Zachgo W, Berg A, Kamin W, Stern‐Sträter C, Steinkamp G, et al. Add‐on salmeterol compared to double dose fluticasone in pediatric asthma: a double‐blind, randomized trial (VIAPAED). Pediatric Pulmonology 2009;44(11):1132‐42. [DOI] [PubMed] [Google Scholar]
Heuck 2000 {published data only}
- Heuck C, Heickendorff L, Wolthers OD. A randomized controlled trial of short term growth and collagen turnover in asthmatics with inhaled formoterol and budesonide. Archives of Disease of Childhood 2000;83(4):334‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuck C, Heickendorff L, Wolthers OD, Sygehus S. Short term growth and collagen turnover in asthmatics treated inhaled formoterol and budesonide. European Respiratory Society Annual Congress; 1999 Oct 9‐13; Madrid. 1999:364.
Langton Hewer 1995 {published data only}
- Langton Hewer S, Hobbs J, French D, Lenney W. Pilgrims progress: the effect of salmeterol in older children with chronic severe asthma. Respiratory Medicine 1995;89(6):435‐40. [DOI] [PubMed] [Google Scholar]
Lemanske 2010 {published data only}
- Lemanske RFJr, Mauger DT, Sorkness CA, Jackson DJ, Boehmer SJ, Martinez FD, et al. Step‐up therapy for children with uncontrolled asthma receiving inhaled corticosteroids. New England Journal of Medicine 2010;362(11):975‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lenney 2013 {published data only}
- Lenney W, McKay AJ, Tudur Smith C, Williamson PR, James M, Price D. Management of asthma in school age children on therapy. Health Technology Assessment 2013; Vol. 17, issue 4:1‐238. [DOI] [PMC free article] [PubMed]
Malone 2005 {published and unpublished data}
- Dorinsky P, Emmett A, Sutton L. Reduced risk for asthma exacerbations in pediatric patients receiving salmeterol plus inhaled corticosteroids (ICS) vs ICS alone [Abstract]. European Respiratory Journal 2004;24(Suppl 48):308s. [Google Scholar]
- House K, Dorinsky PM, Stauffer J, Schoaf L, Ellsworth A. The safety of fluticasone propionate/salmeterol Diskus(R) in pediatric patients ages 4 ‐11 with asthma [Abstract]. Chest 2004;126(Suppl 4):911S. [Google Scholar]
- Malone R, LaForce C, Nimmagadda S, Schoaf L, House K, Ellsworth A, et al. The safety of twice‐daily treatment with fluticasone propionate and salmeterol in pediatric patients with persistent asthma. Annals of Allergy, Asthma, and Immunology 2005;95(1):66‐71. [DOI] [PubMed] [Google Scholar]
- SAS30031. A randomized, double‐blind, 12‐week trial evaluating the safety of the fluticasone propionate/salmeterol DISKUS combination product 100/50mcg BID versus fluticasone propionate DISKUS 100mcg BID in symptomatic pediatric subjects (4‐11 years) with asthma. http://www.gsk‐clinicalstudyregister.com/study/SAS30031?study_ids=SAS30031#rs (accessed 8 May 2015).
- Scott C, Wu W, Ellsworth A, Crim C. Efficacy and safety of fluticasone propionate/salmeterol DISKUS and fluticasone propionate DISKUS and HFA in children [Abstract]. European Respiratory Journal 2005;26(Suppl 49):1057. [Google Scholar]
Meijer 1995 {published data only}
- Meijer GG, Postma DS, Mulder PG, Aalderen WM. Long‐term circadian effects of salmeterol in asthmatic children treated with inhaled corticosteroids. American Journal of Respiratory and Critical Care Medicine 1995;152:1887‐92. [DOI] [PubMed] [Google Scholar]
Morice 2008a {published and unpublished data}
- AstraZeneca SD 039 0682. A 12‐week randomised, double‐blind, parallel‐group, multicentre phase‐III study to compare the efficacy and safety of Symbicort® pMDI (budesonide/formoterol 80/4.5 mcg 2 actuations b.i.d., delivered dose) with that of Pulmicort® pMDI (budesonide 100 mcg 2 actuations b.i.d., metered dose) and Symbicort Turbuhaler®(budesonide/formoterol 80/4.5 mcg 2 actuations b.i.d., delivered dose) in children with asthma. http://www.astrazenecaclinicaltrials.com (accessed 4 January 2008).
- Morice AH, Peterson S, Beckman O, Kukova Z. Efficacy and safety of a new pressurised metered‐dose inhaler formulation of budesonide/formoterol in children with asthma: a superiority and therapeutic equivalence study. Pulmonology Pharmacology Therapeutics 2008;21(1):152‐9. [DOI] [PubMed] [Google Scholar]
Morice 2008b {published data only}
- AstraZeneca. A 12‐week randomised, double‐blind, parallel‐group, multicentre phase‐III study to compare the efficacy and safety of Symbicort®pMDI (budesonide/formoterol 80/4.5 mcg 2 actuations b.i.d., delivered dose) with that of Pulmicort® pMDI (budesonide 100 mcg 2 actuations b.i.d., metered dose) and Symbicort Turbuhaler® (budesonide/formoterol 80/4.5 mcg 2 actuations b.i.d., delivered dose) in children with asthma. http://www.astrazenecaclinicaltrials.com (accessed 4 January 2008).
- Morice AH, Peterson S, Beckman O, Kukova Z. Efficacy and safety of a new pressurised metered‐dose inhaler formulation of budesonide/formoterol in children with asthma: a superiority and therapeutic equivalence study. Pulmonology Pharmacology Therapeutics 2008; Vol. 21, issue 1:152‐9. [DOI] [PubMed]
Murray 2010 {published data only}
Murray 2011 {published data only}
- Glaxo Smith Kline (SFA100316). A stratified, multicenter, randomized, double‐blind, parallel group, 4‐week comparison of fluticasone propionate/salmeterol DISKUS combination product 100/50mcg BID versus fluticasone propionate DISKUS 100mcg BID in pediatric and in adolescent subjects with activity‐induced bronchospasm. http://ctr.gsk.co.uk (accessed 30 April 2008).
- Murray JJ, Waitkus‐Edwards KR, Yancey SW. Evaluation of fluticasone propionate and fluticasone propionate/salmeterol combination on exercise in pediatric and adolescent patients with asthma. Open Respiratory Medical Journal 2011;5:11‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ortega‐Cisneros 1998 {published data only}
- Ortega‐Cisnero M, Maldonado‐Alaniz ML, Rosas Vargas MA, Sierra‐Monge JJL. Salmeterol and inhaled beclomethasone versus high dose inhaled beclomethasone in the control of pediatric patients with moderate asthma. Annals of Allergy, Asthma and Immunology 1998;80:131. [Google Scholar]
Pearlman 2009 {published data only}
- Glaxo Smith Kline (SFA100314). A stratified, multicenter, randomized, double‐blind, parallel group, 4‐week comparison of fluticasone propionate/salmeterol DISKUS combination product 100/50mcg BID versus fluticasone propionate DISKUS 100mcg BID in pediatric and in adolescent subjects with activity‐induced bronchospasm. http://www.ctr.gsk.co.uk (accessed 16 May 2008).
- Pearlman D, Qaqundah P, Matz J, Yancey SW, Stempel DA, Ortega HG. Fluticasone propionate/salmeterol and exercise‐induced asthma in children with persistent asthma. Pediatric Pulmonology 2009 May; Vol. 44, issue 5:429‐35. [DOI] [PubMed]
Pohunek 2006a {published and unpublished data}
- Pohunek P, Kuna P, Boeck K. Budesonide/formoterol improves lung function compared with budesonide alone in children with asthma [Abstract]. European Respiratory Journal 2004;24(Suppl 48):379s. [Google Scholar]
- Pohunek P, Kuna P, Jorup C, Boeck KD. Budesonide/formoterol improves lung function compared with budesonide alone in children with asthma. Pediatric Allergy and Immunology 2006;17(6):458‐65. [DOI] [PubMed] [Google Scholar]
- Pohunek P, Matulka M, Rybnicek O, Kopriva F, Honomichlova H, Svobodova T. Dose‐related efficacy and safety of formoterol (Oxis) Turbuhaler compared with salmeterol Diskhaler in children with asthma. Pediatric Allergy and Immunology 2004;15(1):32‐9. [DOI] [PubMed] [Google Scholar]
Pohunek 2006b {published and unpublished data}
- Pohunek P, Kuna P, Boeck K. Budesonide/formoterol improves lung function compared with budesonide alone in children with asthma [Abstract]. European Respiratory Journal 2004;24(Suppl 48):379s. [Google Scholar]
- Pohunek P, Kuna P, Jorup C, Boeck KD. Budesonide/formoterol improves lung function compared with budesonide alone in children with asthma. Pediatric Allergy and Immunology 2006;17(6):458‐65. [DOI] [PubMed] [Google Scholar]
- Pohunek P, Matulka M, Rybnicek O, Kopriva F, Honomichlova H, Svobodova T. Dose‐related efficacy and safety of formoterol (Oxis) Turbuhaler compared with salmeterol Diskhaler in children with asthma. Pediatric Allergy and Immunology 2004;15(1):32‐9. [DOI] [PubMed] [Google Scholar]
Russell 1995 {published data only}
- Glaxo Smith Kline (SALMP/AH91/D89). A phase III, multi‐centre, double‐blind, placebo controlled, parallel group study assessing the efficacy and safety of inhaled salmeterol xinafoate (Serevent™) 50 micrograms BD via the Diskhaler™ when added to the existing treatment of moderate to severe asthmatic children. www.ctr.gsk.co.uk (accessed 9 June 2008).
- Russell G, Williams DAJ, Weller P, Price JF. Salmeterol xinafoate on children on high dose inhaled steroids. Annals of Allergy, Asthma and Immunology 1995;75(5):423‐28. [PubMed] [Google Scholar]
Rutkowski 2009 {published data only}
- Rutkowski R, Rutkowski K, Bilbin M, Rutkowska J, Milewski R, Kosztyla‐Hojna B. Childhood asthma ‐ Effect of regular and on demand formoterol with budesonide treatment twice a day. International Review of Allergology and Clinical Immunology 2009;15(3‐4):52‐8. [Google Scholar]
SAM40012a {unpublished data only}
- Dorinsky P, Emmett A, Sutton L. Reduced risk for asthma exacerbations in pediatric patients receiving salmeterol plus inhaled corticosteroids (ICS) versus ICS alone [Abstract]. European Respiratory Journal 2004;24(Suppl 48):308s. [Google Scholar]
- Glasxo Smith Kline (SAM40012). A multicentre, randomised, double‐blind, double‐dummy, parallel group comparison of three treatments : 1) salmeterol/fluticasone propionate (SFC) (50/100mcg strength) bd via DISKUS/ACCUHALER inhaler, 2) fluticasone propionate 200mcg bd via DISKUS/ACCUHALER inhaler, 3) fluticasone propionate 100mcg bd via DISKUS/ACCUHALER inhaler in children aged 4‐11 years with asthma. http://www.gsk‐clinicalstudyregister.com/study/SAM40012?study_ids=SAM40012#rs (accessed 8 May 2015).
SAM40012b {unpublished data only}
- Dorinsky P, Emmett A, Sutton L. Reduced risk for asthma exacerbations in pediatric patients receiving salmeterol plus inhaled corticosteroids (ICS) vs ICS alone [Abstract]. European Respiratory Journal 2004;24(Suppl 48):308s. [Google Scholar]
- Glaxo Smith Kline (SAM40012). A multicentre, randomised, double‐blind, double‐dummy, parallel group comparison of three treatments : 1) salmeterol/fluticasone propionate (SFC) (50/100mcg strength) bd via DISKUS/ACCUHALER inhaler, 2) fluticasone propionate 200mcg bd via DISKUS/ACCUHALER inhaler, 3) fluticasone propionate 100mcg bd via DISKUS/ACCUHALER inhaler in children aged 4‐11 years with asthma. http://www.gsk‐clinicalstudyregister.com/study/SAM40012#rs (accessed 8 May 2015) 2005.
SAM40100 {unpublished data only}
- Glaxo Smith Kline (SAM40100). Randomised, double‐blind, comparator study to demonstrate the superiority of salmeterol/fluticasone propionate combination DISKUS™ 50/100mcg bd over fluticasone propionate DISKUS™/ACCUHALER™ 200mcg bd with respect to airway physiology in asthmatic children treated for 6 weeks. http://ctr.gsk.co.uk (accessed 4 January 2008).
SD 039 0714 {published data only}
- AstraZeneca Pharmaceuticals (SD 039 0714). Efficacy and safety of budesonide/formoterol Turbuhaler® (160/4.5 mcg b.i.d. delivered dose) compared to budesonide Turbuhaler® (200 mcg b.i.d. metered dose) in steroid‐using asthmatic adolescent patients. A double‐blind, double‐dummy, randomised, parallel group, phase III, multicentre study. http://www.astrazenecaclinicaltrials.com (accessed 21 February 2006).
SD 039 0718 {unpublished data only}
- AstraZeneca Pharmaceuticals (SD 039 0718). A twelve‐week, randomized, double‐blind, double‐dummy trial of Symbicort® (40/4.5 mcg) versus its mono‐products (budesonide and formoterol) in asthmatic children aged six to fifteen years. http://www.astrazenecaclinicaltrials.com (accessed 4 January 2008).
Simons 1997 {published data only}
- Simons FE, Gerstner TV, Cheang MS. Tolerance to the bronchoprotective effect of salmeterol in adolescents with exercise‐induced asthma using concurrent inhaled glucocorticoid treatment. Pediatrics 1997;99(5):655‐9. [DOI] [PubMed] [Google Scholar]
Stelmach 2007 {published data only}
- Stelmach I, Grzelewskia T, Bobrowska‐Korzeniowska M, Stelmach P, Kuna P. A randomized, double‐blind trial of the effect of anti‐asthma treatment on lung function in children with asthma. Pulmonology Pharmacology and Therapeutics 2007;20(6):691‐700. [DOI] [PubMed] [Google Scholar]
Stelmach 2008 {published data only}
- Stelmach I, Grzelewski T, Majak P, Jerzynska J, Stelmach W, Kuna P, et al. Effect of different antiasthmatic treatments on exercise‐induced bronchoconstriction in children with asthma. Journal of Allergy and Clinical Immunology 2008;121(2):383‐9. [DOI] [PubMed] [Google Scholar]
Tal 2002 {published data only}
- AstraZeneca Pharmaceuticals (SD 039 0353). Efficacy and safety of budesonide/formoterol Turbuhaler® in a fixed combination in steroid‐using asthmatic children. http://www.astrazenecaclinicaltrials.com (accessed 25 April 2008).
- Tal A, Simon G, Vermeulen JH. Symbicort® (budesonide and formoterol in a single inhaler) is effective and well tolerated in children with asthma. Annual Thoracic Society 97th International Conference; 2001 May 18‐23; San Francisco. 2001.
- Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Budesonide/Formoterol in a single inhaler versus inhaled corticosteroids alone in the treatment of asthma. Pediatric Pulmonology 2002;34(5):342‐50. [DOI] [PubMed] [Google Scholar]
- Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Rapid and sustained improvements in lung function and symptom control with budesonide/ formoterol in adolescent asthma. European Respiratory Journal 2001;18(Suppl 33):494s. [Google Scholar]
- Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Symbicort (budesonide and formoterol in a single inhaler) improves lung function in children with asthma. International Paediatric Respiratory and Allergy Congress, April 1‐4; Prague. 2001:85.
- Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Symbicort (budesonide and formoterol in a single inhaler) is more effective that budesonide alone in children with asthma. International Paediatric Respiratory and Allergy Congress April 1‐4; Prague. 2001:84‐5.
- Vermeulen JH, Simon G, Tal A. Symbicort® (budesonide and formoterol in a single inhaler) improves lung function in asthmatic children aged 4‐17 years. Annual Thoracic Society 97th International Conference; 2001 May 18‐23; San Francisco. 2001.
Teper 2005 {published data only}
- Teper AM, Zaragoza SM, Lubovich S, Rodriguez VA, Venalago C, Kofman CD, et al. Effect of fluticasone propionate (FP) with or without salmeterol (S) on bronchial reactivity (BR) in children with mild to moderate persistent asthma [Abstract]. American Thoracic Society 2005 International Conference; May 20‐25; San Diego,. 2005:[C47] [Poster: A5].
Vaessen‐Verberne 2010 {published data only}
- Vaessen‐Verberne AA, Berg NJ, Nierop JC, Brackel HJ, Gerrits GP, Hop WC, et al. Combination therapy salmeterol/fluticasone versus doubling dose of fluticasone in children with asthma. American Journal of Respiratory and Critical Care Medicine 2010;182(10):1221‐7. [DOI] [PubMed] [Google Scholar]
Verberne 1998a {published data only}
- Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerribijn KF. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. American Journal of Respiratory and Critical Care Medicine 1998;158(1):213‐9. [DOI] [PubMed] [Google Scholar]
Verberne 1998b {published data only}
- Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerribijn KF. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. American Journal of Respiratory and Critical Care Medicine 1998;158(1):213‐9. [DOI] [PubMed] [Google Scholar]
Zimmerman 2004a {published data only}
- Zimmerman B, D'Urzo A, Berube D. Efficacy and safety of formoterol turbuhaler(R) when added to inhaled corticosteroid treatment in children with asthma. Pediatric Pulmonology 2004;37(2):122‐7. [DOI] [PubMed] [Google Scholar]
- Zimmerman B, D'Urzo A, Berube D. Efficacy and tolerability of formoterol Turbuhaler in 6‐11 year old children with asthma, not adequately controlled with inhaled corticosteroids. European Respiratory Society 12th Annual Congress; 2002 Sep 14‐18; Stockholm. 2002:P2734.
- Zimmerman B, D'Urzo A, Berube D. Efficacy and tolerability of formoterol turbuhaler(r) compared with placebo, in children (6‐11 yr) with asthma poorly controlled with inhaled corticosteroids [abstract]. American Journal of Respiratory and Critical Care Medicine 2002;165(8 Suppl):A746. [Google Scholar]
Zimmerman 2004b {published data only}
- Zimmerman B, D'Urzo A, Berube D. Efficacy and safety of formoterol turbuhaler(R) when added to inhaled corticosteroid treatment in children with asthma. Pediatric Pulmonology 2004;37(2):122‐7. [DOI] [PubMed] [Google Scholar]
- Zimmerman B, D'Urzo A, Berube D. Efficacy and tolerability of formoterol Turbuhaler in 6‐11 year old children with asthma, not adequately controlled with inhaled corticosteroids. European Respiratory Society 12th Annual Congress; 2002 Sep 14‐18; Stockholm. 2002:P2734.
- Zimmerman B, D'Urzo A, Berube D. Efficacy and tolerability of formoterol turbuhaler(r) compared with placebo, in children (6‐11 yr) with asthma poorly controlled with inhaled corticosteroids [abstract]. American Journal of Respiratory and Critical Care Medicine 2002;165(8 Suppl):A746. [Google Scholar]
References to studies excluded from this review
Aldington 2006 {published data only}
- Aldington S, Williams M, Weatherall M, Beasley R. Duration of action of the salmeterol/fluticasone combination inhaler administered in the evening: a randomized controlled trial in childhood asthma. Respirology 2006;11(5):638‐42. [DOI] [PubMed] [Google Scholar]
Aubier 1999 {published data only}
- Aubier M, Pieters WR, Schlosser NJ, Steinmetz KO. Salmeterol/fluticasone propionate (50/500 mug) in combination in a Diskus(TM) inhaler (Seretide(TM)) is effective and safe in the treatment of steroid‐dependent asthma. Respiratory Medicine 1999;93(12):876‐84. [DOI] [PubMed] [Google Scholar]
Bateman 2008 Jul {published data only}
- Bateman ED, Bousquet J, Busse WW, Clark TJ, Gul N, Gibbs M, et al. Stability of asthma control with regular treatment: an analysis of the Gaining Optimal Asthma controL (GOAL) study. Allergy 2008;63(7):932‐8. [DOI] [PubMed] [Google Scholar]
Bergmann 2004 {published data only}
- Bergmann KC, Lindemann L, Braun R, Steinkamp G. Salmeterol/fluticasone propionate (50/250 microg) combination is superior to double dose fluticasone (500 microg) for the treatment of symptomatic moderate asthma. Swiss Medical Weekly 2004;134(3‐4):50‐8. [DOI] [PubMed] [Google Scholar]
Bernstein 2011 {published data only}
- Bernstein DI, Hebert J, Cheema A, Murphy KR, Cherrez‐Ojeda I, Matiz‐Bueno CE, et al. Efficacy and onset of action of mometasone furoate/formoterol and fluticasone propionate/salmeterol combination treatment in subjects with persistent asthma. Allergy, Asthma, and Clinical Immunology 2011;7(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borker 2005 {published data only}
- Borker R, Emmett A, Jhingran P, Rickard K, Dorinsky P. Determining economic feasibility of fluticasone propionate‐salmeterol vs montelukast in the treatment of persistent asthma using a net benefit approach and cost‐effectiveness acceptability curves. Annals of Allergy, Asthma, and Immunology 2005;95(2):181‐9. [DOI] [PubMed] [Google Scholar]
Boulet 2003 {published data only}
- Boulet LP, Roberts J, Watson EG. Efficacy of salmeterol/fluticasone propionate MDI versus higher dose fluticasone propionate in adolescent and adult asthmatics uncontrolled on fluticasone propionate alone [Abstract]. European Respiratory Journal 2003;22(Suppl 45):Abstract No: [P2799]. [Google Scholar]
Bousquet 2005 {published data only}
- Bousquet J, Gaugris S, Kocevar VS, Zhang Q, Yin DD, Polos PG, et al. Increased risk of asthma attacks and emergency visits among asthma patients with allergic rhinitis: a subgroup analysis of the improving asthma control trial. Clinical and Experimental Allergy 2005;35(6):723‐7. [DOI] [PubMed] [Google Scholar]
Bracamonte 2005 {published data only}
- Bracamonte T, Schauer U, Emeryk A, Godwood A, Balsara S. Efficacy and safety of salmeterol/fluticasone propionate combination delivered by the Diskus or pressurised metered‐dose inhaler in children with asthma. Clinical Drug Investigation 2005;25(1):1‐11. [DOI] [PubMed] [Google Scholar]
Bruce 2005 {published data only}
- Bruce SA, Scherer YK. Maintenance and symptom relief with budesonide plus formoterol reduced severe asthma exacerbations. Evidence‐Based Nursing 2005;8(3):78. [DOI] [PubMed] [Google Scholar]
Bruggenjurgen 2005 {published data only}
- Bruggenjurgen B, Selim D, Kardos P, Richter K, Vogelmeier C, Roll S, et al. Economic assessment of adjustable maintenance treatment with budesonide/formoterol in a single inhaler versus fixed treatment in asthma. Pharmacoeconomics 2005;23(7):723‐31. [DOI] [PubMed] [Google Scholar]
Buchvald 2002 {published data only}
- Buchvald FF, Bisgaard H. Comparison of add‐on of leukotriene receptor antagonist vs. long‐acting beta 2‐agonist of FeNO in asthmatic children on regular inhaled budesonide. European Respiratory Journal 2002;20(Suppl 38):431s. [Google Scholar]
Buhl 2004 {published data only}
- Buhl R, Kardos P, Richter K, Meyer‐Sabellek W, Bruggenjurgen B, Willich SN, et al. The effect of adjustable dosing with budesonide/formoterol on health‐related quality of life and asthma control compared with fixed dosing. Current Medical Research and Opinion 2004;20(8):1209‐20. [DOI] [PubMed] [Google Scholar]
Caffey 2005 {published data only}
- Caffey LF, Raissy HH, Marshik P, Kelly HW. A crossover comparison of fluticasone propionate and montelukast on inflammatory indices in children with asthma. Pediatric Asthma Allergy and Immunology 2005;18(3):123‐30. [Google Scholar]
Chen 2010 {published data only}
- Chen R, Chen M, Xiong J, Yi F, Chi Z, Zhang B. Comparison of heat‐sensitive moxibustion versus fluticasone/salmeterol (seretide) combination in the treatment of chronic persistent asthma: design of a multicenter randomized controlled trial. Trials 2010;11:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chopra 2005 {published data only}
- Chopra N, Williams M, Rimmer M, Kahl L, Jenkins M, SMO30006 International Study Teams, et al. Salmeterol HFA is as effective as salmeterol CFC in children and adults with persistent asthma. Respiratory Medicine 2005;99(SUPPL 1):S1‐S10. [DOI] [PubMed] [Google Scholar]
Chuchalin 2005 {published data only}
- Chuchalin A, Kasl M, Bengtsson T, Nihlen U, Rosenborg J. Formoterol used as needed in patients with intermittent or mild persistent asthma. Respiratory Medicine 2005;99(4):461‐70. [DOI] [PubMed] [Google Scholar]
Corren 2013 {published data only}
Covar 2008 Oct {published data only}
- Covar RA, Szefler SJ, Zeiger RS, Sorkness CA, Moss M, Mauger DT, et al. Factors associated with asthma exacerbations during a long‐term clinical trial of controller medications in children. Journal of Allergy and Clinical Immunology 2008 Oct;122(4):741‐47.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cowan 2004 {published data only}
- Cowan S, Ernst P, Cartier A, Boulet LP. A population‐based evaluation of a regional asthma education centre. Canadian Respiratory Journal 2004;11(1):39‐44. [DOI] [PubMed] [Google Scholar]
Daviskas 2005 {published data only}
- Daviskas E, Anderson SD, Shaw J, Eberl S, Seale JP, Yang IA, et al. Mucociliary clearance in patients with chronic asthma: effects of beta agonists. Respirology 2005;10(4):426‐35. [DOI] [PubMed] [Google Scholar]
Delaronde 2005 {published data only}
- Delaronde S, Peruccio DL, Bauer BJ. Improving asthma treatment in a managed care population. American Journal of Managed Care 2005;11(6):361‐8. [PubMed] [Google Scholar]
Drummond 2011 {published data only}
- Drummond MB, Peters SP, Castro M, Holbrook JT, Irvin CG, Smith LJ, et al. Risk factors for montelukast treatment failure in step‐down therapy for controlled asthma. Journal of Asthma 2011;48(10):1051‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dubus 2003 {published data only}
- Dubus JC, Mely L, Huiart L, Marguet C, Roux P, Reseau de Recherche Clinique en Pneumologie Pediatrique. Cough after inhalation of corticosteroids delivered from spacer devices in children with asthma. Fundamental and Clinical Pharmacology 2003;17(5):627‐31. [DOI] [PubMed] [Google Scholar]
Emeryk 2003 {published data only}
- Emeryk A, Bracamonte T, Schauer U, Balsara S, Athisegaran R. Efficacy of salmeterol/fluticasone propionate (50/100mcg/day) delivered via the Diskus and MDi in children with asthma [Abstract]. European Respiratory Journal 2003;22(Suppl 45):Abstract No: [P1985]. [Google Scholar]
Everden 2004 {published data only}
- Everden P, Campbell M, Harnden C, McGoldrick H, Bodalia B, Manion V, et al. Eformoterol Turbohaler compared with salmeterol by dry powder inhaler in asthmatic children not controlled on inhaled corticosteroids. Pediatric Allergy and Immunology 2004;15(1):40‐7. [DOI] [PubMed] [Google Scholar]
Fardon 2005 {published data only}
- Fardon TC, Lee DK, Hodge MR, Lipworth BJ. Addition of fexofenadine to inhaled corticosteroid therapy to reduce inflammatory biomarkers in atopic asthma. Annals of Allergy, Asthma, and Immunology 2005;95(3):259‐65. [DOI] [PubMed] [Google Scholar]
Grady 1995 {published data only}
- Grady J, Dockhorn R, Blake K. Effects of inhaled salmeterol powder in adult and adolescent asthmatics using concurrent inhaled corticosteroids [abstract]. European Respiratory Journal 1995;8(Suppl 19):2S. [Google Scholar]
Holgate 2004 {published data only}
- Holgate ST, Chuchalin AG, Hebert J, Lotvall J, Persson GB, Chung KF, et al. Efficacy and safety of a recombinant anti‐immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clinical and Experimental Allergy 2004;34(4):632‐8. [DOI] [PubMed] [Google Scholar]
Holt 2005 {published data only}
- Holt S, Ryder‐Lewis S, Masoli M, Weatherall M, Beasley R. Fixed and adjustable dose asthma action plans based on combination therapy: a pilot study. Respirology 2005;10(4):497‐503. [DOI] [PubMed] [Google Scholar]
Ilowite 2004 {published data only}
- Ilowite J, Webb R, Friedman B, Kerwin E, Bird SR, Hustad CM, et al. Addition of montelukast or salmeterol to fluticasone for protection against asthma attacks: a randomized, double‐blind, multicenter study. Annals of Allergy, Asthma, and Immunology 2004;92(6):641‐8. [DOI] [PubMed] [Google Scholar]
Jenkins 2005 {published data only}
- Jenkins CR, Thien FCK, Wheatley JR, Reddel HK. Traditional and patient‐centred outcomes with three classes of asthma medication. European Respiratory Journal 2005;26(1):36‐44. [DOI] [PubMed] [Google Scholar]
Karaman 2007 {published data only}
- Karaman O, Arli O, Uzuner N, Islekel H, Babayigit A, Olmez D, et al. The effectiveness of asthma therapy alternatives and evaluating the effectivity of asthma therapy by interleukin‐13 and interferon gamma levels in children. Allergy and Asthma Proceedings 2007;28(2):204‐9. [DOI] [PubMed] [Google Scholar]
Katial 2011 Mar {published data only}
Kerwin 2008 Apr {published data only}
- Kerwin EM, Nathan RA, Meltzer EO, Ortega HG, Yancey SW, Schoaf L, et al. Efficacy and safety of fluticasone propionate/salmeterol 250/50 mcg Diskus administered once daily. Respiratory Medicine 2008 Apr;102(4):495‐504. [DOI] [PubMed] [Google Scholar]
Lara‐Perez 2005 {published data only}
- Lara‐Perez EA. Emprovement of the asthma in children using salmeterol and fluticasone (Seretide) in inhaled combination [Abstract]. XIX World Allergy Organization Congress. 2005:Abstract 861.
Levy 2005 {published data only}
- Levy R, Pinnas J, Milgrom H, Smith J, Yegen U. Safety and efficacy in children with persistent asthma treated with formoterol 10 mug BID delivered via Certihaler: a novel multidose dry‐powder inhaler. Pediatric Asthma Allergy and Immunology 2005;18(1):25‐35. [Google Scholar]
Li 2010 {published data only}
- Li JS, Qaqundah PY, Weinstein SF, Laforce CF, Ellsworth AV, Ortega HG, et al. Fluticasone propionate/salmeterol combination in children with asthma: key cardiac and overall safety results. Clinical Research and Regulatory Affairs 2010;27(3):87‐95. [Google Scholar]
Lipworth 2013 {published data only}
- Lipworth BJ, Basu K, Donald HP, Tavendale R, Macgregor DF, Ogston SA, et al. Tailored second‐line therapy in asthmatic children with the Arg(16) genotype. Clinical Science 2013;124(8):521‐8. [DOI] [PubMed] [Google Scholar]
LOCCS {published data only}
- American Lung Association Asthma Clinical Research. Randomized comparison of strategies for reducing treatment in mild persistent asthma. New England Journal of Medicine 2007;356(20):2027‐39. [DOI] [PubMed] [Google Scholar]
Lundbäck 2009 Mar {published data only}
Makela 2012 {published data only}
- Makela MJ, Malmberg LP, Csonka P, Klemola T, Kajosaari M, Pelkonen AS. Salmeterol and fluticasone in young children with multiple‐trigger wheeze. Annals of Allergy, Asthma & Immunology 2012;109(1):65‐70. [DOI] [PubMed] [Google Scholar]
Matthys 2004 {published data only}
- Matthys H, Behling B, Behling E. Comparison of formoterol (12 and 6 mug b.i.d.) versus terbutaline (0.5 mg b.i.d.) with equal doses of inhaled budesonide (0.2 mg b.i.d.) in 246 children with mild to moderate asthma. Atemwegs Und Lungenkrankheiten 2004;30(5):251‐6. [Google Scholar]
Miraglia 2007 {published data only}
- Miraglia del Giudice M, Capristo M, Amelio R, Rocco A, Fusco N, et al. Combined fluticasone propionate/salmeterol (diskus) vs fluticasone propionate (Diskus) in the control of persistent asthma in children. American Thoracic Society 99thInternational Conference; 2003 May 16‐21; Seattle. 2003:A117 Poster D78.
- Miraglia del Giudice M, Piacentini GL, Capasso M, Capristo C, Maiello N, Boner AL, et al. Formoterol, montelukast, and budesonide in asthmatic children: effect on lung function and exhaled nitric oxide. Respiratory Medicine 2007;101(8):1809‐13. [DOI] [PubMed] [Google Scholar]
Mitchell 2005 {published data only}
- Mitchell EA, Didsbury PB, Kruithof N, Robinson E, Milmine M, Barry M, et al. A randomized controlled trial of an asthma clinical pathway for children in general practice. Acta Paediatrica 2005;94(2):226‐33. [DOI] [PubMed] [Google Scholar]
Mitra 2003 {published data only}
- Mitra A, Sims EJ, Mukhopadhyay S, Lipworth BJ. Low‐dose inhaled corticosteroid (ICS) confers optimal anti‐inflammatory effects while additional bronchodilator activity is afforded by salmeterol in mild persistent asthmatic children [Abstract]. Journal of Allergy and Clinical Immunology 2003;111(2 Suppl):S145. [Google Scholar]
Morice 2005 {published data only}
- Morice AH, Hochmuth L, Puterman A, Artheden L, Beckman O. Comparable safety of a novel budesonide/formoterol pMDI versus budesonide/formoterol Turbuhaler in adolescents and adults with asthma [Abstract]. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S3. [Google Scholar]
Morice 2005a {published data only}
- Morice AH, Osmanliev D, Arheden L, Beckman O. Therapeutic equivalence of a novel budesonide/formoterol pMDI versus budesonide/formoterol Turbuhaler in adolescents and adults with asthma [Abstract]. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S2. [Google Scholar]
Morice 2008 {published data only}
- Morice AH, Hochmuth L, Ekelund J, Thorén A, Puterman AS. Comparable long‐term safety and efficacy of a novel budesonide/formoterol pressurized metered‐dose inhaler versus budesonide/formoterol Turbuhaler in adolescents and adults with asthma. Pulmonary Pharmacology & Therapeutics 2008;21(1):32‐9. [DOI] [PubMed] [Google Scholar]
Murray 2004 {published data only}
- Murray J, Rosenthal R, Somerville L, Blake K, House K, Baitinger L, et al. Fluticasone propionate and salmeterol administered via Diskus compared with salmeterol or fluticasone propionate alone in patients suboptimally controlled with short‐acting beta2‐agonists. Annals of Allergy, Asthma, & Immunology 2004;93(4):351‐9. [DOI] [PubMed] [Google Scholar]
Nathan 2005 {published data only}
- Nathan RA, Yancey SW, Waitkus‐Edwards K, Prillaman BA, Stauffer JL, Philpot E, et al. Fluticasone propionate nasal spray is superior to montelukast for allergic rhinitis while neither affects overall asthma control. Chest 2005;128(4):1910‐20. [DOI] [PubMed] [Google Scholar]
Nelson 2006 {published data only}
- Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM, SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006;129(1):15‐26. [DOI] [PubMed] [Google Scholar]
Nguyen 2005 {published data only}
- Nguyen WT, Stewart C, Fisher K, Tolley E, Lew DB, Self TH. Maintenance asthma treatment with fluticasone/salmeterol combination via diskus: effect on outcomes in inner‐city children enrolled in Tenncare. Allergy and Asthma Proceedings 2005;26(2):129‐34. [PubMed] [Google Scholar]
Noyes 2013 {published data only}
- Noyes K, Bajorska A, Fisher S, Sauer J, Fagnano M, Halterman JS. Cost‐effectiveness of the School‐Based Asthma Therapy (SBAT). Pediatrics 2013; Vol. 131, issue 3:e709‐17. [DOI] [PMC free article] [PubMed]
O'Byrne 2001 {published data only}
- Barnes PJ, O'Byrne PM, Rodriguez‐Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Oxis and Pulmicort turbuhaler in the management of asthma OPTIMA international study group. Treatment of mild persistent asthma with low doses of inhaled Budesonide alone or in combination with Formoterol. Thorax 2000;55(Suppl 3):A4. [Google Scholar]
- Barnes PJ, O'Byrne PM, Rodriguez‐Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. For the Oxis and Pulmicort Turbuhaler in the Management of Asthma (OPTIMA) international study group. Thorax 2000; Vol. 55, issue Suppl 3:s5.
- Bisgaard H, Hultquist C. Budesonide/formoterol for maintenance and as needed ‐ a new approach to asthma management in children [Abstract]. European Respiratory Journal 2005;26(Suppl 49):Abstract No. 1060. [Google Scholar]
- Jönsson BG, Berggren FE, Svensson K, O'Byrne PM. Budesonide and formoterol in mild persistent asthma compared with doubling the dose of budesonide ‐ a cost‐effectiveness analysis. European Respiratory Journal 2001; Vol. 18, issue Suppl 33:517s.
- Jönsson BG, Berggren FE, Svensson K, O'Byrne PM. Economic results of adding formoterol to budesonide in mild persistent asthma. European Respiratory Journal 2001; Vol. 18, issue Suppl 33:331s.
- O'Byrne PM, Barnes PJ, Rodriguez‐Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. American Journal of Respiratory & Critical Care Medicine 2001;164(8 pt 1):1392‐7. [DOI] [PubMed] [Google Scholar]
- O'Byrne PM, Barnes PJ, Rodriguez‐Roisin R, Sandtröm T, Tattersfield AE, Runnerström EM, et al. Addition of formoterol Turbuhaler® to budesonide Tubuhaler® is safe and well tolerated in the long‐term treatment of mild asthma: results from the OPTIMA trial. European Respiratory Journal 2001;18(Suppl 33):330s. [Google Scholar]
Pearlman 2004 {published data only}
- Pearlman DS, Peden D, Condemi JJ, Weinstein S, White M, Baitinger L, et al. Efficacy and safety of fluticasone propionate/salmeterol HFA 134A MDI in patients with mild‐to‐moderate persistent asthma. Journal of Asthma 2004;41(8):797‐806. [DOI] [PubMed] [Google Scholar]
Peroni 2005 {published data only}
- Peroni DG, Piacentini GL, Bodini A, Ress M, Costella S, Boner AL. Montelukast versus formoterol as second‐line therapy in asthmatic children exposed to relevant allergens. Allergy & Asthma Proceedings 2005;26(4):283‐6. [PubMed] [Google Scholar]
Peters 2008 Sep‐Oct {published data only}
Pijnenburg 2005 {published data only}
- Pijnenburg MW, Bakker EM, Hop WC, Jongste JC. Titrating steroids on exhaled nitric oxide in children with asthma: a randomized controlled trial. American Journal of Respiratory & Critical Care Medicine 2005;172(7):831‐6. [DOI] [PubMed] [Google Scholar]
Prates 2009 {published data only}
- Covar RA, Szefler SJ, Zeiger RS, Sorkness CA, Moss M, Mauger DT. Factors associated with asthma exacerbations during a long‐term clinical trial of controller medication in children. Journal of Allergy and Clinical Immunology 2008;122(4):741‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Price 2011 May {published data only}
- Price D, Musgrave SD, Shepstone L, Hillyer EV, Sims EJ, Gilbert RF, et al. Leukotriene antagonists as first‐line or add‐on asthma‐controller therapy. New England Journal of Medicine 2011 May;364(18):1695‐707. [DOI] [PubMed] [Google Scholar]
Prieto 2005 {published data only}
- Prieto L, Gutierrez V, Perez‐Frances C, Badiola C, Lanuza A, Bruno L, et al. Effect of fluticasone propionate‐salmeterol therapy on seasonal changes in airway responsiveness and exhaled nitric oxide levels in patients with pollen‐induced asthma. Annals of Allergy, Asthma, & Immunology 2005;95(5):452‐61. [DOI] [PubMed] [Google Scholar]
Quirce 2011 Oct {published data only}
Reddel 2010 Aug {published data only}
Renzi 2005 {published data only}
- Renzi PM, Frassen E, Stat P, Watson EG. Salmeterol/fluticasone propionate diskus (ADVAIR) 50/100mcg bid improves asthma outcomes compared with fluticasone propionate (FLOVENT) diskus 100mcg bid when used as initial maintenance treatment in adult and adolescent subjects with symptomatic persistent asthma [Abstract]. American Thoracic Society 2005 International Conference; May 20‐25; San Diego. 2005:[C33] [Poster: F65].
Renzi 2010 Apr {published data only}
SAM30002 {unpublished data only}
- SAM30002 (GSK). A randomised, double blind, double‐dummy, parallel‐group, twelve week comparison of salmeterol/fluticasone propionate (FP) DISKUS/ACCUHALER 50/100mcg bd. with budesonide 200mcg bd. plus formoterol 4.5mcg bd. (both by breath‐activated dry powder inhaler [BADPI]) in adult and adolescent asthmatics. http://www.gsk‐clinicalstudyregister.com/study/SAM30002#rs (accessed 13 May 2015).
SAM40101 {unpublished data only}
- Glaxo Smith Kline. A pilot single centre, randomised, double‐blind, crossover study to demonstrate the superiority of Salmeterol/fluticasone propionate combination product 50/100mcg bd versus fluticasone propionate 100mcg bd when treated for two weeks with respect to activity levels in children aged 7‐15 years. http://ctr.gsk.co.uk (accessed 4 January 2008) 2006.
SAS30021 {unpublished data only}
- SAS30021. A stratified, randomized, double‐blind, placebo‐controlled, parallel‐group, 12‐week trial evaluating the safety and efficacy of the fluticasone propionate/salmeterol DISKUS combination product 100/50mcg once daily versus fluticasone propionate DISKUS 100mcg once daily and placebo in symptomatic pediatric subjects (4‐11 years) with asthma. http://www.gsk‐clinicalstudyregister.com/study/SAS30021#ps (accessed 28 April 2008).
Schauer 2003 {published data only}
- Schauer U, Bracamonte T, Emeryk A, Balsara S, Athisegaran R. Clinical equivalence of salmeterol/fluticasone propionate combination 50/100mcg BID delivered via Diskus or CFC ‐ free metered dose inhaler (MDI) in children with asthma [Abstract]. European Respiratory Journal 2003;22(Suppl 45):Abstract No: [P1986]. [Google Scholar]
Scicchitano 2004a {published data only}
- Scicchitano R, Aalbers R, Ukena D, Manjra A, Fouquert L, Centann S, et al. Efficacy and safety of budesonide/formoterol single inhaler therapy versus a higher dose of budesonide in moderate to severe asthma. Current Medical Research & Opinion 2004;20(9):1403‐18. [DOI] [PubMed] [Google Scholar]
Selroos 2004 {published data only}
- Selroos O, Lofroos AB, Pietinalho A, Riska H. Asthma control and steroid doses 5 years after early or delayed introduction of inhaled corticosteroids in asthma: a real‐life study. Respiratory Medicine 2004;98(3):254‐62. [DOI] [PubMed] [Google Scholar]
SFCF3001 {unpublished data only}
- SFCF3001. A multicentre, randomised, double‐blind, double‐dummy, parallel‐group study to establish equivalence of the salmeterol/fluticasone propionate combination product (50/250µg) via either the reservoir powder inhalation device (RPID) or via the Diskus Inhaler over 12 weeks in adolescents and adults with moderate asthma. http://www.gsk‐clinicalstudyregister.com/study/RPS30002/SFCF3001#rs (accessed 13 May 2015).
SFCF3002 {unpublished data only}
- SFCF3002 (GSK). A multicentre, randomised, double‐blind, double‐dummy, parallel‐group study to establish equivalence of the fluticasone propionate/salmeterol combination (FSC) product (100/50µg) via either the reservoir powder inhalation device (RPID) or via the Diskus inhaler over 12 weeks in children with asthma. http://www.gsk‐clinicalstudyregister.com/study/RPS30001/SFCF3002#rs (accessed 13 May 2015).
Sienra‐Monge 2004 {published data only}
- Sienra‐Monge JJL, Rio‐Navarro BE, Alvarez‐Amador M, Blandon‐Vijil V, Gomez Chico‐Velasco R. The quality of life of the asthmatic child caregiver. Gaceta Medica De Mexico 2004;140(2):139‐45. [PubMed] [Google Scholar]
Soes‐Petersen 2011 Jul {published data only}
- Soes‐Petersen U, Kava T, Dahle R, Lei Y, Dam N. Budesonide/formoterol maintenance and reliever therapy versus conventional best standard treatment in asthma in an attempted 'real life' setting. Clinical Respiratory Journal 2011;5(3):173‐82. [DOI] [PubMed] [Google Scholar]
Sorkness 2007 {published and unpublished data}
- Sorkness CA, Lemanske Jr RF, Mauger DT, Boehmer SJ, Chinchilli VM, Martinez FD, et al. Long‐term comparison of 3 controller regimens for mild‐moderate persistent childhood asthma: The Pediatric Asthma Controller Trial. Journal of Allergy & Clinical Immunology 2007;119(1):64‐72. [DOI] [PubMed] [Google Scholar]
Spector 2012 {published data only}
Stelmach 2008a {published data only}
- Stelmach I, Grzelewski T, Jerzynska J, Kuna P. A randomized, double‐blind trial on the effect of treatment with montelukast, budesonide, montelukast with budesonide, formoterol with budesonide on lung function and clinical symptoms in children with asthma [Abstract]. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S151. [Google Scholar]
- Stelmach I, Grzelewski T, Majak P, Jerzynska J, Stelmach W, Kuna P. Effect of different antiasthmatic treatments on exercise‐induced bronchoconstriction in children with asthma. Journal of Allergy and Clinical Immunology 2008;121(2):383‐9. [DOI] [PubMed] [Google Scholar]
Storms 2004 {published data only}
- Storms W, Chervinsky P, Ghannam AF, Bird S, Hustad CM, Edelman JM, et al. A comparison of the effects of oral montelukast and inhaled salmeterol on response to rescue bronchodilation after challenge. Respiratory Medicine 2004;98(11):1051‐62. [DOI] [PubMed] [Google Scholar]
van den Toorn 2005 {published data only}
- Toorn LM, Prins JB, Jongste JC, Leman K, Mulder PG, Hoogsteden HC, et al. Benefit from anti‐inflammatory treatment during clinical remission of atopic asthma. Respiratory Medicine 2005;99(6):779‐87. [DOI] [PubMed] [Google Scholar]
Vogelmeier 2005 {published data only}
- Vogelmeier C, D'Urzo A, Pauwels R, Merino JM, Jaspal M, Boutet S, et al. Budesonide/formoterol maintenance and reliever therapy: an effective asthma treatment option?. European Respiratory Journal 2005;26(5):819‐28. [DOI] [PubMed] [Google Scholar]
Von Berg 2003 {published data only}
- Berg A, Papageorgiou Saxoni F, Wille S, Carrillo T, Kattamis C, Helms PJ. Efficacy and tolerability of formoterol turbuhaler in children. International Journal of Clinical Practice 2003;57(10):852‐6. [PubMed] [Google Scholar]
Weiler 2005 {published data only}
- Weiler JM, Nathan RA, Rupp NT, Kalberg CJ, Emmett A, Dorinsky PM. Effect of fluticasone/salmeterol administered via a single device on exercise‐induced bronchospasm in patients with persistent asthma. Annals of Allergy, Asthma and Immunology 2005;94(1):65‐72. [DOI] [PubMed] [Google Scholar]
You‐Ning 2005 {published data only}
- You‐Ning L, Humphries M, Du X, Wang L, Jiang J. Efficacy and safety of salmeterol/fluticasone propionate delivered via a hydrofluoroalkane metered dose inhaler in Chinese patients with moderate asthma poorly controlled with inhaled corticosteroids. International Journal of Clinical Practice 2005;59(7):754‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Adams 2005
- Adams NP, Bestall JC, Malouf R, Lasserson TJ, Jones P. Beclomethasone versus placebo for chronic asthma. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD002738.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Adams 2008a
- Adams NP, Bestall JC, Lasserson TJ, Jones P, Cates CJ. Fluticasone versus placebo for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD003135.pub4] [DOI] [Google Scholar]
Adams 2008b
- Adams NP, Bestall JC, Jones P, Lasserson TJ, Griffiths B, Cates CJ. Fluticasone at different doses for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD003534.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2008
- Bateman E, Nelson H, Bousquet J, Kral K, Sutton L, Ortega H, et al. Meta‐analysis: effects of adding salmeterol to inhaled corticosteroids on serious asthma‐related events. Annals of Internal Medicine 2008;149(1):33‐42. [DOI] [PubMed] [Google Scholar]
Bisgaard 2003
- Bisgaard H. Effect of long‐acting β2 agonists on exacerbation rates of asthma in children. Pediatric Pulmonology 2003;36:391‐8. [DOI] [PubMed] [Google Scholar]
BTS 2014
- British Thoracic Society and Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma. A national clinical guideline (Revised January 2014). http://sign.ac.uk/pdf/SIGN141.pdf (accessed 14 May 2015).
CAMP Research Group 2012
- Kelly HW, Sternberg AL, Lescher R, Fuhlbrigge AL, Williams P, Zeiger RS. Effect of inhaled glucocorticoids in childhood on adult height. New England Journal of Medecine 2012;367(10):904‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cates 2008a
- Cates CJ, Cates MJ. Regular treatment with salmeterol for chronic asthma: serious adverse events. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD006363.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cates 2009a
- Cates CJ, Lasserson TJ, Cates MJ. Regular treatment with formoterol and inhaled steroids for chronic asthma: serious adverse events. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006924.pub2] [DOI] [PubMed] [Google Scholar]
Cates 2009b
- Cates CJ, Cates MJ, Lasserson TJ. Regular treatment with salmeterol and inhaled steroids for chronic asthma: serious adverse events. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD006922.pub2] [DOI] [PubMed] [Google Scholar]
Cates 2012
- Cates CJ, Oleszczuk M, Stovold E, Wieland LS. Safety of regular formoterol or salmeterol in children with asthma: an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD010005.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chauhan 2012
- Chauhan BF, Ducharme FM. Anti‐leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD002314.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chauhan 2014
- Chauhan BF, Ducharme FM. Addition to inhaled corticosteroids of long‐acting beta2‐agonists versus anti‐leukotrienes for chronic asthma. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD003137.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Ducharme 2010
- Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long‐acting beta2‐agonists to inhaled corticosteroids versus same dose inhaled corticosteroids for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD005535.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ducharme 2010a
- Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long‐acting beta2‐agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD005533.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
GINA 2015
- Global Initiative for Asthma. From the Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2015. http://www.ginasthma.org (accessed 14 May 2015).
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(557):560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration. www.cochrane‐handbook.org, 2011. [Google Scholar]
Lougheed 2012
- Lougheed MD, Lemiere C, Ducharme FM, Licskai C, Dell SD, Rowe BH, et al. Canadian Thoracic Society Asthma Management Continuum—2010 Consensus Summary for children six years of age and over, and adults. Canadian Respiratory Journal 2012;19(2):127‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manning 2008
- Manning P, Gibson PG, Lasserson TJ. Ciclesonide versus placebo for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD006217.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
NAC Guidelines 2014
- National Asthma Council, Australia. Asthma Management Handbook. www.nationalasthma.org.au (accessed 8 May 2015) 2014.
NAEPP 2011
- National Asthma Education and Prevention Program. NAEPP Expert Panel Report Guidelines for the Diagnosis and Management of Asthma. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf (accessed 13 January 14).
NCT01462344
- NCT01462344. 6‐Month Safety and Benefit Study of ADVAIR in Children 4‐11 Years Old (VESTRI). clinicaltrials.gov (accessed 8 May 2015).
Pruteanu 2014
- Pruteanu A, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: dose‐response effects on growth. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858.CD009878.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager (RevMan) [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sharek 1999
- Sharek PJ, Bergman DA, Ducharme F. Beclomethasone for asthma in children: effects on linear growth. Cochrane Database of Systematic Reviews 1999, Issue 3. [DOI: 10.1002/14651858.CD001282] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skoner 2000
- Skoner DP, Rachelefsky GS, Meltzer EO, Chervinsky P, Morris RM, Seltzer JM, et al. Detection of growth suppression in children during treatment with intranasal beclomethasone dipropionate. Pediatrics 2000;105(2):e23. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ni Chroinin 2009
- Ni Chroinin M, Lasserson TJ, Greenstone I, Ducharme FM. Addition of long‐acting beta‐agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007949] [DOI] [PMC free article] [PubMed] [Google Scholar]


