Abstract
Objectives
This study aimed to explore psychological distress, lifestyle, and demographic factors, as well as their relationship to discretionary choices in women of reproductive age during the coronavirus disease 2019 pandemic in Australia.
Methods
Reproductive-aged women (18–50 y) in Australia participated in a national online survey. Psychological distress score (using a validated 10-item Kessler Psychological Distress Scale questionnaire) was the primary exposure of interest, and key outcomes were frequencies of discretionary choices (sugar-sweetened beverages [SSBs], alcohol, and discretionary foods). Sociodemographic and physical activity data were also collected. Logistic regression was used to report adjusted odds ratio (aOR) and 95% confidence interval to predict SSBs (less than weekly; most days/daily), total discretionary foods (none/<2 times/d; ≥3 times/d), and alcohol use (never/less than monthly; most weeks/daily).
Results
A total of 1005 women were included in the study, of whom 40% had a high level of psychological distress. Women with high psychological distress (aOR: 1.96; 95% CI, 1.32–2.91) and those who gained weight during the pandemic (aOR: 1.71; 95% CI, 1.10–2.65) were more likely to consume discretionary foods ≥3 times/d. There was no association between psychological distress and SSB intake or alcohol; however, Australian, New Zealander, or Pacific Islander background (aOR: 1.68; 95% CI, 1.21–2.33) and more hours of sitting time (aOR: 1.88; 95% CI, 1.07–3.29) were associated with SSB consumption on most days/daily. Older age (aOR: 1.70; 95% CI, 1.00–2.89), higher household income (aOR: 1.44; 95% CI, 1.08–1.92), and moderate or high physical activity (aOR: 1.75; 95% CI, 1.10–2.80) were associated with alcohol intake on most weeks/daily.
Conclusions
Public health messaging to promote healthy eating should take into account the effect of psychological distress on health behavior. Messages aimed at maintaining a positive relationship between food intake and mental wellbeing, particularly among vulnerable groups, are warranted.
Keywords: Discretionary food, Psychological distress, COVID-19, Sugar-sweetened beverage, Alcohol
Introduction
The current COVID-19 pandemic is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus type 2, and was identified first in Wuhan, China in December 2019. COVID-19 was declared a global pandemic by the World Health Organization in March 2020. In Australia, the virus first peaked across numerous states in the first quarter of 2020 [1].
During the pandemic, social distancing and lockdown restrictions affected a range of behavioral factors. In particular, the public health emergencies resulting from COVID-19 negatively affected mental health and psychological distress [2,3]. In the United States, levels of psychological distress were higher during the pandemic compared with two years prior [4]. In the United Kingdom, higher levels of anxiety (21%–37%) were reported during the pandemic in 2020 compared with 2019 [5]. Data from Australian surveys conducted during the pandemic found that around one-fifth of 320 health care workers self-reported moderate-to-severe symptoms of depression, anxiety, and posttraumatic stress disorder [6], with significantly higher scores in one or more psychological distress states found for women and those age 18 to 45 y [7]. The social effect of the COVID-19 pandemic has also been considerable, including employment instability, financial insecurity, increased isolation, loneliness, fear, anxiety, and depression [8].
A recurring finding in cross-sectional studies is that women are most greatly affected physically and psychologically by the COVID-19 pandemic compared with men [9,10]. In addition to having worse mental health [11,12], women across the reproductive age group also face challenges with diet, physical activity [13], and household food insecurity [14]. Furthermore, changes in behavioral factors during the COVID-19 pandemic and lockdown include increased intake of total food consumption, decreased adherence to a healthy diet, and increased snacking [15]. Additionally, food intake was reportedly increased because of emotional eating as a means of comfort and to feel better in response to anxious states [16,17], with higher levels of this reported behavior in women [16].
Given the effect of COVID-19 social distancing and isolation measures, along with the far-reaching economic consequences, exploring lifestyle factors in women of reproductive age is important. Moreover, the indication that discretionary choices increased during the pandemic presents the need to better understand relationships between discretionary choices and psychological stress. Therefore, this study aimed to explore psychological distress, lifestyle, and demographic factors and their relationship with discretionary choices in women of reproductive age (18–50 y) during the COVID-19 pandemic in Australia.
Methods
Study design and population
This study was an Australia-wide cross-sectional study using data collected through an anonymous online survey between October 15 and November 7, 2020 (Suppl. File 1). At this time, Victoria was in their second lockdown, and restrictions were easing throughout the rest of Australia. The survey was designed to explore food insecurity, diet and physical activity behaviors, weight changes, psychological distress, and infant feeding during the COVID-19 pandemic. Women of reproductive age (18–50 y) who resided in Australia were invited via e-mail to complete an online survey, including a series of multiple-choice and short-answer questions. E-mails were sent to women by a cross-panel market research provider (Online Research Unit) with a well-established database of 400 000 members until the target sample size was reached. There are approximately 5 million women in Australia age 15 to 50 y; thus, to conduct a survey with an approximate margin of error of 1% with a 99% confidence interval (CI), a sample size of approximately 1000 responses was required.
To ensure the study population was broadly representative of women in the Australian population according to the Australian Bureau of Statistics by age and location of residence (state/territory), these demographic characteristics of the study population were examined on days 4 and 5 after recruitment commenced to allow for targeted recruitment of underrepresented groups [18]. Although the resulting sample may not be representative across all population characteristics, this approach is widely accepted to obtain a sample broadly consistent with population proportions on predefined characteristics [19].
After online consent, participants were asked to complete the anonymous 10-min online survey and were reimbursed in line with ISO 26362 and industry requirements. The study was approved by the Monash University Human Research Ethics Committee (MUHREC project: 25941).
Assessment of population characteristics
The survey included multiple-choice or short-answer questions to assess participant age group, residential location (state/territory), cultural or ethnic background, the highest level of completed education, employment status before the pandemic, changes in employment status since the pandemic, living circumstances, and annual household income before tax. The level of lockdown restriction was determined based on metropolitan versus regional areas during the 3 mo leading up to the survey [20]. Self-reported height and weight were used to calculate body mass index (BMI) and categorized as underweight (<18.5 kg/m2), normal weight (18.5–25 kg/m2), overweight (25–29.9 kg/m2), or obese (≥30 kg/m2).
Dietary survey questions were developed based on the Irish National COVID-19 Food Survey and adapted to Australian settings using the Australian Guide to Healthy Eating to collect information on the consumption of sugar-sweetened beverages (SSBs), alcohol, and total discretionary foods. The frequency of discretionary food intake was obtained through multiple choice questions of 1 to 2 times per day, 3 to 5 times per day, 5 to 7 times per day, 7 to 10 times per day, >10 times per day, do not eat every day, never, and I do not know. Frequency of discretionary foods was then binary coded into none/<2 times per day (i.e., never, do not eat every day, and 1–2 times/d) and ≥3 times/d (i.e., 3–5, 5–7, 7–10, or >10 times/d) to align with the Australian Guide to Healthy Eating discretionary food recommendations for women of <2.5 times per day [21,22].
The frequency of SSB intake was obtained using multiple-choice options: <1 time per week, 1 to 3 times per week, 4 to 6 times per week, more than once a day, never, and I do not know. SSB frequency was then binary coded into less than weekly (i.e., never and <1 time/wk) and most days/daily (i.e., 1–3 or 4–6 times/wk, more than once a day) based on median intake. Frequency of alcohol consumption was obtained through multiple-choice options (2–3 times/wk, 2–4 times/wk, ≥4 times/mo, monthly or less, never, and I do not know/prefer not to answer), and collapsed into never/less than monthly (i.e., never and monthly or less) and most weeks/daily (i.e., 2–4 times/mo, 2–3 or ≥4 times/wk). Responses of I do not know or I prefer not to answer were excluded from the binomial logistic regression. Fruit and vegetables serving numbers were self-reported (as continuous variables) with outliers deemed as values >3 times the 75th percentile, as per Yaroch et al. [23], and later replaced with an imputed value.
Physical and sedentary activity
The Active Australia Survey, a validated questionnaire on physical activity and sedentary behavior, was used to assess frequency of physical and sedentary activity [24]. Women were asked to report the frequency and total minutes spent during the last week on walking briskly, moderate and vigorous leisure activities, and vigorous household or garden chores. Physical activity outliers were identified by summing total moderate leisure and vigorous leisure frequencies, and marked as missing if the sum was >56 occasions. Total metabolic minutes per week (MET.min/wk) was calculated by summing the products of each type of physical activity with its metabolic equivalent value (MET.min/wk = [weekly walking minutes × 3.33] + [weekly moderate leisure minutes × 3.33] + [weekly vigorous leisure × 6.66] + [weekly vigorous chores × 6.66]) [25]. Total MET.min/wk were categorized as none or very low (<33.3 MET.min/wk), low (33.3–500 MET.min/wk), moderate (500–1000 MET.min/wk), or high (≥1000 MET.min/wk) level of physical activity categories [26].
Sedentary behavior was defined by the total duration (h/min/d) of sitting time during transport, work, watching television, computer use, and other activities on work- and nonworkdays. The total time was categorized into quartiles of 0 to 3, 4 to 7, 8 to 11, and 12 to 15 h. Any total sitting of h/min/d >16 h or 960 min were considered outliers and treated as missing data [27].
Psychological distress
Psychological distress level was assessed using the validated self-administered 10-item Kessler Psychological Distress Scale (K10) questionnaire. Individuals reported depressive and anxiety symptoms experienced during the last 4 wk with a five-level response: None of the time, a little of the time, some of the time, most of the time, and all the time. Total K10 score was obtained by summing the item responses [28], and binary coded as low (<22) or high (≥22) levels of psychological distress.
Statistical analyses
The data were analyzed using the R statistical software (R Core Team, 2020). Descriptive statistics were produced reporting the frequency of responses across key variables and mean (standard deviation [SD]) unless otherwise specified. Outliers were recoded as not applicable values for current height, current weight, and BMI based on biologically plausible height and weight ranges, as per Cheng et al. [29] (i.e., ≥111.8 cm and ≤228.6 cm [height], ≥24.9 kg and ≤453.6 kg [weight], and ≥12 and ≤70 BMI).
Missing data for the predictor variables were managed by using multiple imputations with the Multivariate Imputations by Chained Equation package in R [30]. We assumed that the data were missing at random. Patterns of missingness in the data were inspected before multiple imputations were computed. This procedure produced 30 imputed data sets with 10 iterations, each according to recommendations for the number of iterations [31]. All key variables associated with missingness were imputed in the imputation model, except for outcome variables. Similarly, outcome variables were not used as imputer variables. The Predictive Mean Matching algorithm from the Multivariate Imputations by Chained Equation R package was used to impute missing values, using a linear regression model to impute missing values for continuous variables (or logistic regression model for categorical variables) and a randomly generated value using observed data [32]. Categorical variables were recoded based on the imputed values (e.g., BMI categories using imputed current height and current weight values).
Logistic regression was used to report unadjusted and adjusted odds ratios to predict the following outcomes: SSBs (less than weekly; most days/daily), total discretionary foods (none/<2 times/d; ≥3 times/d), and alcohol (never/less than monthly; most weeks/daily). Univariate modelling included the following predictor variables: Psychological distress (K10), age, annual household income before tax (in AU$), ethnicity, BMI, weight status, employment status change, current living circumstances, lockdown restrictions, fruit portions number, vegetable portions number, physical activity category, and work- and nonworkday sitting hours categories (Table 1 ). Regression models were fitted to each of the imputed data sets, and model estimates were pooled using the rules by Rubin et al. [33] to provide an overall estimate. Variables selected to go into the multivariable regressions were sociodemographic and lifestyle variables related to food intake. An alpha level of 0.05 was used for statistical significance.
Table 1.
Sociodemographic and lifestyle characteristics of participants
| Characteristic | Frequency, n (%) |
|---|---|
| Age, y (n = 1005) | |
| 18–24 | 158 (15.7) |
| 25–34 | 349 (34.7) |
| 35–44 | 329 (32.7) |
| 45–50 | 169 (16.8) |
| State of residency (n = 1005) | |
| Queensland | 198 (19.7) |
| New South Wales | 311 (30.9) |
| Victoria | 278 (27.7) |
| Northern Territory | 3 (0.3) |
| Western Australia | 97 (9.7) |
| Tasmania | 29 (2.9) |
| South Australia | 68 (6.8) |
| Australian Capital Territory | 21 (2.1) |
| Ethnicity (n = 960) | |
| European or North American | 242 (25.2) |
| Australian, New Zealander, or Pacific Islander | 561 (58.4) |
| Other* | 31 (3.2) |
| Asian | 126 (13.1) |
| Annual household income before tax, AU$ (n = 865) | |
| 0–99 999 | 436 (50.4) |
| ≥100 000 | 429 (49.6) |
| Current living circumstances (n = 996) | |
| Own home | 492 (49.4) |
| Rented home or emergency accommodation | 306 (30.7) |
| Living with family | 198 (19.9) |
| Lockdown restrictions | |
| Yes (Metropolitan Melbourne) | 241 (24.0) |
| No | 764 (76.0) |
| Employment status change (n = 1004) | |
| Yes | 252 (25.1) |
| No | 752 (74.9) |
| Body mass index, kg/m2 (n = 716) | |
| <18.5 | 33 (4.6) |
| 18.5–25 | 384 (53.6) |
| 25–30 | 157 (21.9) |
| ≥30 | 142 (19.8) |
| Weight change status (n = 967) | |
| Stayed the same | 400 (41.4) |
| Gained | 400 (41.4) |
| Lost | 167 (17.3) |
| Physical activity, metabolic min/wk (n = 1003) | |
| <33.3 | 116 (11.6) |
| <500 | 310 (30.9) |
| 500–1000 | 215 (21.4) |
| ≥1000 | 362 (36.1) |
| Workday sitting, h/d (n = 835) | |
| 0–3 | 136 (16.3) |
| 4–7 | 205 (24.6) |
| 8–11 | 329 (39.4) |
| 12–15 | 165 (19.8) |
| Nonworkday sitting, h/d (n = 918) | |
| 0–3 | 162 (17.6) |
| 4–7 | 401 (43.7) |
| 8–11 | 246 (26.8) |
| 12–15 | 109 (11.9) |
| Sugar-sweetened beverages (n = 967) | |
| Less than weekly | 521 (53.9) |
| Most days/daily | 446 (46.1) |
| Total discretionary foods (n = 978) | |
| None/<2 times/d | 836 (85.5) |
| ≥3 times/d | 142 (14.5) |
| Alcohol use (n = 985) | |
| Never/less than monthly | 502 (51.0) |
| Most weeks/daily | 483 (49.0) |
| 10-item Kessler Psychological Distress Scale score (n = 983) | |
| <22 | 585 (59.5) |
| ≥22 | 398 (40.5) |
African, Middle Eastern, American, and Caribbean Islander
Results
Participant characteristics
The sociodemographic characteristics of the 1005 women who participated in the study are shown in Table 1. The majority of women (67.4%) were age 25 to 44 y and lived in New South Wales (30.9%) or Victoria (27.7%). More than half identified as Australian, New Zealander, or Pacific Islander, 25.2% as European or North American, and 13.1% as Asian. At the time of the survey, 24.0% of women lived under lockdown restrictions and 40.5% were identified to have a high level of psychological distress (Table 1).
The mean BMI was 25.7 kg/m2 (SD: 6.3 kg/m2; n = 716), of whom 41.7% were overweight or obese. Less than one-half of women self-reported to have no, very low, or a low level of physical activity (Table 1). The mean number of sitting hours on a work- and nonworkday were 8.1 h (SD: 4.1 h) and 7.0 h (SD: 3.6 h), respectively, with around 60% and 40% of women reporting to spend 8 to 15 h of sitting in the respective work- and nonworkday (Table 1).
Around half of all women reported consuming SSBs most days/daily and alcohol most weeks/daily. In addition, 14.5% of women consumed discretionary choices ≥3 times per day (Table 1). Women consumed an average of 1.7 (SD: 1.0) and 2.5 (SD: 1.3) servings per day of fruits and vegetables, respectively.
Psychological distress and association with discretionary choices
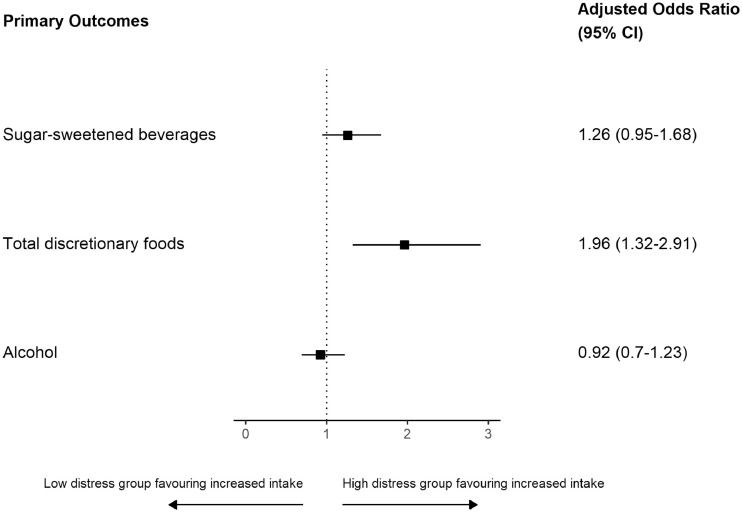
A summary of the effect of psychological distress on SSBs, total discretionary foods, and alcohol is reported in Figure 1 . Compared with women with a low level of psychological distress (score <22), those with a high level of psychological distress had near doubled odds (OR: 1.96; 95% confidence interval, 1.32–2.91) of reporting increased total discretionary foods. There was no association between psychological stress and SSBs or alcohol.
Fig. 1.
Summary of effect of psychological distress on three outcomes. Extracting odds ratio for psychological distress (low <22 [reference]; high 22+) from three separate multivariate models, there is a significant result for total discretionary foods (i.e., those with high-level distress had almost double odds of reporting increased total discretionary foods).
Characteristics and association with discretionary choices
Sugar-sweetened beverages
The association between characteristics of the women' and consumption of SSB in the unadjusted and adjusted analyses are reported in Table 2 . In the multivariable regression analyses, compared with the reference groups, Australian, New Zealander, or Pacific region women and those who reported 12 to 15 h of sitting on a nonworkday were more likely to consume SSBs most days/daily. Comparatively, older women, women with a higher annual household income, and women with a high level of physical activity were less likely to consume SSBs most days/daily (Table 2).
Table 2.
Association between participant characteristics and consumption of sugar-sweetened beverages
| Characteristic | Unadjusted OR (95% CI) | Adjusted* OR (95% CI) |
|---|---|---|
| Psychological distress | ||
| Low | Ref | Ref |
| High | 1.42 (1.10–1.84)† | 1.26 (0.95–1.68) |
| Age, y | ||
| 18–24 | Ref | Ref |
| 25–34 | 0.86 (0.58–1.26) | 0.91 (0.58–1.41) |
| 35–44 | 0.85 (0.58–1.26) | 0.81 (0.50–1.31) |
| 45–50 | 0.59 (0.38–0.93)‡ | 0.58 (0.34–1.00)‡ |
| Ethnicity | ||
| European or North American | Ref | Ref |
| Australian, New Zealander, or Pacific Islander | 1.71 (1.25–2.34)§ | 1.68 (1.21–2.33)† |
| Other | 1.55 (0.73–3.30) | 1.36 (0.62–3.00) |
| Asian | 1.43 (0.92–2.22) | 1.30 (0.81–2.09) |
| Annual household income before tax, AU$ | ||
| 0–99 999 | Ref | Ref |
| ≥100 000 | 0.61 (0.47–0.80)§ | 0.68 (0.51–0.91)‡ |
| Current living circumstances | ||
| Own home | Ref | Ref |
| Rented home or emergency accommodation | 1.04 (0.77–1.39) | 0.86 (0.62–1.19) |
| Living with family | 1.41 (1.01–1.98)‡ | 1.18 (0.78–1.78) |
| Lockdown restrictions | ||
| No | Ref | ― |
| Yes (Metropolitan Melbourne) | 0.88 (0.65–1.19) | ― |
| Employment status change | ||
| No | Ref | ― |
| Yes | 1.15 (0.86–1.54) | ― |
| Body mass index, kg/m2 | ||
| Normal weight | Ref | Ref |
| Underweight | 1.01 (0.50–2.06) | 0.86 (0.41–1.80) |
| Overweight | 1.25 (0.87–1.79) | 1.21 (0.82–1.78) |
| Obese | 1.42 (0.99–2.04) | 1.25 (0.83–1.88) |
| Weight change status | ||
| Stayed the same | Ref | Ref |
| Gained | 1.20 (0.91–1.60) | 1.12 (0.81–1.53) |
| Lost | 1.00 (0.69–1.45) | 1.00 (0.67–1.48) |
| Fruit serving number | 0.96 (0.83–1.11) | ― |
| Vegetable serving number | 0.90 (0.81–1.00)‡ | 0.97 (0.86–1.08) |
| Physical activity, metabolic min/wk | ||
| None or very low | Ref | Ref |
| Low | 0.82 (0.53–1.28) | 0.82 (0.51–1.30) |
| Moderate | 0.67 (0.42–1.06) | 0.66 (0.40–1.09) |
| High | 0.44 (0.29–0.69)§ | 0.47 (0.29–0.76)† |
| Workday sitting, h/d | ||
| 0–3 | Ref | Ref |
| 4–7 | 0.89 (0.57–1.40) | 0.93 (0.58–1.51) |
| 8–11 | 0.71 (0.47–1.06) | 0.75 (0.48–1.19) |
| 12–15 | 0.91 (0.58–1.44) | 0.86 (0.51–1.45) |
| Nonworkday sitting, h/d | ||
| 0–3 | Ref | Ref |
| 4–7 | 0.94 (0.64–1.37) | 1.11 (0.73–1.69) |
| 8–11 | 1.07 (0.71–1.60) | 1.26 (0.80–2.00) |
| 12–15 | 1.66 (1.00–2.73)‡ | 1.88 (1.07–3.29)‡ |
CI, confidence interval; OR, odds ratio; Ref, reference
Adjusted for age, ethnicity, current living circumstances, annual household income before tax, physical activity category, workday sitting hours category, non-workday sitting hours category, weight change status, body mass index, and psychological distress
P < 0.05
P < 0.01
P < 0.001
Total discretionary foods
Table 3 shows the association between women's characteristics and the consumption of total discretionary foods for both the unadjusted and adjusted analyses. In the multivariable regression analyses, compared with the reference groups, women with high psychological distress and those who gained weight during the pandemic had a higher likelihood of consuming discretionary foods ≥3 times per day. Compared with women who reported sitting 0 to 3 h per day, those who reported 4 to 7 h or 8 to 11 h sitting in a workday had lower odds of consuming total discretionary foods ≥3 times per day.
Table 3.
Association between participant characteristics and consumption of total discretionary foods
| Characteristic | Unadjusted OR (95% CI) | Adjusted* OR (95% CI) |
|---|---|---|
| Psychological distress | ||
| Low | Ref | Ref |
| High | 2.17 (1.50–3.12)† | 1.96(1.32–2.91)† |
| Age, y | ||
| 18–24 | Ref | Ref |
| 25–34 | 0.97 (0.58–1.62) | 1.21 (0.67–2.18) |
| 35–44 | 0.89 (0.52–1.51) | 1.14 (0.60–2.20) |
| 45–50 | 0.58 (0.30–1.12) | 0.82 (0.38–1.77) |
| Ethnicity | ||
| European or North American | Ref | Ref |
| Australian, New Zealander, or Pacific Islander | 1.51 (0.95–2.40) | 1.53 (0.94–2.48) |
| Other | 0.88 (0.25–3.13) | 1.06 (0.28–4.00) |
| Asian | 1.30 (0.69–2.47) | 1.31 (0.66–2.60) |
| Annual household income before tax, AU$ | ||
| 0–99 999 | Ref | Ref |
| ≥100 000 | 0.64 (0.44–0.94)‡ | 0.69 (0.45–1.06) |
| Current living circumstances | ||
| Own home | Ref | Ref |
| Rented home or emergency accommodation | 1.28 (0.85–1.93) | 1.04 (0.66–1.64) |
| Living with family | 1.47 (0.93–2.33) | 1.36 (0.78–2.37) |
| Lockdown restrictions | ||
| No | Ref | ― |
| Yes (Metropolitan Melbourne) | 1.22 (0.81–1.83) | ― |
| Employment status change | ||
| No | Ref | Ref |
| Yes | 1.48 (1.00–2.17)‡ | 1.31 (0.86–2.00) |
| Body mass index, kg/m2 | ||
| Normal weight | Ref | Ref |
| Underweight | 1.03 (0.38–2.81) | 0.89 (0.32–2.52) |
| Overweight | 0.97 (0.58–1.64) | 0.84 (0.47–1.48) |
| Obese | 1.57 (0.97–2.54) | 1.37 (0.79–2.38) |
| Weight change status | ||
| Stayed the same | Ref | Ref |
| Gained | 1.87 (1.25–2.81)§ | 1.71 (1.10–2.65)‡ |
| Lost | 0.88 (0.47–1.62) | 0.76 (0.40–1.45) |
| Fruit serving number | 1.06 (0.87–1.29) | ― |
| Vegetable serving number | 0.95 (0.81–1.12) | ― |
| Physical activity, metabolic min/wk | ||
| None or very low | Ref | Ref |
| Low | 0.98 (0.52–1.85) | 1.18 (0.60–2.32) |
| Moderate | 1.52 (0.80–2.89) | 1.91 (0.95–3.82) |
| High | 0.89 (0.48–1.67) | 1.37 (0.68–2.73) |
| Workday sitting, h/d | ||
| 0–3 | Ref | Ref |
| 4–7 | 0.57 (0.32–1.01) | 0.52‡ (0.28–0.97) |
| 8–11 | 0.50 (0.29–0.84)§ | 0.49‡ (0.28–0.88) |
| 12–15 | 0.78 (0.43–1.40) | 0.73 (0.39–1.37) |
| Nonworkday sitting, h/d | ||
| 0–3 | Ref | |
| 4–7 | 0.76 (0.46–1.28) | ― |
| 8–11 | 0.81 (0.46–1.40) | ― |
| 12–15 | 1.24 (0.66–2.33) | ― |
CI, confidence interval; OR, odds ratio; Ref, reference
Adjusted for age, ethnicity, current living circumstances, annual household income before tax, physical activity category, workday sitting hours category, nonworkday sitting hours category, weight change status, body mass index, and psychological distress
P < 0.05
P < 0.01
P < 0.001
Alcohol
The association between women's characteristics and the consumption of alcohol in the unadjusted and adjusted multivariable regression analyses is reported in Table 4 . Older women (age 45–50 y), those who reported a higher annual household income (≥100 000 AU$), and those who reported moderate or high physical activity were more likely to consume alcohol most weeks/daily. Asian women, women who lived under lockdown restriction versus no lockdown, and those with obesity compared with normal weight were less likely to consume alcohol most weeks/daily (Table 4).
Table 4.
Association between participant characteristics and alcohol consumption
| Characteristic | Unadjusted OR (95% CI) | Adjusted* OR (95% CI) |
|---|---|---|
| Psychological distress | ||
| Low | Ref | Ref |
| High | 0.81 (0.62–1.04) | 0.92 (0.70–1.23) |
| Age, y | ||
| 18–24 | Ref | Ref |
| 25–34 | 0.96 (0.66–1.41) | 0.93 (0.60–1.43) |
| 35–44 | 1.21 (0.82–1.77) | 1.15 (0.71–1.85) |
| 45–50 | 1.91 (1.22–2.97)† | 1.70 (1.00–2.89)‡ |
| Ethnicity | ||
| European or North American | Ref | Ref |
| Australian, New Zealander, or Pacific Islander | 0.79 (0.58–1.07) | 0.81 (0.59–1.12) |
| Other | 0.42 (0.19–0.92)‡ | 0.50 (0.22–1.10) |
| Asian | 0.26 (0.16–0.42)§ | 0.28 (0.17–0.47)§ |
| Annual household income before tax, AU$ | ||
| 0–99 999 | Ref | Ref |
| ≥100 000 | 1.58 (1.21–2.07)§ | 1.44 (1.08–1.92)‡ |
| Current living circumstances | ||
| Own home | Ref | Ref |
| Rented home or emergency accommodation | 0.78 (0.58–1.04) | 0.90 (0.65–1.24) |
| Living with family | 0.61 (0.44–0.86)† | 0.72 (0.48–1.08) |
| Lockdown restrictions | ||
| No | Ref | Ref |
| Yes (Metropolitan Melbourne) | 0.75 (0.56–1.01) | 0.73 (0.53–1.00) |
| Employment status change | ||
| No | Ref | ― |
| Yes | 1.01 (0.76–1.34) | ― |
| Body mass index, kg/m2 | ||
| Normal weight | Ref | Ref |
| Underweight | 0.64 (0.33–1.28) | 0.83 (0.41–1.69) |
| Overweight | 1.10 (0.77–1.56) | 0.96 (0.65–1.41) |
| Obese | 0.77 (0.53–1.11) | 0.68 (0.45–1.02) |
| Weight status | ||
| Stayed the same | Ref | ― |
| Gained | 0.88 (0.67–1.17) | ― |
| Lost | 0.94 (0.65–1.35) | ― |
| Fruit serving number | 0.91 (0.79–1.05) | ― |
| Vegetable serving number | 1.11‡ (1.00–1.23) | 1.02 (0.91–1.14) |
| Physical activity, metabolic min/wk | ||
| None or very low | Ref | Ref |
| Low | 0.93 (0.59–1.44) | 1.00 (0.63–1.60) |
| Moderate | 1.51 (0.94–2.40) | 1.59 (0.97–2.61) |
| High | 1.89 (1.22–2.91)† | 1.75 (1.10–2.80)‡ |
| Workday sitting, h/d | ||
| 0–3 | Ref | ― |
| 4–7 | 1.10 (0.71–1.71) | ― |
| 8–11 | 1.07 (0.71–1.61) | ― |
| 12–15 | 1.28 (0.81–2.01) | ― |
| Nonworkday sitting, h/d | ||
| 0–3 | Ref | ― |
| 4–7 | 0.98 (0.67–1.43) | ― |
| 8–11 | 1.02 (0.68–1.53) | ― |
| 12–15 | 1.00 (0.60–1.65) | ― |
CI, confidence interval; OR, odds ratio; Ref, reference
Adjusted for age, ethnicity, current living circumstances, annual household income before tax, physical activity category, workday sitting hours category, nonworkday sitting hours category, weight change status, body mass index, and psychological distress
P < 0.05
P < 0.01
P < 0.001
Discussion
In this cross-sectional survey conducted during the COVID-19 pandemic in Australia, a high level of psychological distress was associated with the consumption of discretionary foods ≥3 times per day, but not alcohol consumed most weeks or daily. The relationship between psychological distress and SSBs was not as clear, because a significant univariate association appeared to disperse when adjusting for other factors in the multivariable analysis. Low levels of physical activity and more sitting time were associated with the consumption of SSBs, but gaining weight during the pandemic was associated with a higher intake of discretionary foods.
To our knowledge, this is the first study to report on the association between psychological distress and discretionary foods during the COVID-19 pandemic in reproductive-age women in Australia. We also report that gaining weight during the pandemic was associated with higher intakes of discretionary foods. These findings add to studies conducted internationally that demonstrated positive associations between increased consumption of poor food choices and psychological stress during the pandemic [34], [35], [36]. Higher stress scores during the pandemic have also been associated with increased energy intake [37], with other studies linking increased hunger with weight gain [38]. Discretionary foods typically high in energy, saturated fatty acids, sugar, and sodium, contribute to proinflammatory pathways [39], and such dietary patterns are associated with a higher incidence of depressive symptoms [40,41].
Furthermore, negative emotions affect food choices through neurobiological processes [42] and altered hippocampal function [43]. However, these relationships are not unique to the pandemic [44]. Current and past findings on psychological distress and poor dietary behavior suggest a bidirectional relationship between mental health and food intake. From the current cross-sectional survey, we do not know whether psychological stress increased in women compared with before the pandemic; thus, if our findings of a relationship between psychological distress and discretionary food intake was amplified during lockdown is unclear. However, given that 40% of women in our study had a high level of psychological distress, which is slightly higher than a smaller (33%) sample of Australian adults during the COVID-19 pandemic [45], but much higher than the 17% reported in women age 18 to 55 y from Australian population data from 2014 to 2015 [46], suggesting that higher intakes of discretionary choices may be a coping strategy for psychological distress and, for some women, perpetuating weight gain during the pandemic.
Psychological distress was not associated with a higher consumption of alcohol. This is in contrast to three other Australian studies conducted during the pandemic that showed that increased alcohol was associated with increased depression and anxiety [7,47], higher psychological distress, and higher levels of fear of COVID-19 [45]. Often, alcohol consumption is reported as a coping mechanism for psychological factors, including alleviating stress [48]. Different types of stressors have been linked to increased alcohol intake, such that heavier drinking was most strongly connected to childcare stressors among women in Australia, but more commonly associated with job loss or reductions in paid employment hours for men [49].
Social isolation, concomitant with changes in employment status or future insecurity, may also elicit an increase in alcohol intake in vulnerable individuals [50]. During the pandemic in Australia, alcohol stores were considered essential services, and did not close. Interestingly, Australian population data report no clear patterns of the effects of COVID-19 restrictions on alcohol and other drug consumption, with many people reporting unchanged levels of consumption [51]. Furthermore, the closure of licensed premises and social distancing measures appear to have reduced harmful alcohol consumption in younger drinkers, particularly young women [52]. Nevertheless, despite the inconsistent relationships between psychological stress and alcohol in our study and compared with other studies, alcohol is recognized as an underreported item among men and women of different ages [53,54], and people do not often adjust their responses to account for standard drink units [55,56]. These factors may partly explain our findings. Strategies to reduce alcohol use during COVID-19 restrictions should be targeted at those who already have higher levels of psychological stress, and effects of change in alcohol use during the COVID-19 pandemic on mental health are needed.
We report that a longer duration of sitting time was associated with higher SSB intake, but older women, higher physical activity, and higher income were associated with lower consumption of SSB. Among U.S. adults during the pandemic, similar associations were reported, with drinking more SSBs associated with being younger, having less education, lower household income, and being obese [57]. A qualitative study in young adults in Australia reported replacing meals with beverages or snacks, which may have been a way to manage financial instability and food insecurity [58]. Another study in Norway reported an association between high-sugar foods and beverages in those with psychological distress [59], but the relationship we detected with psychological distress was no longer significant after adjusting for confounders, which may be due to underreporting of SSBs more broadly [60,61]. The high proportion of younger women with significant psychological distress warrants further research on the direct and indirect effect of psychological burden on health behaviors in this group.
This study adds to the growing body of literature investigating diet and lifestyle factors during the COVID-19 pandemic, and contributes to the knowledge regarding the association of these factors with psychological distress. We calculated our sample size based on the current population of women in Australia age 15 to 50 y, with a small margin of error of 1%. This small percentage indicates that responses from our sample likely well reflect the views of the overall population. Limitations include that this cross-sectional survey was not specifically designed to examine changes in diet and lifestyle factors, nor psychological distress, over the course of the pandemic, but rather we captured a snapshot of current effects. As stated in our subsequent paper on pregnancy intention and psychological distress [62], we determined the level of pandemic restrictions based on location. Although there was a clear distinction in the level of viral transmission rates and lockdown restrictions in metropolitan Melbourne compared with all other regions in Australia during the months leading up to and during the survey, other factors related to living in metropolitan Melbourne, diet and lifestyle factors, and psychological distress may explain our findings.
Conclusions
Higher levels of psychological distress were associated with a higher intake of discretionary foods and SSBs, but not alcohol. After adjusting for confounders, only the association between psychological distress and discretionary food intake remained significant. Although these findings were reported to occur during the COVID-19 pandemic, they reflect consistent relationships outside such a circumstance. Public health messaging promoting healthy eating should take into account the effect of psychological distress on health behavior. Messages aimed at maintaining a positive relationship between food intake and mental wellbeing, particularly among vulnerable groups, are warranted. Further studies on the relationship between psychological well-being and food intake would be helpful.
Acknowledgements
The authors are grateful for Edward Meehan who assisted with developing the Qualtrics version of this survey.
Footnotes
Jessica A. Grieger is funded by a National Health and Medical Research Council Ideas Grant (APP2000905). Siew Lim is funded by a National Health and Medical Research Council Early Career Fellowship (APP1139481).
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.nut.2022.111794.
Appendix. Supplementary materials
References
- 1.Australian Government, Department of Health. Coronavirus (COVID-19) at a glance. Available at: https://www.health.gov.au/resources/publications/coronavirus-covid-19-at-a-glance-31-may-2020_2020. Accessed February 20, 2021.
- 2.Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public-a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by U.S. adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office for National Statistics. Coronavirus and anxiety, Great Britain: 3 April 2020 to 10 May. 2020. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusandanxietygreatbritain/3april2020to10may2020. Accessed February 20, 2021.
- 6.Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. 2021;29:26–30. doi: 10.1177/1039856220965045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17:4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connor J, Madhavan S, Mokashi M, Amanuel H, Johnson NR, Pace LE, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266 doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thibaut F, van Wijngaarden-Cremers PJM. Women's mental health in the time of COVID-19 pandemic. Front Glob Womens Health. 2020;1 doi: 10.3389/fgwh.2020.588372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin SC, Tyus N, Maloney M, Ohri B, Sripipatana A. Mental health status among women of reproductive age from underserved communities in the United States and the associations between depression and physical health. A cross-sectional study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. doi: 10.1016/j.bpobgyn.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 13.Fathnezhad-Kazemi A, Hajian S. Factors influencing the adoption of health promoting behaviors in overweight pregnant women: a qualitative study. BMC Pregnancy Childbirth. 2019;19:43. doi: 10.1186/s12884-019-2199-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav. 2007;39:31–36. doi: 10.1016/j.jneb.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 15.Chew HSJ, Lopez V. Global impact of COVID-19 on weight and weight-related behaviors in the adult population: a scoping review. Int J Environ Res Public Health. 2021;18:1876. doi: 10.3390/ijerph18041876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Renzo L, Gualtieri P, Cinelli G, Bigioni G, Soldati L, Attinà A, et al. Psychological aspects and eating habits during COVID-19 home confinement: results of EHLC-COVID-19 Italian online survey. Nutrients. 2020;12:2152. doi: 10.3390/nu12072152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scarmozzino F, Visioli F. COVID-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9:675. doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Australian Bureau of Statistics. Australian demographics statistics 2020. Available from: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release. Accessed February 20, 2021.
- 19.Webb P, Bain C, Page A. 3rd ed. Cambridge University Press; Cambridge, MA: 2017. Essential epidemiology: an introduction for students and health professionals. [Google Scholar]
- 20.Victoria State Government. Identifying metro Melbourne restricted postcodes. Available at: https://www.coronavirus.vic.gov.au/sites/default/files/2020–10/Metro-Melb-Postcodes-Factsheet.pdf. Accessed May 30, 2021.
- 21.Australian Government, National Health and Medical Research Council. Eat for health. Discretionary food and drink choices. Available at: https://www.eatforhealth.gov.au/food-essentials/discretionary-food-and-drink-choices. Accessed February 20, 2021.
- 22.Australian Government, National Health and Medical Research Council. Australian dietary guidelines, eat for health. Available from: www.nhmrc.gov.au/guidelines-publications/n55. Accessed April 19, 2021.
- 23.Yaroch AL, Tooze J, Thompson FE, Blanck HM, Thompson OM, Colón-Ramos U, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute's food attitudes and behaviors survey. J Acad Nutr Diet. 2012;112:1570–1577. doi: 10.1016/j.jand.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Australian Government, Australian Institute of Health and Welfare. The Active Australia Survey: A guide and manual for implementation, analysis and reporting. Available at: https://www.aihw.gov.au/reports/physical-activity/active-australia-survey/summary. Accessed June 12, 2021.
- 25.Brown WJ, Bauman AE, Bull FC, Burton NW. Development of evidence-based physical activity recommendations for adults (18–64 years): report prepared for the Australian Government Department of Health, August 2012. Available at: https://www.health.gov.au/resources/publications/development-of-evidence-based-physical-activity-for-adults-18-to-64-years. Accessed June 12, 2021.
- 26.Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): volume 5–Remoteness Structure, July 2016. Available at: https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005. Accessed June 12, 2021.
- 27.van Uffelen JGZ, Watson MJ, Dobson AJ, Brown WJ. Comparison of self-reported week-day and weekend-day sitting time and weekly time-use: results from the Australian Longitudinal Study on Women's Health. Int J Behav Med. 2011;18:221–228. doi: 10.1007/s12529-010-9105-x. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 29.Cheng FW, Gao X, Mitchell DC, Wood C, Still CD, Rolston D, et al. Body mass index and all-cause mortality among older adults. Obesity (Silver Spring) 2016;24:2232–2239. doi: 10.1002/oby.21612. [DOI] [PubMed] [Google Scholar]
- 30.Van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67. [Google Scholar]
- 31.Raghunathan TE, Solenberger PW, Van Hoewyk J. Survey Methodology Program. Survey Research Center, Institute for Social Research, University of Michigan; 2002. IVEware: imputation and variance estimation software. Ann Arbor, MI. [Google Scholar]
- 32.van Ginkel JR, Linting M, Rippe RCA, van der Voort A. Rebutting existing misconceptions about multiple imputation as a method for handling missing data. J Pers Assess. 2020;102:297–308. doi: 10.1080/00223891.2018.1530680. [DOI] [PubMed] [Google Scholar]
- 33.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–598. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 34.Brytek-Matera A, Obeid S, Akel M, Hallit S. How does food addiction relate to obesity? Patterns of psychological distress, eating behaviors and physical activity in a sample of Lebanese adults: the MATEO study. Int J Environ Res Public Health. 2021;18:10979. doi: 10.3390/ijerph182010979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, Szabo de Edelenyi F, Allès B, Andreeva VA, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March-May 2020): results from the French NutriNet-Sante cohort study. Am J Clin Nutr. 2021;113:924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khubchandani J, Kandiah J, Saiki D. The COVID-19 pandemic, stress, and eating practices in the United States. Eur J Investig Health Psychol Educ. 2020;10:950–956. doi: 10.3390/ejihpe10040067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. JMIR Public Health Surveill. 2020;6:e19630. doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanchez E, Lecube A, Bellido D, Monereo S, Malagón MM, Tinahones FJ, et al. Leading factors for weight gain during COVID-19 lockdown in a Spanish population: a cross-sectional study. Nutrients. 2021;13:894. doi: 10.3390/nu13030894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leonard BE. Inflammation and depression: a causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 2018;30:1–16. doi: 10.1017/neu.2016.69. [DOI] [PubMed] [Google Scholar]
- 40.Oddy WH, Allen KL, Trapp GSA, Ambrosini GL, Black LJ, Huang RC, et al. Dietary patterns, body mass index and inflammation: pathways to depression and mental health problems in adolescents. Brain Behav Immun. 2018;69:428–439. doi: 10.1016/j.bbi.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 41.Phillips CM, Shivappa N, Hébert JR, Perry IJ. Dietary inflammatory index and mental health: a cross-sectional analysis of the relationship with depressive symptoms, anxiety and well-being in adults. Clin Nutr. 2018;37:1485–1491. doi: 10.1016/j.clnu.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 42.Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. Nutrients. 2017;9:1274. doi: 10.3390/nu9111274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parent MB, Darling JN, Henderson YO. Remembering to eat: hippocampal regulation of meal onset. Am J Physiol Regul Integr Comp Physiol. 2014;306:R701–R713. doi: 10.1152/ajpregu.00496.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gomersall SR, Dobson AJ, Brown WJ. Weight gain, overweight, and obesity: determinants and health outcomes from the Australian longitudinal study on women's health. Curr Obes Rep. 2014;3:46–53. doi: 10.1007/s13679-013-0077-4. [DOI] [PubMed] [Google Scholar]
- 45.Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, et al. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Global Health. 2020;16:95. doi: 10.1186/s12992-020-00624-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Australian Institute of Health and Welfare. Australia's Health 2018: psychological distress. Available at: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/indicators-of-australias-health/psychological-distress. Accessed March 12, 2021.
- 47.Tran TD, Hammarberg K, Kirkman M, Nguyen HTM, Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J Affect Disord. 2020;277:810–813. doi: 10.1016/j.jad.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Becker HC. Influence of stress associated with chronic alcohol exposure on drinking. Neuropharmacology. 2017;122:115–126. doi: 10.1016/j.neuropharm.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Biddle N, Edwards B, Gray M, Sollis K. Alcohol consumption during the COVID-19 period. Available at: https://openresearch-repository.anu.edu.au/bitstream/1885/213196/1/Alcohol_consumption_during_the_COVID-19_period.pdf. Accessed March 12, 2021.
- 50.Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. 2020;5:e259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Australian Institute of Health and Welfare. Alcohol, tobacco & other drugs in Australia. Impacts of COVID-19 on alcohol and other drug use. Available at: https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/impact-of-covid-19-on-alcohol-and-other-drug-use. Accessed January 20, 2022.
- 52.Callinan S, Smit K, Mojica-Perez Y, D'Aquino S, Moore D, Kuntsche E. Shifts in alcohol consumption during the COVID-19 pandemic: early indications from Australia. Addiction. 2021;116:1381–1388. doi: 10.1111/add.15275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gemming L, Ni Mhurchu C. Dietary under-reporting: what foods and which meals are typically under-reported? Eur J Clin Nutr. 2016;70:640–641. doi: 10.1038/ejcn.2015.204. [DOI] [PubMed] [Google Scholar]
- 54.Knibbe RA, Bloomfield K. Alcohol consumption estimates in surveys in Europe: comparability and sensitivity for gender differences. Subst Abus. 2001;22:23–38. doi: 10.1080/08897070109511443. [DOI] [PubMed] [Google Scholar]
- 55.Devos-Comby L, Lange JE. My drink is larger than yours"? A literature review of self-defined drink sizes and standard drinks. Curr Drug Abuse Rev. 2008;1:162–176. doi: 10.2174/1874473710801020162. [DOI] [PubMed] [Google Scholar]
- 56.Gilligan C, Anderson KG, Ladd BO, Yong YM, David M. Inaccuracies in survey reporting of alcohol consumption. BMC Public Health. 2019;19:1639. doi: 10.1186/s12889-019-7987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Park S, Lee SH, Yaroch AL, Blanck HM. Reported changes in eating habits related to less healthy foods and beverages during the COVID-19 pandemic among U.S. adults. Nutrients. 2022;14:526. doi: 10.3390/nu14030526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kombanda KT, Margerison C, Booth A, Worsley A. The impact of the COVID-19 pandemic on young Australian adults' food practices. Curr Dev Nutr. 2022;6:nzac009. doi: 10.1093/cdn/nzac009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bemanian M, Mæland S, Blomhoff R, Rabben ÅK, Arnesen EK, Skogen JC, et al. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int J Environ Res Public Health. 2020;18:130. doi: 10.3390/ijerph18010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bingham SA, Gill C, Welch A, Day K, Cassidy A, Khaw KT, et al. Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br J Nutr. 1994;72:619–643. doi: 10.1079/bjn19940064. [DOI] [PubMed] [Google Scholar]
- 61.Krebs-Smith SM, Graubard BI, Kahle LL, Subar AF, Cleveland LE, Ballard-Barbash R. Low energy reporters vs others: a comparison of reported food intakes. Eur J Clin Nutr. 2000;54:281–287. doi: 10.1038/sj.ejcn.1600936. [DOI] [PubMed] [Google Scholar]
- 62.Schoenaker D, Bennett C, Grieger J, Harrison C, Hill B, Enticott J, Moran L, Teede H, O'Reilly S, Lim S. Association between pregnancy intention and psychological distress among women exposed to different levels of restrictions during the COVID-19 pandemic in Australia. PLoS One. 2022. 10.1371/journal.pone.0273339. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.