Abstract
Objectives
Despite established standards and guidelines, substantial variation remains in the delivery of hip fracture care across the United Kingdom. We aimed to determine which hospital-level organisational factors predict adverse patient outcomes in the months following hip fracture.
Methods
We examined a national record-linkage cohort of 178,757 patients aged ≥60 years who sustained a hip fracture in England and Wales in 2016–19. Patient-level hospital admissions datasets, National Hip Fracture Database and mortality data were linked to metrics from 18 hospital-level organisational-level audits and reports. Multilevel models identified organisational factors, independent of patient case-mix, associated with three patient outcomes: length of hospital stay (LOS), 30-day all-cause mortality and emergency 30-day readmission.
Results
Across hospitals mean LOS ranged from 12 to 41.9 days, mean 30-day mortality from 3.7 to 10.4% and mean readmission rates from 3.7 to 30.3%, overall means were 21.4 days, 7.3% and 15.3%, respectively. In all, 22 organisational factors were independently associated with LOS; e.g. a hospital’s ability to mobilise >90% of patients promptly after surgery predicted a 2-day shorter LOS (95% confidence interval [CI]: 1.2–2.6). Ten organisational factors were independently associated with 30-day mortality; e.g. discussion of patient experience feedback at clinical governance meetings and provision of prompt surgery to >80% of patients were each associated with 10% lower mortality (95%CI: 5–15%). Nine organisational factors were independently associated with readmissions; e.g. readmissions were 17% lower if hospitals reported how soon community therapy would start after discharge (95%CI: 9–24%).
Conclusions
Receipt of hip fracture care should be reliable and equitable across the country. We have identified multiple, potentially modifiable, organisational factors associated with important patient outcomes following hip fracture.
Keywords: hip fracture, organisational factors, patient outcomes, mortality, length of stay
Key Points
We simultaneously assessed a range of organisational factors against important patient outcomes post-hip fracture.
Comprehensive national data identified several modifiable organisational factors associated with improved patient outcomes.
A hospital’s ability to mobilise >90% of patients promptly after surgery was associated with a 2-day shorter length of hospital stay.
Discussion of patient experience feedback at clinical governance meetings was associated with 10% lower 30-day mortality.
The ability of hospitals to report how soon community therapy starts after discharge was associated with 17% fewer emergency 30-day readmissions.
Introduction
Each year more than 70,000 older adults are admitted to a UK hospital after a hip fracture [1]; events that lead to substantial loss of quality of life [2], high mortality risk [3] and, after discharge, high risk of emergency hospital readmission [4]. Hip fracture services are provided through complex multidisciplinary organisational structures. There are established national standards, guidelines, audit (National Hip Fracture Database, NHFD), and financial incentives (Best Practice Tariff, BPT) for hip fracture care [5]. The latter is a reimbursement to hospitals based on achievement of seven nationally agreed quality metrics. Through transparent reporting and benchmarking, the NHFD audit has improved overall hip fracture care over the last decade [6]. However, we and others have shown that substantial variation in hospital delivery of hip fracture care persists [7–9]. Nationally, we see marked differences between hospitals in patient outcomes; mortality, functional recovery and need for institutional care [3]. Whilst this is in part explained by patient-level characteristics, we hypothesized that much of the remaining variation in hip fracture care delivery can be explained by organisational factors. Understanding predictors of variation in care delivery, and the effects on patient outcomes, will inform service-level interventions to reduce unwarranted variation, maximise health equity and ultimately improve patient experience.
We linked data from multiple national datasets quantifying elements of hip fracture care at both patient- and hospital-levels. Using hospital-level metrics, we quantified each hospital’s organisational capacity to manage fragility fractures across a range of care domains, including the delivery of emergency, surgical, orthogeriatric and rehabilitation services, along with overarching governance structures. We then examined which hospital-level organisational factors, and corresponding care domains, predicted patient outcomes post-hip fracture across England and Wales.
Methods
Study population
The REDUCE study (REducing unwarranted variation in the Delivery of high-qUality hip fraCture services in England and Wales) used linked anonymised patient-level data for index hip fracture cases from the routinely collected Hospital Episodes Statistics (HES) Admitted Patient Care database, Office for National Statistics (ONS) Civil Registration Deaths and NHFD, a Healthcare Quality Improvement Partnership (HQIP) clinical audit of hip fracture care (Figure S1) [10–12]. This included hip fracture admissions to all English hospitals within the National Health Service (NHS). The equivalent patient-level Patient Episode Database for Wales (PEDW) data for admitted patient care was linked for Wales.
Our study population consisted of all index hip fracture cases (i.e. first occurrence of hip fracture), among English or Welsh residents aged 60 years or more, admitted to an English or Welsh hospital between 1 April 2016 and 31 March 2019. Patient follow-up was analysed for 12 months post-hip fracture (last follow-up: 31st March 2020) (see Supplementary Methods).
Patient outcomes
These were: (i) acute NHS ‘superspell’ length of stay (LOS), (ii) cumulative (all-cause) mortality at 30 days from hospital admission and (iii) emergency (all-cause) readmissions to any English/Welsh NHS hospital within 30 days of discharge. ‘Superspell’ LOS starts from the date of admission for the index hip fracture to the final date of discharge alive from an NHS acute or rehabilitation hospital; it includes the index hip fracture admission, plus any planned or unplanned hospital transfers for elective or emergency care, respectively.
Patient case-mix
Case-mix adjustment was the same as that used in the NHFD clinical audit (Table 1) [13] and included age, sex, American Society of Anesthesiologists’ (ASA) classification of pre-operative physical status [14], hip fracture type, pre-fracture residence and pre-fracture mobility [13].
Table 1.
Characteristics of patients admitted to hospital with a hip fracture in England and Wales from 2016 to 2019
| Pre-fracture characteristics and post-fracture outcomes | All | England | Wales | |||||
|---|---|---|---|---|---|---|---|---|
| N | N | % | Mean (SD) | N | % | Mean (SD) | ||
| N patients | 178,757 | 168,359 | 94 | 10,398 | 6 | |||
| N hospitals | 172 | 159 | 92.4 | 13 | 7.6 | |||
| Age (years) | 178,757 | 82.7 (8.6) | 82.3 (8.6) | |||||
| Age (years) | 60–69 | 16,062 | 15,082 | 9 | 980 | 9 | ||
| 70–79 | 41,096 | 38,562 | 23 | 2,534 | 24 | |||
| 80–89 | 80,863 | 76,177 | 45 | 4,686 | 45 | |||
| 90+ | 40,736 | 38,538 | 23 | 2,198 | 21 | |||
| Sex | Female | 126,278 | 118,859 | 71 | 7,419 | 71 | ||
| ASA grade | I and II | 45,222 | 42,272 | 25 | 2,975 | 29 | ||
| III | 102,323 | 96,460 | 57 | 5,836 | 56 | |||
| IV and V | 31,212 | 29,627 | 18 | 1,587 | 15 | |||
| Hip fracture type | Intracapsular | 105,082 | 99,029 | 59 | 6,053 | 58 | ||
| Inter, subtrochanteric or other | 73,675 | 69,330 | 41 | 4,345 | 42 | |||
| Pre-fracture residence | Own home/sheltered housing | 146,642 | 137,877 | 82 | 8,761 | 84 | ||
| Not from own home | 32,115 | 30,482 | 18 | 1,637 | 16 | |||
| Pre-fracture mobility | Freely mobile without walking aids | 66,440 | 62,598 | 37 | 3,872 | 37 | ||
| Mobile outdoors with 1 or 2 aids or frame | 66,521 | 62,499 | 37 | 3,977 | 38 | |||
| Some indoor, or no functional, mobility | 45,796 | 43,262 | 26 | 2,549 | 25 | |||
| Post-fracture outcomes | ‘Superspell’ LOS | 165,350 | 21.4 (19.6) | 21.4 (23.4) | ||||
| Cumulative 30-day mortality | 178,757 | 12,321 | 7 | 805 | 8 | |||
| Emergency 30-day readmissions | 165,350 | 24,499 | 16 | 740 | 8 | |||
SD = standard deviation.
Organisational-level data
Publicly available hospital/trust provider-level data were extracted from 18 national audits, data series or ratings [12], generating 231 organisational factors, characterising each stage of the hip fracture care pathway from admission to discharge (Table S1). We used a systematic approach, as previously described [12], to categorise organisational factors that could potentially be associated with patient outcomes. Firstly, we mapped each factor to one or more of 14 a priori defined hip fracture care domains by stakeholder consensus (see Supplementary Methods) [12]. Each organisational-level factor was mapped as potentially relevant to one or more patient outcomes by expert consensus [12]. Secondly, each factor was assigned to one overarching theme (pre-, peri-, post-op, governance or workload). Time-specific organisational-level factors were linked to patient-level data using hospital/trust provider codes and the year (and month/quarter if available) appropriate to the date of hip fracture admission.
Approvals
These were obtained from: NHS Health Research Authority, London City & East Research Ethics Committee (20/LO/0101); Royal College of Physicians Falls and Fragility Fracture Audit Programme (FFFAP/2018/003) and HQIP330; NHS Wales Informatics Service (NWIS/30941), with an NHS Digital Data Sharing Agreement (DARS-NIC-334549-B1Y6X-v1.4).
Statistical analysis
Multilevel regression models estimated associations between organisational-level factors and patient-level outcomes, adjusting for patient case-mix. The hierarchical data structure consisted of patients (level 1), nested within hospitals (level 2). Using C-statistics or R2, we identified the proportion of variance in each patient outcome that was explained by patient-level factors (i.e. case-mix) and quantified between-hospital variability explained by fixed organisational effects. Organisational factors were binarized, categorised or if continuous converted to linear splines at quartiles (or tertiles). Backward stepwise elimination determined organisational factors most strongly associated with each outcome. Organisational factors were simplified by expert review and splines binarized/categorised at appropriate threshold(s) or converted back to continuous measures on an appropriate scale. For each outcome, organisational factors were added sequentially by domain to a case-mix adjusted multilevel model. Analyses of superspell LOS were limited to those who survived the admission to avoid bias by early mortality. Statistical analyses were performed in Stata 16.1 (StataCorp LP, College Station, TX) and MLwiN v3.01 (Centre for Multilevel Modelling, University of Bristol, UK). We followed STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidance [15].
Results
The characteristics of 178,757 patients admitted with a hip fracture between 2016 and 2019 were similar between England and Wales, with only 6% (10,398/178,757) admitted in Wales (Table 1, Figure S1). Annual admission numbers differed by hospital; from 168 to 2,552 in England and 349 to 1,495 in Wales. Average LOS was 21.4 days (standard deviation, 19.9 days); 13,126 (7.3%) patients died within 30 days (either in hospital or post-discharge) and 25,239 (15.3%) were readmitted within 30 days. Patient outcomes were similar between countries, other than lower 30-day readmissions in Wales (8%) versus England (16%). Across hospitals mean LOS ranged from 12 to 41.9 days, mean 30-day mortality from 3.7 to 10.4% and mean readmission rates from 3.7 to 30.3%.
Between-hospital variability explained by organisational factors
Prediction of all patient outcomes was improved by the addition of case-mix to our models (e.g. C-statistic for mortality increased from 0.55 [95% confidence interval, CI: 0.55, 0.56] without case-mix, to 0.76 [95%CI: 0.76, 0.77] with case-mix) but was unchanged by the addition of organisational factors (Table S2). The domains to which organisational factors were assigned did not discriminate for any outcome (data not presented). Hip fracture clinical governance was strongly associated with all outcomes (Figures 1–3).
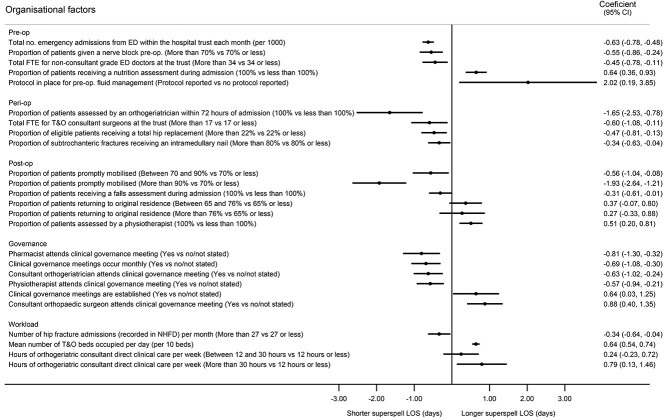
Figure 1.
The association between organisational factors and superspell LOS, after accounting for patient case-mix. Organisational factors are adjusted for case-mix (age, sex, ASA classification, hip fracture type, pre-fracture residence and pre-fracture mobility) and mutually adjusted for all backward selected factors reported in Supplementary Table S2. Factors with P-value < 0.1 shown. N = 165,350. ED = emergency department. FTE = full time equivalent. op = operative. Rehab. = rehabilitation. T&O = Trauma and orthopaedic.
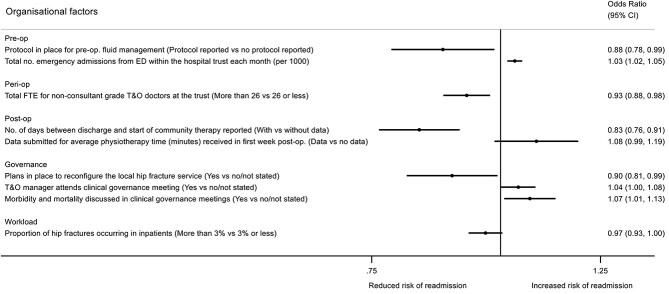
Figure 3.
The association between organisational factors and emergency readmissions within 30 days of discharge, after accounting for patient case-mix. Organisational factors adjusted for case-mix (age, sex, ASA classification, hip fracture type, pre-fracture residence and pre-fracture mobility) and mutually adjusted for all backward selected factors reported in Supplementary Table S4. Factors with P-value < 0.1 shown. N = 165,350.
Organisational factors associated with superspell LOS
In mutually adjusted analyses, hospitals with busier emergency departments (EDs) (i.e. with more emergency admissions per month), higher levels of non-consultant staffing (i.e. >34 full-time staff grades and/or junior doctors) and those giving a greater proportion of nerve blocks (femoral nerve or fascia-iliaca) pre-theatre were all associated with shorter LOS (Figure 1, Table S3). Hospitals reporting 100% compliance with the BPT qualifier ‘nutrition assessment’, conversely had longer LOS, as did hospitals reporting a pre-operative fluid management protocol. Perioperatively, hospitals where all patients received orthogeriatric assessment within 72 hours of admission had an ~1.5-day (1.65, 95%CI: 0.78, 2.53 days) shorter LOS, compared with hospitals where not all patients received timely assessment (only 17 hospitals reported 1 month or more where 100% of orthogeriatric assessments within 72 hours were achieved). Greater orthopaedic consultant staffing and provision of hip replacements in eligible patients were both associated with shorter LOS.
Post-operatively, the organisational factor most strongly, and independently, associated with reduced superspell LOS was the ability to get patients out of bed by the day after surgery. Sixty hospitals reported being able to mobilise >90% of patients within this window, during some or all of the 3-year study period. Each patient these hospitals managed achieved a 2-day (−1.93, 95%CI: −2.64, −1.21 days) shorter LOS, compared with hospitals where fewer than 70% were promptly mobilised. A strong dose–response association was seen between prompt mobilisation and LOS. Paradoxically, hospitals reporting 100% compliance with the BPT qualifier of ‘physiotherapy assessment’ had longer LOS. Several governance-related factors were independently associated with LOS. Hospitals holding monthly hip fracture service clinical governance meetings had on average shorter LOS. However, whilst attendance at these meetings by the orthogeriatric consultant, pharmacist and physiotherapist was associated with shorter LOS, attendance by the orthopaedic consultant was associated with longer LOS.
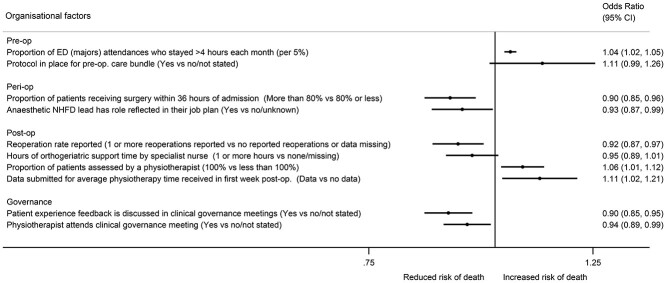
Organisational factors associated with 30-day mortality
ED performance predicted mortality: for every 5% increase in the proportion of ED (majors) attendances breaching the 4-hour trolley wait each month, mortality was 4% higher (Figure 2, Table S4). A total of 89 hospitals reported prompt surgery (within 36 hours of admission) for >80% of patients for ≥1 year; this was associated with a 10% (95%CI: −15%, −4%) lower mortality in these hospitals. Hospitals with an anaesthetic lead for hip fracture care, with time specified for this role in their job plan, had a 7% (95%CI: −13%, −1%) lower 30-day mortality. Those able to report reoperation rates after hip fracture surgery had 8% lower mortality than hospitals reporting zero reoperations or providing no data. Local awareness of post-operative duration of physiotherapy was associated with a higher 30-day mortality. Hospitals (n = 112) where the BPT qualifier ‘physiotherapy assessment’ was reported as being achieved 100% of the time had higher mortalities (and longer LOS, Table S3). In total, 103 hospitals reported discussion of patient experience feedback, and this element of clinical governance was the strongest independent factor associated with mortality, being associated with 10% (95%CI: −15%, −5%) lower mortality. Notably, physiotherapist attendance at clinical governance meetings was associated with 6% lower mortality.
Figure 2.
The association between organisational factors and mortality at 30 days, after accounting for patient case-mix. Organisational factors adjusted for case-mix (age, sex, ASA classification, hip fracture type, pre-fracture residence and pre-fracture mobility) and mutually adjusted for all backward selected factors reported in Supplementary Table S3. Factors with P-value < 0.1 shown. N = 178,757.
Organisational factors associated with 30-day readmissions
Hospitals with busier EDs had increased readmissions; every additional 1,000 monthly (all cause) ED admissions was associated with a 3% (95%CI: 2%, 5%) increase in hip fracture patient readmissions (Figure 3, Table S5). Hospitals with a preoperative fluid management protocol had on average 12% (95%CI: −22%, −1%) fewer readmissions. Perioperatively, orthopaedic staffing was important; hospitals with >26 full-time non-consultant grade doctors (i.e. staff grades and/or junior doctors) had on average 7% (95%CI: −12%, −2%) fewer readmissions. Post-operatively, hospitals able to provide data regarding the time between discharge and initiation of community therapy (n = 50) saw on average 17% (95%CI: −24%, −9%) fewer readmissions. As with mortality, those hospitals able to provide physiotherapy audit data on whether patients would receive physiotherapy in their 1st week post-operatively had a trend towards higher readmissions. In terms of governance, hospitals reporting plans in place to reconfigure local hip fracture services had lower readmissions. However, clinical governance meeting attendance by orthopaedic departmental managers was associated with 4% higher readmissions (95%CI: 0, 8%), as was discussion of morbidity and mortality with 7% higher readmissions (95%CI: 1%, 13%).
Discussion
Main findings
We have identified multiple organisational-level factors throughout the hip fracture care pathway, many potentially amenable to change, which are associated with important clinical outcomes. The ability to mobilise >90% of patients by the day after surgery was associated with substantially shorter superspell LOS. Discussion of feedback from patients about their hospital experience at clinical governance meetings was associated with a similar (10%) lower 30-day mortality as was seen in centres providing prompt surgery (within 36 hours of admission) to >80% of patients. Hospitals able to report time between discharge and community therapy start-up had on average 17% fewer readmissions.
Comparison with other literature
Hip fracture clinical governance was strongly associated with all outcomes. The strong association between routine review of patient experience feedback at governance meetings and mortality may be explained by other unmeasured characteristics. The Friends and Family Test (FFT) was rolled-out across the NHS in 2014 as a system for providing patient experience feedback [16, 17], producing over 75 million pieces of feedback to date; it is the largest source of patient feedback worldwide [18]. It may be that teams prepared to put time aside to examine their patients’ experience are motivated to improve services. The association may also reflect the original intention of FFT that time taken to listen to patient views helps identify what in a service works well and what can be improved upon and how this might be achieved [18]. Planning to reconfigure services may similarly serve as a marker of active interest in improvement of services, and this too was associated with improved patient readmission outcomes.
The ability to get people out of bed promptly after surgery was the strongest predictor of hospital stay, with a clear dose–response. Prompt mobilisation reduces LOS [19] and mortality [20]. Extrapolating our rates, we estimate that if all hospitals could mobilise >90% of patients by the day after surgery, this would save 16,550 bed-days/year nationally. Prompt orthogeriatric assessment was associated with shorter LOS. Hitherto studies have focussed on the effect of single organisational factors across hospitals, for example showing interventions such as increased orthogeriatrician involvement reduces mortality [21, 22]. Only one previous study attempted to compare multiple aspects of the hip fracture care pathway simultaneously to identify the most important targets for intervention. Using 1 year of data, authors assessed hospital-level factors associated with 30-day mortality and overall LOS (rather than superspell in our study); hospitals involved in research trials had lower mortality, and hip fracture admission volume, and inpatient bed and theatre availability all predicted LOS [23]. However, only hospital-level aggregated outcomes were included in a univariable analysis, without adjusting for patient case-mix or other competing factors that our study included [23].
Since the introduction of BPT in 2010, mortality, readmissions and LOS have improved in England (compared with Scotland where no tariffs apply) [24]. The BPT financially incentivises timely geriatrician assessment (within 72 hours) and assessments addressing physiotherapy, falls risk, bone health, cognition and nutrition [5]. The tariff also incentivises timely operation (within 36 hours), which we found had a strong association with lower 30-day mortality, consistent with other studies [24, 25]. If the prompt surgery rates achieved in the best category (>80%) were generalised to all hip fracture patients, we estimate that 182 excess deaths within 30-days could be avoided in England and Wales each year. Unlike time-to-surgery, case definitions for physiotherapy assessment (associated with higher mortality) and nutrition assessment (associated with longer LOS) are non-specific; ‘assessment’, a process measure is open to interpretation and is not a delivered ‘intervention’. We speculate some units reporting 100% compliance are simply ‘ticking a BPT box’ and not actioning assessment as thoroughly as other units that report more realistic figures. Hospitals submitting data on reoperation rates had lower mortality, potentially indicating organised services more able to audit surgical outcomes.
The 2017 physiotherapy audit of hip fracture practice found that 79% of patients waited over a week for rehabilitation to begin at home following discharge [26]. It is therefore not surprising that we found hospitals that showed understanding of delays between discharge and initiation of community therapy had substantially fewer readmissions, as this knowledge would contribute to risk mitigation when discharge planning [27]. We estimate 890 excess readmissions/year might be avoided in England and Wales if hospitals not providing these data were able to do so.
Our finding that hospitals investing in job-planned anaesthetic leadership for hip fracture care had lower 30-day mortality further supports the importance of anaesthetic practices. Use of femoral or fascia-iliaca nerve blocks pre-surgery reduces opiate analgesic use and associated side-effects, reducing delirium [28], and in our analyses was associated with reduced LOS. However, in 2020, nationally only 60% of hip fracture patients received a nerve block, with use varying from 2% to 98% between hospitals [6]. Consistent with our findings, in Canada variation in nerve block use is explained by structures and processes at the hospital and anaesthetist level, rather than by patient-specific factors [29]. We cannot be sure whether the benefits we observe reflect the direct effects of nerve block intervention or indirect effects of better organised anaesthetic services.
Strengths and limitations
We used a unique linkage of national databases for NHS-treated patients across two nations, with 18 different organisational data sources. The 3-year study period allowed for temporal fluctuations giving representative overall estimates for each hospital. Multilevel analysis, accounting for within-hospital clustering, enabled a true hospital-level assessment of associations. Large sample sizes can generate associations that appear important statistically, which may not be clinically meaningful and are prone to type 1 error. Causality cannot be inferred from these observational data and despite our multivariable models there may still be trust-level residual confounding. There is also the risk of the ecological fallacy, so that protective factors that operate at a trust level may not apply at an individual level, e.g. preoperative nerve block. However, many of these organisational factors are ecological in nature, e.g. governance procedures, and would apply to all patients within a trust. Consistent with other studies, the discriminatory abilities of models for all outcomes were improved by the addition of case-mix adjustment, and organisational factors explained minimal amounts of between-hospital variation, with the remaining variation potentially explained by unobserved patient- or hospital-level factors, or patient factors associated with organisational factors [30]. Whilst these organisational factors were derived from high-quality NHFD and other publicly available audits and NHS data, these could not be independently validated. Some audits were troubled by missing data, such that some variables could not be used, meaning some components of the care pathway could not be operationalised, and remain unmeasured. Other audits with fewer missing data required inclusion of a missing category or were supplemented with data from available years. Outcomes were limited as patient-reported outcomes collected at this scale are not available. Our study population includes patients with a first hip fracture during the 3-year study period, who may be expected to be healthier than those who went on to have a second hip fracture during this period, which we did not examine. Had all hip fractures been included, mortality, LOS and readmissions would likely have been higher, and certain organisational factors, such as orthogeriatrician input, may have been associated with greater benefits than reported here. Stepwise selection may detect coincidental associations whilst missing some causal associations; multilevel models made bootstrapping too computationally intensive to provide internal validation.
Conclusions
Hip fractures are a devastating injury, for which health care should be reliable and equitable, across the country. We have identified multiple, potentially modifiable, organisational-level factors associated with important clinical outcomes. Our findings, if causal, support performance incentives if they promote time-specific ‘outcome measures’ for orthopaedic surgery and post-operative mobilisation. Our results highlight the importance of well-embedded, multi-disciplinary clinical governance systems and favour consideration of incentivisation of routine review of patient experience feedback in monthly governance meetings.
Supplementary Material
Acknowledgements
Professor Rachael Gooberman-Hill for her valued inputs in the conception of the study, securing funding and study organisation. Dr Jenny Neuburger for providing code to assist with cleaning, merging and deriving HES-ONS-NHFD-PEDW datasets. Transparency Statement: C.L.G. affirms that the manuscript is an honest, accurate and transparent account of the study being reported that no important aspects of the study have been omitted and that any discrepancies from the study as originally planned have been explained.
Contributor Information
Rita Patel, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK.
Andrew Judge, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK; Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, UK; NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol, UK.
Antony Johansen, Division of Population Medicine, School of Medicine, Cardiff University and University Hospital of Wales, Cardiff, UK; National Hip Fracture Database, Royal College of Physicians, London, UK.
Elsa M R Marques, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK; NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol, UK.
Jill Griffin, Clinical & Operations Directorate, Royal Osteoporosis Society, Bath, UK.
Marianne Bradshaw, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK.
Sarah Drew, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK.
Katie Whale, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK; NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol, UK.
Tim Chesser, Department of Trauma and Orthopaedics, Southmead Hospital, North Bristol NHS Trust, Bristol, UK.
Xavier L Griffin, Barts Bone and Joint Health, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, London, UK; Royal London Hospital, Barts Health NHS Trust, London, UK.
Muhammad K Javaid, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, UK.
Yoav Ben-Shlomo, Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK.
Celia L Gregson, Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK; Older People’s Unit, Royal United Hospital NHS Foundation Trust Bath, Combe Park, Bath, UK.
Data Sharing
Linked data are available through data applications to Royal College of Physicians Falls and Fragility Fracture Audit Programme and Healthcare Quality Improvement Partnership, NHS Wales Informatics Service and NHS Digital.Data Declaration: This publication is based on data collected by or on behalf of the Healthcare Quality Improvement Partnership, who have no responsibility or liability for the accuracy, currency, reliability and/or correctness of this publication.
Declaration of Sources of Funding
This work is funded by Versus Arthritis (reference 22086). This study is supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. M.K.J. is supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). The views expressed are those of the author(s) and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
Declaration of Conflicts of Interest
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare no support from any organisation for the submitted work; A.Jo. is the clinical lead for the National Hip Fracture Database, at the Royal College of Physicians, London. T.C. is the past British Orthopaedic Association (BOA) representative and previously sat on the board of the Falls and Fragility Fracture Audit Project (which includes the National Hip Fracture Database), he helped set up and perform many of the BOA multidisciplinary peer reviews for hip fractures, he has design and educational contracts with Stryker, Acumed and Swemac. M.K.J. has received honoraria, unrestricted research grants, travel and/or subsistence expenses from: Amgen, Consilient Health, Kyowa Kirin Hakin, UCB, Abbvie and Besin healthcare. EMRM has received research funding from CeramTec UK limited. A.Ju. has received consultancy fees from Freshfields, Bruckhaus, Derringer and Anthera Pharmaceuticals Ltd. J.G. has an educational contract with Stryker; no other relationships or activities that could appear to have influenced the submitted work.
References
- 1. Health and Social Care Information Centre . HES Data Dictionary: Admitted Patient Care. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-episode-statistics-for-admitted-patient-care-outpatient-and-accident-and-emergency-data:2017.
- 2. Griffin XL, Parsons N, Achten J, Fernandez M, Costa ML. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick hip trauma evaluation--a prospective cohort study. Bone Joint J 2015; 97-B: 372–82. [DOI] [PubMed] [Google Scholar]
- 3. Royal College of Physicians . National Hip Fracture Database (NHFD) annual report 2017. London: RCP London, 2017. https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/reports2017. [Google Scholar]
- 4. The NHS Information Centre . Emergency readmissions 2010–11 summary. https://www.gov.uk/government/publications/emergency-readmissions-data: Department of Health, London. 2013. [Google Scholar]
- 5. Consultation on 2021/22 National Tariff Payment System . Annex DtC: Guidance on best practice tariffs. https://improvement.nhs.uk/documents/484/Annex_DtD_Best_practice_tariffs.pdf(accessed 18 November 2020). 2021.
- 6. Royal College of Physicians . Facing new challenges — the NHFD report on 2020 (January–December 2020). London: RCP, 2021. https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/reports2021. [Google Scholar]
- 7. Royal College of Physicians . National Hip Fracture Database (NHFD) annual report 2019. London: RCP, 2019. https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/reports2019. [Google Scholar]
- 8. National Institute for Health and Care Excellence (NICE) . Hip fracture in adults: Quality standard [QS16]. Manchester: NICE, 2017. https://www.nice.org.uk/Guidance/QS16. [Google Scholar]
- 9. Scottish Intercollegiate Network (SIGN) . SIGN Guidelines 111 Management of Hip Fracture in Older People. Available athttps://wwwsignacuk/our-guidelines/. 2010.
- 10.Royal College of Physicians: National Hip Fracture Database (NHFD) https://www.rcplondon.ac.uk/projects/national-hip-fracture-database-nhfd(accessed 18 November 2020).
- 11. NHS Digital . Linked HES-ONS mortality data. 2018(25 May 2018). Available at:https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/linked-hes-ons-mortality-data.
- 12. Patel R, Drew S, Johansen Aet al. REducing unwarranted variation in the delivery of high qUality hip fraCture services in England and Wales (REDUCE): protocol for a mixed-methods study. BMJ Open 2021; 11: e049763. 10.1136/bmjopen-2021-049763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Royal College of Physicians: National Hip Fracture Database (NHFD) 2019 annual report: methods used for statistical analysis at https://www.nhfd.co.uk/files/2019ReportFiles/NHFD_Statistical_Methods_Update_2019.pdf.
- 14. American Society of Aneshthesiology . New classification of physical status. Anesthesiology 1963; 24: 111. [Google Scholar]
- 15. Vandenbroucke JP, Von Elm E, Altman DGet al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 2007; 4: e297. 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Davis R. How the friends and family test is conveyed to the public should be reconsidered. BMJ 2013; 347: f5158. 10.1136/bmj.f5158. [DOI] [PubMed] [Google Scholar]
- 17. Kmietowicz Z. Critics question whether "friends and family" test in NHS is fit for prime minister's purpose. BMJ 2013; 346: f83. 10.1136/bmj.f83. [DOI] [PubMed] [Google Scholar]
- 18. NHS England : Friends and Family Test. https://www.england.nhs.uk/fft/.
- 19. Goubar A, Ayis S, Beaupre Let al. The impact of the frequency, duration and type of physiotherapy on discharge after hip fracture surgery: a secondary analysis of UK national linked audit data. Osteoporos Int 2022; 33: 839–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ferris H, Brent L, Coughlan T. Early mobilisation reduces the risk of in-hospital mortality following hip fracture. Eur Geriatr Med 2020; 11: 527–33. [DOI] [PubMed] [Google Scholar]
- 21. Neuburger J, Currie C, Wakeman Ret al. Increased orthogeriatrician involvement in hip fracture care and its impact on mortality in England. Age Ageing 2017; 46: 187–92. [DOI] [PubMed] [Google Scholar]
- 22. Moyet J, Deschasse G, Marquant B, Mertl P, Bloch F. Which is the optimal orthogeriatric care model to prevent mortality of elderly subjects post hip fractures? A systematic review and meta-analysis based on current clinical practice. Int Orthop 2019; 43: 1449–54. [DOI] [PubMed] [Google Scholar]
- 23. Farrow L, Hall AJ, Ablett AD, Johansen A, Myint PK. The influence of hospital-level variables on hip fracture outcomes. Bone Joint J 2021; 103-B: 1627–32. [DOI] [PubMed] [Google Scholar]
- 24. Metcalfe D, Zogg C, Judge Aet al. Pay for performance and hip fracture outcomes: an interrupted time series and difference-in-differences analysis in England and Scotland. Bone Joint J 2019; 101-B: 1015–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Klestil T, Roder C, Stotter Cet al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep 2018; 8: 13933. 10.1038/s41598-018-32098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Royal College of Physicians . Recovering after a hip fracture: helping people understand physiotherapy in the NHS. Physiotherapy ‘hip sprint’ audit report 2017. London: RCP, 2018. https://www.rcplondon.ac.uk/projects/outputs/recovering-after-hip-fracture-helping-people-understand-physiotherapy-nhs. [Google Scholar]
- 27. Papanicolas I, Riley K, Abiona Oet al. Differences in health outcomes for high-need high-cost patients across high-income countries. Health Serv Res 2021; 56: 1347–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lim EJ, Koh WU, Kim H, Kim HJ, Shon HC, Kim JW. Regional nerve block decreases the incidence of postoperative delirium in elderly hip fracture. J Clin Med 2021; 10. 10.3390/jcm10163586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McGinn R, Talarico R, Hamiltoon GMet al. Hospital-, anaesthetist-, and patient-level variation in peripheral nerve block utilisation for hip fracture surgery: a population-based cross-sectional study. Br J Anaesth 2022; 128: 198–206. [DOI] [PubMed] [Google Scholar]
- 30. Gutacker N, Bloor K, Bojke C, Walshe K. Should interventions to reduce variation in care quality target doctors or hospitals? Health Policy 2018; 122: 660–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.