Abstract
Background
We indirectly compared the effects of immune checkpoint inhibitors alone (ICI) and ICI-combined chemotherapy (chemo-ICI) in patients with non-small cell lung cancer who had high programmed death-ligand 1 (PD-L1) expression (defined as tumour proportion score ≥50% or TC3/IC3) through network meta-analyses.
Methods
Through literature searches, we shortlisted 22 randomised controlled trials encompassing 4289 patients, with objective response rate (ORR), progression-free survival (PFS), and overall survival (OS) set as the primary outcomes. The dichotomous data for ORR and hazard ratios (HRs) and their 95% confidence intervals (CIs) for OS and PFS were extracted.
Results
We found that chemo-ICI had significantly improved ORR (OR 1.7, 95% CI 1.1–2.5) and PFS (HR 0.59, 95% CI: 0.48–0.74) relative to ICI. Although no significant difference in OS was observed, the analyses revealed that the chemo-ICI patients tended to undergo fewer progression events than ICI patients (HR 0.82, 95% CI 0.6–1.1). In subgroup analysis, the non-squamous, PD-1 inhibitor and first-line treatment cohorts exhibited significant differences in ORR and PFS, but not in OS. However, in the squamous, PD-L1 inhibitor, and previously treated cohorts, PFS, OS and ORR were not different between chemo-ICI and ICI patients.
Conclusions
In conclusion, for non-squamous NSCLC patients, accepting PD-1 as the first-line treatment may be a relatively better option.
Subject terms: Non-small-cell lung cancer, Cancer immunotherapy
Introduction
Lung cancer is the major cause of cancer-related deaths worldwide [1]. Non-small cell lung cancer (NSCLC) accounts for 85% of primary lung cancer, while squamous carcinoma accounts for nearly two-thirds of all NSCLC cases [2]. With the advancement in the research on NSCLC, a variety of treatment methods for corresponding mechanisms are being developed, which has contributed to gradually refining the treatment of NSCLC. For patients with NSCLC who had EGFR or ALK mutations, targeted therapy or chemotherapy is mostly used as the first-line therapy [3]. However, for those without EGFR or ALK mutations, chemotherapy remains the first-line therapy. With the wide adoption of immunotherapy, several new options have become available as the first-line treatment for patients with NSCLC, including the research on immune checkpoint inhibitors (ICIs) as the most matured and commonly used option [4].
PD-1 and PD-L1 inhibitors are the most widely used ICIs in the treatment of NSCLC. Particularly, several clinical studies have reported the efficacy of ICIs or ICI-combined chemotherapy (chemo-ICI) for the treatment of patients with NSCLC who had high programmed death-ligand 1 (PD-L1) expression [5–15]. These clinical trials define high PD-L1 expression as a tumour proportion score (TPS) of >50% or TC3/IC3. For example, KEYNOTE 024 indicated that the use of ICI alone had better efficacy than chemotherapy, in patients with NSCLC who had high programmed death-ligand 1 (PD-L1) expression [16]. In addition, subgroup analysis of the high PD-L1 expression NSCLC cohort in KEYNOTE 407 confirmed the effectiveness of immune checkpoint inhibitors combined with chemotherapy (chemo-ICI) [5]. Recently, RATIONALE 307 [17] and ORIENT-11 [18] established the clinical efficacy of Tislelizumab combined chemotherapy and Sintilimab combined chemotherapy, respectively. Empower Lung-1 proved the efficacy of Cemiplimab monotherapy [14].
However, head-to-head randomised controlled trials (RCTs) comparing ICI and chemo-ICI are lacking. Therefore, we adopted the NMA-based approach to compare the effect of ICI versus chemo-ICI in patients with NSCLC who had high PD-L1 expression [9]. Meanwhile, we also conducted some subgroup analyses to explore whether other factors contributed to the efficacy. Subgroup analysis was conducted according to the treatment lines across the entire cohort. Subgroup analysis by histological type was also performed. Furthermore, PD-1 and PD-L1 inhibitors were categorised for subgroup analysis.
Methods
Search strategies
We searched all RCTs related to NSCLC from PubMed, Cochrane Library, Embase, and other databases from inception until March 2021, with no start data limit applied. In addition, we also performed a manual search for the reference lists across all available original studies, reviews, and meeting reports from the main international lung cancer meetings. The keywords used to search included: “non-small cell lung cancer”, “non-squamous lung cancer”, “nivolumab”, “pembrolizumab”, “atezolizumab”, “PD-1 inhibitor”, “PD-L1 inhibitor”, “programmed cell death-Ligand 1”, “cemiplimab” and others (Supplemental Methods). The language the RCTs used was limited to English. Two authors accomplished the search independently, and any discrepancy was figured out by mutual discussion to reach a consensus.
Selection criteria
According to the PICOS framework, papers that conformed to the following criteria were included: (I) only NSCLC patients, representative of high PD-L1 expression cohort. (II) Studies that included the ICI cohort and chemotherapy cohort or included the Chemo-IC cohort and the chemotherapy cohort. (III) Studies that included a comparison of the ICI cohort with the chemotherapy cohort or chemo-ICI cohort with the chemotherapy cohort. (IV) Studies that reported outcomes including more than one of the following: ORR, PFS, OS and hazard ratios (HRs) and their 95% confidence intervals (CIs) for OS and PFS. (V) Studies that were all RCTs.
The following were the exclusion criteria: (I) Patients who had previously undergone systemic immunosuppressive therapy or active autoimmune disease. (II) Studies that included trials with radiotherapy as an intervention. (II) Case–control studies, retrospective studies, cohort studies, case reports, meta-analyses and systematic reviews were excluded.
Data extraction
Two authors independently examined the title, summary, full text and supplementary materials to evaluate the eligibility and collect data from the included papers. The data were extracted into a spreadsheet. The data extracted for critical appraisal included the country clinical trial number, year of publication, first author, intervention, study stage, the number of patients in each group, and participant characteristics (if any). In addition, data on OS, PFS and ORR were extracted on a spreadsheet; it also included HRs and their 95% CIs for OS and PFS. Similarly, dichotomous ORR data were clustered. We treated the items as NR (not reported) if any of the categories above were not reported data in the RCTs.
Quality assessment
The Cochrane Collaboration’s Risk of Bias tool was used to evaluate the methodological quality of the included RCTs. Factors such as randomness, double-blindness, the integrity of the outcome data, and bias in selective reporting were evaluated. The risk of bias was assessed according to the following criteria: low risk, high risk and ambiguous risk. The two authors completed this work independently and resolved all disputes by discussion.
Statistical analysis
The HRs for PFS and OS as well as odds ratios (ORs) for ORR were primary endpoints in this network meta-analyses. A Bayesian approach was accordingly adopted. The survival analysis of PFS and OS were presented as HRs and their 95% CIs. ORR were treated as dichotomous variables; therefore, odds ratios (ORs) were used to present these parameters. We used the χ2 test and I2 statistics to evaluate the statistical heterogeneity of the included studies. A fixed-effects model would be selected to count the pooled estimate, if the P value for χ2 > 0.1 and I2 was <50% [19]. If not, a random-effects model would be used to combine the studies. When I2 statistic >50% or P value for χ2 < 0.1, it would be considered to be statistically significant for heterogeneity. It would be considered no statistically significant difference when the 95% CI for indirect comparison comprised 1. Chemotherapy (arm C) was used as the common therapeutic arm in this adjusted indirect comparison. This network meta-analysis indirectly evaluated the relative efficacy of ICI versus chemo-ICI, via comparing ICI (arm A) with chemotherapy (arm C) and chemo-ICI (arm B) with chemotherapy (arm C) [20]. The following formula was used to estimate the result of log HR: log HRAB = log HRAC − log HRBC. The log HR of the regulated indirect comparison between arm A and arm B was presented as log HRAB. Similarly, the log HR of the regulated indirect comparison between arm A and arm C was presented as log HRAC, while the log HR of regulated indirect comparison between arm B and arm C was presented as log HRBC. The formula: SE (log HRAB) = √SE(log HRAC)2 + SE(log HRBC)2 was used to estimate standard error (SE) [20]. ORs and the corresponding SEs were similarly calculated. The Bayesian network meta-analysis estimated the relative treatment effects by HRs and their 95% CI values. The treatment effects ranking of all comparison variables (PFS, OS and ORR) indicated the possibilities. For each upshot, three Markov chains with dissimilar starting values were run in parallel for 100,000 iterations, and each chain used a thinning interval of 10 and 10,000 burn-ins. The NMA computed the possibilities of each therapy being the best among all therapies by ranking the effects of all therapies in each iteration and then calculating the percentage of each therapy being ranked first across all iterations (where, 0 = a therapy that is certain to be the worst, 1 = a therapy that is certain to be the best). Subgroup analyses were conducted according to the treatment lines across the entire cohort. Non-squamous or squamous NSCLC and PD-1 inhibitor or PD-L1 inhibitor were also categorised for subgroup analyses. Based on the pre-arranged grouping factors, we collected the data of relevant subgroups in all included trials. We used the funnel plot and Eegg and Bgger tests to evaluate publication bias. All statistical analyses were executed using the R (version 4.0.5) and R Studio software. Gemtc package contributed to the statistical analyses.
Results
Studies included in the meta-analysis
We searched 11,459 associated publications in the beginning, and all of these were from ClinicalTrials.gov and contained conference abstracts. Subsequently, 3272 publications were removed because of duplicates, and 8187 articles were screened. After reading the titles, 8024 articles were excluded because of unrelated topics. Upon scrutinising the abstracts of the remaining 163 articles, we eliminated 34 systematic reviews, 68 retrospective studies, and 29 meta-analyses. After examining the full text, 32 articles were finally evaluated for eligibility. Among these, six trials lacked the high PD-L1 expression group and another six trials had unexpected interventions, including ipilimumab and bevacizumab. In the end, 22 RCTs were included in this NMA. The selection flowchart for the searched articles is presented in Supplemental Fig. 1. Among the 22 RCTs, 11 were related to ICI alone versus chemotherapy (n = 3113 patients) and 11 were on chemo-ICI (n = 1176 patients). Of the 11 RCTs that involved ICI intervention, 4 were on atezolizumab, 3 were on pembrolizumab, 1 was on avelumab, 1 was on cemiplimab, 1 was on durvalumab, and 1 was on nivolumab. In the 11 RCTs that had a chemo-ICI intervention, 3 were on chemo-pembrolizumab, 2 were on chemo-atezolizumab, 2 were on chemo-tislelizumab, 2 were on chemo-sintilimab, and 2 were on chemo-camrelizumab. The risk assessed by the risk of bias evaluation was within acceptable limits. The primary baseline characteristics of the 14 applicable studies are described in Table 1.
Table 1.
Primary characteristics and the results of the applicable studies.
| Study | Year | Fiest-authour | Treatment | PD-L1/PD-1 | Number of events/Number of patients | ORR | PFS HR 95% CI | OS HR 95% CI |
|---|---|---|---|---|---|---|---|---|
| keynote-010-1 [26] | 2016 | Roy S Herbst | ICI | PD-1 | 42/139 | 30.2 | 0.59 (0.44–0.78) | 0.54 (0.38–0.77) |
| chemotherapy | 12/152 | 7.9 | ||||||
| keynote-010-2 [26] | 2016 | Roy S Herbst | ICI | PD-1 | 44/151 | 29.1 | 0.59 (0.45–0.78) | 0.50 (0.36–0.70) |
| chemotherapy | 12/152 | 7.9 | ||||||
| keynote-021 | 2016 | Corey J Langer | ICI + chemo | PD-1 | 16/20 | 80 | NR | NR |
| chemotherapy | 6/17 | 35 | ||||||
| keynote-024 | 2016 | Martin Reck | ICI | PD-1 | 69/154 | 44.8 | 0.50 (0.37–0.68) | 0.60 (0.41–0.89) |
| chemotherapy | 42/151 | 27.8 | ||||||
| keynote-042 | 2019 | Tony SK Mok | ICI | PD-1 | 118/229 | 39 | 0.81 (0.67–0.99) | 0.69 (0.56–0.85) |
| chemotherapy | 96/300 | 32 | ||||||
| keynote-407 | 2020 | Luis Paz-Ares | ICI + chemo | PD-1 | 44/73 | 60.3 | 0.37 (0.24–0.58) | 0.64 (0.37–1.10) |
| chemotherapy | 24/73 | 32.9 | ||||||
| IMpower110 | 2020 | Roy S Herbst | ICI | PD-L1 | 41/107 | 38.3 | 0.63 (0.45–0.88) | 0.59 (0.40–0.89) |
| chemotherapy | 28/98 | 28.6 | ||||||
| IMpower130 | 2019 | Howard West | ICI | PD-L1 | NR/88 | NR | 0.51 (0.34–0.77) | 0.84 (0.51–1.39) |
| chemotherapy | NR/42 | NR | ||||||
| IMpower 131 | 2020 | Robert Jotte | ICI + chemo | PD-L1 | 29/47 | 61.7 | 0.44 (0.27–0.71) | 0.48 (0.29–0.81) |
| chemotherapy | 14/44 | 31.8 | ||||||
| IMpower 132 | 2020 | Makoto Nishio | ICI + chemo | PD-L1 | 18/25 | 72 | 0.46 (0.22–0.96) | 0.73 (0.31–1.73) |
| chemotherapy | 11/20 | 55 | ||||||
| IMpower189 [27] | 2020 | L Gandhi | ICI + chemo | PD-1 | 81/132 | 61.4 | 0.36 (0.26–0.51) | 0.42 (0.26–0.68) |
| chemotherapy | 16/70 | 22.9 | ||||||
| CheckMate 026 [28] | 2017 | DP Carbone | ICI | PD-1 | 35/88 | 34 | 1.07 (0.77–1.49) | 0.90 (0.63–1.29) |
| chemotherapy | 49/126 | 39 | ||||||
| Camel | 2020 | Caicun Zhou | ICI + chemo | PD-1 | NR/30 | NR | 0.39 (0.14–0.99) | NR |
| chemotherapy | NR/20 | NR | ||||||
| Camel-sq | 2021 | Caicun Zhou | ICI + chemo | PD-1 | NR/37 | NR | 0.30 (0.17–0.55) | 0.48 (0.21–1.12) |
| chemotherapy | NR/44 | NR | ||||||
| Empower-lung 1 | 2021 | Ahmet Sezer | ICI | PD-1 | 111/283 | 39 | 0.54 (0.43–0.68) | 0.57 (0.42–0.77) |
| chemotherapy | 57/280 | 20 | ||||||
| JAVELIN Lung 200 | 2018 | Fabrice Barlesi | ICI | PD-L1 | 42/168 | 25 | 0.65 (0.49–0.88) | 0.67 (0.51–0.89) |
| chemotherapy | 15/147 | 10 | ||||||
| MYSTIC [15] | 2020 | Naiyer A Rizvi | ICI | PD-L1 | NR/118 | NR | 0.76 (0.55–1.04) | 0.76 (0.55–1.04) |
| chemotherapy | NR/107 | NR | ||||||
| OAK | 2016 | Achim Rittmeyer | ICI | PD-L1 | 22/72 | 30.6 | 0.63 (0.43–0.91) | 0.41 (0.27–0.64) |
| chemotherapy | 7/65 | 10.8 | ||||||
| ORIENT-11 | 2020 | Yunpeng Yang, MD | ICI + chemo | PD-1 | 73/107 | 68.2 | 0.31 (0.20–0.49) | NR |
| chemotherapy | 24/61 | 39.3 | ||||||
| ORIENT 12 [29] | 2021 | Caicun Zhou, MD, PhD | ICI + chemo | PD-1 | NR/58 | NR | 0.46 (0.30–0.70) | NR |
| chemotherapy | NR/63 | NR | ||||||
| POPLAR | 2016 | Louis Fehrenbacher | ICI | PD-L1 | 9/25 | 37.5 | 0.60 (0.31–1.16) | 0.49 (0.22–1.07) |
| chemotherapy | 3/23 | 13 | ||||||
| RATIONALE 304 [30] | 2021 | Shun Lu, MD, PhD | ICI + chemo | PD-1 | NR/74 | NR | 0.31 (0.17–0.57) | NR |
| chemotherapy | NR/36 | NR | ||||||
| RATIONALE 307-1 | 2021 | Jie Wang, MD, PhD | ICI + chemo | PD-1 | 33/42 | 78.6 | 0.50 (0.28–0.89) | NR |
| chemotherapy | 22/41 | 53.7 | ||||||
| RATIONALE 307-2 | 2021 | Jie Wang, MD, PhD | ICI + chemo | PD-1 | 37/42 | 88.1 | 0.43 (0.23–0.78) | NR |
| chemotherapy | 22/41 | 53.7 |
ICI immune checkpoint inhibitors, ICI + chemo ICI-combined chemotherapy.
Network meta-analysis
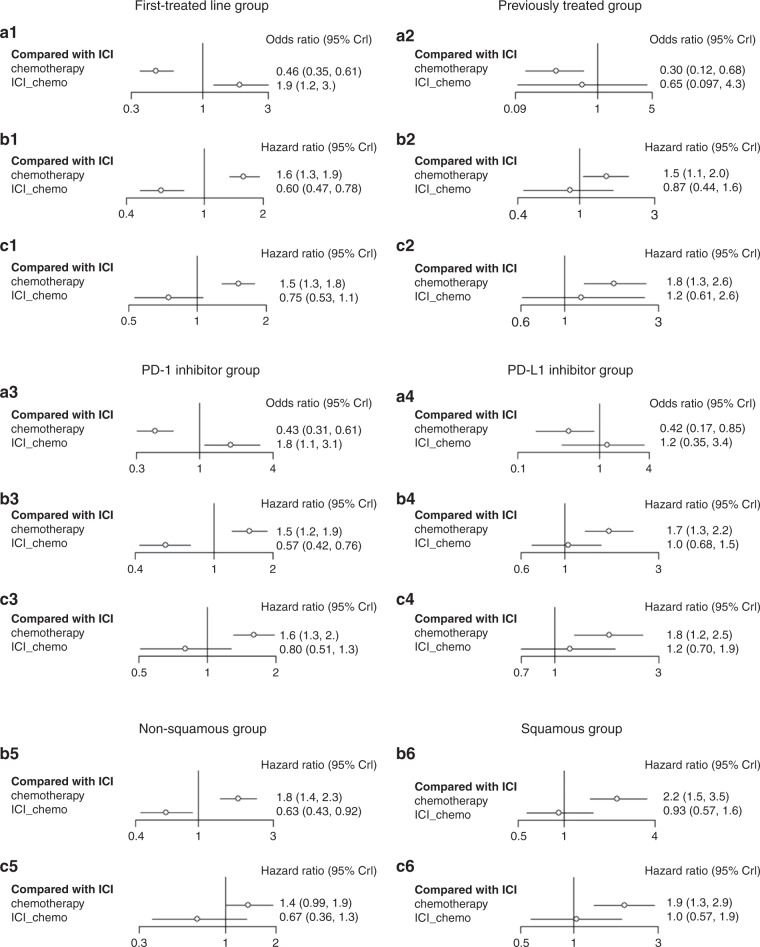
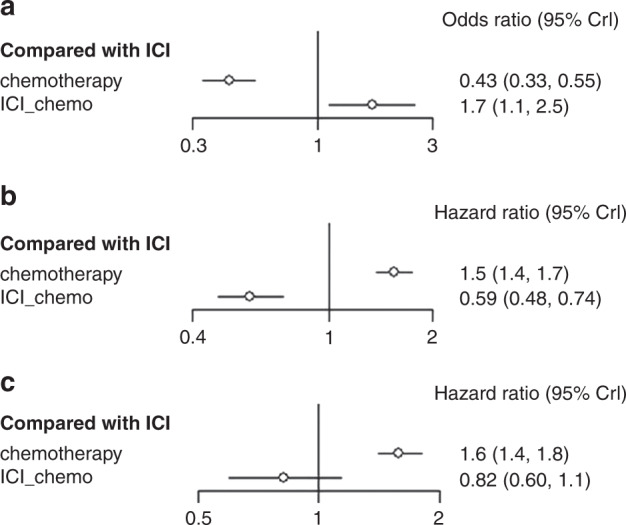
Indirect comparison of ORR
The network plot displays the comparisons between each treatment (Supplemental Fig. 2). The OR was 2.3 (95% CI: 1.8–3.0) for ICI vs chemotherapy and 3.9 (95% CI: 2.8–5.5) for chemo-ICI vs chemotherapy. An indirect comparison between the two treatment protocols revealed that patients receiving chemo-ICI were more likely to respond than those receiving ICI (OR 1.7, 95 % CI 1.1–2.5) (Fig. 1a). When compared with chemotherapy, chemo-ICI exhibited a better effect than ICI (Table 2) in pairwise comparison. In Bayesian ranking, the curves indicated the probability of each treatment being ranked from first to last concerning OR and 95% CI. The chemo-ICI was the most possible therapy to be ranked first (Fig. 2a).
Fig. 1. Forest plot of odds ratio or hazard ratios for ORR, PFS and OS in network meta-analysis.
Forest plots presenting ORR (a) odds ratio analysis and PFS (b) and OS (c) hazard ratio analysis. ICI immune checkpoint inhibitors, chemo-ICI ICI-combined chemotherapy.
Table 2.
Comparative efficacy of treatments for ORR in network meta-analysis.
| Chemotherapy | 2.32 (1.83, 3) | 3.9 (2.78, 5.39) |
| 0.43 (0.33, 0.55) | ICI | 1.67 (1.11, 2.5) |
| 0.26 (0.19, 0.36) | 0.6 (0.4, 0.9) | ICI-chemo |
ICI immune checkpoint inhibitors, ICI-chemo ICI-combined chemotherapy.
Fig. 2. Ranking probabilities base on the multiple comparisons on ORR, PFS and OS in network meta-analysis.
Ranking probabilities on ORR (a), PFS (b), and OS (c) in NSCLC patients with a high PD-L1 expression according to multiple comparisons. ICI immune checkpoint inhibitors, chemo-ICI ICI-combined chemotherapy.
Indirect comparison of PFS
The HRs of PFS in patients with NSCLC who had high PD-L1 expression and were treated with ICI, chemo-ICI, or chemotherapy are shown in Fig. 1. Significant advantages in PFS (HR 0.59, 95% CI: 0.48–0.73) were observed for chemo-ICI over ICI. The Bayesian ranking results indicated the probability of chemo-ICI being ranked first (Fig. 2b). This result suggested that patients with NSCLC who had high PD-L1 expression may showcase more clinical benefit if they received chemo-ICI.
Indirect comparison of OS
The HRs of OS were 0.63 (95% CI: 0.55–0.71) for ICI vs chemotherapy and 0.52 (95% CI: 0.39–0.7) for chemo-ICI vs chemotherapy. Although a significant difference in OS was not observed for chemo-ICI when compared with ICI, an indirect comparison between the two treatment protocols signified that patients receiving chemo-ICI tended to have fewer progression events than those receiving ICI (HR 0.82, 95% CI 0.6–1.1, Fig. 1c). Furthermore, the result was confirmed by the ranking curves described on the basis of the Bayesian ranking results (Fig. 2c).
Subgroup analysis
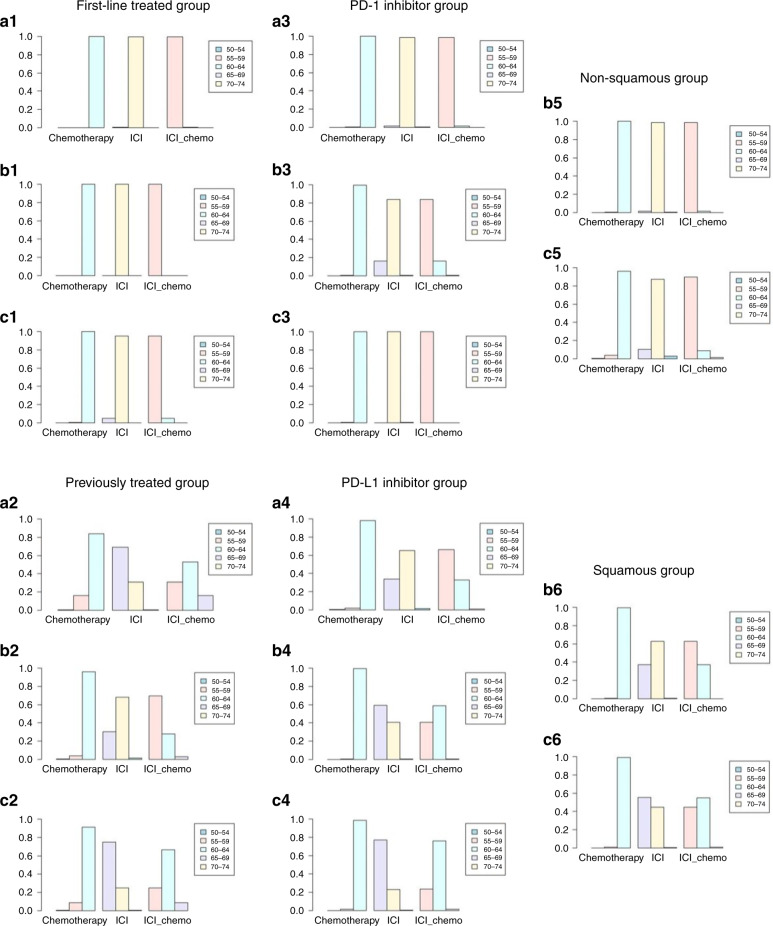
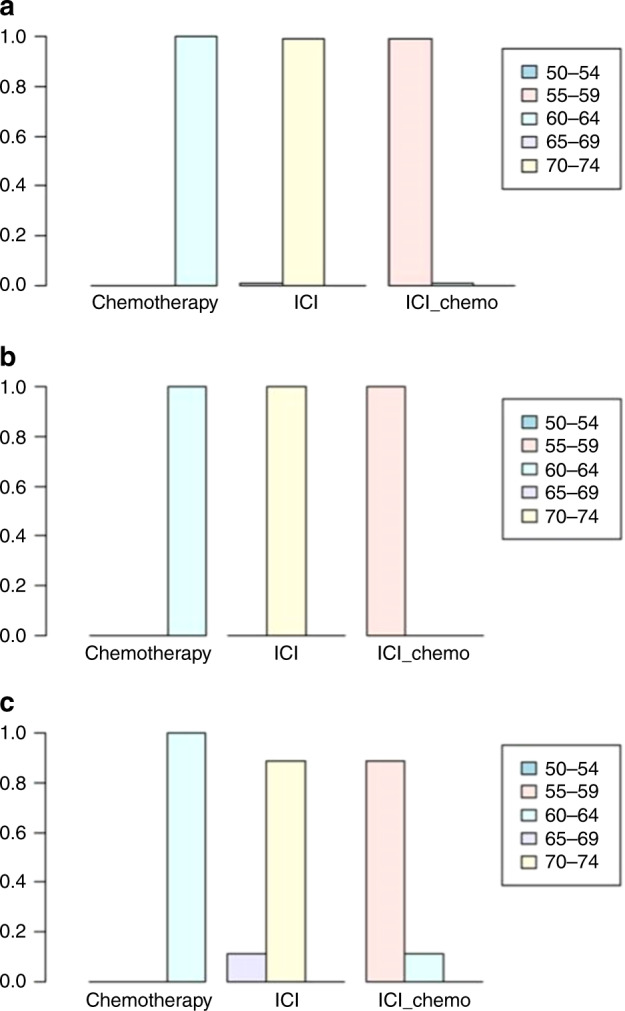
treatment line (first-line treated/previously treated)
In patients with NSCLC who had high PD-L1 expression and received PD-1 as first-line treatment, immense improvements in PFS (HR 0.60, 95% CI 0.47–0.78) and ORR (HR 1.9, 95% CI 1.2–3.0) were evident for chemo-ICI when compared with ICI (Fig. 3). Nonetheless, no significant difference was seen in OS (HR 0.75, 95% CI 0.53–1.1). The probability of each treatment ranking described according to the Bayesian ranking results showed that patients receiving ICI tended to endure more progression events than those receiving chemo-ICI (Fig. 4).
Fig. 3. Forest plot of odds ratio or hazard ratios for ORR, PFS and OS in the subgroup analysis.
Forest plots showing ORR (a1), PFS (b1) and OS (c1) hazard ratio analyses in the first-line treated group, ORR (a2), PFS (b2) and OS (c2) hazard ratio analyses in the previously treated group, ORR (a3), PFS (b3) and OS (c3) hazard ratio analyses in the PD-1 inhibitor group, ORR (a4), PFS (b4) and OS (c4) hazard ratio analyses in the PD-L1 inhibitor group, PFS (b5) and OS (c5) hazard ratio analyses in the non-squamous group and PFS (b6) and OS (c6) hazard ratio analyses in the squamous group. ICI immune checkpoint inhibitors, chemo-ICI ICI-combined chemotherapy.
Fig. 4. Ranking probabilities base on the multiple comparisons on ORR, PFS and OS in the subgroup analysis.
Ranking probabilities based on the multiple comparisons on ORR (a1), PFS (b1) and OS (c1) in the first-line treated group, ORR (a2), PFS (b2) and OS (c2) in the previously treated group, ORR (a3), PFS (b3) and OS (c3) in the PD-1 inhibitor group, ORR (a4), PFS (b4) and OS (c4) in the PD-L1 inhibitor group, PFS (b5) and OS (c5) in the non-squamous group and PFS (b6) and OS (c6) in the squamous group. ICI immune checkpoint inhibitors, chemo-ICI ICI-combined chemotherapy.
In patients with NSCLC who had high PD-L1 expression and were treated previously, PFS, OS and ORR were not different between chemo-ICI and ICI (Fig. 3). Based on the Bayesian ranking results, the probability of each treatment ranking further confirmed this result (Fig. 4).
PD-1 inhibitor/PD-L1 inhibitor
In patients with NSCLC who had high PD-L1 expression and were treated with a PD-1 inhibitor, significantly improved PFS (HR 0.63, 95% CI 0.43–0.92) and ORR (HR 1.8, 95% CI 1.1–3.1) were noticed in chemo-ICI when compared with IC (Fig. 3). However, no significant differences were perceived in OS (HR 0.8, 95% CI 0.51–1.3, Fig. 3). According to the Bayesian ranking results, the treatment ranking showed that patients receiving chemo-ICI may have better effects than those receiving ICI (Fig. 4).
In patients with NSCLC who had high PD-L1 expression and were treated with a PD-L1 inhibitor, PFS, OS and ORR were not different between chemo-ICI and ICI (Fig. 3). Furthermore, the results were presented based on the probability of each treatment ranking (Fig. 4).
Histological type (non-squamous/squamous)
In patients with non-squamous NSCLC who had high PD-L1 expression, chemo-IC was conspicuously superior to ICI in terms of PFS (HR 0.63, 95% CI 0.43–0.92). However, no significant difference in OS was noted (HR 0.67, 95% CI 0.36–1.3, Fig. 3). The probability of each treatment ranking described in accordance with the Bayesian ranking results demonstrated that chemo-ICI tended to be a better choice than ICI (Fig. 4).
In patients with squamous NSCLC who had high PD-L1 expression, both PFS and ORR were not different between chemo-ICI and ICI (Fig. 3). The treatment ranking in accordance with the Bayesian ranking results also confirmed this finding (Fig. 4).
Discussion
The results of NMA revealed that chemo-ICI was associated with significantly improved ORR (OR 1.7, 95% CI 1.1–2.5) and PFS (HR 0.59, 95% CI: 0.48–0.73) when compared with ICI. Although significant differences in OS were not observed, an indirect comparison exposed that patients receiving ICI tend to experience more progression events than those receiving chemo-ICI (HR 0.82, 95% CI 0.6–1.1). In subgroup analysis, the non-squamous cohort, PD-1 inhibitor cohort, and first-line treatment cohort exhibited significant differences in ORR and PFS. In the case of OS, the indirect comparison demonstrated that patients receiving chemo-ICI tended to have a better effect than those receiving ICI. Nevertheless, in the squamous cohort, PD-L1 inhibitor cohort, and previously treated cohort, differences in PFS, OS, and ORR were not noted between chemo-ICI and ICI. These results provide instrumental evidence that a more individualised therapy is required in NSCLC.
In our squamous cohort subgroup analysis, we found no significant difference between PFS and OS, which may be attributed to the lack of inclusion of the related RCTs. Only subgroup analysis in impower lung-1 [14] and Keynote 042 [21] showed large examples and both involved studies comparing ICIs with chemotherapy. Hence, the examples of chemo-ICI vs chemotherapy were smaller than those of examples of ICI vs. chemotherapy. Moreover, only keynote 407 and impower 131 reported ORR dates, which were the date of chemo-ICI and chemotherapy, respectively, lacking ORR data of ICI and chemotherapy. The limited example and data may be the partial reason devoted to the results obtained.
In our PD-L1 inhibitor cohort subgroup analysis, we included 8 RCTs but only impower 131 and impower 132 [22] reported the data of chemo-ICI vs chemotherapy, with the examples being 91 and 45, respectively. Hence, the total example of ICI vs chemotherapy was larger than that of chemo-ICI vs chemotherapy. Meanwhile, both impower 131 and impower 132 RCTs compared atezolizumab plus chemotherapy with chemotherapy, while the others compared various ICIs to chemotherapy. These factors may have partially contributed to the unobserved differences in PFS, OS, and ORR.
In 2019, an indirect comparison meta-analysis evaluated the efficacy of pembrolizumab alone versus pembrolizumab combined chemotherapy for the first-line treatment of advanced NSCLC patients with PD-L1 TPS of ≥50%. The meta-analysis indicated that, for patients with NSCLC and high PD-L1 expression, the use of pembrolizumab combined chemotherapy as the first-line treatment may have had a better effect than that with pembrolizumab alone (ORR RRpem + chemo/pem 1.62, 95% CI 1.18–2.23 and PFS HRpem + chemo/pem 0.55, 95% CI 0.32–0.97) [23]. This result was verified by the current study. In contrast with the previously reported indirect comparison meta-analysis, we conducted a further subgroup analysis to explore the effect of histological type, treatment lines, and ICI type. Our meta-analysis included 22 RCTs, which, to our knowledge, is the most extensive NMA to date.
This study has several limitations. To start with, our meta-analysis depended on published results instead of individual patient data. Moreover, the antibodies used to test PD-L1 expression differed between the tests. The determination method of PD-L1 antibody detection used in RCT included in this paper is TPS and TC and IC calculation, respectively. The main difference between the different methods was based on whether they involved the calculation of the number of immunocytes with a positive expression in the tumour region. TPS means (number of pD-L1 membrane staining positive tumour cells/total tumour cells)*100%, TC means (PD-L1 membrane staining positive tumour cells at any strength/total tumour cells)*100% and IC means (PD-L1 membrane staining positive tumour-associated immune cells at any strength/total tumour-associated immune cells)*100%. Owing to the spatial and temporal heterogeneity in PD-L1 expression and the differences in detection mechanisms, PD-L1 was an imperfect biomarker [24]. However, PD-L1 expression in the tumour cells is currently the most widely applied biomarker for the stratification of patients [25]. Finally, data from head-to-head comparison of RCTs were lacking. We retrieved data about each treatment from subgroup analyses of RCTs. Some of the trials did not report OS and HRs and their 95% CIs for OS in their subgroup analyses. Besides, some trials had limited samples in the subgroup analysis of the high PD-L1 expression NSCLC cohort.
In summary, based on the results of our NMA, it could be stated that previously untreated patients with non-squamous NSCLC may show improved results if they accepted PD-1 treatment. Moreover, they may have longer progression-free survival and probably have more objective responses. In the future, the treatment of NSCLC is expected to get more precise, with a greater number of studies conducted on NSCLC patients under different situations. Our results provide evidence for the treatment of NSCLC patients with a high PD-L1 expression.
Supplementary information
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and MJEditor (www.mjeditor.com) for their linguistic assistance during the preparation of this manuscript.
Author contributions
Concept and design: YMW, HDH, YS and HBL. Provision of study materials or patients: YMW and HDH. Collection and assembly of the data: YMW and HDH. Data analysis and interpretation: YMW, HDH, TFL and PZ. Formal analysis: YMW, HDH, FZ and MXY. Manuscript writing: all authors. Final approval of manuscript: all authors.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82172728 and 21890741) and the Social Development Foundation of China (No. BE2019719).
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Ethical Review Committee of the Affiliated Jinling Hospital (DBNJ20219). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Consent to publish
This study does not contain any individual person’s data in any form (including individual details, images or videos).
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yimin Wang, Hedong Han.
Contributor Information
Yong Song, Email: yong_song6310@yahoo.com.
Hongbing Liu, Email: netlhb@126.com.
Supplementary information
The online version contains supplementary material available at 10.1038/s41416-022-01832-4.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Planchard D, Popat S, Kerr K, Novello S, Smit EF, Faivre-Finn C, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:iv192–iv237. doi: 10.1093/annonc/mdy275. [DOI] [PubMed] [Google Scholar]
- 3.Shi Y, Chen W, Li C, Zhang Y, Bo M, Qi S, et al. Efficacy and safety of first-line treatments with immune checkpoint inhibitors plus chemotherapy for non-squamous non-small cell lung cancer: a meta-analysis and indirect comparison. Ann Palliat Med. 2021;10:2766–75. doi: 10.21037/apm-20-1498. [DOI] [PubMed] [Google Scholar]
- 4.Pathak R, De Lima LG, Yu H, Aryal MR, Ji W, Frumento KS, et al. Comparative efficacy of chemoimmunotherapy versus immunotherapy for advanced non-small cell lung cancer: a network meta-analysis of randomized trials. Cancer-Am Cancer Soc. 2021;127:709–19. doi: 10.1002/cncr.33269. [DOI] [PubMed] [Google Scholar]
- 5.Paz-Ares L, Vicente D, Tafreshi A, Robinson A, Soto PH, Mazières J, et al. A randomized, placebo-controlled trial of pembrolizumab plus chemotherapy in patients with metastatic squamous NSCLC: protocol-specified final analysis of KEYNOTE-407. J Thorac Oncol. 2020;15:1657–69. doi: 10.1016/j.jtho.2020.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Herbst RS, Giaccone G, de Marinis F, Reinmuth N, Vergnenegre A, Barrios CH, et al. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N. Engl J Med. 2020;383:1328–39. doi: 10.1056/NEJMoa1917346. [DOI] [PubMed] [Google Scholar]
- 7.Jotte R, Cappuzzo F, Vynnychenko I, Stroyakovskiy D, Rodríguez-Abreu D, Hussein M, et al. Atezolizumab in combination with carboplatin and nab-paclitaxel in advanced squamous NSCLC (IMpower131): results from a randomized phase III trial. J Thorac Oncol. 2020;15:1351–60. doi: 10.1016/j.jtho.2020.03.028. [DOI] [PubMed] [Google Scholar]
- 8.West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:924–37. doi: 10.1016/S1470-2045(19)30167-6. [DOI] [PubMed] [Google Scholar]
- 9.Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, Mazieres J, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–46. doi: 10.1016/S0140-6736(16)00587-0. [DOI] [PubMed] [Google Scholar]
- 10.Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65. doi: 10.1016/S0140-6736(16)32517-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barlesi F, Vansteenkiste J, Spigel D, Ishii H, Garassino M, de Marinis F, et al. Avelumab versus docetaxel in patients with platinum-treated advanced non-small-cell lung cancer (JAVELIN Lung 200): an open-label, randomised, phase 3 study. Lancet Oncol. 2018;19:1468–79. doi: 10.1016/S1470-2045(18)30673-9. [DOI] [PubMed] [Google Scholar]
- 12.Zhou C, Chen G, Huang Y, Zhou J, Lin L, Feng J, et al. Camrelizumab plus carboplatin and pemetrexed versus chemotherapy alone in chemotherapy-naive patients with advanced non-squamous non-small-cell lung cancer (CameL): a randomised, open-label, multicentre, phase 3 trial. Lancet Respir Med. 2021;9:305–14. doi: 10.1016/S2213-2600(20)30365-9. [DOI] [PubMed] [Google Scholar]
- 13.Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, Powell SF, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol. 2016;17:1497–508. doi: 10.1016/S1470-2045(16)30498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sezer A, Kilickap S, Gümüş M, Bondarenko I, Özgüroğlu M, Gogishvili M, et al. Cemiplimab monotherapy for first-line treatment of advanced non-small-cell lung cancer with PD-L1 of at least 50%: a multicentre, open-label, global, phase 3, randomised, controlled trial. Lancet. 2021;397:592–604. doi: 10.1016/S0140-6736(21)00228-2. [DOI] [PubMed] [Google Scholar]
- 15.Rizvi NA, Cho BC, Reinmuth N, Lee KH, Luft A, Ahn MJ, et al. Durvalumab with or without tremelimumab vs standard chemotherapy in first-line treatment of metastatic non-small cell lung cancer: the MYSTIC phase 3 randomized clinical trial. JAMA Oncol. 2020;6:661–74. doi: 10.1001/jamaoncol.2020.0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375:1823–33. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Lu S, Yu X, Hu Y, Sun Y, Wang Z, et al. Tislelizumab plus chemotherapy vs chemotherapy alone as first-line treatment for advanced squamous non-small-cell lung cancer: a phase 3 randomized clinical trial. JAMA Oncol. 2021;7:709–17. doi: 10.1001/jamaoncol.2021.0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Y, Wang Z, Fang J, Yu Q, Han B, Cang S, et al. Efficacy and safety of sintilimab plus pemetrexed and platinum as first-line treatment for locally advanced or metastatic nonsquamous NSCLC: a randomized, double-blind, phase 3 study (Oncology pRogram by InnovENT anti-PD-1-11) J Thorac Oncol. 2020;15:1636–46. doi: 10.1016/j.jtho.2020.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Heijkoop B, Parker N, Kiroff G, Spernat D. Effectiveness and safety of inpatient versus extended venous thromboembolism (VTE) prophylaxis with heparin following major pelvic surgery for malignancy: protocol for a systematic review. Syst Rev. 2019;8:249. doi: 10.1186/s13643-019-1179-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al. Indirect comparisons of competing interventions. Health Technol Assess. 2005;9:1–134. doi: 10.3310/hta9260. [DOI] [PubMed] [Google Scholar]
- 21.Mok T, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393:1819–30. doi: 10.1016/S0140-6736(18)32409-7. [DOI] [PubMed] [Google Scholar]
- 22.Nishio M, Saito H, Goto K, Watanabe S, Sueoka-Aragane N, Okuma Y, et al. IMpower132: atezolizumab plus platinum-based chemotherapy vs chemotherapy for advanced NSCLC in Japanese patients. Cancer Sci. 2021;112:1534–44. doi: 10.1111/cas.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou Y, Lin Z, Zhang X, Chen C, Zhao H, Hong S, et al. First-line treatment for patients with advanced non-small cell lung carcinoma and high PD-L1 expression: pembrolizumab or pembrolizumab plus chemotherapy. J Immunother Cancer. 2019;7:120. doi: 10.1186/s40425-019-0600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song F, Harvey I, Lilford R. Adjusted indirect comparison may be less biased than direct comparison for evaluating new pharmaceutical interventions. J Clin Epidemiol. 2008;61:455–63. doi: 10.1016/j.jclinepi.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Peng L, Liang WH, Mu DG, Xu S, Hong SD, Stebbing J, et al. First-line treatment options for PD-L1-negative non-small cell lung cancer: a Bayesian network meta-analysis. Front Oncol. 2021;11:657545. doi: 10.3389/fonc.2021.657545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herbst RS, Baas P, Kim DW, Felip E, Pérez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 27.Garassino MC, Gadgeel S, Esteban E, Felip E, Speranza G, Domine M, et al. Patient-reported outcomes following pembrolizumab or placebo plus pemetrexed and platinum in patients with previously untreated, metastatic, non-squamous non-small-cell lung cancer (KEYNOTE-189): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21:387–97. doi: 10.1016/S1470-2045(19)30801-0. [DOI] [PubMed] [Google Scholar]
- 28.Carbone DP, Reck M, Paz-Ares L, Creelan B, Horn L, Steins M, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 2017;376:2415–26. doi: 10.1056/NEJMoa1613493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou C, Wu L, Fan Y, Wang Z, Liu L, Chen G, et al, Sintilimab plus platinum and gemcitabine as first-line treatment for advanced or metastatic squamous NSCLC: results from a randomized, double-blind, phase 3 trial (ORIENT-12). J Thorac Oncol. 2021;16:1501–11. [DOI] [PubMed]
- 30.Lu S, Wang J, Yu Y, Yu X, Hu Y, Ai X, et al, Tislelizumab plus chemotherapy as first-line treatment for locally advanced or metastatic nonsquamous NSCLC (RATIONALE 304): a randomized phase 3 trial. J Thorac Oncol. 2021;16:1512–22. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its supplementary information files).