Graphical abstract
Keywords: COVID-19, Asthma, ICU admission, Meta-analysis
In this Journal, Fernadez-de-las-Penas et al. reported a similar prevalence of long-term post-coronavirus disease (COVID) symptoms in patients with asthma compared to non-asthmatics,1 which suggests that asthma seems not to be a risk factor for more severe long-term post-COVID symptoms but also either was a “protective” factor for that.1 We have had a valuable opportunity to carefully read this interesting paper and additional published articles regarding the relationship between pre-existing asthma and clinical outcomes of patients with coronavirus disease 2019 (COVID-19). We noticed that a number of published studies have explored the impact of pre-existing asthma on the risk for intensive care unit (ICU) admission among patients with COVID-19, however, the conclusions drawn for the previous individual studies were inconsistent. Although, several meta-analyses have been performed to address this issue, they uniformly failed to find the significant association between pre-existing asthma and the risk for ICU admission among patients with COVID-19.3, 4, 5, 6, 7, 8, 9, 2 To our knowledge, the previous meta-analyses regarding the association between pre-existing asthma and the risk for ICU admission in COVID-19 patients had limited number of included studies (Sunjaya et al.’s paper has the most included studies, with 21).2 Moreover, many studies on this topic are emerging since then. Therefore, it is necessary to clarify the impact of pre-existing asthma on the risk for ICU admission among COVID-19 patients on the basis of the latest data.
This meta-analysis strictly abided by the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). An extensive search of the literature was performed in PubMed, Springer Link, Web of Science, Wiley Library, EMBASE, Scopus, Elsevier ScienceDirect and Cochrane Library to find all compliant articles published from January 1, 2020 to October 30, 2021. The following keywords were exerted on the search strategy: “COVID-19”, “2019-nCoV”, “SARS-CoV-2”, “2019 novel coronavirus”, “coronavirus disease 2019”, “severe acute respiratory syndrome coronavirus 2”, “asthma”, “asthmatic”, “ICU”, “intensive care unit admission” and “ICU admission”. The reference lists, cited by the included studies and relevant reviews, were eligible as an exploratory objective to identify extensive articles. The inclusion criteria included: (1) adult COVID-19 patients confirmed by reverse transcriptase-polymerase chain reaction (rt-PCR); (2) peer-reviewed original articles in English; (3) individual study populations being at least fifteen cases; (4) the key available data of the included studies, four-table data or effect (95% confidence interval (CI)), must be clearly stated. Case reports, repeated articles, review papers and preprints were eliminated.
The pooled risk ratio (RR) with corresponding 95% CI was utilized to evaluate the association between asthma and ICU admission among COVID-19 patients throughout a random-effects meta-analysis model. The heterogeneity of effect among the included studies was quantitatively presented by I2 statistic. Sensitivity analysis was conducted to check whether the result was robust or not. The potential publication bias was evaluated by Begg's test. The package “meta” of R software (Version 4.1.1) was applied. Significant association was not admitted until two tailed P < 0.05.
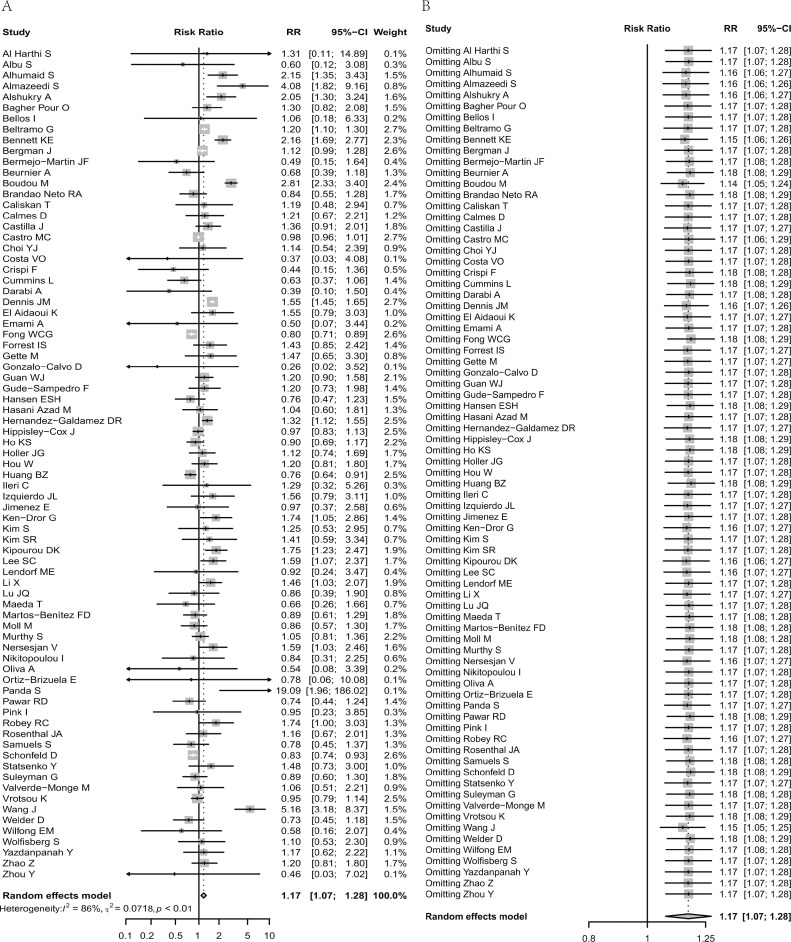
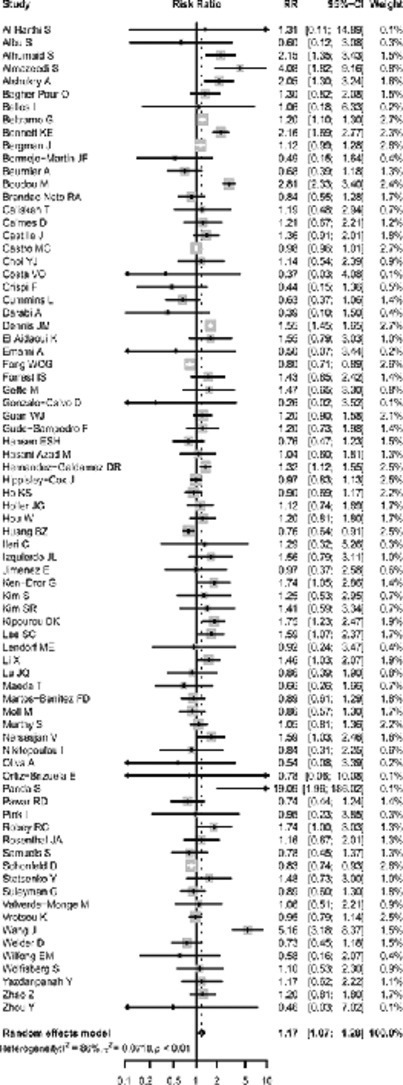
Eventually, seventy and seven eligible articles encompassing 854,405 COVID-19 patients were included in our meta-analysis. The included studies stemmed from 26 countries distributed in five continents - North America (n = 19 studies), Europe (n = 32 studies), Asia (n = 21 studies), South America (n = 4 studies) and Africa (n = 1 study). Seventy studies reported the association between asthma and ICU admission among hospitalized COVID-19 patients. The general information of included studies is summarized in Table 1 . Overall, this present meta-analysis showed that there was a significant association between pre-existing asthma and the increased risk for ICU admission among COVID-19 patients (RR: 1.17, 95% CI: 1.07–1.28; I2 = 86%, random-effects model) (Fig. 1 A). In the further subgroup analysis by continents, we observed that COVID-19 patients with asthma were at higher risk for ICU admission compared with those without asthma in Asia (RR: 1.59, 95% CI: 1.26–2.00) and Europe (RR: 1.17, 95% CI: 1.01–1.36), rather than in South America (RR: 0.91, 95% CI: 0.78–1.04), North America (RR: 0.96, 95% CI: 0.84–1.11) and Africa (RR: 1.55, 95% CI: 0.79–3.02). When the setting of patients was restricted to hospitalization, the significant association between asthma and the increased risk for ICU admission among COVID-19 patients still existed (RR: 1.19, 95% CI: 1.09–1.31). Subsequently stratified analyses based on age, sample size, study design and male percentage (%) showed that COVID-19 patients with asthma had a significantly higher risk for ICU admission compared to those without asthma among studies with < 60 years old (RR: 1.26, 95% CI: 1.06–1.51), studies with ≥ 1000 cases (RR: 1.21, 95% CI: 1.08–1.37), studies with male percentage ≥ 50% (RR: 1.22, 95% CI: 1.10–1.36) and retrospective studies (RR: 1.23, 95% CI: 1.09–1.38). The forest plot of sensitivity analysis demonstrated the robustness of our findings (Fig. 1B). There was no potential publication bias in Begg's test (P = 0.0641).
Table 1.
The general information of the eligible studies in the meta-analysis.
| Author | Location | Study design | Cases | Male (%) | Age | ICU | Non-ICU | Setting | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Asthma | Non-asthma | Asthma | Non-asthma | |||||||
| Lee SC (PMID: 33311519) | Korea | Retrospective study | 6811 | NR | NR | 27 | 163 | 615 | 6006 | Hospitalized |
| Bergman J (PMID: 33704634) | Sweden | Nationwide study | 15,872 | 59.4 | 64.1 ± 18.4 | 211 | 2283 | 997 | 12,381 | Hospitalized |
| Castilla J (PMID: 34199198) | Spain | Prospective study | 2080 | 51.92 | NR | 23 | 223 | 124 | 1710 | Hospitalized |
| Choi YJ (PMID: 32978309) | Korea | Retrospective study | 7590 | 40.8 | 44.5 | 7 | 208 | 211 | 7164 | All patients |
| Gude-Sampedro F (PMID: 33349845) | Spain | Retrospective study | 2492 | 53.13 | 70.2 ± 15.4 | 14 | 270 | 89 | 2119 | Hospitalized |
| Hansen ESH (PMID: 33527079) | Denmark | Retrospective study | 5104 | 47 | 54.8 (40.5–72.3) | 17 | 299 | 337 | 4451 | All patients |
| Martos-Benítez FD (PMID: 33411264) | Mexico | Retrospective study | 38,324 | 58.3 | 46.9 ± 15.7 | Effect (95% CI): 0.89 (0.61–1.28) | Hospitalized | |||
| Schonfeld D (PMID: 33571300) | Argentina | National database | 41,703 | 53.2 | 55 (37–72) | 269 | 5383 | 2090 | 33,961 | Hospitalized |
| Dennis JM (PMID: 33097559) | UK | Retrospective study | 19,256 | 60.1 | 67 ± 16.88 | 669 | 4778 | 929 | 12,880 | Hospitalized |
| Wang J (PMID: 33332437) | China | Retrospective study | 562 | 51.6 | 47 (35.0–57.0) | 22 | 31 | 46 | 463 | Hospitalized |
| Almazeedi S (PMID: 32766546) | Kuwait | Retrospective study | 1096 | 81 | 41 (25–75) | 6 | 36 | 37 | 1017 | Hospitalized |
| Beurnier A (PMID: 32732333) | France | Prospective study | 112 | 53.6 | 60 | 11 | 33 | 26 | 42 | Hospitalized |
| Calmes D (PMID: 33038592) | Belgium | Retrospective study | 596 | 50.7 | 58.8 | 10 | 78 | 47 | 461 | Hospitalized |
| Emami A (PMID: 32835530) | Iran | Retrospective study | 1239 | 55.9 | 51.48 ± 19.54 | 1 | 97 | 24 | 1117 | Hospitalized |
| Fong WCG (PMID: 33626216) | UK | Retrospective study | 617 | NR | NR | 78 | 495 | 24 | 20 | Hospitalized |
| Guan WJ (PMID: 33684635) | China | Retrospective study | 39,420 | 49.9 | 55.7 | 41 | 5507 | 203 | 33,669 | Hospitalized |
| Ho KS (PMID: 33647451) | USA | Retrospective study | 4902 | 55.9 | 64.99 ± 16.92 | 45 | 1005 | 188 | 3664 | Hospitalized |
| Kim S (PMID: 33012003) | Korea | Retrospective study | 2043 | 35 | 56.1 | 5 | 120 | 61 | 1857 | Hospitalized |
| Kipourou DK (PMID: 33902520) | Kuwait | Prospective study | 3995 | 70.4 | NR | 31 | 284 | 204 | 3476 | Hospitalized |
| Rosenthal JA (PMID: 33059035) | USA | Retrospective study | 274 | NR | NR | 11 | 57 | 28 | 178 | Hospitalized |
| Valverde-Monge M (PMID: 34149705) | Spain | Retrospective study | 2539 | 50.2 | 62.7 | 7 | 142 | 106 | 2284 | Hospitalized |
| Ortiz-Brizuela E (PMID: 32584326) | Mexico | Prospective study | 140 | 60.7 | 49.0 (39.0–61.3) | 0 | 29 | 2 | 109 | Hospitalized |
| Zhao Z (PMID: 32730358) | China | Retrospective study | 593 | 60.4 | 58.88 ± 17.49 | 16 | 179 | 25 | 373 | Hospitalized |
| El Aidaoui K (PMID: 33033687) | Morocco | Retrospective study | 134 | 54.5 | 53 (36–64) | 5 | 40 | 5 | 84 | Hospitalized |
| Yazdanpanah Y (PMID: 33058220) | France | Prospective study | 246 | 57 | 62 (50–73) | 7 | 64 | 14 | 161 | Hospitalized |
| Hippisley-Cox J (PMID: 32737124) | UK | Prospective study | 19,486 | 48.12 | 62.18 ± 20.84 | 178 | 1108 | 2586 | 15,614 | All patients |
| Ken-Dror G (PMID: 33199428) | UK | Prospective study | 429 | 56.4 | 70 ± 18 | 13 | 69 | 29 | 318 | Hospitalized |
| Bermejo-Martin JF (PMID: 33317616) | Canada | NR | 200 | 55.5 | 65 ± 19.5 | 2 | 98 | 6 | 94 | Hospitalized |
| Caliskan T (PMID: 33331576) | Turkey | Retrospective study | 565 | NR | 48 ± 19.664 | 4 | 87 | 17 | 457 | Hospitalized |
| Samuels S (PMID: 33409769) | USA | Retrospective study | 493 | 51.93 | 62.9 ± 18.3 | 10 | 137 | 32 | 314 | Hospitalized |
| Holler JG (PMID: 33421989) | Denmark | Cohort study | 2431 | 54.1 | 69 (53–80) | 20 | 339 | 102 | 1970 | Hospitalized |
| Crispi F (PMID: 33536488) | Spain | Prospective study | 397 | 50.4 | 47 ± 12.2 | 3 | 57 | 39 | 298 | Hospitalized |
| Bennett KE (PMID: 33880459) | Ireland | Retrospective study | 2811 | 57.5 | NR | 50 | 388 | 108 | 2265 | Hospitalized |
| Cummins L (PMID: 33942510) | UK | Retrospective study | 1195 | 62 | NR | 14 | 138 | 152 | 891 | Hospitalized |
| Castro MC (PMID: 33947740) | Brazil | Retrospective study | 465,857 | 56.2 | 61 (47–73) | 4947 | 167,526 | 8639 | 284,745 | Hospitalized |
| Beltramo G (PMID: 34016619) | France | Retrospective study | 89,530 | 53.05 | 65 ± 20 | 640 | 2633 | 14,464 | 71,793 | Hospitalized |
| Wolfisberg S (PMID: 34375985) | Switzerland | Retrospective study | 486 | 65 | 65.9 ± 14.7 | 6 | 86 | 23 | 371 | Hospitalized |
| Panda S (PMID: 34468994) | China, India | Retrospective study | 420 | 66.4 | 37 (24–50) | Effect (95% CI): 19.09 (1.55–147.19) | Hospitalized | |||
| Oliva A (PMID: 34501466) | Italy | Retrospective study | 97 | 62 | 65 (58–78) | 1 | 24 | 6 | 66 | Hospitalized |
| Boudou M (PMID: 34531478) | Ireland | Retrospective study | 3781 | 56.5 | 62.2 | 75 | 540 | 103 | 3063 | Hospitalized |
| Murthy S (PMID: 33688026) | Canada | Cohort study | 188 | 61.2 | 64 (53–75) | 38 | 290 | 52 | 431 | Hospitalized |
| Jimenez E (PMID: 33172949) | Spain | Retrospective study | 572 | 60.2 | 53 | 4 | 46 | 43 | 479 | Hospitalized |
| Gonzalo-Calvo D (PMID: 34048985) | Spain | Prospective study | 79 | 72.22 | 68.0 (56.6–77.0) | 0 | 36 | 3 | 40 | Hospitalized |
| Alshukry A (PMID: 33216801) | Kuwait | Retrospective study | 417 | 62.83 | 45.39 ± 17.064 | 15 | 67 | 26 | 309 | Hospitalized |
| Alhumaid S (PMID: 34030733) | Saudi Arabia | Cohort study | 1014 | 57 | 47.2 ± 19.3 | 11 | 194 | 15 | 794 | Hospitalized |
| Li X (PMID: 33194455) | USA | Retrospective study | 1108 | 57.3 | 61.94 ± 18.68 | 23 | 248 | 43 | 794 | Hospitalized |
| Brandao Neto RA (PMID: 33411707) | Brazil | Prospective study | 506 | 57.3 | 60.1 ± 15.1 | 11 | 289 | 11 | 195 | Hospitalized |
| Statsenko Y (PMID: 33637550) | United Arab Emirates | Retrospective study | 560 | 66.25 | 39.0 (33.0–49.0) | 7 | 65 | 31 | 457 | Hospitalized |
| Huang BZ (PMID: 34389242) | USA | Retrospective study | 3404 | NR | NR | 107 | 845 | 377 | 2075 | Hospitalized |
| Nersesjan V (PMID: 33438076) | Denmark | Prospective study | 61 | 63 | 62.7 | 3 | 32 | 0 | 26 | Hospitalized |
| Lendorf ME (PMID: 32800073) | Denmark | Retrospective study | 111 | 60 | 68.7 (56–78) | 2 | 18 | 10 | 81 | Hospitalized |
| Bellos I (PMID: 33820751) | Greece | Cohort study | 42 | 69 | 56.65 ± 14.12 | 1 | 9 | 3 | 29 | Hospitalized |
| Hasani Azad M (PMID: 34196210) | Iran | Retrospective study | 2351 | 52.5 | 47.02 ± 20.4 | 12 | 216 | 107 | 2016 | Hospitalized |
| Suleyman G (PMID: 32543702) | USA | Case series | 355 | 46.5 | 61.4 | 19 | 122 | 34 | 180 | Hospitalized |
| Pink I (PMID: 34021897) | Germany | Retrospective study | 99 | 73.7 | 57 | 1 | 51 | 1 | 46 | Hospitalized |
| Ileri C (PMID: 33501850) | Turkey | NR | 140 | 58.6 | 55 ± 16 | 2 | 12 | 14 | 112 | Hospitalized |
| Zhou Y (PMID: 33109234) | China | Retrospective study | 1087 | 48.3 | 61.94 ± 18.68 | 0 | 97 | 11 | 979 | Hospitalized |
| Welder D (PMID: 34132393) | USA | Cohort study | 658 | 52.7 | 61.4 | 15 | 124 | 79 | 440 | Hospitalized |
| Hernandez-Galdamez DR.(PMID: 32747155) | Mexico | Cross-sectional study | 23,084 | NR | NR | 143 | 1563 | 1358 | 20,020 | Hospitalized |
| Darabi A (PMID: 34476916) | Iran | Case series | 400 | 51.2 | 49.2 | 2 | 66 | 27 | 305 | All patients |
| Hou W (PMID: 33746590) | USA | Retrospective study | 593 | 60.4 | 58.3 | 16 | 179 | 25 | 373 | Hospitalized |
| Lu JQ (PMID: 33976972) | USA | Retrospective study | 1307 | 58.2 | 60.86 ± 17.72 | 6 | 98 | 81 | 1122 | Hospitalized |
| Forrest IS (PMID: 34089483) | USA | Retrospective study | 688 | 63.5 | 67.2 | 10 | 153 | 20 | 505 | Hospitalized |
| Gette M (PMID: 34070021) | France | Retrospective study | 292 | 63.7 | 68 (57–81) | 5 | 44 | 16 | 227 | Hospitalized |
| Izquierdo JL (PMID: 33090964) | Spain | Retrospective study | 10,504 | 52.5 | 58.2 ± 19.7 | 9 | 74 | 750 | 9671 | All patients |
| Robey RC (PMID: 34278556) | UK | Retrospective study | 221 | 61 | 58 | 13 | 31 | 30 | 147 | Hospitalized |
| Kim SR (PMID: 33260724) | Korea | Retrospective study | 2959 | 39.8 | 53.15 (38.64–65.87) | 5 | 128 | 75 | 2751 | Hospitalized |
| Bagher Pour O (PMID: 34454118) | Iran | Prospective study | 226 | 50.4 | 56.36 ± 18.54 | 7 | 105 | 4 | 110 | Hospitalized |
| Wilfong EM (PMID: 34179689) | USA | Retrospective study | 128 | 58.6 | 56.0 (45.4–67.8) | 2 | 37 | 9 | 80 | Hospitalized |
| Costa VO (PMID: 34411145) | Brazil | Retrospective study | 58 | 22.1 | 34 ± 22.1 | 0 | 39 | 1 | 18 | Hospitalized |
| Maeda T (PMID: 32720702) | USA | Retrospective study | 224 | 56.7 | 63 ± 17 | 4 | 53 | 19 | 148 | Hospitalized |
| Vrotsou K (PMID: 33795313) | Spain | Retrospective study | 14,197 | 38.9 | 53.7 ± 17.4 | 88 | 3622 | 266 | 10,221 | All patients |
| Moll M (PMID: 32710891) | USA | Retrospective study | 210 | 48.1 | 62.21 ± 16.23 | 15 | 87 | 20 | 88 | Hospitalized |
| Pawar RD (PMID: 34133005) | USA | Cohort study | 396 | 54.3 | 64.8 ± 17.0 | 12 | 110 | 39 | 235 | Hospitalized |
| Albu S (PMID: 33998551) | Spain | Cross-sectional study | 30 | 63.3 | 54 (43.8–262) | 1 | 15 | 2 | 12 | Outpatient |
| Al Harthi S (PMID: 34567884) | Oman | Cross-sectional study | 102 | 77.5 | 49.9 ± 14.7 | 0 | 19 | 1 | 82 | Hospitalized |
| Nikitopoulou I (PMID: 34576169) | Greece | Cohort study | 116 | 74.1 | 60.5 | 2 | 67 | 2 | 45 | Hospitalized |
Note: The age (years) was presented as mean ± standard deviation or median (interquartile range, IQR); CI, confidence interval; ICU, intensive care unit; NR, not clearly reported; UK, The United Kingdom; USA, the United States of America.
Fig. 1.
(A) Forest plot indicated that coronavirus disease 2019 (COVID-19) patients with asthma had a significantly increased risk for admission to intensive care unit (ICU) compared to those without asthma: pooled risk ratio (RR) with its 95% confidence intervals (CI); (B) Sensitivity analysis for pooled RR and 95% CI by deleting one single study from overall pooled analysis each time showed that our results were robust.
In conclusion, our study demonstrated that pre-existing asthma was significantly associated with an increased risk for ICU admission among COVID-19 patients. Thus, COVID-19 patients with asthma should receive greater medical attention to prevent illness progression. Further well-designed studies based on risk factors-adjusted estimates are warranted to confirm our findings.
Data availability statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.
Funding
This study was supported by grants from the Key Scientific Research Project of Henan Institution of Higher Education (No. 21A330008), National Natural Science Foundation of China (No. 81973105), and Joint Construction Project of Henan Medical Science and Technology Research Plan (No. LHGJ20190679). The funders have no role in the data collection, data analysis, preparation of manuscript and decision to submission.
CRediT authorship contribution statement
Xueya Han: Data curation, Formal analysis, Writing – original draft. Jie Xu: Data curation, Formal analysis. Hongjie Hou: Data curation, Formal analysis. Haiyan Yang: Conceptualization, Data curation. Yadong Wang: Conceptualization, Data curation.
Declaration of Competing Interest
All authors report that they have no potential conflicts of interest.
Acknowledgments
We would like to thank Yang Li, Peihua Zhang, Jian Wu, Xuan Liang, Wenwei Xiao, Ying Wang and Li Shi (All are from Department of Epidemiology, School of Public Health, Zhengzhou University) for their kind help in searching articles and collecting data, and valuable suggestions for analyzing data.
References
- 1.Fernandez-de-Las-Penas C., Torres-Macho J., Velasco-Arribas M., Arias-Navalon J.A., Guijarro C., Hernandez-Barrera V., et al. Similar prevalence of long-term post-COVID symptoms in patients with asthma: a case-control study. J Infect. 2021;83(2):237–279. doi: 10.1016/j.jinf.2021.04.034. AugPubMed PMID: 33957161. Pubmed Central PMCID: 8089027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sunjaya A.P., Allida S.M., Di Tanna G.L., Jenkins C.R. Asthma and coronavirus disease 2019 risk: a systematic review and meta-analysis. Eur Respir J. 2021 doi: 10.1183/13993003.01209-2021. Aug 24PubMed PMID: 34385278. Pubmed Central PMCID: PMC8361304 Allida has nothing to disclose. Conflict of interest: Dr. Di Tanna has nothing to disclose. Conflict of interest: Dr. JENKINS has nothing to disclose. Epub 2021/08/14. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu S., Cao Y., Du T., Zhi Y. Prevalence of comorbid asthma and related outcomes in COVID-19: a Systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2021;9(2):693–701. doi: 10.1016/j.jaip.2020.11.054. FebPubMed PMID: 33309934. Pubmed Central PMCID: PMC7725230. Epub 2020/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sitek A.N., Ade J.M., Chiarella S.E., Divekar R.D., Pitlick M.M., Iyer V.N., et al. Outcomes among patients with COVID-19 and asthma: a systematic review and meta-analysis. Allergy Asthma Proc. 2021;42(4):267–273. doi: 10.2500/aap.2021.42.210041. Jul 1PubMed PMID: 34187619. Epub 2021/07/01. [DOI] [PubMed] [Google Scholar]
- 5.Pardhan S., Wood S., Vaughan M., Trott M. The risk of COVID-19 Related hospitalsation, intensive care unit admission and mortality in people with underlying asthma or COPD: a systematic review and meta-analysis. Front Med (Lausanne) 2021;8 doi: 10.3389/fmed.2021.668808. PubMed PMID: 34222281. Pubmed Central PMCID: PMC8242585. Epub 2021/07/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hussein M.H., Elshazli R.M., Attia A.S., Nguyen T.P., Aboueisha M., Munshi R., et al. Asthma and COVID-19; different entities, same outcome: a meta-analysis of 107,983 patients. J Asthma. 2021:1–8. doi: 10.1080/02770903.2021.1881970. Feb 22PubMed PMID: 33504226. Epub 2021/01/29. [DOI] [PubMed] [Google Scholar]
- 7.Wu X., Xu Y., Jin L., Wang X., Zhu H., Xie Y. Association of preexisting asthma and other allergic diseases with mortality in COVID-19 patients: a systematic review and meta-analysis. Front Med (Lausanne) 2021;8 doi: 10.3389/fmed.2021.670744. PubMed PMID: 34249969. Pubmed Central PMCID: PMC8264065. Epub 2021/07/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geng J., Yu X., Bao H., Feng Z., Yuan X., Zhang J., et al. Chronic diseases as a predictor for severity and mortality of COVID-19: a systematic review with cumulative meta-analysis. Front Med (Lausanne) 2021;8 doi: 10.3389/fmed.2021.588013. PubMed PMID: 34540855. Pubmed Central PMCID: PMC8440884. Epub 2021/09/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sunjaya A.P., Allida S.M., Di Tanna G.L., Jenkins C. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: systematic review and meta-analysis. J Asthma. 2021:1–14. doi: 10.1080/02770903.2021.1888116. Apr 1PubMed PMID: 33556287. Pubmed Central PMCID: PMC8022341. Epub 2021/02/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.