Abstract
Background
A significant number of coronary artery disease patients do not attain guideline recommended LDL levels. Participating in a cardiac rehabilitation (CR) program has been shown to improve adherence to medical therapy.
Objectives
Evaluate the specific lipid lowering therapy (LLT) prescribed and percent of subjects achieving LDL levels of <70 mg/dL before and after 3 months following CR program initiation.
Methods
From May 2017 to April 2019, we prospectively recruited patients referred to our CR program and compared 1015 of them at 4 time points; (P1) just prior to the index hospitalization, (P2) during the index hospitalization, (P3) upon entering the CR program, roughly 3 months after the index hospitalization, and (P4) 3 months into the CR program. Included in the analysis were parameters of lipid levels, the dispensed medication given, as well as patient adherence to treatment. Results: At CR intake, LDL goals were partially achieved with 57% of patients below 70 mg/dL. After completion of 3 months of CR, 63% of patients had LDL levels below 70 mg/dL, despite the fact that the majority (95%) were prescribed high-dose potent statins. Aside from the LDL levels at CR intake, we found no other independent predictors for not attaining the lipid goals at 6 months.
Conclusions
A significant treatment gap is present even in a selected population participating in CR, with the vast majority receiving guideline recommended LLT. In order to improve goals, we need to intensify LLT treatment, and increase patient adherence to therapy.
Keywords: Lipids, Cardiac rehabilitation, Statins, PCSK-9 inhibitors
1. Introduction
Cardiovascular diseases are the leading cause of mortality worldwide. Clinical studies have demonstrated that LDL reduction reduces clinical events [1]. Despite the multitude of evidence and guideline recommendations linking optimal lipid management and outcomes, a significant number of patients do not attain recommended target levels [2]. Recent clinical studies have also demonstrated that aggressive LDL reduction further reduces clinical events [3,4]. We sought to provide comprehensive information regarding whether subjects with ischemic heart disease within out-patient clinics or cardiac rehabilitation (CR) programs reached target LDL levels.
2. Methods
The study design consisted of a registry of study data, which were collected partially retroactively based on medical records, information about pre-hospital treatment, admission to rehabilitation, and laboratory tests upon admission to rehabilitation. From May 2017 to April 2019, we recruited 1015 patients who entered the CR program at our institution. All patients suffered a myocardial infarction or underwent coronary revascularization 3 months earlier (index hospitalization). Data regarding lipid profiles and treatment was available at 4 time points (Fig. 1). We obtained data for all 1015 patients: (P1) just prior to the index hospitalization, (P2) during the index hospitalization, and (P3) upon entering the CR program, which was roughly 3 months after the index hospitalization. Only 540 patients continued to participate in the CR program and had repeated lipid profiles performed at (P4) 3 months into the CR program.
Fig. 1.
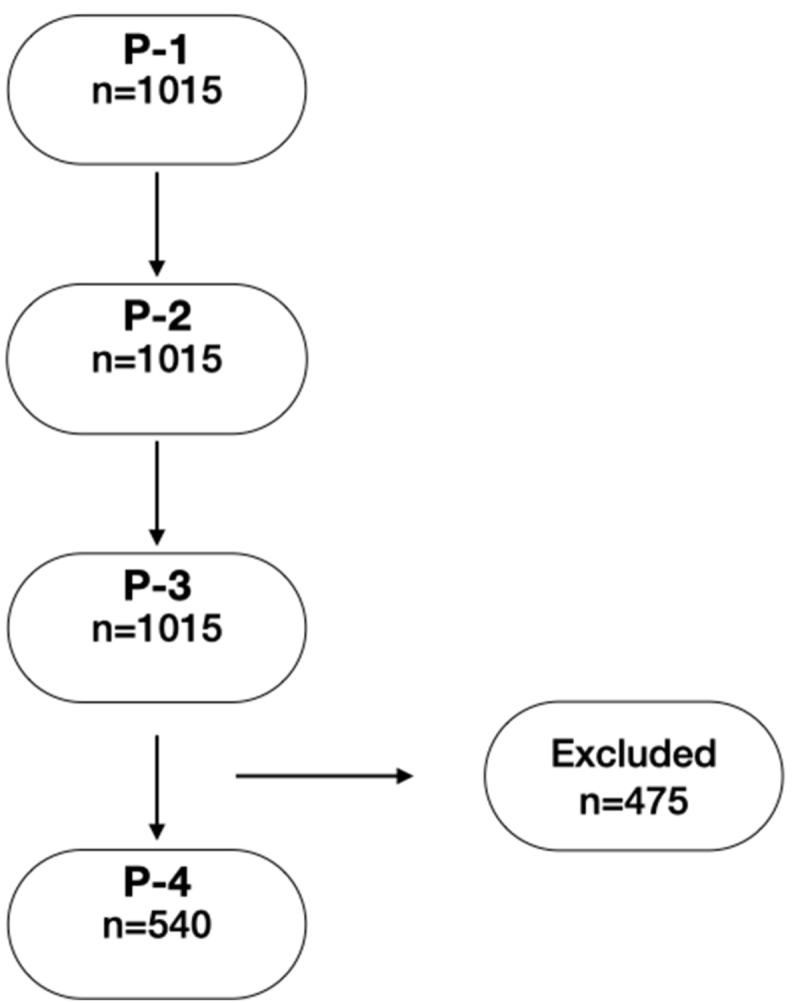
Flow chart showing the number of patients at 4 time points. P-1: prior to index hospitalization; P-2: during index hospitalization; P-3: on entering the CRP; P-4: 3 months into the CRP. The 475 patient quitted the CR program therefore were excluded.
The CR program at our institution contains a comprehensive lifestyle and risk factor management, in addition to medical therapy which includes LLT.
The target LDL level for our study population was defined as =< 70 mg/Dl based on the 2016 ESC guidelines on dyslipidemia [5].
We collected data regarding lipid levels, medication recommendations, and the dispensed medication (including generic medication name and dose). This data was obtained from the interoperability medical record system that incorporates data from all the healthcare organizations in Israel. No core lab was available for this study, thus all blood tests were performed according to the health care organization policy using individual facilities. Patients were also asked about their adherence to the treatment recommended by the doctor (i.e. taking the prescribed dose) as well as reasons for any changes in dosages.
Descriptive statistics are summarized according to 3 groups of LDL values (below 70, 70 to 100, and above 100 mg/dL) at CR intake. Similarly we compared population by the LDL levels attained 3 months later using the same group definitions. Additionally, we analyzed the cohort according to statin use prior to the index hospitalization.
The 3 LDL level groups were examined through the use of chi-square test and one-way ANOVA, according to variable type and respective distribution. Characteristics of patients according to statin use before the index hospitalization were compared using chi-square test for categorical data, and 2-sided Student t-test or Wilcoxon rank-sum tests for continuous data, as appropriate.
Logistic regression multivariate analysis was used to explore the independent association of predefined covariants and the outcome of LDL >70 mg/dL at 3 months after CR initiation.
All P values reported were unadjusted unless otherwise specified. Differences achieving p < 0.05 were considered statistically significant. Analysis was performed using R version 3.21 (R foundation).
3. Results
Baseline characteristics of patients according to their LDL levels available at the CR intake are summarized in Table 1. Patients are divided according to LDL level at the time of CR program intake. As shown, at that time, LDL levels of 57% of patients were below 70 mg/dL (e.g. at target level per ESC dyslipidemia guidelines prior to 2019 update). Furthermore, only 33% of patients attained LDL levels below 55 mg/dL, despite a valid prescription for high-dose potent statins in 95.5% of patients (defined as Atorvastatin 40 mg; Rosuvastatin 20 mg, or higher daily doses). At CR intake, 88% of patients prescribed Atorvastatin had a documented purchase of 40 mg or more, whereas 72% had purchased Rosuvastatin of 20 mg or more. The average daily dose of Atorvastatin and Rosuvastatin, was 61 mg and 25 mg, respectively. Interestingly, compared to the hospital issued prescription, at CR intake, 14% had a statin dose reduction despite an LDL >70 mg/dL. The reason for the statin dose reduction was made by the family physician (41%) or the patient's own decision (26%), as stated by the patient. Only 3% had a dose increase after hospital discharge and the CR intake.
Table 1.
Baseline characteristics of study population by LDL levels (mg/dL) at CR intake (approximately 3 months post hospitalization).
| LDL <70 | LDL 70-100 | LDL ≥100 | p-value | |
|---|---|---|---|---|
| n (%) | 582 (57) | 312 (31) | 121 (12) | |
| Gender (male) (%) | 483 (83.0) | 252 (80.8) | 96 (79.3) | 0.530 |
| Age (mean (sd)) | 63.78 (10.71) | 64.81 (10.03) | 61.20 (11.75) | 0.007 |
| Heart Failure history (%) | 34 (9.0) | 19 (8.9) | 10 (11.4) | 0.766 |
| MI past (>6 months) (%) | 38 (6.5) | 27 (2.33) | 8 (6.61) | 0.164 |
| MI recent (%) | 354 (60.8) | 154 (49.3) | 50 (41.3) | 0.164 |
| CABG past (>6 months) (%) | 29 (4.98) | 11 (3.52) | 6 (4.95) | 0.265 |
| CABG recent (%) | 75 (12.8) | 54 (17.3) | 19 (15.7) | 0.265 |
| PCI prior (>6 months) (%) | 29 (4.98) | 25 (8.01) | 10 (8.26) | 0.054 |
| PCI recent (past 6 months) (%) | 447 (76.8) | 225 (72.1) | 71 (58.6) | 0.054 |
| PVD (%) | 30 (8.0) | 17 (8.1) | 5 (5.7) | 0.759 |
| CVA/TIA (%) | 26 (6.9) | 29 (13.9) | 5 (5.7) | 0.009 |
| Diabetes (%) | 178 (41.2) | 106 (44.4) | 31 (31.3) | 0.084 |
| Hypertension (%) | 290 (60.8) | 142 (56.1) | 45 (43.7) | 0.006 |
| Family history of coronary disease (%) | 205 (41.3) | 91 (34.3) | 37 (44.0) | 0.112 |
| Smoking status: (%) | 0.283 | |||
| Current smoker | 41 (7.3) | 22 (7.3) | 15 (12.8) | |
| Never | 294 (52.7) | 154 (50.8) | 61 (52.1) | |
| Past smoker (>6 Months) | 223 (40.0) | 127 (41.9) | 41 (35.0) | |
| LVEF <50 (%) | 146 (29.2) | 71 (26.6) | 24 (24.5) | 0.545 |
| TG: Before hospitalization (mean (sd)) | 149.50 (72.19) | 144.47 (73.11) | 198.85 (179.63) | <0.001 |
| HDL:Before hospitalization (mean (sd)) | 42.70 (12.21) | 45.66 (18.28) | 45.66 (11.53) | 0.065 |
| LDL:Before hospitalization (mean (sd)) | 107.28 (52.50) | 112.37 (40.37) | 134.15 (47.29) | 0.002 |
| LDL: during hospitalization (mean (sd)) | 102.64 (36.93) | 107.42 (36.50) | 132.99 (45.25) | <0.001 |
| LDL: At initiation of rehabilitation (mean (sd)) | 51.98 (12.16) | 81.49 (7.75) | 129.36 (31.16) | <0.001 |
| Medication: Before hospitalization (%) | ||||
| rosuvastatin | 31 (14.4) | 17 (11.6) | 5 (11.6) | |
| pravastatin | 6 (2.8) | 4 (2.7) | 1 (2.3) | |
| atorvastatin | 103 (47.7) | 76 (51.7) | 28 (65.1) | |
| simvastatin | 74 (34.3) | 49 (33.3) | 8 (18.6) | |
| ezetimibe before hospitalization (%) | 9 (2.7) | 4 (2.1) | 2 (2.4) | 0.897 |
*proportions (%) are calculated out of subjects with complete data available.
Table 2 shows data collected 3 months after the initiation of CR program (e.g. 6 month after the index hospitalization). At that time, LDL levels of 63% of patients were below 70 mg/dL whereas the proportion of patients below 55 mg/dL did not significantly change compared to CR intake value (32%). Of the patients with LDL >70 mg/dL at the CR intake, approximately 45% attained the LDL goals of below 70 mg/dL after 3 months following CR intake, whereas 55% of this group were still above target goal 3 months into the CR program. Medication in the group not attaining the LDL goal, despite participating in CR for 3 months, was comprised largely of high-dose potent statins: 73% Atorvastatin (average dose 53 mg), 16.7% Rosuvastatin (average dose 26 mg) and 3% Simvastatin (average dose 32 mg). Ezetimibe was also recommended in 8.6% of these cases. Complete follow-up data, including repeated lab results, was only available for 53% of the original cohort, mainly due to dropout, program completion, or lack of additional lab results from the community. Interestingly, 3 months after index hospitalization, 22% of patients who had LDL levels within goal (<70 mg/dL) ended up having LDL levels above target goal 6 months after index hospitalization.
Table 2.
Follow-up data by LDL levels 3 months following CR intake (approximately 6 months post index hospitalization).
| LDL <70 | LDL 70-100 | LDL ≥100 | p-value | |
|---|---|---|---|---|
| n (%) | 340 (63) | 174 (32) | 26 (5) | |
| Clinical events since prior visit (%) | 20 (7.1) | 20 (14.9) | 5 (25.0) | 0.004 |
| ACS (%) | 3 (1.1) | 2 (1.5) | 1 (5.0) | 0.337 |
| CVA/TIA (%) | 0 (0.0) | 2 (1.5) | 0 (0.0) | 0.104 |
| PCI (%) | 9 (2.6) | 8 (4.6) | 1 (3.8) | 0.501 |
| Chest Pain (%) | 18 (6.2) | 13 (9.5) | 2 (10.0) | 0.444 |
| Heart Failure event (%) | 2 (0.7) | 1 (0.7) | 0 (0.0) | 0.929 |
| Other hospitalizations (%) | 20 (7.7) | 16 (12.2) | 3 (17.6) | 0.182 |
| LDL: Follow up 3 months (mean (sd)) | 53.61 (10.71) | 80.73 (8.45) | 132.46 (39.78) | <0.001 |
| HDL: Follow up 3 months (mean (sd)) | 40.14 (10.41) | 42.42 (11.09) | 45.29 (10.92) | 0.010 |
| TG: Follow up 3 months (mean (sd)) | 111.92 (72.99) | 123.99 (62.14) | 122.32 (52.34) | 0.203 |
| Medication by group (%) | 0.385 | |||
| atorvastatin + ezetimibe | 3 (0.9) | 0 (0.0) | 0 (0.0) | |
| rosuvastatin | 56 (17.7) | 28 (17.2) | 6 (27.3) | |
| pravastatin | 1 (0.3) | 0 (0.0) | 0 (0.0) | |
| atorvastatin | 251 (79.2) | 132 (81.0) | 14 (63.6) | |
| simvastatin | 5 (1.6) | 3 (1.8) | 2 (9.1) | |
| Dose (mg) of rosuvastatin (%) | 0.160 | |||
| 5 | 1 (1.8) | 4 (14.3) | 1 (16.7) | |
| 10 | 12 (21.4) | 4 (14.3) | 0 (0.0) | |
| 20 | 23 (41.1) | 7 (25.0) | 3 (50.0) | |
| 40 | 20 (35.7) | 13 (46.4) | 2 (33.3) | |
| Dose (mg) of atorvastatin (%) | 0.711 | |||
| 5 | 3 (1.2) | 1 (0.8) | 0 (0.0) | |
| 10 | 6 (2.4) | 5 (3.8) | 2 (14.3) | |
| 20 | 23 (9.2) | 21 (15.9) | 0 (0.0) | |
| 30 | 1 (0.4) | 1 (0.8) | 0 (0.0) | |
| 40 | 87 (34.9) | 47 (35.6) | 6 (42.9) | |
| 80 | 129 (51.8) | 57 (43.2) | 6 (42.9) | |
| Dose (mg) of simvastatin (%) | 0.672 | |||
| 10 | 1 (20.0) | 0 (0.0) | 0 (0.0) | |
| 20 | 3 (60.0) | 1 (33.3) | 1 (50.0) | |
| 40 | 1 (20.0) | 2 (66.7) | 1 (50.0) | |
| Dose or medication change during follow-up (%) | 58 (19.6) | 24 (14.8) | 5 (22.7) | 0.379 |
| Reason for dose or medication change - follow-up (%) | 0.001 | |||
| Doctor decision | 36 (57.1) | 14 (56.0) | 1 (16.7) | |
| LDL not at goal | 3 (4.8) | 0 (0.0) | 0 (0.0) | |
| Myalgia | 21 (33.3) | 5 (20.0) | 1 (16.7) | |
| Patient decision | 1 (1.6) | 3 (12.0) | 3 (50.0) | |
| Unknown reason | 2 (3.2) | 3 (12.0) | 1 (16.7) |
*Presented data are based on patients with follow-up data only.
At the 6 month follow-up visit, a total of 27 patients reported significant myalgia that led to medication changes. Approximately 80 patients had minor symptoms, mostly transitory or nonspecific, that were mainly considered to be due to statin therapy and did not lead to any changes in therapy. We received no reports regarding severe or serious adverse events related to lipid lowering therapy.
A logistic regression model, was constructed for the outcome of LDL >70 at the 6-month follow-up. The variables involved were: Age, gender, rehabilitation indication, LDL level at the rehabilitation intake visit. With the exception of LDL levels at CR intake: OR 1.04 (0.78–0.97), we found no other significant independent predictor for the failure to attaining the lipid goals at 6 months.
The use of PCSK-9 inhibitors was very low, with only 7 patients taking this medication at the 6 month follow-up visit. All had an LDL level <55 mg/dL at 1–2 months after treatment initiation.
Characteristics according to statin use prior to the index hospitalization are presented in supplementary 1 S. Patients treated with statins prior to the index hospitalization predating the CR intake, were significantly older, with significantly greater comorbidity (diabetes, hypertension, history of myocardial infarction, and cerebrovascular accident) compared to non-statin-treated patients. Among the statin-treated patients, 52% were on Atorvastatin, 33% on Simvastatin, 13% on Rosuvastatin and 3% on Pravastatin. Approximately 6% of patients were taking Ezetimibe as well.
As expected, the average LDL levels were significantly lower in the statin-treated group versus the non-statin-treated group: 99.8 ± 53.8 vs 124 ± 39.7. A spontaneous mild decrease in LDL levels was noted 24 h after index admission in both groups: 92.7 ± 31.2 vs 117 ± 40.1.
4. Discussion
At CR intake, 57% of patients with coronary artery disease had LDL levels below 70 mg/dL and only 33% of patients attained LDL levels below 55 mg/dL. After 3 months into the CR program, a significant proportion (37%) of patients with coronary artery disease still had LDL levels above 70 mg/dL and only 32% had LDL levels below 55 mg/dL. This is despite the fact that patients were all under the combined supervision of a cardiac rehabilitation team, a community family physician, as well as a cardiologist.
Other international data consistently show similar trends. For example, this trend can be seen in the prospective SOLID-TMI52 study in which 36 countries participated and lipid lowering drug use was strongly encouraged. Only 50% of the 12,446 participants had LDL <70 mg/dL at 3 month follow-up despite 95% use of statins at baseline [6]. Similarly, in a large German retrospective cohort study (based on the QuintilesIMS® Disease Analyzer with >2 million individuals annually), >14,000 patients assessed each year (mean age 71 years, 35% female, all high risk for future cardiovascular events), found that approximately 80% had LDL-C ≥ 70 mg/dL despite being on moderate-/high-intensity statins [7].
It is worth noting that our cohort is composed of patients with higher than average motivation and healthcare literacy, as has been shown in most studies with patient participation in CR programs and general patients after coronary revascularization or MI [8]. Furthermore, financial factors are less likely to play a significant role in this study, as statins are widely reimbursed in Israel and all Israeli citizens are covered by the national insurance program [9].
Two principal obstacles explain the suboptimal lipid management results presented in our study. One obstacle could have been the suboptimal adherence to the prescribed medication. In our study, almost all included participants had a prescription for high-dose potent statins. Non-adherence is a multifactorial problem which requires a multistep solution [10]. Current data suggests that improved adherence to lipid lowering treatment (LLT) may be achieved by implementing team-based intensified patient care interventions, such as electronic reminders, pharmacist-led interventions, and healthcare professional education of patients [10,11]. Another obstacle which could explain suboptimal lipid management is that prescribing physicians in our study underutilized the maximal tolerated doses for patients. Additionally, we observed that there were frequent dose reductions made by prescribing physicians which were not driven by any stated clinical reasons.
In order to minimize this treatment gap, it is important to intensify LLT. A recently published meta-analysis including 152,507 patients in secondary prevention from 19 trials (15 with statins, 3 with PCSK-9 inhibitors and 1 with Ezetimibe) compared more-intensive (N = 76,678) to less-intensive (N = 75,829) LDL-C lowering strategies. Risk reduction was more pronounced in the more-intensive strategy, with a risk ratio (RR) of 0.81, 95% CI 0.77–0.86 [12].
Based on the results of our study and other global studies, it is clear that current treatments for lowering lipid levels are not optimal for a variety of reasons. Patients in our study were in a rigorous CR program, in one of the largest hospitals in Israel, with the most extensive and accurate recommendations on treatment upon discharge after hospitalization. They all had covered health insurance provided by the Israeli Health Ministry and had clear accessibility to various LLT drugs. Additionally, they had been advised and treated by both attending physicians and a cardiologist. Despite all of these factors, most patients did not achieve the goals of lipid treatment, which were to reduce LDL levels <70 mg/dL (and even fewer patients achieved the latest recommended goals of reducing LDL levels <55 mg/dL). The use of Ezetimibe, although widely available in Israel and fully reimbursed, was very low at all time points. For this reason, we believe that more intensive LLT therapies, such as PCSK-9 inhibitors, are necessary in reducing LDL levels to acceptable values in these vulnerable patients.
PCSK-9 inhibitors have real-world evidence of their efficacy and safety. PCSK-9 inhibitors have been shown to reduce the risk of major adverse cardiovascular events compared to alternate LLTs [13]. More specifically, PCSK-9 inhibitors, when added to a background of statin therapy, lower LDL-C to previously unattainable levels. Overall, PCSK-9 inhibitors are well tolerated with the most common reported side effects being nasopharyngeal problems, nausea, injection-site reactions, and myalgia. Emerging data have shown that there are no negative effects on neurocognition or glycemic control [14]. In addition, PCSK-9 inhibitors are bi-monthly injections [15]. For this reason, they can help overcome existing barriers to adherence when compared to conventional treatment.
Study limitations: Our study has a number of limitations. First, although most of the data was collected prospectively, some information was retrospective (i.e. hospitalization data and pre-hospitalization management), partly based on medical records, which did not always include complete information. Second, follow-up laboratory data was not available for all the patients, mostly due to patients quitting the program, as a result of 1015 patients referred to our CR program only 540 participated in the analysis. thus limiting generalizability of the results. Lastly, adherence to treatment is ultimately up to the patient, which can be variable. Some patients may have not always followed the treatment exactly as they were required to and did not always tell the truth to their physician.
Despite mostly appropriate discharge recommendations, LDL levels attained 3 months and 6 months following an acute coronary event or coronary revascularization are suboptimal. Additional systematic efforts are necessary in order to attain desired LDL levels post acute coronary syndrome. Although most patients are already receiving lipid modifying medication, dosing and medication choices should be optimized. This treatment gap will be even larger following the 2019 ESC new lipid guideline, recommending an LDL goal of <55 mg/dL for very high-risk individuals. While potent statins are widely available and use of PCSK-9 inhibitors greatly increases the odds of attaining this goal, it is important to further identify barriers to the appropriate long-term use of lipid lowering drugs.
Credit author statement
David Rott: Conceptualization, Methodology, Writing- Reviewing and Editing. Ilan Hay: Data curation, Writing – original draft. Irene Nabutovsky: Application of statistical techniques to analyze study data. Alexis Heller: Writing – original draft.. Daniel Breitner: Validation Investigation. Robert Klempfner: Writing- Reviewing and Editing.
Footnotes
This study was funded by Sanofi Israel.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcrp.2022.200145.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cholesterol Treatment Trialists’ (CTT) Collaboration. Baigent C., Blackwell L., Emberson J., Holland L.E., Reith C., Bhala N., Peto R., Barnes E.H., Keech A., Simes J., Collins R. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Backer G., Jankowski P., Kotseva K., Mirrakhimov E., Reiner Ž., Rydén L., Tokgözoğlu L., Wood D., De Bacquer D., EUROASPIRE V collaborators; Writing Committee; Scientific Steering/Executive Committee; Coordinating centre; Diabetes centre; Data management centre; Statistical analysis centre; Central laboratory; Study centres, organisations, investigators and other research personnel (National Co-ordinators in each country are indicated by asterisk Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis. 2019;285:135–146. doi: 10.1016/j.atherosclerosis.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 3.Sabatine M.S., Giugliano R.P., Keech A.C., Honarpour N., Wiviott S.D., Murphy S.A., Kuder J.F., Wang H., Liu T., Wasserman S.M., Sever P.S., Pedersen T.R. FOURIER steering committee and investigators. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 2017;376:1713–1722. doi: 10.1056/NEJMoa1615664. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz G.G., Steg P.G., Szarek M., Bhatt D.L., Bittner V.A., Diaz R., Edelberg J.M., Goodman S.G., Hanotin C., Harrington R.A., Jukema J.W., Lecorps G., Mahaffey K.W., Moryusef A., Pordy R., Quintero K., Roe M.T., Sasiela W.J., Tamby J.F., Tricoci P., White H.D. Zeiher AM, ODYSSEY OUTCOMES committees and investigators. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 2018;379:2097–2107. doi: 10.1056/NEJMoa1801174. [DOI] [PubMed] [Google Scholar]
- 5.Catapano A.L., Graham I., De Backer G., Wiklund O., Chapman M.J., Drexel H., Hoes A.W., Jennings C.S., Landmesser U., Pedersen T.R., Reiner Z., Riccardi G., Taskinen M.R., Tokgozoglu L., Verschuren W.M.M., Vlachopoulos C., Wood D.A., Zamorano J.L., Cooney M.T. ESC scientific document group. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur. Heart J. 2016;37:2999–3058. doi: 10.1093/eurheartj/ehw272. [DOI] [PubMed] [Google Scholar]
- 6.Eisen A., Cannon C.P., Braunwald E., Steen D.L., Zhou J., Goodrich E.L., Im K., Dalby A.J., Spinar J., Daga S., Lukas M.A., O'Donoghue M.L. Predictors of nonuse of a high-potency statin after an acute coronary syndrome: insights from the stabilization of plaques using darapladib-thrombolysis in myocardial infarction 52 (SOLID-TIMI 52) trial. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.004332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox K.M., Tai M.H., Kostev K., Hatz M., Qian Y., Laufs U. Treatment patterns and low-density lipoprotein cholesterol (LDL-C) goal attainment among patients receiving high- or moderate-intensity statins. Clin. Res. Cardiol. 2018;107:380–388. doi: 10.1007/s00392-017-1193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghisi G.L.D.M., Abdallah F., Grace S.L., Thomas S., Oh P. A systematic review of patient education in cardiac patients: do they increase knowledge and promote health behavior change? Patient Educ. Counsel. 2014;95:160–174. doi: 10.1016/j.pec.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . 2018. Medicines Reimbursement Policies in Europe.https://www.euro.who.int/__data/assets/pdf_file/0011/376625/pharmaceutical-reimbursement-eng.pdf?ua=1 [Google Scholar]
- 10.Vonbank A., Agewall S., Kjeldsen K.P., Lewis B.S., Torp-Pedersen C., Ceconi C., Funck-Brentano C., Kaski J.C., Niessner A., Tamargo J., Walther T., Wassmann S., Rosano G., Schmidt H., Saely C.H., Drexel H. Comprehensive efforts to increase adherence to statin therapy. Eur. Heart J. 2017;38:2473–2479. doi: 10.1093/eurheartj/ehw628. [DOI] [PubMed] [Google Scholar]
- 11.Deichmann R.E., Morledge M.D., Ulep R., Shaffer J.P., Davies P., van Driel M.L. A metaanalysis of interventions to improve adherence to lipid-lowering medication. Ochsner J. 2016;16:230–237. [PMC free article] [PubMed] [Google Scholar]
- 12.Koskinas K.C., Siontis G.C.M., Piccolo R., Mavridis D., Räber L., Mach F., Windecker S. Effect of statins and non-statin LDL-lowering medications on cardiovascular outcomes in secondary prevention: a meta-analysis of randomized trials. Eur. Heart J. 2018;39:1172–1180. doi: 10.1093/eurheartj/ehx566. [DOI] [PubMed] [Google Scholar]
- 13.Turgeon R.D., Tsuyuki R.T., Gyenes G.T., Pearson G.J. Cardiovascular efficacy and safety of PCSK9 inhibitors: systematic review and meta-analysis including the ODYSSEY OUTCOMES trial. Can. J. Cardiol. 2018;34:1600–1605. doi: 10.1016/j.cjca.2018.04.002. 2018. [DOI] [PubMed] [Google Scholar]
- 14.Iqbal Z., Dhage S., Mohamad J.B., Abdel-Razik A., Donn R., Malik R., Ho J.H., Liu Y., Adam S., Isa B., Stefanutti C., Soran H. Efficacy and safety of PCSK9 monoclonal antibodies. Expet Opin. Drug Saf. 2019;18:1191–1201. doi: 10.1080/14740338.2019.1681395. [DOI] [PubMed] [Google Scholar]
- 15.Wong N.D., Rosenblit P.D., Greenfield R.S. Advances in dyslipidemia management for prevention of atherosclerosis: PCSK9 monoclonal antibody therapy and beyond. Cardiovasc. Diagn. Ther. 2017;7:11–20. doi: 10.21037/cdt.2017.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


