Editor-Neurologic dysfunction following major cardiac surgery is characterized by a decline in memory and executive function.1 This cognitive decline, which approximates Alzheimer's Disease and Related Dementias (ADRD), is evident at hospital discharge, followed by early improvement at six months, and worsening at five years.1 Worse, the cognitive decline associated with patients who develop postoperative delirium is accelerated.2 Recent studies suggest underlying patient vulnerabilities contribute to delirium.3,4 Midlife cardiovascular risk factors have been associated with increased amyloid aggregation in the brain5 and cognitive impairment later in life.6 However, a critical unknown is whether major cardiac surgery exacerbates latent pathophysiology underlying ADRD.
The phosphorylated tau isoforms at threonine 217 (P-tau 217) and 181 (P-tau 181) are newly identified systemic biomarkers of ADRD7 associated with synaptic and neuronal dysfunction and neurodegeneration. Interestingly, total tau (T-tau) and P-tau 181 levels have been shown to be increased following major cardiac surgery compared to preoperative levels.8 Postoperative plasma tau levels are associated with delirium incidence in noncardiac9 and thoracic vascular surgical cohorts,10 though it remains unclear if associations between elevated tau levels and postoperative delirium extend to major cardiac surgical populations.
We performed a case-control study of data from patients (n = 38) scheduled for major cardiac surgery with cardiopulmonary bypass to assess relative tau and phosphorylated-tau levels in serum before and after surgery to identify any associations with development of postoperative delirium. The Mass General Brigham Human Research Committee approved this human research study (Supplemental Methods). All participants gave written informed consent. Blood was collected before surgical incision and on postoperative day 1. Patients were screened for postoperative delirium and severity with the Confusion Assessment Method twice daily beginning on postoperative day 1 until postoperative day 3. We used the newly developed nanoneedle technology to measure serum concentrations of tau. Models were created to assess associations between tau and delirium, both before and after adjusting for age and preoperative cognitive status. Odds ratio (OR), area under the receiver operating curve (AUROC), and beta coefficients were used to enable inferences. All analyses used two-tailed hypothesis testing, with statistical significance interpreted at p<0.05.
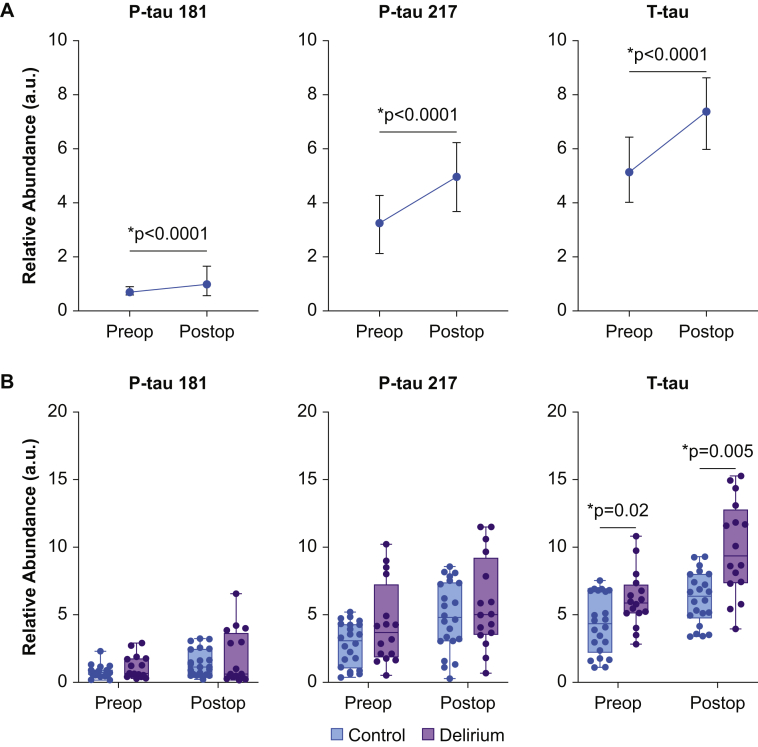
Our study cohort comprised 12 women and 26 men with median age of 70 (range, 60 to 85) yr who underwent major cardiac surgery (Supplementary Table S1). We found that P-tau 181 (mean difference: 0.67, 95% Confidence Interval (CI) [0.4 to 0.95]), p<0.0001), P-tau 217 (mean difference: 1.85 [CI 1.35 to 2.34]), p<0.0001), and T-tau (mean difference: 2.69 [CI 2.03 to 3.35]), p<0.0001) were elevated after surgery (Fig 1A). However, only preoperative T-tau (OR: 1.52 [CI 1.06 to 2.17]; p=0.02) and postoperative T-tau (OR: 1.66 [CI 1.17 to 2.36]; p=0.005) were associated with delirium (Fig 1B). Moreover, postoperative T-tau was more specific than preoperative T-tau for postoperative delirium (AUROC: 0.81 [CI 0.67 to 0.96] vs AUROC: 0.7 [CI 0.53 to 0.87], respectively) and significantly correlated with delirium severity (β coefficient: 0.34 [CI 0.05 to 0.63], p=0.02, Supplementary Fig. S1). These results were conserved for models adjusted for age and baseline cognitive function (Supplementary Table S2) and were not affected by surgical admission status (in-patient or same-day admission; Supplementary Figure S2).
Fig 1.
Preoperative and postoperative total tau serum levels are associated with delirium. (A) Relative abundance of P-tau 181, P-tau 217, and T-tau before and after surgery (postoperative day 1, POD1). Data shown as median (95% CI). Statistical significance between preoperative and postoperative levels were determined based on paired t-test. (B) Preoperative and postoperative serum levels in patients with delirium compared to age- and sex-matched control patients. Tau protein serum levels were measured as a relative abundance in arbitrary units (a.u.). Statistical significance was based on an unadjusted univariate model constructed using logistic regression. The values from the multivariable model are adjusted for age and preoperative a-MoCA (shown in Supplementary Table S2).
In this case-control analysis, we show that serum T-tau, P-tau 217, and P-tau 181 were elevated after major cardiac surgery. Only T-tau was associated with the incidence and severity of postoperative delirium, suggesting a mechanistic link between postoperative delirium and T-tau, upstream of tau hyperphosphorylation and cortical aggregation of these tau isoforms. Our findings suggest that T-tau could be developed as a biomarker for postoperative delirium. Further, they suggest that the perioperative period may be leveraged to enable fundamental new insights into tau regulation and ADRD pathophysiology. Future studies of P-tau 181, P-tau 217, and other P-tau isoforms, including later timepoints beyond postoperative day 3, are expected to enable insights into the longer-term decline in memory and executive function associated with cardiac surgery.
Authors' contributions
Conception: OA, ZX, JW-K, JQ, TBM.
Design: all authors.
Data acquisition: FL, JQ, ZX, TBM.
Data analysis: AM, TBM, OA.
Data interpretation: OA, TBM.
Drafting/revising/approving of final paper: all authors.
Funding
This work was supported by the National Institutes of Health R01AG053582 (Bethesda, MD, USA). We would also like to acknowledge the research fund from the Department of Anesthesia, Critical Care and Pain Medicine at Massachusetts General Hospital and Harvard Medical School in supporting the Anesthesia Biomarker Core. The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of Interest
The authors declare no conflict of interests.
Editor: Hugh C Hemmings Jr
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2022.04.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Newman M.F., Kirchner J.L., Phillips-Bute B., Gaver V., Grocott H., Jones R.H., et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 2.Saczynski J.S., Marcantonio E.R., Quach L., Fong T.G., Gross A., Inouye S.K., et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–39. doi: 10.1056/NEJMoa1112923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neuman M.D., Feng R., Carson J.L., Gaskins L.J., Dillane D., Sessler D.I., et al. Spinal Anesthesia or General Anesthesia for Hip Surgery in Older Adults. N Engl J Med. 2021;385:2025–2035. doi: 10.1056/NEJMoa2113514. [DOI] [PubMed] [Google Scholar]
- 4.Li T., Li J., Yuan L., Wu J., Jiang C., Daniels J., et al. Effect of Regional vs General Anesthesia on Incidence of Postoperative Delirium in Older Patients Undergoing Hip Fracture Surgery: The RAGA Randomized Trial. JAMA. 2021;327:50–58. doi: 10.1001/jama.2021.22647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottesman R.F., Schneider A.L., Zhou Y., Coresh J., Green E., Gupta N., et al. Association Between Midlife Vascular Risk Factors and Estimated Brain Amyloid Deposition. Jama. 2017;317:1443–1450. doi: 10.1001/jama.2017.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gottesman R.F., Albert M.S., Alonso A., Coker L.H., Coresh J., Davis S.M., et al. Associations Between Midlife Vascular Risk Factors and 25-Year Incident Dementia in the Atherosclerosis Risk in Communities (ARIC) Cohort. JAMA Neurol. 2017;74:1246–1254. doi: 10.1001/jamaneurol.2017.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thijssen E.H., La Joie R., Strom A., Fonseca C., Iaccarino L., Wolf A., et al. Plasma phosphorylated tau 217 and phosphorylated tau 181 as biomarkers in Alzheimer's disease and frontotemporal lobar degeneration: a retrospective diagnostic performance study. Lancet Neurol. 2021;20:739–752. doi: 10.1016/S1474-4422(21)00214-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feinstein I., Wilson E.N., Swarovski M.S., Andreasson K.I., Angst M.S., Greicius M.D. Plasma Biomarkers of Tau and Neurodegeneration During Major Cardiac and Noncardiac Surgery. JAMA Neurol. 2021;78:1407–1409. doi: 10.1001/jamaneurol.2021.2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ballweg T., White M., Parker M., Casey C., Bo A., Farahbakhsh Z., et al. Association between plasma tau and postoperative delirium incidence and severity: a prospective observational study. Br J Anaesth. 2021;126:458–466. doi: 10.1016/j.bja.2020.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker M., White M., Casey C., Kunkel D., Bo A., Blennow K., et al. Cohort Analysis of the Association of Delirium Severity with Cerebrospinal Fluid Amyloid-Tau-Neurodegeneration Pathologies. J Gerontol A Biol Sci Med Sci. 2021:glab203. doi: 10.1093/gerona/glab203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.