Abstract
Background
Prevention of hearing loss via addressing potentially modifiable risk factors may offer means of reducing the global burden of hearing loss. Prior studies reported associations between individual markers of inflammation and risk of hearing impairment. Allostatic load is an index of cumulative physiological stressors, including inflammation, to multiple biological systems. Our aims were to investigate associations between allostatic load and both audiometric and self-reported hearing impairment and examine whether associations are stronger over time due to prolonged high allostatic load.
Methods
Data were taken from the English Longitudinal Study of Ageing (ELSA), a nationally representative study of people aged 50+ living in England over 3 time points between 2008 and 2014. Allostatic load score was comprised of thirteen different measures available at baseline and 4 years post-baseline (high-density lipoprotein/total cholesterol, triglyceride, fibrinogen, haemoglobin A1c, C-reactive protein, insulin-like growth factor 1 (IGF-1), systolic and diastolic blood pressure, mean arterial pressure, resting pulse rate, peak expiratory flow, BMI and waist circumference), measured using clinical cut-off points for normal biomarker parameters. Hearing acuity was measured with a simple handheld tone-producing device at follow-up 7 years post-baseline, while self-reported hearing impairment was measured at time point.
Results
We included samples of 4373 and 4430 for the cross-sectional and longitudinal analysis, respectively. In the cross-sectional model high allostatic load was associated both self-reported (OR = 1.08, 95% CI 1.0,1.1; p < 0.01) and objective hearing loss (OR = 1.10, 95% CI 1.1,1.2; p < 0.001) adjusting for age and sex. Cross-sectional associations between allostatic load and hearing were not significant after further adjustment for covariates (qualification, physical activity and smoking).
In longitudinal modelling, high allostatic load was associated with both audiometric (Z score OR = 1.11, 95% CI 1.1,1.2; p < 0.001) and self-reported hearing impairment (OR = 1.08, 95% CI 1.0,1.1; p < 0.001) adjusting for age and sex. Allostatic load was no longer associated with self-reported hearing loss but the association with audiometric hearing impairment (OR = 1.08, 95% CI 1.03,1.13; p < 0.001) remained following additional adjustment for baseline self-reported hearing, education, physical activity, and smoking.
Conclusions
Prolonged high allostatic load was associated with risk of hearing impairment. Reducing allostatic load via healthy lifestyle changes including non-smoking, healthy diet and exercise may offer an opportunity to reduce the risk of hearing impairment in later life.
Keywords: Allostatic load, Hearing impairment, Fibrinogen, Haemoglobin A1c, C-reactive protein, Insulin-like growth factor 1 (IGF-1), Ageing
Highlights
-
•
Allostatic load captures cumulative physiological stress which has consequence for subsequent hearing function.
-
•
Prolonged high allostatic load was associated with risk of objectively measured hearing impairment.
-
•
This association is shown in nationally representative longitudinal ageing study.
1. Introduction
Around 1 in five UK adults has a hearing impairment (RNID, 2021). Hearing impairment is the 4th leading cause of years lived with disability globally (Murray et al., 2020). It is associated with a range of detrimental health outcomes including disability (Chen et al., 2015), depression (Cosh et al., 2019), dementia risk (Livingston et al., 2020) and lower quality of life (Dalton et al., 2003), while also placing burdens on economic and healthcare systems through costly management and unemployment (Huddle et al., 2017). As age-related hearing impairment is incurable, preventing or delaying hearing impairment by management of modifiable risk factors is an important means of reducing its impact.
Allostatic load is a cumulative measure of the physiological stressors to the body throughout the life course, reflected by damage to multiple biological systems over time (McEwen, 1998; Seeman et al., 2001, 2010). An advantage using allostatic load in predicting health outcomes, as opposed to the use of single biomarkers, is that it captures the effects of stressors on several biological systems simultaneously (Gallo et al., 2014; Juster et al., 2010). Additionally, the effects of individual biomarkers are susceptible to socio-demographic biases, such as gender and race, and using a composite measure of a number of biomarkers is a potentially more reliable means of modelling effects on health outcomes (Gupta et al., 2019). Allostatic load is linked to socioeconomic position (Gruenewald et al., 2012; Szanton et al., 2005), suggesting that allostatic load is a useful means of identifying health risks as well as the mechanisms of ageing across the life course. Allostatic load predicts various health outcomes, including physical function, frailty, self-reported health, mental well-being, dementia and mortality (McEwen and Rasgon, 2018; Read and Grundy, 2014).
Several conditions implicated with high allostatic load have associations with hearing impairment, including diabetes (Samocha-Bonet et al., 2021), obesity (Croll et al., 2019), sub-clinical atherosclerosis (Fischer et al., 2015) and vascular degeneration (Lowthian et al., 2016) as have behaviours including poor diet (Dawes et al., 2020) and smoking (Dawes et al., 2014). However, little work has been carried out into the association between inflammatory biomarkers and hearing impairment, and none (to our knowledge) on the association with allostatic load. A small number of studies have found associations between individual inflammation factors and risk of incident audiometric hearing impairment, including lower levels of insulin-like growth factor I (Lassale et al., 2017), high C-reactive protein (Nash et al., 2014) and higher white blood cell count (Lassale et al., 2020). Studies have also reported associations between higher white blood cell count and prevalent audiometric hearing impairment (Verschuur et al., 2012, 2014). One study showed allostatic load was associated with a range of disabilities but was not associated with self-reported hearing impairment, although the work was cross-sectional and sample size was small (Hollar, 2013). Longitudinal studies suggest that high levels of inflammation biomarkers sustained over several years have a stronger association with hearing impairment than high levels of inflammation biomarkers at a single time point (Lassale et al., 2020; Nash et al., 2014). Nash et al. (2014) reported that serum levels of C-reactive protein, interleukin-6 or tumor necrosis factor-α from a single time point were not associated with incident audiometric hearing impairment. But among people younger than 60 years, those with consistently high levels of C-reactive protein over 10 years were twice as likely to develop hearing loss than those with low levels of C-reactive protein. It has been postulated that analyses of health outcomes in relation to allostatic load should be longitudinal due to allostatic load being a measure of sustained stress on biological systems (Gallo et al., 2014). This study will test i) associations between allostatic load and both audiometric and self-reported hearing impairment and ii) whether associations are stronger over time due to increased duration of higher allostatic load.
2. Methods
Data were taken from the English Longitudinal Study of Ageing (ELSA), a nationally representative study of people aged 50 and over living in England (Zaninotto et al., 2019). Data were collected in biannual assessment waves commencing in 2002. Biomarker data were included in every even numbered wave. This study used biomarker data from waves 4 and 6 (2008 and 2012), omitting data from wave 2 due to a smaller number of measures available and higher sample attrition over time. Audiometric hearing assessment was included at wave 7 (2014), the only wave at which it was measured. For the longitudinal analysis, the sample included 4430 core members with biomarker data and no missing covariate data at wave 4 and who had completed the hearing test at wave 7. The cross-sectional analysis consisted of 4373 with biomarker and full covariate data at wave 6, again who had also completed the hearing test at wave 7.
2.1. Hearing acuity
At wave 7, respondents underwent an audiometric hearing test using a Siemens HearCheck device (Parving et al., 2008). Respondents did not do the hearing test if they used cochlear implants, had an ear infection or were unable to participate for other reasons. If respondents wore a hearing aid, it was removed for the test. During the test, participants were asked how many of the three tones they heard for each frequency (1000 Hz and 3000 Hz) in each ear. A binary variable was constructed from the results, with respondents classed as not having a hearing impairment if they heard two or more low-pitched sounds (1000Hz) and at least one high-pitched sound (3000Hz) in the better hearing ear, corresponding to audiometric hearing thresholds greater than 35 dB HL at 1000 Hz and 3000 Hz. The Siemens HearCheck test has good sensitivity (78%–92%) and acceptable to good specificity (62%–95%) in comparison with full pure tone audiometry (Reyes-quintos et al., 2011). At each wave of ELSA, respondents were asked to self-report their hearing, using a hearing aid if they usually wore one, within categories of ‘excellent’, ‘very good’, ‘good’, ‘fair’ or ‘poor’. Respondents were defined as having a self-reported hearing impairment if they selected ‘fair’ or ‘poor’. Self-reported hearing is a measure of self-perceived hearing disability, rather than a measure of impairment. However, self-reported hearing strongly correlates with audiometric hearing impairment, and self-reported hearing is commonly used to index hearing impairment in population studies. The Australian Blue Mountains hearing study estimated sensitivity, specificity, positive predictive value and negative predictive value rates of 78%, 67%, 61% and 82% of self-report hearing measures against audiometrically identified hearing impairment (Sindhusake et al., 2001). The American Epidemiology of Hearing loss study (Nondahl et al., 1998) reported similar rates (71%, 71%, 68% and 74%).
2.2. Allostatic load
Allostatic load score was comprised of thirteen different measures available in both waves 4 and 6 of ELSA (high-density lipoprotein/total cholesterol, triglyceride, fibrinogen, haemoglobin A1c, C-reactive protein, insulin-like growth factor 1 (IGF-1), systolic and diastolic blood pressure, mean arterial pressure, resting pulse rate, peak expiratory flow, BMI and waist circumference), reflecting five biological systems (cardiovascular, metabolic, body fat, inflammation and respiratory). This measure is line with other studies of allostatic load using observational studies (Read and Grundy, 2014; Tampubolon and Maharani, 2018). Details of how all biomarker variables were measured and collected are described elsewhere (NatCen Social Research, 2018).
Considering previously inconsistent findings relating to individual biomarkers and hearing, we tested robustness of results by calculating four versions of the allostatic load score previously reported in research literature. Firstly, we used clinical cut-off points for each biomarker and assigned a binary response where 1 identified a value out of normal range (Sibille et al., 2017): (HDL <1.03 mmol/L (Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults, 2001); triglyceride >1.7 mmol/L (National Institute for Health and Clinical Excellence, 2011); fibrinogen >4.0gL (Koenig, 2003); Hb1AC >6.5% (Nathan et al., 2008); CRP >3.0 mg/l (Pearson et al., 2003); IGF-1 <5 and >26 nmol/L for men, <4 and >23 nmol/L for women (Mayo Clinic, 2014); systolic blood pressure >140mmHg, diastolic blood pressure >90 mmHg, mean arterial pressure <70 mmHg or >110 mmHg (James et al., 2014); resting pulse <60 beats per minute or >100 beats per minute (James et al., 2014); peak expiratory flow <5 L (Barreiro and Perillo, 2004); BMI >30 kg/m2, waist circumference >102 cm for men, >88 cm for women (National Institute for Health and Clinical Excellence, 2011). Potential scores ranged from 0 (no biomarkers outside of normal range) to 13 (all biomarkers outside normal range). Secondly, we created Z scores by standardising each individual biomarker variable to have a mean of zero and standard deviation of one, subsequently taking the average of the standardised scores and creating a summary score with a range of −1.28 (lower allostatic load) to 1.78 (higher allostatic load) (Tampubolon and Maharani, 2018). Thirdly, we calculated a score based on individuals belonging to the highest quartile biomarker level indicating risk to health using sample distributions for men and women. The proportion of biomarkers falling within the top quartile for each individual was calculated for each of the five biological systems to weight the score, with a final range of 0–514. Fourthly, we included the top quartile biomarker scores as an unweighted continuous summed score, with a range of 0–13. Main results are presented using the clinical cut-off variable, with results using the other three measures in the Appendix 1.
To measure long-term exposure to allostatic load following previous research on biomarker exposure and hearing (Lassale et al., 2020), we calculated mean scores for each of the four allostatic load variables from waves 4 and 6. Taking the average of each biomarker measurement also limits potential bias due to biological variability and natural fluctuations in biomarker levels (Clarke et al., 1999). Where individuals had only biomarker information at one wave, this score was included. A sensitivity analysis was run (Appendix 2), whereby only individuals with biomarker data at both waves 4 and 6 were included in models.
2.3. Covariates
Fully adjusted models controlled for a variety of covariates measured at baseline. Education was included as a three-category variable with response options ‘less than O-level (GCSE)’, ‘O-level or equivalent’ and ‘higher than O-level’. O-levels are the end of secondary-level education in the United Kingdom, taken at age 16. Reported physical activity level, with categories of ‘vigorous’, ‘moderate’, ‘mild’ and ‘sedentary’ was dichotomised to compare those with sedentary lifestyles to any form of physical activity. Finally, smoking status was categorised and included as ‘never’, ‘former’ or ‘current’. In each model, baseline self-reported hearing was controlled for, as was respondent age and sex.
2.4. Statistical analysis
The association between hearing impairment and allostatic load was investigated by means of logistic regression models. Models for objectively measured and self-reported hearing impairment were run separately. Two sets of models were run: the first controlled only for baseline self-reported hearing, age and sex, and the second further controlled for educational attainment, physical activity and smoker status. Firstly, cross-sectional models were run using only allostatic load scores and covariates from wave 6, in relation to both objectively measured and self-reported hearing impairment at wave 7. Secondly, to establish whether long-term exposure to higher allostatic load influences hearing, longitudinal models regressed the four mean allostatic load scores from waves 4 and 6 on audiometric hearing and self-reported hearing impairments at wave 7. The sensitivity analysis was run for all longitudinal models. Analyses were performed using Stata 14.
3. Results
Table 1 shows descriptive statistics of the sample. Of all respondents, 37.8% had an audiometric hearing impairment, while 21.3% had a self-reported hearing impairment at wave 7. Individuals with audiometric hearing impairment were more likely to be older, male, have lower educational attainment and to have a sedentary lifestyle. For all measures of allostatic load, those with an audiometric hearing impairment had higher scores than those with no impairment. Less than a third of people with an audiometric hearing impairment at wave 7 self-reported hearing impairment in the same wave.
Table 1.
Sample characteristics at baseline (wave 4) by hearing impairment at follow-up (wave 7) and objective hearing impairment by self-reported hearing impairment at wave 7.
| Overall | No hearing impairment | Hearing impairment | p-value | |
|---|---|---|---|---|
| N (%) | 4430 | 2757 (62.23%) | 1673 (37.77%) | |
| Age | 64.1 (7.99) | 61.6 (SD 6.63) | 68.2 (SD 8.34) | p < 0.001 |
| Female | 54.75% | 57.78% | 49.80% | p < 0.001 |
| Education | p < 0.001 | |||
| Less than o-level or equivalent | 35.20% | 29.75% | 44.08% | |
| O-level or equivalent | 28.99% | 30.59% | 26.39% | |
| Higher than o-level | 35.81% | 39.66% | 29.54% | |
| Physical activity | p < 0.001 | |||
| Sedentary | 5.9% | 3.48% | 9.85% | |
| Smoker status | p = 0.126 | |||
| Never smoked | 41.92% | 43.06% | 40.07% | |
| Former smoker | 46.82% | 45.77% | 48.54% | |
| Current smoker | 11.25% | 11.17% | 11.39% | |
| Self-reported hearing | p < 0.001 | |||
| Excellent | 20.27% | 26.38% | 10.30% | |
| Very good | 29.04% | 33.75% | 21.35% | |
| Good | 33.70% | 31.65% | 37.03% | |
| Fair | 14.11% | 7.55% | 24.79% | |
| Poor | 2.90% | 0.67% | 6.53% | |
| Allostatic load scores | ||||
| Z-score | −0.12 (0.42) | −0.03 (0.424) | 0.02 (0.41) | p < 0.001 |
| Clinical cut-off | 3.39 (1.79) | 3.30 (1.78) | 3.53 (1.80) | p < 0.001 |
| Weighted top quartile | 1.24 (0.94) | 1.15 (0.93) | 1.38 (0.96) | p < 0.001 |
| Continuous top quartile |
3.39 (2.56) |
3.21 (2.56) |
3.68 (2.53) |
p < 0.001 |
| Wave 7 only | ||||
| Has hearing impairment defined by self-reported variable | ||||
| 21.33% | 30.69% | 69.31% | p < 0.001 | |
Notes: Reported are mean (SD) or percentage.
3.1. Cross-sectional analysis
Table 2 shows the results of the cross-sectional models of allostatic load and hearing impairment. Model 1, controlling for just age and sex, produced significant estimates for the effect of allostatic load, measured by means of clinical cut-off points, on audiometric hearing impairment (OR = 1.10, 95% CI 1.1,1.2; p < 0.001). Appendix 1 shows similar results using the three alternative measures of allostatic load (z scores, weighted top quartiles and continuous top quartiles). Allostatic load was also a significant predictor self-reported hearing impairment (OR = 1.08, 95% CI 1.0,1.1; p < 0.01). The alternative allostatic load measures produced similar associations with self-reported hearing impairment (Appendix 1).
Table 2.
Cross-sectional association between allostatic load (measured using clinical cut-off points for normal biomarker parameters) and hearing impairment. Results of logistic regression models (odds ratios and confidence intervals).
| Hearing loss |
Self-reported hearing loss |
|||
|---|---|---|---|---|
| Model 1 | Model2 | Model 1 | Model 2 | |
| Allostatic load | 1.10*** (1.1,1.2) | 1.06 (0.99,1.13) | 1.08** (1.0,1.1) | 1.08 (0.9,1.2) |
| Baseline self-reported hearing (ref. excellent) | ||||
| Very good | 1.56** (1.1,2.1) | |||
| Good | 3.11*** (2.3,4.2) | |||
| Fair | 7.92*** (5.5,11.5) | |||
| Poor | 39.33*** (15.9,97.9) | |||
| Female | 0.64*** (0.6,0.8) | 0.91 (0.7,1.1) | 0.47*** (0.4,0.6) | 0.68** (0.5,0.9) |
| Age | 1.11*** (1.1,1.1) | 1.11*** (1.1,1.1) | 1.04*** (1.0,1.1) | 1.02** (1.0,1.0) |
| Qualifications (ref. Higher than O-level) | ||||
| Less than O-level | 1.58*** (1.2,2.0) | 1.02 (0.8,1.4) | ||
| O-level or equivalent | 1.18 (0.9,1.5) | 0.88 (0.7,1.2) | ||
| Sedentary lifestyle | 2.25** (1.3,4.7) | 1.49 (0.7,3.4) | ||
| Smoker status (ref. Never smoked) | 0.95 (0.8,1.2) | 0.89 (0.7,1.2) | ||
| Former | 1.09 (0.8,1.6) | 0.99 (0.6,1.6) | ||
| Current | ||||
***p < 0.001; **p < 0.01; *p < 0.05.
Models 1 control for age and sex. Models 2 control for age, sex, qualification, physical activity and smoker status.
All cross-sectional results become non-significant when controlling for confounding factors. Age was consistently associated with poorer hearing when measured both audiometrically and via self-report and being female with better hearing for both measures. Sedentary lifestyle and poorer educational attainment were associated with audiometric hearing impairment, but not self-reported hearing impairment.
3.2. Longitudinal analysis
Table 3 shows the results of the longitudinal models of allostatic load with audiometric and self-reported hearing impairment. Using the measure based on clinical cut-off points, allostatic load had a positive association with audiometric hearing impairment (Z score OR = 1.11, 95% CI 1.1,1.2; p < 0.001) and self-reported hearing impairment (OR = 1.08, 95% CI 1.0,1.1; p < 0.001) in Model 1.
Table 3.
Longitudinal association between allostatic load (measured using clinical cut-off points for normal biomarker parameters) and hearing impairment. Results of logistic regression models (odds ratios and confidence intervals).
| Hearing loss |
Self-reported hearing loss |
|||
|---|---|---|---|---|
| Model 1 | Model2 | Model 1 | Model 2 | |
| Allostatic load | 1.113*** (1.15,1.26) | 1.08*** (1.04,1.13) | 1.08** (1.05,1.12) | 1.05 (1.05,1.11) |
| Baseline self-reported hearing (ref. excellent) | ||||
| Very good | 1.54*** (1.23,1.93) | 2.44*** (1.61,3.70) | ||
| Good | 2.66*** (2.15,3.29) | 8.33*** (5.67,12.25) | ||
| Fair | 7.17*** (5.54,9.28) | 30.43*** (20.39,45.41) | ||
| Poor | 19.72*** (11.43,34.05) | 62.61*** (36.35,107.84) | ||
| Female | 0.63*** (0.63,0.75) | 0.73*** (0.63,0.85) | 0.47*** (1.05,1.10) | 0.59*** (0.50,0.70) |
| Age | 1.12*** (1.11,1.13) | 1.12*** (1.11,1.13) | 1.05*** (1.01,1.03) | 1.03*** (1.02,1.04) |
| Qualifications (ref. Higher than O-level) | ||||
| Less than O-level | 1.40*** (1.17,1.66) | 1.21 (0.99,1.48) | ||
| O-level or equivalent | 1.18 (0.98,1.41) | 1.03 (0.83,1.27) | ||
| Sedentary lifestyle | 2.11** (1.38,3.22) | 1.55 (0.99,2.42) | ||
| Smoker status (ref. Never smoked) | ||||
| Former | 0.88 (0.76,1.02) | 0.89 (0.74,1.06) | ||
| Current | 1.29* (1.02,1.64) | 1.18 (0.89,1.56) | ||
***p < 0.001; **p < 0.01; *p < 0.05.
Models 1 control for age and sex. Models 2 control for age, sex, qualification, physical activity and smoker status.
In Model 2, with additional adjustment for baseline self-reported hearing, education, physical activity and smoker status, allostatic load retained its association with audiometric hearing impairment (clinical cut-off score OR = 1.08, 95% CI 1.03,1.13; p < 0.001) but not for self-reported hearing impairment. Appendix 2 shows models with alternative measures of allostatic load produced the same significant positive coefficients, after controlling for all other variables.
4. Discussion
Among adults aged 50 and over living in England, long-term exposure to higher allostatic load was associated with increased likelihood of audiometric hearing impairment, but not with self-reported hearing impairment. This finding remained significant after controlling for socio-demographic factors including age, sex, education and physical activity. There was no cross-sectional association between allostatic load and either audiometric or self-report measures of hearing impairment, suggesting short-term exposure to high allostatic load is not a significant risk factor for hearing impairment. That consistently high allostatic load should increase risk of hearing impairment is consistent with the conceptualisation of the adverse health impacts of allostatis due to chronic stress to biological systems. Associations between higher allostatic load and poorer audiometric hearing outcomes were robust to four alternative allostatic load indices.
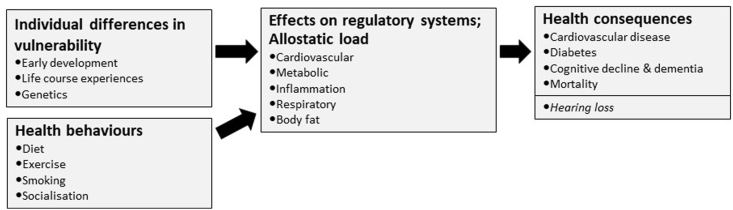
The observation that allostatic load is related to hearing impairment correlates with previous work on various markers of general health and hearing. These include higher BMI (Croll et al., 2019), diabetes (Samocha-Bonet et al., 2021) and atherosclerosis (Fischer et al., 2015). As many of the biomarkers included in the allostatic load score share links with single biomarkers of general health, the similarity in association with hearing impairment is not surprising. But there are benefits to using a composite health index such as allostatic load rather than single biomarkers in relation to understanding the impact of systemic health on hearing. Firstly, while individual biomarkers might demonstrate the effect of the health of one biological system on hearing, the effects of stress on health over time affect various biological systems simultaneously, and allostatic load is a useful means of capturing this. Secondly, individual biomarkers are subject to bias from factors including gender, and using a composite biomarker measure is a means of reducing such bias (Seeman et al., 1997). The finding that relationships between allostatic load and hearing impairment were only present in longitudinal analyses is in line with research suggesting longer-term exposure to allostatic load is a greater risk factor to hearing than short term exposure (Nash et al., 2014). Fig. 1 shows potential health consequences of long-term exposure to excess allostatic load, including hearing loss. Hearing loss is a major source of burden in terms of years lived with disability (Murray et al., 2020), so understanding causal pathways to inform interventions to reduce risk of hearing loss is worthwhile in itself. A recent review additionally identified hearing loss as a potentially modifiable risk for dementia (Livingston et al., 2020), stimulating interest in whether hearing loss interventions may reduce dementia risk. But based as it is on observational data, the studies linking hearing loss to risk of dementia summarised in Livingston et al.’s review do not elucidate whether hearing loss is causally linked to dementia risk or not. A possible explanation for the association is that hearing loss is a marker of dementia risk due to shared causes that impact both hearing and cognitive health (Wayne and Johnsrude, 2015). We are currently modelling allostatic load as a ‘common cause’ versus other hypotheses for relationships between hearing loss and dementia risk.
Fig. 1.
Conceptual schematic of health consequences of long-term exposure to excess allostatic load.
The finding that allostatic load is a predictor of audiometric but not self-reported hearing impairments corroborates with evidence suggesting that self-reported hearing loss strongly correlates with, but under-estimates audiometric hearing impairment (Nondahl et al., 1998; Sindhusake et al., 2001). This under-estimation is due to self-reported hearing indexing the perceived psychosocial impacts of hearing difficulties, and may be biased by denial and/or individual circumstances affecting a person's own view of their hearing ability (Choi et al., 2016; Keidser et al., 2015; Pronk et al., 2018). In other words, self-reported hearing is a measure of self-perceived disability - which is affected by psychosocial context - while audiometric measures index hearing impairment – which is not. It follows that audiometric measures are more closely associated with pathology causing hearing impairment than measures of hearing disability. This study is the first that we know of to compare the effect of allostatic load on both an objective and subjective health outcome.
This study expands on previous work examining associations between biomarkers and hearing impairment in several ways. First, it is the only study to examine the effect of allostatic load on hearing, rather than that of individual biomarkers. Second, we used a large, nationally representative dataset where previous work has often been based on small sample sizes. Third, we have been able to include a longitudinal element with good follow-up, where much previous work has been cross-sectional in nature (Hollar, 2013; Hollar Jr and Lewis, 2015; Verschuur et al., 2012, 2014). Fourth, the study used four measures of allostatic load to ensure robustness of results.
There are some limitations to the current study. Results may be biased by attrition, with individuals dropping out between study waves more likely to be those with greater risk factors for both outcome and exposure, such as those who are older, less educated and more likely to engage in unhealthy lifestyle behaviours (Banks et al., 2011). However, as individuals with greater risk of dropout are often those with poorer health in the first instance (Matthews et al., 2004; Mein et al., 2012), any bias would lead towards a null hypothesis rather than an exaggeration of true effects. A second limitation is that there may be residual or uncontrolled confounds that impact associations between allostatic load and hearing (for example, if those with high allostatic load also have higher levels of damaging noise exposure). A second limitation is the HearCheck assessment, which tests hearing at only two frequencies (1 kHz and 3 kHz), compared to pure tone audiometry, the gold standard measure of hearing impairment which typically includes frequencies from 0.250 kHz to 8 kHz. The differences between HearCheck and pure tone audiometry may limit comparability with other studies that used pure tone audiometry. However, HearCheck does reliably identify hearing impairment (Parving et al., 2008; Reyes-quintos et al., 2011), and HearCheck data have been used to estimate prevalence of hearing impairment in the Health Survey for England (Scholes et al., 2018).
Hearing impairment is associated with prolonged high allostatic load. The individual components of allostatic load can be modified by healthy lifestyle changes including non-smoking, healthy diet and exercise. Monitoring biomarkers in older age and maintaining a healthy lifestyle may therefore lead to a reduced risk of hearing impairment in later-life.
Funding sources
The English Longitudinal Study of Ageing was developed by a team of researchers based at University College London, NatCen Social Research, the Institute for Fiscal Studies, the University of Manchester and the University of East Anglia. The data were collected by NatCen Social Research. The funding is currently provided by the National Institute on Aging in the US (grant numbers: 2RO1AG7644 and 2RO1AG017644-01A1), and a consortium of UK government departments coordinated by the National Institute for Health Research. Funding has also been received by the Economic and Social Research Council. The current analysis was supported by an International Project Grant from the Royal National Institute for Deaf People (RNID) and Alzheimer's Research UK. Piers Dawes was supported by the NIHR Manchester Biomedical Research Centre. The funders had no role in the design of this study and did not have any role during its execution, analyses, interpretation, and storage of the data or decision to submit results. The views expressed in this publication are those of the authors and not necessarily those of NIHR.
Data sharing
ELSA data are open access at https://www.ukdataservice.ac.uk/.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbih.2022.100496.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data are available by application to the English Longitudinal Study of Ageing (ELSA)
References
- Banks J., Muriel A., Smith J.P. Attrition and health in ageing studies: evidence from ELSA and HRS. Longitudinal Life Course Stud. 2011;2(2) doi: 10.14301/llcs.v2i2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreiro T., Perillo I. An approach to interpreting spirometry. Am. Fam. Physician. 2004;69(5):1107–1114. [PubMed] [Google Scholar]
- Chen D.S., Betz J., Yaffe K., Ayonayon H.N., Kritchevsky S., Martin K.R., Harris T.B., Purchase-Helzner E., Satterfield S., Xue Q.-L. Association of hearing impairment with declines in physical functioning and the risk of disability in older adults. J. Gerontol.: Biomed. Sci. Med. Sci. 2015;70(5):654–661. doi: 10.1093/gerona/glu207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.S., Betz J., Deal J., Contrera K.J., Genther D.J., Chen D.S., Gispen F.E., Lin F.R. A comparison of self-report and audiometric measures of hearing and their associations with functional outcomes in older adults. J. Aging Health. 2016;28(5):890–910. doi: 10.1177/0898264315614006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke R., Shipley M., Lewington S., Youngman L., Collins R., Marmot M., Peto R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am. J. Epidemiol. 1999;150(4):341–353. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- Cosh S., Helmer C., Delcourt C., Robins T.G., Tully P.J. Depression in elderly patients with hearing loss: current perspectives. Clin. Interv. Aging. 2019;14:1471. doi: 10.2147/CIA.S195824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croll P.H., Voortman T., Vernooij M.W., de Jong R.J.B., Lin F.R., Rivadeneira F., Ikram M.A., Goedegebure A. The association between obesity, diet quality and hearing loss in older adults. Aging (Albany NY) 2019;11(1):48. doi: 10.18632/aging.101717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton D.S., Cruickshanks K.J., Klein B.E.K., Klein R., Wiley T.L., Nondahl D.M. The impact of hearing loss on quality of life in older adults. Gerontol. 2003;43(5):661–668. doi: 10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- Dawes P., Cruickshanks K.J., Marsden A., Moore D.R., Munro K.J. Relationship between diet, tinnitus, and hearing difficulties. Ear Hear. 2020;41(2):289. doi: 10.1097/AUD.0000000000000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawes P., Cruickshanks K.J., Moore D.R., Edmondson-Jones M., McCormack A., Fortnum H., Munro K.J. Cigarette smoking, passive smoking, alcohol consumption, and hearing loss. J. Assoc. Res. Otolaryngol. 2014;15(4):663–674. doi: 10.1007/s10162-014-0461-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Fischer M.E., Schubert C.R., Nondahl D.M., Dalton D.S., Huang G.-H., Keating B.J., Klein B.E., Klein R., Tweed T.S., Cruickshanks K.J. Subclinical atherosclerosis and increased risk of hearing impairment. Atherosclerosis. 2015;238(2):344–349. doi: 10.1016/j.atherosclerosis.2014.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo L.C., Fortmann A.L., Mattei J. Allostatic load and the assessment of cumulative biological risk in biobehavioral medicine: challenges and opportunities. Psychosom. Med. 2014;76(7):478. doi: 10.1097/PSY.0000000000000095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald T.L., Karlamangla A.S., Hu P., Stein-Merkin S., Crandall C., Koretz B., Seeman T.E. History of socioeconomic disadvantage and allostatic load in later life. Soc. Sci. Med. 2012;74(1):75–83. doi: 10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Curhan S.G., Curhan G.C. Biomarkers of systemic inflammation and risk of incident hearing loss. Ear Hear. 2019;40(4):981. doi: 10.1097/AUD.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollar D. Cross-sectional changes in patterns of allostatic load among persons with varying disabilities, NHANES: 2001–2010. Disabil. Health J. 2013;6(3):177–187. doi: 10.1016/j.dhjo.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Hollar D.W., Jr., Lewis J.S. Heart age differentials and general cardiovascular risk profiles for persons with varying disabilities: NHANES 2001–2010. Disabil. Health J. 2015;8(1):51–60. doi: 10.1016/j.dhjo.2014.07.007. [DOI] [PubMed] [Google Scholar]
- Huddle M.G., Goman A.M., Kernizan F.C., Foley D.M., Price C., Frick K.D., Lin F.R. The economic impact of adult hearing loss: a systematic review. JAMA Otolaryngol. Head Neck Surg. 2017;143(10):1040–1048. doi: 10.1001/jamaoto.2017.1243. [DOI] [PubMed] [Google Scholar]
- James P.A., Oparil S., Carter B.L., Cushman W.C., Dennison-Himmelfarb C., Handler J., Lackland D.T., LeFevre M.L., MacKenzie T.D., Ogedegbe O. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- Juster R.-P., McEwen B.S., Lupien S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Keidser G., Seeto M., Rudner M., Hygge S., Rönnberg J. On the relationship between functional hearing and depression. Int. J. Audiol. 2015;54(10):653–664. doi: 10.3109/14992027.2015.1046503. [DOI] [PubMed] [Google Scholar]
- Koenig W. Fibrin (ogen) in cardiovascular disease: an update. Thromb. Haemostasis. 2003;89:601–609. 04. [PubMed] [Google Scholar]
- Lassale C., Batty G.D., Steptoe A., Zaninotto P. Insulin-like growth factor 1 in relation to future hearing impairment: findings from the English longitudinal study of ageing. Sci. Rep. 2017;7(1):1–9. doi: 10.1038/s41598-017-04526-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassale C., Vullo P., Cadar D., Batty G.D., Steptoe A., Zaninotto P. Association of inflammatory markers with hearing impairment: the English Longitudinal Study of Ageing. Brain Behav. Immun. 2020;83:112–119. doi: 10.1016/j.bbi.2019.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Huntley J., Sommerlad A., Ames D., Ballard C., Banerjee S., Brayne C., Burns A., Cohen-Mansfield J., Cooper C. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowthian J.A., Britt C., Rance G., Lin F., Woods R., Wolfe R., Nelson M., Dillon H., Ward S., Reid C. Slowing the progression of age-related hearing loss: rationale and study design of the ASPIRIN in HEARING, retinal vessels imaging and neurocognition in older generations (ASPREE-HEARING) trial. Contemp. Clin. Trials. 2016;46:60–66. doi: 10.1016/j.cct.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews F.E., Chatfield M., Freeman C., McCracken C., Brayne C., Cfas M. Attrition and bias in the MRC cognitive function and ageing study: an epidemiological investigation. BMC Publ. Health. 2004;4(1):1–10. doi: 10.1186/1471-2458-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo Clinic Interpretative handbook; test 35100: insulin-like growth factor 1 (IGF-1) and insulin-like growth factor binding protein 3 (IGFBP-3) growth panel. Clin. Inf. 2014 [Google Scholar]
- McEwen B.S. Stress, adaptation, and disease: allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen B.S., Rasgon N.L. 2018. The Brain and Body on Stress: Allostatic Load and Mechanisms for Depression and Dementia. [Google Scholar]
- Mein G., Johal S., Grant R.L., Seale C., Ashcroft R., Tinker A. Predictors of two forms of attrition in a longitudinal health study involving ageing participants: an analysis based on the Whitehall II study. BMC Med. Res. Methodol. 2012;12(1):1–7. doi: 10.1186/1471-2288-12-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C.J., Abbafati C., Abbas K.M., Abbasi M., Abbasi-Kangevari M., Abd-Allah F., Abdollahi M., Abedi P., Abedi A., Abolhassani H. Five insights from the global burden of disease study 2019. Lancet. 2020;396(10258):1135–1159. doi: 10.1016/S0140-6736(20)31404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash S.D., Cruickshanks K.J., Zhan W., Tsai M.Y., Klein R., Chappell R., Nieto F.J., Klein B.E.K., Schubert C.R., Dalton D.S. Long-term assessment of systemic inflammation and the cumulative incidence of age-related hearing impairment in the Epidemiology of hearing loss study. J. Gerontol.: Biol. Sci. Med. Sci. 2014:1–8. doi: 10.1093/gerona/glt075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NatCen Social Research User guide to the nurse visit datasets: waves 2, 4, 6, 8. 2018. http://doc.ukdataservice.ac.uk/doc/8346/mrdoc/pdf/8346_waves_2-4-6-8_nurse_data_user_guide_v01.pdf
- Nathan D.M., Kuenen J., Borg R., Zheng H., Schoenfeld D., Heine R.J., Group, A. c.-D. A. G. S Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31(8):1473–1478. doi: 10.2337/dc08-0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health & Clinical Excellence . National Institute for Clinical Excellence; London: 2011. Hypertension: Clinical Management of Primary Hypertension in Adults. [Google Scholar]
- Nondahl D.M., Cruickshanks K., Wiley T.L., Tweed T.S., Klein R., Klein B. Accuracy of self-reported hearing loss. Audiology. 1998;37:295–301. doi: 10.3109/00206099809072983. [DOI] [PubMed] [Google Scholar]
- Parving A., Sørup Sørensen M., Christensen B., Davis A.C. Evaluation of a hearing screener. Audiol. Med. 2008;6(2):115–119. [Google Scholar]
- Pearson T.A., Mensah G.A., Alexander R.W., Anderson J.L., Cannon R.O., III, Criqui M., Fadl Y.Y., Fortmann S.P., Hong Y., Myers G.L. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- Pronk M., Deeg D.J., Kramer S.E. Explaining discrepancies between the digit triplet speech-in-noise test score and self-reported hearing problems in older adults. J. Speech Lang. Hear. Res. 2018;61(4):986–999. doi: 10.1044/2018_JSLHR-H-17-0124. [DOI] [PubMed] [Google Scholar]
- Read S., Grundy E. Allostatic load and health in the older population of England: a crossed-lagged analysis. Psychosom. Med. 2014;76(7):490. doi: 10.1097/PSY.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes-quintos M.R.T., Tantoco M.L.C., Fellizar-lopez K.R., Abes G.T. Accuracy of Siemens HearCheck™ navigator as a screening tool for hearing loss. Philippine J. Otolaryngol. Head Neck Surg. 2011;26(1):1. 1. [Google Scholar]
- RNID Facts and figures on hearing loss and tinnitus. 2021. https://rnid.org.uk/about-us/research-and-policy/facts-and-figures/
- Samocha-Bonet D., Wu B., Ryugo D.K. Diabetes mellitus and hearing loss: a review. Ageing Res. Rev. 2021;71 doi: 10.1016/j.arr.2021.101423. [DOI] [PubMed] [Google Scholar]
- Scholes S., Biddulph J., Davis A., Mindell J.S. Socioeconomic differences in hearing among middle-aged and older adults: cross-sectional analyses using the Health Survey for England. BMJ Open. 2018;8(2) doi: 10.1136/bmjopen-2017-019615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T., Epel E., Gruenewald T., Karlamangla A., McEwen B.S. Socio‐economic differentials in peripheral biology: cumulative allostatic load. Ann. N. Y. Acad. Sci. 2010;1186(1):223–239. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- Seeman T.E., McEwen B.S., Rowe J.W., Singer B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T.E., Singer B.H., Rowe J.W., Horwitz R.I., McEwen B.S. Price of adaptation—allostatic load and its health consequences: MacArthur studies of successful aging. Arch. Intern. Med. 1997;157(19):2259–2268. [PubMed] [Google Scholar]
- Sibille K.T., McBeth J., Smith D., Wilkie R. Allostatic load and pain severity in older adults: results from the English Longitudinal Study of Ageing. Exp. Gerontol. 2017;88:51–58. doi: 10.1016/j.exger.2016.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sindhusake D., Mitchell P., Smith W., Golding M., Newall P., Hartley D., Rubin G. Validation of self-reported hearing loss. The Blue Mountains hearing study. Int. J. Epidemiol. 2001;30(6):1371–1378. doi: 10.1093/ije/30.6.1371. [DOI] [PubMed] [Google Scholar]
- Szanton S.L., Gill J.M., Allen J.K. Allostatic load: a mechanism of socioeconomic health disparities? Biol. Res. Nurs. 2005;7(1):7–15. doi: 10.1177/1099800405278216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tampubolon G., Maharani A. Trajectories of allostatic load among older Americans and Britons: longitudinal cohort studies. BMC Geriatr. 2018;18(1):1–10. doi: 10.1186/s12877-018-0947-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verschuur C., Agyemang-Prempeh A., Newman T.A. Inflammation is associated with a worsening of presbycusis: evidence from the MRC national study of hearing. Int. J. Audiol. 2014;53(7):469–475. doi: 10.3109/14992027.2014.891057. [DOI] [PubMed] [Google Scholar]
- Verschuur C.A., Dowell A., Syddall H.E., Ntani G., Simmonds S.J., Baylis D., Gale C.R., Walsh B., Cooper C., Lord J.M. Markers of inflammatory status are associated with hearing threshold in older people: findings from the Hertfordshire Ageing Study. Age Ageing. 2012;41(1):92–97. doi: 10.1093/ageing/afr140. [DOI] [PubMed] [Google Scholar]
- Wayne R.V., Johnsrude I.S. A review of causal mechanisms underlying the link between age-related hearing loss and cognitive decline. Ageing Res. Rev. 2015;23:154–166. doi: 10.1016/j.arr.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Zaninotto P., Steptoe A., Gu D., Dupre M.E. Springer International Publishing; Cham: 2019. English Longitudinal Study of Ageing. Encyclopedia of Gerontology and Population Aging; pp. 1–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available by application to the English Longitudinal Study of Ageing (ELSA)